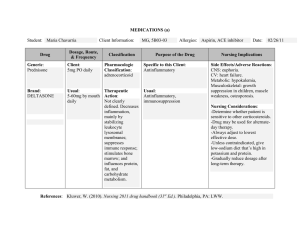
PLAN IHUMAN OF CARE PATIENT ASSESSMENT Age: ____52______ Gender: ____M______ Resuscitation Status _ Full code ________ Allergies__Shellfish____________________ Reason for Admission: ______Total Knee replacement surgery, an elective surgery.____________________________________________________________________________ Medical Diagnoses: ___Chronic Osteoarthritis___________________________________________________________ ________________________________________________________________________________________________________ Surgeries/Procedures and Dates: ____________________________________________________________________________ Past medical history__Chronic osteoarthritis ______________________________________________________________________________________ ________________________________________________________________________________________________________ Current Orders: Diet________NPO until after surgery____________________ Activity________ OOB with assistance ________________________ Intake ___________________ Output_________________ Accu Cheks__no____________________________ Vital signs____ Oral temperature 98.6, BP:122/76, pulse 72 with no diminished pulses to the right lower extremity. Respirations 24, and 98% oxygen saturation on room air.___________________________________________________________________________________________ Drsg changes/wound care_________________Dressing changes:_Incision site on right knee________________________________________________________________ Foley___________________________ NG/G-tube/PEG?PEJ______________________________________________________ IV _______ R forearm, NS 75 mL/hr ; 5 mL q8h _________________ Reason for IV____________________________________________ Other orders: ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ 1 ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ ______________________________________________________________________________________________________ Most recent Imaging Findings: (CXR? CT? MRI?) Type of Imaging (X-Ray, CT, MRI, etc) X-ray Body Area Imaged Reason for testing and results of test Upper and Lower extremity Musculoskeletal fractures, structural abnormalities, location of emboli and thrombi, heart and lung abnormalities. Most Recent Significant /Recent Lab Results: (Chemistry? Hematology? Drug Levels? Coagulation tests?) Date Lab Test Glu BUN Creat Na K Cl Ca CO2 Hct PT INR ABO WBC RBC Hgb MCV Platelets Results 108 18 0.7 135 4.5 99 9.5 22 47 15 0.9 AB Negative 5660 5.2 16 87 296 Norms 70-110 8-21 0.6-1.3 138-145 3.5-5.1 95-102 8.7-10.7 22-29 42-54 11-15 0.8-1.1 Comments Fast blood glucose Kidney fx 4,000-10,000 4.5-5.9 14-18 82-103 150-399 Immune fx Electrolytes ABGs Blood Viscosity Clotting fx O2 carrying capacity of blood Other recent, significant procedures or tests (EKG, etc) Date Test ECG Reason for testing and results of test Pt is overweight and recently stopped smoking a week ago Based on the information on these pages and your assessment of this patient, what is your FIRST or PRIORITY concern and why? 2 Medications You may copy and paste these tables onto the next sheet if you have more medications Brand Name and Generic Name Normal Dosage Ranges 500 mg to 1 gram cefazolin Pharmacotherapeutic Class cephalosporin Dosage Ordered 2 g IV Why is patient receiving this med? (Can list related diagnosis, symptom, or need) Route and Frequency treat certain infections caused by bacteria from joint pain PO every morning Brand Name and Generic Name Normal Dosage Ranges Lactated Ringers 25-50 mg deep IM or slow IV/IO; maximum dose 100 mg Pharmacotherapeutic Class Dosage Ordered Alkalinizing Agents Why is patient receiving this med? (Can list related diagnosis, symptom, or need) used as a source of electrolytes, calories and water for hydration Brand Name and Generic Name 74 mL/hr Route and Frequency During surgery Normal Dosage Ranges 400 to 3000 mg Calcium Carbonate Pharmacotherapeutic Class antacids Dosage Ordered 600 Contraindications patients who have a history of immediate hypersensitivity reactions Adverse Reactions Swelling, redness, pain, or soreness at the injection site may occur Nursing Considerations and Teaching Watch for seizures: Monitor signs of pseudomembranous colitis Contraindications contraindicated where the administration of sodium, potassium, calcium, chloride or lactate could be clinically detrimental. Adverse Reactions localized or generalized hives and itching, swelling of the eyes, face, or throat, coughing, sneezing, or difficulty breathing Nursing Considerations and Teaching Administer only in high acuity areas. For short-term use to correct critical electrolyte abnormalities. Monitor electrolytes and assess for hypervolemia Contraindications hypersensitivity, renal calculus, high urine calcium levels, elevated serum calcium Adverse Reactions upset stomach, vomiting, stomach pain, belching. Medications Why is patient receiving this med? (Can list related diagnosis, symptom, or need) Route and Frequency Nursing Considerations and Teaching may cause cardiac arrest and arrhythmias; Do not continue this medication beyond 1–2 week, since it may cause acid rebound PO qAM relieve heartburn, acid indigestion, and upset stomach. Brand Name and Generic Name Normal Dosage Ranges 50 to 400 mg Contraindications Docusate Pharmacotherapeutic Class Dosage Ordered 100 mg Colace Why is patient receiving this med? (Can list related diagnosis, symptom, or need) stool softener. Brand Name and Generic Name Normal Saline (0.9%) Pharmacotherapeutic Class Crystalloid Fluid Why is patient receiving this med? (Can list related diagnosis, symptom, or need) For Extracellular fluid replacement Route and Frequency PO BID Normal Dosage Ranges recommend aiming for a correction of 8 mEq/L/day; serum sodium should not increase by more than 10 to 12 mEq/L in the first 24 hours Dosage Ordered Normal Saline (0.9%) 75 mL/hr Normal Saline (0.9%) 5 mL IV q8 hours Hypersensitivity reaction to any of the docusate ingredients. Avoid concomitant use of mineral oil; Nausea or vomiting Adverse Reactions Abdominal cramping, Stomach pain, Diarrhea, excessive bowel activities, ntestinal obstruction Nursing Considerations and Teaching cause of constipation Evaluate therapeutic response Contraindications patients with congestive heart failure, severe renal impairment, conditions of sodium retention, oedema, liver cirrhosis and irrigation during electrosurgical procedures. Do not use unless the solution is clear Adverse Reactions Fever, injection site swelling, redness, and infection Route and Frequency Nursing Considerations and Teaching 75 mL/hr 5 mL IV q8 hours May worsen existing hypovolemia and hypotension causing cardiovascular collapse. Monitor for signs of fluid volume deficit, such as confusion in older adults and dizziness. Never administer to patients at risk for increased ICP as the potential fluid shift may cause cerebral edema. Medications Brand Name and Generic Name Normal Dosage Ranges Contraindications Oxycodone Orally 5 to 15 mg every 4 to 6 hours Before using this medication, tell your doctor or pharmacist your medical history, especially of: brain disorders (such as head injury, tumor, seizures), breathing problems (such as asthma, sleep apnea, chronic obstructive pulmonary disease-COPD), kidney disease, liver disease, mental/mood disorders Pharmacotherapeutic Class Analgesic, Opioid Why is patient receiving this med? (Can list related diagnosis, symptom, or need) Pain management related to chronic osteoarthritis Dosage Ordered Oxycodone ER 10 mg PO BID Oxycodone IR 5 mg q4 hours score pain of 4/10 or less Oxycodone IR 10 mg q4 hours score pain of 5/10 or greater Route and Frequency IR 5 mg q4 hours IR 10 mg q4 hours Adverse Reactions Nausea, vomiting, constipation, dry mouth, weakness, sweating, lightheadedness, dizziness, or drowsiness may occur Nursing Considerations and Teaching CNS depression Constipation Respiratory depression May cause severe hypotension Routine Findings Skin –Skin warm and dry. Incision site well approximated with no redness, swelling, or drainage. Area of warmth, redness, and 1+ pitting edema on medial aspect of R calf. R calf is 3 cm wider in girth than L calf. Pt complains of pain upon palpation of R leg Head and neck – Head Normocephalic, atraumatic No deformities Facial feature symmetric Temporal arteries non- tender to palpation Frontal and maxillary sinuses non- tender Eyes Eyes H – Test normal Right pupil normal reactive Left pupil normal reactive External auditory canals clear, hearing intact Eyelids- no ptosis erythema or swelling Conjunctiva- pink, no discharge Sclerae- anicteric Orbital area- no edema, redness, tenderness or lesions noted Mouth/pharynx No hoarseness Clear mucosa, tonsils without exudate Tongue normal color, symmetrical No swelling or ulcerations No unusual smell in mouth Nose No discharge or polyps. No edema or tenderness over4 the frontal or maxillary sinuses Ears Tympanic membrane translucent, pinkish-gray in color Normal landmarks Hearing intact in both ears Neck Trachea is midline and freely mobile No nodes present No asymmetry or accessory respiratory muscle use with quiet breathing Patient Variations/Abnormals 1+ pitting edema on medial aspect of R calf. R calf is 3 cm wider in girth than L calf. Pt complains of pain upon palpation of R leg None to note Respiratory – Clear breath sounds in all lobes. Tachypnea. Breathing unlabored. Cardiovascular S1S2. No adventitious sounds. Pulses regular in all extremities. Cap refill 2 seconds in fingers RR is 24 and normal respiration rate is between 12-20 therefore the patient has tachypnea and toes. No JVD present. 1+ pitting edema in R calf. No diminished pulses in R lower extremity. 1+ pitting edema in R calf Abdomen – Abdomen soft and non-tender. Normoactive bowel sounds in all quadrants. . Bowel continence? normal Last BM? Last night Bowel Plan? n/a Neurological AAO x4. PERRLA. Musculoskeletal - . Upper extremities strength is 5/5 bilaterally. Right lower extremity strength 3/5 bilaterally Left Lower extremity strength 5/5 Right lower extremity strength 3/5 bilaterally Genitourinary – Urinary continence? normal Toileting plan? n/a Voiding clear yellow urine Nursing Diagnosis #1: Ineffective peripheral infusion Related to (RT): Venous spacious, decrease blood flow As evident by (AEB): Swelling, redness, 1+ pitting edema on lower right leg Planning/Desired Outcome(s): Patient identifies factors that improve circulation. Patient identifies necessary lifestyle changes. Patient exhibits growing tolerance to activity. Patient shows no further worsening/repetition of deficits. Implementation/Nursing intervention(s): Rationale Assist with position changes. Gently repositioning patient from a supine to sitting/standing position can reduce the risk for orthostatic BP changes. Older patients are more susceptible to such drops of pressure with position changes. Promote active/passive ROM exercises. Exercise prevents venous stasis and further circulatory compromise. Administer medications as prescribed to treat underlying problem. Note the response. These medications facilitate perfusion for most causes of impairment. Evaluation/Patient Response Assess the site of the problem, patient noted that the pain in his calf has decreased. The was no presents of DVT. Nursing Diagnosis #2: Impaired Physical Mobility Related to (RT): Pain and discomfort, musculoskeletal impairment As evident by (AEB): Limited ROM; decreased muscle strength/control Planning/Desired Outcome(s): Client will display increased strength and function of affected joint and limb. Participate in ADLs/rehabilitation program. Implementation/Nursing intervention(s): Rationale Perform and assist with the range of motion exercises to unaffected joints. Patient with degenerative joint disease can quickly lose joint function during periods of restricted activity. Medicate before procedures and activities. Muscle relaxants, narcotics, analgesics decrease pain, reduce muscle tension and facilitate participation in therapy. Maintain affected joint in prescribed position and body in alignment when in bed. Provides for stabilization of prosthesis and reduces the risk of injury Evaluation/Patient Response Nursing Diagnosis #3: Acute Pain Related to (RT): Pain/discomfort As evident by (AEB): Reports of pain, spasm, tingling, numbness Planning/Desired Outcome(s): Patient will report satisfactory pain control at a level less than 3 to 4 on a scale of 0 to 10. Patient will exhibit increased comfort such as baseline levels for HR, BP, respiration, and relaxed muscle tone or body posture. Patient will engage in desired activities without an increase in pain level. Implementation/Nursing intervention(s): Rationale Evaluation/Patient Response Provide for adequate rest periods Fatigue impairs the ability to cope with discomfort. Assess the patient’s description of pain. Pain may manifest as an ache, progressing to sharp pain when the affected area is brought to full weight-bearing or a full range of motion (ROM). Medicate for pain before activity and exercise therapy. Exercise is necessary to maintain joint mobility, but patient may be reluctant to participate in exercise if they are in too much pain. Problem#__1_______ To Do: Problem#______2___ ND: immunity, Risk for allergic reaction ND: Impaired Physical Mobility RT Pain and discomfort, Medical Diagnoses: Total right knee replacement secondary to osteoarthritis. musculoskeletal impairment AEB Reports of pain, spasm, tingling, numbness assess the pt pain on a pain scale of 0-10 , ten being the worse pain after they finish the exercise therapy to see if the medication work effectively RT pt allergic reaction to shellfish Key Assessments: 1. Knee pain that is gradual in onset and worse with activity AEB the appearance of rashes on his body after consuming the shellfish 2. Knee stiffness and swelling 3. Pain after prolonged sitting or resting. Problem#_____3____ ND: Impaired Physical Mobility Problem#____5_____ Problem#______4___ ND: Lack of activity ND: Behavior changes