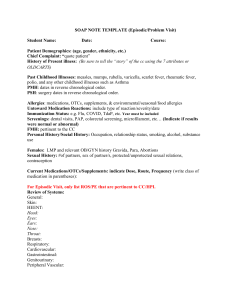
SOAP NOTE TEMPLATE (Episodic/Problem Visit) Student Name: Date: Course: Patient Demographics: (age, gender, ethnicity, etc.) Chief Complaint: “quote patient” History of Present illness: (Be sure to tell the “story” of the cc using the 7 attributes or OLDCARTS) Past Childhood Illnesses: measles, mumps, rubella, varicella, scarlet fever, rheumatic fever, polio, and any other childhood illnesses such as Asthma PMH: dates in reverse chronological order. PSH: surgery dates in reverse chronological order. Allergies: medications, OTCs, supplements, & environmental/seasonal/food allergies Untoward Medication Reactions: include type of reaction/severity/date Immunization Status: e.g. Flu, COVID, TdaP, etc. Year must be included Screenings: dental visits, PAP, colorectal screening, microfilament, etc… (Indicate if results were normal or abnormal) FMH: pertinent to the CC Personal History/Social History: Occupation, relationship status, smoking, alcohol, substance use Females: LMP and relevant OB/GYN history Gravida, Para, Abortions Sexual History: #of partners, sex of partner/s, protected/unprotected sexual relations, contraception Current Medications/OTCs/Supplements: indicate Dose, Route, Frequency (write class of medication in parentheses): For Episodic Visit, only list ROS/PE that are pertinent to CC/HPI. Review of Systems: General: Skin: HEENT: Head: Eyes: Ears: Nose: Throat: Breasts: Respiratory: Cardiovascular: Gastrointestinal: Genitourinary: Peripheral Vascular: Musculoskeletal: Neurologic: Hematologic: Lymphatic: Endocrine: Psychiatric: For Episodic Visit, only list ROS/PE that are pertinent to CC/HPI. Physical Exam: Vital Signs: Blood Pressure- P- RR- T- Height- Weight- BMIGeneral: Skin: HEENT: Head: Eyes: Ears: Nose: Throat: Neck: Breasts: Lungs: Heart: Abdomen: Genitourinary: Rectal: Peripheral Vascular: Lymphatic: Extremities: Musculoskeletal: Neurological: Pertinent Labs/Diagnostic Testing: Indicate any previous labs or diagnostics done that are relevant to today’s visit, as well as any Point of Care Testing (POCT) done during the visit with results. Differential Diagnosis Diagnostic Reasoning Exercise: Minimum of 3 differential diagnoses/maximum of 5 differentials—the table will help with the narrative write-up required below the table. Differential Diagnoses 1. 2. 3. 4. Pathophysiology (include APA citations) Pertinent Positives Pertinent Negatives 5. In a narrative format explain how you arrived at your final diagnosis or working diagnoses based on the CC/HPI, PMH, PSH, ROS, & Physical Exam (pertinent +/– will guide this process). This should be written using examples of how the history/clinical presentation led to the final diagnosis or working diagnosis (APA citations to your references must be included – use resources with Evidence Based Guidelines) Assessment/Plan: Include a brief summary of the visit here (APA citations required in your plan) List diagnoses applicable to your patient encounter. Diagnosis #1 is your primary/working diagnosis made at the time of the visit. If you have not made a diagnosis, then you would use the ICD-10 code for the symptomatology since r/o diagnoses are not billable. This should be followed by a plan of care that is evidenced based. Diagnosis # 1 ICD-10 (must be related to CC/HPI) a. Plan listed here (plan should be evidenced based, if not, state why the plan deviated from the evidence) b. c. Diagnosis # 2 ICD-10 may be a chronic condition which is being followed-up (e.g. Asthma, diabetes) a. Plan listed here b. c. Diagnosis # 3 ICD-10 may be a chronic condition which is being followed-up (e.g. HTN, Asthma) a. Plan listed here b. c. Health Maintenance: Required App for USPSTF screening guidelines https://epss.ahrq.gov/PDA/index.jsp Must list all screenings/lifestyle recommendations that are age appropriate (e.g. seasonal flu vaccine, HIV screening; STI screenings, obesity—nutritional/exercise counseling; smoker— tobacco cessation program, etc.even though you may not address in an episodic visit) RTC: (Document disposition) References (APA Format)