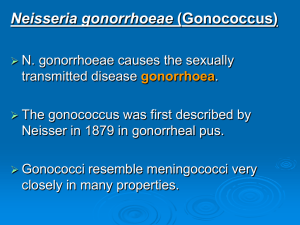
1. 2. 3. 1. 2. CCBS-3 PELVIC INFECTIONS 1. GENITAL ULCER DISEASE Manifests as a breach in the skin or mucosa of the genitalia Herpes simplex virus type 2 (HSV-2) is the most common etiology in most geographic areas Followed by syphilis and chancroid The most important noninfectious cause is behçet’s disease In chancroid, a cytotoxin secreted by Haemophilus ducreyi - important in epithelial cell injury Pathogens Common infectious etiologies of genital ulcer disease include: HSV-2 - genital herpes Treponema pallidum - primary syphilis H. ducreyi – chancroid Less common pathogens include: Chlamydia trachomatis serovars L1–3 - lymphogranuloma venereum Klebsiella granulomatis - granuloma inguinale/ donovanosis STD’S Diagnosis Sexual and medical history Physical examination Clinical characteristics Often overlap in presentation May also be multiple syndromes copresenting Therefore, diagnostic testing is highly recommended Testing for other Sexually transmitted diseases including human immunodeficiency virus (HIV) is also important because there is often cotransmission of multiple pathogens Treatment & Prevention Genital herpes is acyclovir, famciclovir or valacyclovir Primary and secondary syphilis – long acting penicillin, benzathine penicillin G Chancroid - azithromycin Lymphogranuloma venereum – doxycycline Consistent use of condoms Partner notification and treatment 2. VAGINITIS Inflammation of the vagina that can result in discharge, itching, and pain Common causes of vaginitis are: Candidiasis Trichomoniasis Bacterial vaginosis Noninfectious causes - lichen planus and certain medications (e.g., oral contraceptives Patients are usually prompted to seek medical attention because of an abnormal vaginal discharge This may be accompanied by pruritus, pain (including dyspareunia), and symptoms of vaginal irritation Pathophysiology The use of antibiotics that inhibit the normal flora of the vagina, especially lactobacilli, predisposes to Candida vaginitis Candida is a member of the normal flora of many women The pathogenesis of bacterial vaginosis is uncertain, but it does not appear to be a sexually transmitted disease Trichomoniasis - sexually transmitted disease Pathogens Candida albicans is the most common cause of vaginal candidiasis Trichomonas vaginalis is the cause of trichomoniasis Overgrowth of bacteria such as Gardnerella vaginalis is implicated in bacterial vaginosis, but anaerobes such as Mobiluncus are also involved Diagnosis Careful history - time of last menstrual period, medications, and sexual activity Physical examination - microscopic examination of the vaginal discharge itself on a glass slide using a drop of 0.9% saline solution (to look for motile trichomonads or clue cells), followed by a drop of 10% potassium hydroxide (to look for Candida) Clue cells as large, vaginal epithelial cells dotted with bacteria - Gardnerella Appearance of the yeasts and pseudohyphae of Candida Cultures for Gardnerella are not done because at least 50% of asymptomatic women carry the organism Treatment Metronidazole is the drug of choice for both bacterial vaginosis and trichomoniasis For candidiasis, either oral fluconazole or vaginally administered miconazole or butoconazole is the drug of choice T. vaginalis is a sexually transmitted infection, so a one-time treatment regimen of patient and partner is preferred 3. CERVICITIS Cervicitis is inflammation of the uterine cervix Acute cervicitis is usually due to a sexually transmitted infection caused by either C. trachomatis or Neisseria gonorrhoeae or both Other less common etiologies include HSV and T. vaginalis Clinical Manifestations A large proportion of women with cervicitis are asymptomatic In many cases, cervicitis is detected on speculum examination and/or following routine screening for C. trachomatis and N. gonorrhoeae Women who have concomitant urethral infection may have dysuria On physical examination, increased friability of the cervical tissue after a swab is inserted may be a clue to the diagnosis Diagnosis A clinical diagnosis may be made based on increased friability of the cervix, with or without mucopurulent discharge To make a laboratory diagnosis, nucleic acid amplification testing (NAAT) for C. trachomatis and N. gonorrhoeae is routinely performed in many centers If NAAT testing is not available, then Gram stain and culture may be performed Treatment If there is clinical evidence of cervicitis, empiric treatment for both C. trachomatis and N. gonorrhoeae (ceftriaxone intramuscularly plus azithromycin orally) is recommended, particularly if follow-up of test results by the patient is uncertain Sex partners of patients with a confirmed diagnosis should also be notified and treated Prevention Consistent use of condoms is an important measure that can prevent sexually transmitted diseases Partner notification and treatment are important prevention strategies as well 4. PELVIC INFLAMMATORY DISEASE Pelvic inflammatory disease (PID) is a polymicrobial infection of upper genital tract structures, namely the uterus, fallopian tubes, and ovaries Pathophysiology When the endocervical canal barrier is compromised, vaginal bacteria can ascend into the normally sterile space of the upper genital tract (uterus, fallopian tubes, and ovaries) A sexually transmitted infection affecting the cervix (e.g., N. gonorrhoeae and C. trachomatis) can initiate the process, permitting the anaerobic bacteria of the vagina to ascend Having multiple sex partners increases the risk of PID Multiple episodes of PID lead to scarring of the fallopian tubes and an increased risk of ectopic pregnancy and sterility Clinical Manifestations Patients can present with a range of symptoms, from lower back pain to fever, chills, lower abdominal pain, and cervical and adnexal tenderness On physical exam, pain and tenderness on motion of the cervix are important diagnostic signs Pathogens PID is primarily associated with N. gonorrhoeae and C. trachomatis, together with enteric gram-negative rods and anaerobes Diagnosis Because it is often difficult to diagnose PID precisely (given the nonspecific findings) and because the consequences of not treating PID can be grave, many opt to treat with minimum diagnostic criteria such as uterine, adnexal, or cervical motion tenderness Fever, the presence of leukocytes on cervical or vaginal discharge, elevated C-reactive protein, and laboratory evidence of cervical infection with N. gonorrhoeae or C. trachomatis can increase the specificity of the diagnosis Treatment If symptoms are mild, women can be treated as outpatients with cefoxitin or ceftriaxone (one dose) plus doxycycline (14 days) Metronidazole is sometimes added to the regimen In the inpatient setting, intravenous therapy is preferred Cefoxitin or cefotetan with doxycycline, or clindamycin plus gentamicin are initial options with oral antibiotics only after 24 hours of improvement of the patient 5. URETHRITIS Urethritis is inflammation of the urethra It is usually caused by a sexually transmitted infection, particularly in sexually active men A noninfectious cause is Reiter’s syndrome, an autoimmune disease that includes urethritis, uveitis, and reactive arthritis Clinical Manifestations Dysuria is a common presenting complaint Discharge from the urethra, pruritus, and burning are also common complaints Pathogens N. gonorrhoeae and C. trachomatis are the most common organisms implicated Other organisms include Mycoplasma genitalium and T. vaginalis Diagnosis Nucleic acid amplification testing (NAAT) for C. trachomatis and N. gonorrhoeae is routinely performed in many centers Treatment If there is clinical evidence of urethritis such as a purulent urethral discharge, empiric treatment for both N. gonorrhoeae and C. trachomatis (ceftriaxone intramuscularly plus azithromycin orally) is recommended Prevention Consistent use of condoms is an important measure that can prevent sexually transmitted diseases Partner notification and treatment are important prevention strategies as well CASE A 24-year-old man is referred to the local genito-urinary medicine (GUM) clinic. He has been complaining of recent onset of dysuria and has also noticed a yellowish urethral discharge. He denies any constitutional symptoms, frequency or haematuria. He has not noticed any rash, conjunctivitis or joint pains. His background history is unremarkable. He is heterosexual with a number of sexual partners, and admits to practising unsafe sex Examination General examination is normal. There is a small amount of muco-purulent discharge evident from the urethra, which was mildly erythematous around the meatus. There is no rash visible, nor any evidence of genital ulceration or inguinal lymphadenopathy. The testes and prostate are non-tender and not enlarged. Urine and urethral swabs are taken for investigation. Due to his risky sexual behaviour, blood is taken for syphilis, HIV and hepatitis B. A list of his sexual contacts is requested for contact tracing. INVESTIGATIONS Microbiology Urethral swab Microscopy (performed in the clinic) WBC +++ Epithelial cells ++ Intracellular diplococci (coffee-bean shaped) Microscopy (performed in the lab) WBC +++ Epithelial cells ++ Gram-negative intracellular diplococci Culture: Neisseria gonorrhoeae Urine MC&S Microscopy WBC +++ RBC + Epithelial cells + Bacteria +++ Culture: No growth Urine nucleic acid amplification test (NAAT): positive for Neisseria gonorrhoeae, negative for Chlamydia trachomatis Questions 1. What is the differential diagnosis for a urethral discharge? 2. How is this condition diagnosed? 3. How would you manage this patient? The differential diagnosis of a urethral discharge is classically divided into gonococcal urethritis (GU) and non-gonococcal urethritis (NGU) GU is a sexually transmitted infection caused by the gram-negative diplococcus Neisseria gonorrhoeae There is generally a short history of dysuria and a thick urethral discharge occurring after a recent contact In women the presentation can be slower, and may be asymptomatic Disseminated infection occurs if the organism spreads to the systemic circulation This is characterized by fever, rash and suppurative arthritis NGU presentation tends to be more indolent, with a 3–4-week history being usual The dysuria and discharge are less prominent, and the discharge is more watery than for GU Causes of NGU include: • Chlamydia trachomatis, the most common cause of sexually transmitted infection reported in the UK, especially in young adults and adolescents. Symptoms may come and go over several weeks, and it may appear to spontaneously resolve in some. It may also be asymptomatic, especially in women. There is co-infection with N. gonorrhoeae in about 20% of patients, and empiric treatment will usually treat both these infections simultaneously Mycoplasma genitalium, emerging as a common cause of NGU, and is more commonly symptomatic than C. trachomatis. It is more difficult to diagnose and is therefore sometimes treated empirically • Trichomonas vaginalis infection, a common cause of vaginitis in women and also an important source of urethritis in men. A 22% urethral prevalence was found among male partners of women with known trichomonal infection. The condition should be suspected in patients with symptoms but little or no discharge on physical examination Ureaplasma urealyticum, more recently thought to be a cause of NGU. It may account for 10–40% of NGU cases and is sexually transmitted • Herpes simplex virus infection, most often associated with painful superficial genital ulcers that are usually visible on the external genitalia • Prostatitis, especially in older men with enlarged prostates, predisposing to obstruction and infection. Minor penile discharge may be present. Symptoms of urinary outflow obstruction and perineal discomfort may be the predominant symptoms No test is currently 100% sensitive or specific for N. gonorrhoeae Routine urine MC&S culture media does not support its growth Options for diagnosis of urethritis are microscopy, culture and molecular tests: • Microscopy: staining of the urethral discharge is helpful in looking for pus cells as well as the typical intracellular, bean-shaped diplococci of N. gonorrhoeae If a gram stain is performed the bacteria will look pink in colour (gram-negative) Microscopy has a sensitivity of 90–95% in symptomatic men for N. gonorrhoeae Sensitivity is poor for endocervical (<50%), rectal and throat swabs, and in asymptomatic men (50–75%) Culture: using specific selective media, N. gonorrhoeae will grow if plated soon after the specimen is taken It is a fragile organism and a delay in the specimen reaching the lab will result in a false negative culture, as it will have died en route Thus some GUM clinics plate the specimens directly onto culture plates in the clinic It is not practical to culture for Chlamydia or Ureaplasma because it is technically difficult, takes two to three days to get a result, and is expensive Molecular tests: Nucleic acid amplification test (NAAT) is the standard diagnostic and screening test used for N. gonorrhoeae and C. trachomatis It is >96% sensitive even on asymptomatic cases and can be performed on swabs from any site as well as urine samples from men Sensitivity on urine samples from women is significantly lower than from an endocervical swab and is not recommended N. gonorrhoeae has become significantly resistant to a spectrum of antibiotics There are no longer any oral antibiotics that can be recommended alone for first-line treatment with the certainty of curing the infection First-line treatment for uncomplicated gonococcal infection is currently a single dose of parenteral ceftriaxone with oral azithromycin The azithromycin is thought to have a synergistic effect with the cephalosporin, and is also used to try to delay emergence of resistance to the cephalosporin Testing for cure and contact tracing is recommended after treatment