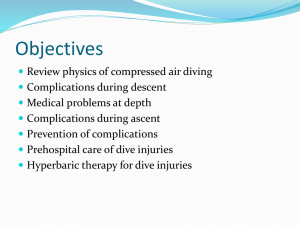
[Section head] 21 Environmental Emergencies [Chapter head] 21.xx the pt with a Diving Emergency Concepts used in this chapter include: [sub head] Overview A large number of Australians engage in compressed gas diving for recreational, scientific and occupational reasons. All patients with complaints after diving should seek some form of medical advice. Some of them will need specialist hyperbaric unit review. Symptoms can range from minor ear pain to sudden death Prehospital management of patients with significant diving related illness should involve oxygen, positioning the patient supine, fluids and transport to a recompression facility Exposure of patients to altitude may worsen symptoms [sub head 1] Case Study Case xxxx,15:30. Dispatch Details: A 24 year-old female was involved in a training dive to 10 meters for 10 minutes, when she panicked and rapidly ascended to the surface. She cried out on surfacing and lost consciousness immediately afterwards. She was rescued into the boat and is returning to shore. The boat ramp is 20 minutes from the nearest tertiary hospital and 45 minutes from the nearest hyperbaric chamber. 1 Initial Presentation, 16:05: The ambulance crew finds the patient dressed in a wetsuit lying on the deck of the boat receiving high flow oxygen via a face mask. She is confused and agitated. She has a dense right hemiparesis. Her observations are unremarkable apart from a GCS of 13. [sub head 1] Definition need ref [sub head 1] Pathophysiology Most diving related emergencies result from the consequences of a diver’s exposure to air (or other gasses) at higher than normal pressure. There are two broad categories of problems 1. Barotrauma 2. Decompression sickness (or the bends) [margin note] [end note] 1. Barotrauma Barotrauma refers to physical damage to tissues caused by changes in volume of gas filled spaces as a consequence of changes in pressure. It arises as a consequence of Boyle’s law which states that at constant temperature, the volume of a gas is directly proportional to the pressure of that gas. This means that if the pressure of a gas doubles its volume will halve and vice versa. The pressure at sea level is about 100 kilopascals or one atmosphere absolute (ATA). Pressure increases by one atmosphere for every 10 meters a diver descends (see table). Depth (meters of seawater) Pressure (ATA) Gas volume Gas density Surface 1 100% 1 10 2 50% 2 20 3 33% 3 30 4 25% 4 2 . . . . 60 6 16% 6 etc Barotrauma can occur as the diver is descending or ascending. Descent barotrauma is caused by gas filled spaces becoming smaller as the pressure increases and ascent barotrauma is caused by gas filled spaces becoming bigger as pressure decreases. Any gas filled space in the body can be affected by barotrauma but the most clinically significant things affected are the, sinus, face mask, ears and, most importantly the lungs. Sinuses Sinus barotrauma occurs on descent. As the pressure surrounding the diver rises, the volume of gas in the sinuses tends to decrease. Unless gas is added to the sinuses, the decrease in volume will casue some tissue damage, namely oedema and bleeding. Symptomatically the diver will experience pain in the sinuses which may be relieved by ‘equalising’ the pressure. If the diver continues the dive the pain will decrease as the sinuses become filled with oedema fluid and blood. On ascent this fluid and blood will be expelled through the nose. Sinus barotrauma is self limiting and does not cause serious morbidity. Ears Lungs 2. Decompression sickness Decompressin sickness (DCS) is an acute condition that occurs following an acute reduction in ambient pressure. It is caused by bubbles which form when the partial pressure of a gas dissolved in the blood or a tissue exceeds the ambient pressure. DCS was first described in compressed air workers in tunnels in the 19th centurty (Caisson disease) and subsequently observed in divers, high altitue pilots and astronauts. Bubbles can form in the venous blood or in pretty much any tissue. Bubbles cause symptoms by both direct mechanical effects and by acting at the cellular and tissue level. Bubbles can cause endothelial disruption, complement activation, platelet activation, nitric oxide production and leukocyte activation. Commonly affected tissues include: Tissue/organ affected Effects Joints/bones Local pain (may be severe). Bone necrosis if repeated Spinal Cord Neurological symptoms Veins Spinal cord venous stasis and infarction. Cardiopulmonary collapse with massive bubble load blocking the pulmonary venous circulation. Arterial bubbles if there is a right to left 3 shunt present Brain Any conceivable neurological symptom or sign Inner ear Vertigo and hearing loss Skin Rash and bruising [box] Definitions: Decompression sickness (DCS) is caused by bubbles forming from gas coming out of solution. Arterial gas embolus (AGE) is caused by bubbles moving directly from the alveolus to the arterial circulation. Decompression illness (DCI) describes both decompression sickness and arterial gas embolus. [end box] [sub head 1] Clinical Reasoning 1: Assessment Patient History This patient has serious neurological symptoms and signs following a rapid ascent form a short, shallow dive. She almost certainly has a cerebral arterial gas embolus. Given that the diagnosis is not in doubt the issues for the paramedics are about how to prevent the situation from deteriorating and what is the most appropriate transport destination. An initial set of vital signs will act as a baseline against which to measure any changes. [box] HISTORY Ask! Details of the dive (depth, duration, first dive of the day?) Are the symptoms better or worse? [sub head 1] Clinical Reasoning 2: Confirm! Are You Sure? Part of the clinical reasoning process is to take your initial hypothesis and seek to confirm of challenge it by finding clinical signs that should occur with your provisional diagnosis. 4 What other possibilities are there? It is unlikely that the presentation could be due to another diving related cause (and unimportant given that the prehospital treatment doesn’t change. A non diving related cause is also unlikely given the history. [box] DIFFERENTIAL DIAGNOSIS Cerebral arterial gas embolus, or Trauma Toxins Hypoxia CVA Subarachnoid haemorrhage Hypoglycaemia Cardiovascular [sub head 1] Clinical Reasoning 3: Treatment Emergency Management Safety Pissing in boats Positioning If the patient has circulating arterial bubbles then these bubble may travel against the direction of blood flow to whichever area of the body is highest (ie they will ‘float’). So if the patient is positioned with the head up bubbles will go to the brain and worsen the damage. Because of this it is vital that patients with possible CAGE are kept supine at ALL times. [box] DISCUSSION TOPIC: If bubbles travel to whichever part of the body is the highest, why not transport them feet up? [end box] Detail yes 5 Oxygen Oxygen is indicated for all patients with significant diving related illness. Bubbles are in equilibrium with gas dissolved in the surrounding tissues, so, in patients breathing air, they are composed mainly of nitrogen..why (with smaller amounts of oxygen, carbon dioxide and water). By eliminating nitrogen from the inspired gas the nitrogen in the bubbles will be reabsorbed into the venous circulation and the bubbles will shrink. So some oxygen is good, more is better and 100% inspired oxygen is best. Transport Definitive management of cerebral arterial gas embolus is recompression in a hyperbaric oxygen facility, and transport should not be delayed in these patients. If possible the patient should be transported to a hosital with a hyperbaric facility and other hospitals should be bypassed, unless there are procedures such as endotracheal intubation and resuscitation that are immediately required and are beyond the skills of the crew in attendance. Notification of the receiving hospital with patient details (including the details of the dive) can assist in preparing the hospital. A phone call to the Diver’s Emergency Service can help the paramedics with treatment advice and contact with hyperbaric staff at the treating facility. [box] The Diver’s Emergency Service: The Royal Adelaide hospital Hyperbaric Unit provides a 24 hour medical specialist cover of the Divers Emergency Service (DES) telephone. This can be accessed by calling: Within Australia (Toll Free) 1800 088 200 Outside Australia +61-8-8212 9242 The service primarily acts as a consultation service for diving-related emergencies. The hyperbaric specialist on the DES phone can provide diagnostic and treatment advice as well as liason with local hyperbaric facilities [end box] [sub head 1] On-Going Management Definitive treatment for decompression illness is obviously not usually available in the prehospital environment so management of conscious patients should be supportive of symptoms and all efforts focussed on delivering the patient to definitive care. [insert clinical reasoning model] 6 Fluids Endothelial damage caused by bubbles causes vasodilation and increased capillary permeability leading to loss of circulating blood volume see SIRS. Administration of fluids to support perfusion should be commenced according to local guidelines. Consulting with the receiving hospital is recommended and transport must not be delayed in order to gain IV access. Pain Relief Opioid pain relief should be considered according to local guidelines for patient comfort but with careful consideration of side-effects. [box] PRINCIPLES OF MANAGEMENT Decompression illness POSITIONING: Keep the patient supine at ALL times OXYGEN: 100%. FLUIDS: To maintain perfusion TRANSPORT: To recompression facility SUPPORTIVE: Manage pain, nausea as required. [end of box] On-Going Management Recompression therapy for decompression illness Patients with DCI need recompression to resolve symptoms and help prevent long term morbidity. All Australian and New Zealand tertiary hospital hyperbaric facilities can offer full intensive care treatment and monitoring to patients in the hyperbaric chamber. Once assessed patients are placed in the chamber on 100% oxygen. The chamber is then pressurised to at least 2.8 ATA (the equivalent of 18m of seawater) so the patient has an FIO2 of 2.8ATA (compared with 0.2 in a patient breathing air at sea level). The increased pressure will cause bubbles to shrink (in accordance with Boyle’s law), and increase the partial pressure of nitrogen in the bubbles. The 100% oxygen will create a large gradient for the nitrogen in the bubbles to be reabsorbed. 7 The hyperbaric oxygen has a number of beneficial physiologic effects including changes in neutrophil marginalisation, changes in nitric oxide levels and many others. Evaluate [box] EVALUATE IS YOUR PT . . . Protecting their airway and ventilating adequately? Consider intubation to ensure airway protection and adequate ventilation. Adequately perfused? Commence or increase IV fluid infusion rate. Ensure receiving hospital is notified. [box] SITUATIONAL AWARENESS Suspect call [end box] [sub head 1] Long term Impact [sub head 1] Summary Case Study 2 [sub head] 12:20. Dispatch: “Case xxxx, A 38 year-old male collapsed after climbing steps following surfacing from a 30 minute dive to seven meters. Breathing but coughing 8 pink, frothy sputum [sub head] ASSESS 12:33. Arrival at scene: Patient is lying on a jetty at the top of a flight of steps. He is anxious and looks unwell 12:40. Primary Survey: Pt has a GCS of 13 (E3, V4, M6) 12.42. Pertinent Hx: Diving with a friend with a maximum depth of 7 meters. He made four or five rapid ascents to the surface during the dive. He developed severe shortness of breath after the last ascent and collapsed walking up the stairs. 12.30. Vital Signs Survey: Difficult assessment due to the presence of a wetsuit PEFUSION STATUS: HR 135 thready, Skin cool, pale and clammy RESP STATUS: RR 45 BPM, coughing. Pink frothy sputum CONSCIOUS STATE: GCS = 13, eyes closed, confused 12:33. Secondary Survey: - No abnormalities found 12:34. Past Hx: Heavy smoker, BMI 40. [sub head] CONFIRM What is your provisional diagnosis? 1. Cardiovascular 2. DCI 3. Near drowning 4. Envenomation 5. Anaphylaxis 6. Poisoning HOW WOULD YOU NARROW THESE? [sub head] ARE YOU SURE? 9 Explore your hypothesis and try to narrow it [box] Planning Is this patient time critical? Is this patient transport critical? What other assessments do you need to consider? Have you got enough history and scene assessment? What are you management regimes you are considering? [sub head] TREAT How would you treat this patient? Consider your clinical decision making for this case and then turn the page. [sub head] ARE YOU SURE? What else could it be? 1. Cardiovascular: A primary cardiac event is possible in an obese heavy smoker. 2. DCI: Coronary AGE is another possibility. 3. Near drowning: Near drowning does not fit the symptoms particularly well given the rapidity of deterioration after the man exited the water by himself. Possible 4. Envenomation: The only envenomation which would fit this man’s presentation is Irukandjii syndrome. This diagnosis needs to be considered if the incident occurred in the Irukandjii jellyfishes distribution 5. Anaphylaxis: Allergen exposure underwater would be quite unusual but anaphylaxis cannot be excluded. 6. Poisoning: Poisoning by contaminated gas is a possibility, a combination of carbon monoxide and inhaled hydrocarbons could explain his symptoms. This is a case where it is impossible to definitely make a diagnosis in the field and the paramedics must manage the patient symptomatically and resolve the basic 10 issues of airway, breathing and circulation before reassessing to see if the underlying cause has become clearer. [sub head] TREAT Oxygen @ 8l/min via BVM and breathing supplemented to 1212:40. Treatment: 16BPM @ 8-10mls/kg Remove the patient’s wesuit 12:45. Evaluate: PEFUSION STATUS: HR 124, Sinus Tach, BP 75/50, Skin cold and clammy RESPIRATORY STATUS: RR 40 BPM, Air Entry L = R, increased work of breathing, widespread fine crepitations CONSCIOUS STATE: GCS = 9 (E2 V2 M5) . [head] Case Study 3 [sub head] A 40 year-old male complains of severe dizzyness and vomiting following a 90 meter cave dive near Mt Gambier 11:15. Dispatch: “Case xxxx, A 40 year-old male has surfaced after a 90 meter dive and developed vertigo and vomiting shortly afterwards. He is lying in a paddock. Mt Gambier is a large town in the South East of South Australia. It is 4 hours by road from the nearest hyperbaric facilities in Adleaide and Melbourne. The local hospital has an Emergency Department with 24 hour staffing and a High Dependency Unit. [sub head] ASSESS 11:48. Arrival at scene: Crew are met at the paddock gate by a group of divers and escorted to the patient, who is lying on the ground wearing a drysuit. The crew are told that the diver became unwell shortly after climbing 15 meters up a rope ladder following a 120 minute, 90 meter decompression dive using a closed circuit rebreather, breathing trimix (a mixture of helium, oxygen and air). The other divers 11 are adamant that the patient cannot be suffering from DCI because they dived strictly according to the profiles provided by their computers. Pt is lying supine and is conscious, but very 11:50. Primary Survey: distressed. He says that the world is spinning around and he is very nauseous, retching frequently. 11.51. Vital Signs Survey: PERFUSION STATUS: HR 115, Sinus, BP difficult to assess due to clothing, Skin cold, clammy RESPIRATORY STATUS: RR 24 BPM, SpO2 96% (Air) GCS: = 15 11:53. Pertinent Hx: The patient denies any significant past medical history or allergies. He had a small amount of trouble clearing his ears at the start of the dive, which was otherwise uneventful. He felt well until just after he finished climbing the ladder. 11:54. Secondary Survey: Head - Profound nystagmus with rapid phase to the left. Neck - Nil abnormalities found Chest - Nil abnormalities found Abdo - Nil abnormalities found Pelvis - Nil abnormalities found Limbs - Nil abnormalities found. Back - Nil abnormalities found. BSL - 6.1 Temp - 36.2 degC [box] HISTORY Ask! Medical Hx Any illicit drugs or ETOH 12 [box] SCENE MANAGEMENT: Does the patient need immediate management? (Are A, B and C adequate?) Is the patient time critical? Do you have the resources you need to manage this patient? Are you going to seek specialised hyperbaric advice or simply transport the patient to the regional hospital? [end box] [sub head] TREAT 11:55. Treatment: Oxygen @ 15l/min via BVM [sub head] CONFIRM What is your provisional diagnosis? 1. DCI 2. Inner ear barotrauma 3. Labyrinthitis 4. Stroke/SAH HOW WOULD YOU NARROW THESE? What else could it be? 1. DCI: The patient has neurological symptoms after a very deep dive. Whilst AGE is unlikely in an experienced diver, DCI is certainly possible, even likley 2. Inner ear barotrauma: The patient’s symptoms are also entirely consistent with inner ear barotrauma. The history of some difficulty with his ears at the start of the dive supports this diagnosis 3. Labyrinthitis: Again the symptoms are consistent with labyrinthitis as a diagnosis, although he would have to be a bit unlucky to develop symptoms immediately after the dive! 4. CVA/SAH: Are possible but much less likely. Cannot, however, be completely excluded. 13 [sub head] CONFIRM This case has the potential to challenge the pre-hospital care provider who may not be familiar with the intricacies of mixed gas, closed circuit decompression diving. The diagnostic uncertainty in this patient is a major issue, in that recompression is mandatory to prevent significant disability if the patient does have DCI, but will possibly do more harm if the diagnosis is inner ear barotrauma. The main issue in this patient is to involve people with the expertise to resolve this uncertainty as soon as possible. This expertise may well not exist in a regional hospital. [sub head] TREAT 12:01. Treatment: CRYSTALLOID FLUID, 20ml/kg 12:02. Treatment: Intravenous antiemetic SCENE MANAGEMENT: After the hyperbaric unit was notified, fixed wing aircraft evacuated the patient sea level. He remained very symptomatic until he was recompressed to 18 meters on oxygen, but his symptoms did not completely resolve until the treatment was increased to 30 meters. He made a full recovery. The patient requested investigation for a possible patent foramen ovale? Why? [end box] 14