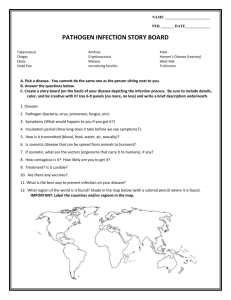
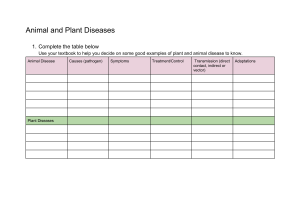
1: Causes of Infectious Disease – How are diseases transmitted? Infectious diseases and disease transmission Classifying different pathogens: (disease causing agents) • Microscopic, cellular (living) o Protozoa: Unicellular eukaryotes, parasites. Usually reproduce through binary fission, motile (moves with flagellum/cilia). Obligate—only continues life cycle in host. o Fungi: Eukaryotic. Can be unicellular (yeast, e.g. thrush) or multicellular (mould, e.g. tinea). Usually attack body surfaces. Consist of branching filaments called hyphae which form a structure called mycelium. Opportunistic—waits for immune system weakness before becoming pathogenic. o Bacteria: Unicellular prokaryotes. Can cause disease by competing with good bacteria or through exotoxins (secreted) or endotoxins (released upon death). Genetic material = 1 circular chromosome. • Microscopic, non-cellular (non-living) o Viruses: Cannot reproduce independently. Have nucleic acid contained in a protein coat/capsid. Can be DNA-based (adenoviruses, e.g. common cold) or RNA-based (retroviruses, e.g. HIV). Invades a host cell, where its nucleic acid is translated into proteins, forming new copies (virions). The cell is filled with these virions and bursts, releasing them. Obligate and intracellular—only reproduces in host. o Prions: An abnormally folded protein. Can convert normal proteins into abnormal form. More stable and resistant to denaturation than normal proteins. There are no known cures. Aggregate together to form amyloid fibrils that cause disease. • Macroscopic organisms (parasites—grows on host and benefits at their expense) o Ecto-parasites: Usually arthropods (insects, spiders). Can directly inject toxins into the body or indirectly cause disease by acting as a vector (organism that transmits pathogen). o Endo-parasites: Usually helminths—worm-like organisms. Live on host’s nutrients, often in digestive system. Disease examples Pathogen Disease Features Bacteria—salmonella enterica Salmonellosis (food poisoning) Vomiting, dehydration, abdominal cramps Fungi—trychophyton Tinea Itchiness, scaliness, yellowing/hardening nails Protozoa—plasmodium spp. Malaria Fever, fatigue, headaches, vomiting Helminth (endo-parasite) —taenia solium/saginata Tapeworm Lack of appetite, restlessness, weight loss, abdominal pain Arthropod (ecto-parasite) —sarcoptes scabei Scabies Itching, red skin, crusting of skin Transmission of disease in an epidemic • Epidemic: affects great no. of people/animals, spreads to new areas • Pandemic: epidemic on a global scale Equine influenza virus • In 2007, several cases of sick horses were reported in Sydney, and also in breeding stallions in Japan. • EIV symptoms: fever, watery nasal discharge, cough, lack of appetite, muscle pain. • Transmission: Highly contagious. Spread directly through horses (nasal secretions, body fluids), and indirectly through humans (contaminated shoes, clothes, grooming equipment, food/water buckets). Spread much faster in areas of high horse stocking density. • Management: Lockdown was put on movement of horses, horse properties quarantined. • Future control: Restrict horse importations, strict biosecurity measures, educate those in the horse industry, biosecurity training. Microbial testing of water/food • Can be done by inoculating nutrient agar plates with food or water samples and incubating at 30 degrees for a few days. • Sterile technique (using alcohol to sterilise workplace and Bunsen burner to sterilise inoculating loop, not opening agar plate more than 45 degrees) is important to prevent contamination and control variables. • Interpreting agar plates (FEMSOC): Form, elevation, margin, surface, opacity, colour. • Bacterial colonies: White/cream, circular/irregular, small, defined margin, look wet and shiny. • Fungal colonies: Appear fuzzy, filamentous margin, powder-like. o Yeasts: White, glossy. o Mould: White/grey/green, fuzzy. Modes of transmission Transmission requires a chain of infection, consisting of a susceptible host, a pathogen, and a mode of transmission. A passive carrier is an uninfected host that can transmit the disease to others, while an active carrier is infected. Active carriers who don’t show signs or symptoms are asymptomatic carriers. Animal diseases that can be transmitted to humans are called zoonotic diseases. • Direct contact: Physical contact. Between child and parent = vertical transmission, other (in same species) = horizontal. Includes touching, biting, blood-to-blood, contact with wounds, sexual contact. • Indirect contact: Uses reservoir outside of host—a fomite = infection carrying object/ substance (e.g. infected water, surface, air, food, unsterilized surgical instrument, spit particles from a sneeze). • Vector transmission: A specific type of indirect transmission. Usually occurs through arthropods (e.g. mosquitoes, fleas, ticks) but sometimes fungi, plants and mammals such as bats. Often transferred when insects suck blood/are ingested. Vector diseases (e.g. malaria, dengue fever) usually occur in warm, humid conditions. Robert Koch and Louis Pasteur Koch’s postulates • Developed bacteriological techniques and agar plate technique; identified bacterium responsible for anthrax, TB, and cholera; showed specific microbes cause specific diseases. • Developed a system for identifying a pathogen—Koch’s postulates. 1. Microbe must be present in all cases of the disease. 2. Microbe is isolated from host and grown in culture medium (e.g. agar). 3. Microbe is grown and inserted into healthy host, must cause same disease. 4. Microbe is reisolated and grown again in a culture medium, must be proven to be same microbe isolated from first host. Pasteur’s microbial contamination experiments • Proved that microbes caused fermentation (beer/wine), spoilage (food) and rotting. • Pasteur’s 1862 classic XPT: o Filled a swan-necked and a straight-necked flask with broth. Swan-necked remained clear, open flask became cloudy and smelly. o Disproved spontaneous-generation theory (that disease occur spontaneously), proved decay and disease were caused by air-borne microbes—germ theory. • Discovered attenuated (weakened) pathogens could cause immunity, showed relationship between anthrax spores and anthrax infection. • Developed vaccines for chicken cholera, anthrax, rabies, and identified specific parasites responsible for silkworm disease. Causes and effects of diseases on agriculture Types of disease in agriculture: endemic (consistently present), exotic (introduced). Factors that can contribute to infectious disease development include host factors (susceptibility, immune system), pathogen factors (availability, adaptations, virulence factors), and environmental factors (hygiene and density). Factors increasing risk of disease today include increasing mobility of human populations, industrial agriculture, deforestation, irrigation, climate change, pesticide resistance, loss of genetic diversity, and inexperienced farmers. Plant diseases • Plant pathogens: Fungi, bacteria, viruses. • E.g. rust: Fungus invades stem tissue of plants and destroys leaf tissue, reducing photosynthetic capacity. It produces spores which spread to other parts of the plant and other plants until the whole crop is covered. Rust destroyed 15 million tonnes of wheat world-wide annually. • Impacts: Cost millions of dollars, reduce productivity, increase production, impact ability to trade, harm the environment, and decrease plant variety. • Plant disease symptoms: Death of plants, necrosis (tissue destruction), abnormal growth, discolouration, wilting. Animal diseases • Animal pathogens: fungi, bacteria, viruses, arthropods, helminths. • E.g. Classical Swine Fever: Viral infection, last broke out in 1961. Had serious impacts on domestic and export production of pork. • Impacts: Animal deaths, economic loss to farmer, loss of trading opportunities, human illness (zoonooses), low growth rates, loss of fertility, loss of economic value of individual animals. Adaptations of different pathogens that facilitate their adhesion, invasion and transmission For an organism to cause disease it must enter the host, multiply in host tissues, overcome/bypass host defence mechanisms, and damage the host. Adaptations assist this process. Pathoge Virulence factors (adaptations to facilitate adhesion/invasion) n Prions • ‘Piggyback’ other proteins to facilitate movement through the gut. Secrete substances that allow invasion of lymphoid (lymphatic system—removes fluids that leak from blood vessels) tissues. Prions then invade nervous tissues and travel to the brain. • • Adhesion • Viral surface proteins adhere to surface of host cell. Invasion • Viruses enter cell through endocytosis (viruses are enveloped and enclosed in membrane) or by delivering viral genome through pore in membrane. • Adhesion • Use pili and fimbria (hair like structures on surface) • Adhesins on surface resist washing action of secretions (urine, mucus) • Form a biofilm (community of bacteria attached to a host surface). Invasion • Enzymes break down cell • Capsule of biofilm resist phagocytosis (engulfment by WBCs) • Chemicals destroy immune defences • Toxins are secreted to damage cells • • • • Viruses Bacteria Transmission route • • • • • Mainly unknown Vertical (mother to child)—can transmit across placenta/become aerolised. Indirectly through infected meat Direct contact (can be blood-borne— use RBCs to facilitate growth) Indirect contact with fomites Airborne transmission—can stimulate sneezing/ coughing, remain suspended in air Direct contact Indirect contact and infected substances/fomites Airborne— stimulate sneezing/ coughing, resist drying out in air Vector-borne transmission— produces proteins to attach to vectors, vector is unaffected Protozoa n • Microtubule penetrates host cell and facilitates entry, membrane is formed to protect from lysosomes • • Fungi Adhesion • Assisted by cell wall/capsule molecules Invasion • Thermotolerance—heat shock proteins cope with body temperatures • Cell wall and capsules protect fungi from host attacks • Secretion of hydrolytic enzymes damages host cells and provides nutrients MacroHookworms • Secrete proteins that reduce host cell parasites responses Ticks • Secrete molecules to prevent vasoconstriction, clotting or inflammatory response • • • • Faeco-oral (e.g. infected food/ water)—induces diarrhoea and transmission Direct contact Direct contact Airborne transmission Soil-borne—form endospores to resist desiccation (drying), stable in a range of conditions Direct contact 2: Responses to Pathogens – How does a plant or animal respond to infection? Response of a named plant to a named pathogen Root rot/dieback disease • Cause: Phytopthora cinnamomi fungus • Symptoms: Wilting, decreased fruit size, necrosis, plant death. • Pathogen o Thrives in moist conditions and lives in soil, plant tissues, and water o Feed off root and stem tissue of plants, leaving lesions in plant and reducing movement of water and nutrients o Can become dormant in harsh weather and germinate in suitable conditions o Transmits indirectly—water-borne and soil-borne • Plant response (e.g. Banskia) o Polygalacturonase inhibitor proteins inhibit the activity of pathogens in penetrating cell wall o Chemical compounds ward off fungus and reduce growth o Enzymes are produced to break down toxins released by fungus o Chemical receptors activate active defence—hydrogen peroxide is released to kill fungus, cell wall is reinforced to seal off fungus. Analyse responses to the presence of pathogens by assessing physical and chemical changes in animal cells and tissues Physical barriers • Skin: Consists of outer epidermis, dermis, hypodermis. Good blood supply = access for WBCs, RBCs, platelets. Epidermis is covered in keratin (waterproof protein = extra barrier). Upper epidermis = barrier of dead skin cells. • Mucous membrane: Line body cavities. Features—cilia (to remove particles), secrete protective substances (mucus traps and flushes away foreign substances) • Tight junctions: Line blood vessels to prevent diffusion of pathogens. • Peristalsis: Alimentary canal (mouth to anus) contracts, moving food and preventing bacteria from reproducing. • Vomiting, diarrhoea, increased urination: expel harmful substances and pathogens. Chemical barriers • Urine: Antimicrobial peptides secreted along urinary tract prevent bacteria binding to cells and break down bacterial cells. • Sweat: Secretes lysozomes that lyse (break down) bacterial cell walls. • Saliva: Has a flushing action and antimicrobial molecules. • Tears: Produced by lacrimal glands, contains antimicrobial substances. • Gastric secretions: Hydrochloric acid’s high acidity discourages growth and survival of microbes. 3: Immunity – How does the human immune system respond to exposure to a pathogen? Innate and adaptive/acquired immune systems and responses to pathogens Non-specific defence (innate immunity) First line of defence (physical barriers) • Skin: Dry, waterproof surface. Limits pathogen growth and prevents entry. Secretions from sebaceous glands inhibit pathogen growth. • Mucous membranes: Line alimentary canal (mouth to anus), respiratory tract, and urinogenital tract. Secrete substances to trap pathogens and inhibit their growth. • Cilia: Small hairs in nose and upper respiratory tract. Mucous coating filters out microbes. Hairs move pathogens to throat to be sneezed/coughed out. • Chemical barriers: Anti-microbial secretions from skin, stomach wall, mucous membranes, vagina. Stomach and vagina secretions are acidic -> reduce microbe growth. • Other secretions: Lysozymes (enzymes that break bacterial walls) in tears and saliva. Acidity of urine inhibits pathogen growth. Secretions of fatty acids from sebaceous glands in skin reduces microbial growth. Second line of defence • Cells involved o Granulocytes—neutrophils, eosinophils, basophils o Monocytes—macrophages, dendritic cells • Inflammation response (first response) o Area of infection becomes hot and swollen as histamine (hormone) is released into blood, making blood vessels dilate and increase permeability > fluid containing phagocytes (a type of leukocyte/WBC) enters tissues. o Phagocytes engulf and destroy pathogen through phagocytosis. Types of phagocytes—macrophages (chronic infection) and neutrophils (acute infection). o Destroyed pathogens, phagocytes and body cells are known as pus. Pus is carried to lymph nodes (swell in process) to be filtered. • Granuloma o If inflammation cannot kill a pathogen, macrophages assemble around pathogen to seal it from food supply and kill it. This is a granuloma. • Fever o Pyrogens (chemicals) are released by phagocytes into the blood, where they travel to the brain, causing body temperature to raise to about 40 degrees to decrease pathogen growths/survivability. Specific defence (adaptive immunity) Third line of defence • Antibodies: Produced by lymphocytes (a form of WBC found in lymphatic system) when antigens (foreign objects) are detected in body. Each is specific to a specific antigen. They combine with antigens to kill/inactivate them or clump them together so macrophages can find them easier. • B-cells: Lymphocyte made in bone marrow. Naïve until exposed to antigen, then they differentiate. Achieve antibody mediated immunity. o Plasma B-cell: Produce antibodies. o Memory B-cell: Remain in body to detect later infection by same antigen. Required antibody can be produced quickly in large amounts. • T-cells: Lymphocyte made in bone marrow and thymus gland. Achieve cell mediated immunity. o Killer T-cell: Attack and destroy macrophages that have engulfed antigens. o Helper T-cell: Secrete chemicals to stimulate B and T cell cloning. o Memory T-cell: Remain in body and reactivate quickly with future infections from same antigen. o Suppressor T-cell: Inactivate B and T-cells when antigen is destroyed. 4: Prevention, Treatment and Control – How can the spread of infectious disease be controlled? Interrelated factors involved in limiting local, regional and global spread of a named disease Local • Sanitation—waste and sewage disposal • Overcrowding • Communication networks and roads • Education • Animal husbandry practices • Local cultural/spiritual beliefs (e.g. Madagascar—famadihana, involves dancing with dead relatives -> plague outbreak) Regional • Geography (e.g. mountains, deserts, rainforests) • Rainforest destruction • Mobility/isolation • Bacteria/viruses in seafood in coastal regions • Trade of fresh food • Seasonal variations in temperature Global • Mass international travel • Migrants—food insecurity, overcrowding, lack of access to healthcare • Pre-migrant medical examinations • Misuse of antibiotics • Ease of communication via internet Polio vaccination campaign (1980s)—factors • Local: Faeco-oral transmission, water sources and waste systems, sanitation and hygiene, rumour that vaccines were sterilisations to reduce Muslim populations, danger to polio-eradication workers • Regional: Political and military instability • Global: Disease occurred in most countries, international travel, worldwide eradication was questioned Procedures employed to limit the spread of disease Hygiene practices • Policies/guidelines: Safe Water System, 1997 Food Regulation, Universal Precautions • Sewage/garbage disposal • Filter/chlorinate drinking water, narrow-mouth plastic containers • Washing hands • Cough/sneeze etiquette • Cover hair/skin lesions when preparing food • Clean/sterilise medical equipment • Gloves (change every patient) and masks while treating patients • Cooking food thoroughly Quarantine • = period of compulsory isolation on animals/items. • Helped our nation to be one of the few free from sever pests and diseases. • Seeks to prevent entry of harmful disease and pests. • Department of Agriculture and Water Resources (DAWR) screens and inspects thousands, and uses pre-border, border and post-border quarantine. • They use research, international resources/intelligence, monitoring, etc. • Quarantine involves fumigation and destruction of infected goods. • Works closely with other government agencies—ACBPS, FSANZ, DHA • Measures: Legislation, border control, dog teams, X-ray inspection, surveillance, quarantine (plants and animals, mosquito trapping programs, public awareness campaigns (Quarantine Matters w/ Steve Irwin), Northern Australia Quarantine strategy (early warning system—sentinel animals are checked for diseases and used to detect entry of diseases) Vaccination (passive and active immunity) • First vaccine: Developed by Edward Jenner in 1976 for smallpox -> eradicated the disease. • Vaccine for polio in 1955 -> reduced cases by 80% • Active acquired immunity: immune response occurs, memory cells produced. o Naturally induced: Body undergoes immune response and suffers disease. o Artificially induced: Through vaccines, which contain modified toxins—toxoids; attenuated (weakened, e.g. rabies), dead, or similar but less harmful pathogens (e.g. cowpox for smallpox). o If antigen reinfects body, secondary response occurs, producing many memory cells and antibodies -> destroy antigens before disease develops. o Booster shots over years -> lifelong immunity, counteracts decrease of memory cells. o -> Herd immunity. • Passive acquired immunity o Artificial: Introduction of antibodies from someone who has experienced the disease (immunoglobulins) into the body to prevent disease development -> short-term immunity (couple months) as no memory cells are produced. o Natural: E.g. mother’s antibodies -> child through placenta or milk. • Advantages: Active immunity, limit disease spread, eradicate disease, decrease healthcare costs. • Disadvantages: Possible mild symptoms, human error, allergies. Public health campaigns • Sewage treatment, garbage disposal, pollution monitoring • Advertising campaigns (e.g. Slip Slop Slap, Grim Reaper ads for AIDS) • Screening programs (BreastScreen, bone density tests for osteoporosis) • Laws/regulations (1997 Food Regulations, diseases classified as ‘notifiable’ e.g. AIDS) • Immunisation • Quarantine Pesticides • Chemicals that destroy pests—e.g. disease vectors, damage crops • DDT—used to kill mosquitoes and prevent spread of malaria, now banned in many places due to negative ecological and health effects (e.g. reduced fertility, breast cancer) • Organophosphates, pyrethrums—safer, popular, used to control mosquitoes. • Other uses—e.g. spraying potato crops to destroy aphids with the potato leaf roll virus. Genetic engineering • Uses biotech to alter genotype of an organism -> creates disease-resistant transgenic organisms -> prevent and control spread of disease. • E.g. Bt cotton—contains Bt bacterium gene that produces toxins to kill certain insects. • E.g. Inserting human insulin gene into E. Coli bacteria -> produce large amounts of insulin to treat diabetes. Effectiveness of pharmaceuticals in treating and controlling infectious disease Antibiotics • Chemicals made by microbes to kill/inhibit microbes by targeting prokaryotic metabolism, destroying cell walls (e.g. penicillin), inhibiting DNA production (e.g. tetracyclines), destroying membranes/enzymes/ribosomes etc. • Selectively toxic—can target fungi, bacteria, protozoans. • DO NOT work on viruses (as they have no metabolism), but can be prescribed to prevent secondary infections. • -> reduce mortality and disease rates. • Can be broad spectrum (act against range of microbes e.g. tetracyclines) or narrow spectrum. • Effectiveness has diminished—bacteria evolving/conferring resistance (e.g. Golden Staph), people not taking whole course, over-prescribed antibiotics. Antivirals • Inhibit development of viral infections (DO NOT cure them) • Target virus-specific features—e.g. target the capsid, prevent virus entry, prevent virus releasing DNA/RNA into cell. • E.g. anti-herpetic agents (Helpin), anti-influenza agents (Tamiflu) Environmental management and quarantine methods used in epidemics/pandemics Ebola Virus 2014-16 • Severe infectious disease, causes rapid death (50% death rate), spread through direct contact, a zoonose. • Management incl. broad spectrum antibiotics, replacement of lost fluids. • Admin control—organisation of response, allocation of tasks • Environmental control—facilities for barrier nursing, hand hygiene, waste management (leak proof bags, covered bins), PPE (masks, gloves, waterproof boots, respirator, suit), surfaces sterilised every day. • Quarantine—isolate patients in single room/at least 3m between patient beds. Same clinical staff and equipment assigned to single patients. Visits restricted. • Work w/ and educate community on transmission and prevention. Incidence and prevalence of infectious disease in populations Mobility of individuals, and portion that are immune/immunised • Incidence: New cases during a certain time. • Prevalence: Proportion of population with a disease at a certain time. • Historical mobility o Silk Road—trade route from China to Europe -> spread the Black Death. o Christopher Columbus—introduced 30 infectious disease into the Americas e.g. smallpox, malaria. • Modern mobility o Mobility in WWI spread the Spanish flu -> killed more people than died in the war. o HIV—originated in Democratic Republic of Congo. Increased, improved, cheaper travel options -> pandemic by 1980s. o Urbanisation -> overcrowding, pressure on healthcare, increasing homeless population, poor living conditions -> spread of disease e.g. TB, ebola. • About 86% of the global population is immunised today. Malaria/Dengue Fever in South East Africa • Seasonal disease, first roughly 20 weeks of 2019: o E.g. Malaysia: 50,000+ cases, 0.002% prevalence, 2x higher than last year. o E.g. Singapore: Almost 4000 cases, 0.0007% prevalence, 4x higher than last year. • Climate change -> increase spread. • Dengue causes 10 million cases and 10,000 deaths per day. Historical, culturally diverse, and current strategies to predict and control spread of disease Historical John Snow, 1854 London cholera outbreak—used maps to record deaths and pinpoint the pathogen source Egypt, 69-30 BCE—Cleopatra used mosquito nets. Middle Ages—bodily fluids (‘humours’) balanced through purging, bleeding, etc. Pleasant scent from pomander (container w/ spiced wax) used to repel Black Death. Plague doctors wore full length gowns and masks. Culturally Philippines—traditional foods, e.g. garlic and onion, contain quercetin to diverse lower blood pressure. Traditional Chinese Medicine—acupuncture, herbal medicine, specific diet, massage, etc. Bitter and cold herb formula treatment, herbs incl. ginseng, honeysuckle -> antibiotic properties. Current Australia’s National Framework for Communicable Disease Control— prevention, detection and response. Surveillance system—detecting disease, notifying organisations e.g. National Notifiable Diseases Surveillance System -> investigation, control. Quarantine (e.g. severe acute respiratory syndrome outbreak in 2003, people isolated in houses/homes) Contemporary application of Aboriginal protocols and importance of recognising/ protecting Aboriginal cultural/intellectual property Bush medicine • Plants substances used include tannins, oils, alkaloids, etc -> antimicrobial properties. • Animal fat often incorporated into medicines to increase fat solubility and absorption rates. • Plants may be crushed and applied to skin (e.g. Witchetty grubs for burns), drunk, inhaled, mashed up and ingested (e.g. clay to deactivate gastrointestinal toxins). • Tea tree oil: Traditionally brewed/consumed -> antiseptic properties. Now used as a household cleaner, to treat fungal infections and skin issues. • Kakadu plum: Richest vitamin C source in the world. Traditionally used as antiseptic and healing agent. Today known to contain phytochemicals that work as antimicrobials/inflammatories, and now used in cosmetics, vitamins, pharmaceuticals and food. • Emu Bush: Traditionally used to treat wounds, ailments, infections, etc. Now known to have antibiotic properties equal in strength to antibiotics -> trialled for use as a sterilisation medium for prosthetic implants. Cultural/intellectual property • Indigenous cultural heritage needs to be protected from commercialisation and exploitation. • Australian laws do not adequately recognise/protect this. • Many pharmaceutical companies have exclusive rights to native Australian plants -> Indigenous people cannot use them. • 1933—Julayinbul Statement on Indigenous Intellectual Property Rights -> insisted that ATSI property be acknowledged. • Ongoing concerns -> Australian Government Intellectual Property legislation, 2015; Nagoya protocol—official agreement to protect ATSI biological resources. Smokebush in Western Australia • Grow in SW Western Australia, NSW, TAS. • Often have big, woolly white flowers, member of Protaceae family. • Currently investigated for potential use against cancer and HIV/AIDS due to chemical concurovone. • 1990s—WA gave Amrad (VIC biotech company) the rights to smokebush to develop an anti-aids drug. There were projected royalties of $100 million per year by 2002, but Indigenous people weren’t recognised and would receive no profit, even though Nyoongah people had used smokebush for centuries.