Gastrointestinal Diseases: Symptoms, Causes, and Treatment
advertisement
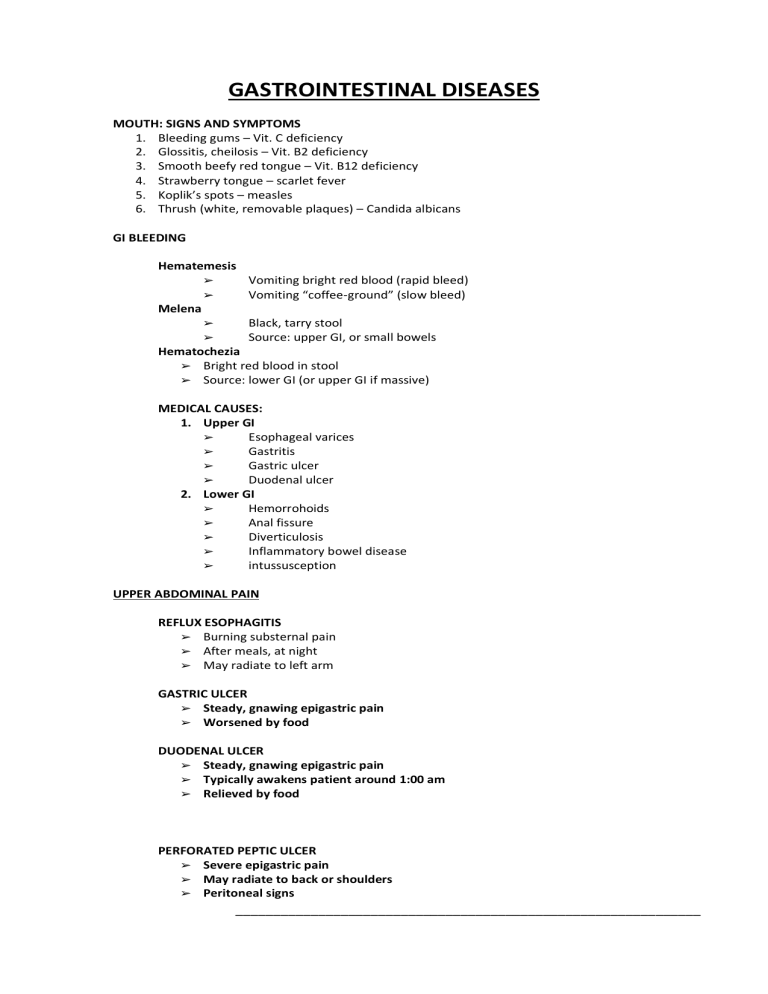
GASTROINTESTINAL DISEASES MOUTH: SIGNS AND SYMPTOMS 1. Bleeding gums – Vit. C deficiency 2. Glossitis, cheilosis – Vit. B2 deficiency 3. Smooth beefy red tongue – Vit. B12 deficiency 4. Strawberry tongue – scarlet fever 5. Koplik’s spots – measles 6. Thrush (white, removable plaques) – Candida albicans GI BLEEDING Hematemesis ➢ ➢ Vomiting bright red blood (rapid bleed) Vomiting “coffee-ground” (slow bleed) ➢ ➢ Black, tarry stool Source: upper GI, or small bowels Melena Hematochezia ➢ Bright red blood in stool ➢ Source: lower GI (or upper GI if massive) MEDICAL CAUSES: 1. Upper GI ➢ Esophageal varices ➢ Gastritis ➢ Gastric ulcer ➢ Duodenal ulcer 2. Lower GI ➢ Hemorrohoids ➢ Anal fissure ➢ Diverticulosis ➢ Inflammatory bowel disease ➢ intussusception UPPER ABDOMINAL PAIN REFLUX ESOPHAGITIS ➢ Burning substernal pain ➢ After meals, at night ➢ May radiate to left arm GASTRIC ULCER ➢ Steady, gnawing epigastric pain ➢ Worsened by food DUODENAL ULCER ➢ Steady, gnawing epigastric pain ➢ Typically awakens patient around 1:00 am ➢ Relieved by food PERFORATED PEPTIC ULCER ➢ Severe epigastric pain ➢ May radiate to back or shoulders ➢ Peritoneal signs ______________________________________________________________ CHOLECYSTITIS ➢ Cramp-like epigastric pain ➢ May radiate to tip of right scapula ➢ Murphy’s sign-painful splinting of respiration during deep inspiration and right upper quadrant palpation. ACUTE PANCREATITIS ➢ Severe, boring abdominal pain ➢ Often radiates to back ➢ Peritoneal signs (rebound tenderness, abdominal rigidity) HIATAL HERNIA 1. SLIDING HERNIA: gastroesophageal junction and part of stomach slide upwards 2. PARAESOPHAGEAL: part of stomach turns adjacent to esophagus Assessment 1. Often asyptomatic 2. Heartburn 3. Regurgitation of food 4. Diagnosis: chest X-ray or barium swallow Implementation 1. If asymptomatic: no treatment necessary 2. Small frequent meals 3. Elevate head of bed to reduce acid reflux 4. Avoid activities that increase abdominal pressure: (lifting heavy objects, bending over etc.) ESOPHAGEAL VARICES Liver cirrhosis: elevated portal vein pressure> esophageal varices Assessment 1. History of alcohol (liver cirrhosis) 2. Hematemesis = vomiting blood 3. Melena = black, tarry stools 4. Signs of shock if bleeding is severe Implementation 1. Watch for hemorrhage, hypotension, signs of shock 2. Monitor vital signs if acute bleeding 3. Watch for signs of hepatic encephalopathy 4. Assist with Sengstaken tube Sengstaken tube (to compress varices) ➢ Monitor bleeding in gastric drainage ➢ Watch for signs of asphyxiation ➢ Watch for tube displacement GASTRITIS Inflammation of gastric mucosa ACUTE GASTRITIS (Erosive) ➢ Acute hemorrhagic lesions ➢ Stress ulcers ➢ Aspirin, NSAIDs ➢ Alcohol CHRONIC GASTRITIS TYPE A (Non-erosive) ➢ Autoimmune gastritis ➢ Involves body and fundus ______________________________________________________________ ➢ Pernicious anemia CHRONIC GASTRITIS TYPE B (Non-erosive) ➢ Involves body and fundus ➢ H. pylori Assessment 1. Nausea, anorexia 2. Sour taste in mouth 3. Belching 4. Cramping, pain Implementation 1. Watch for signs of GI bleeding (“coffee-ground” vomit) 2. CBC if suspected pernicious anemia Medications 1. Antacids 2. Antihistamine (to reduce acid secretion) 3. Antibiotics (to eradicate H. pylori) PEPTIC ULCER DISEASE GASTRIC ULCER ➢ Normal or decreased acid production ➢ Decreased mucosal resistance ➢ Chronic NSAID use ➢ Pain gets worse after meals DUODENAL ULCER ➢ Increased acid production ➢ Pain typically relieved by meals Assessment 1. Gnawing, burning epigastric pain 2. Vomiting 3. GI bleeding>anemia Diagnosis 1. upper GI series or endoscopy 2. test for presence of Helicobacter pylori Implementation 1. Watch for signs of bleeding- “coffee-ground” vomit, tarry stools 2. Avoid irritating food 3. Avoid cigarette smoking 4. Avoid aspirin, NSAIDs and steroids Medications 1. Antihistamine 2. Antibiotics to eradicate H. pylori Note: gastric resection is much common nowadays due to more effective drugs including the use of antibiotics to eradicate H. pylori LIVER: SIGNS & SYMPTOMS ______________________________________________________________ Jaundice - diminished bilirubin secretion Fetor hepaticus - sulfur compounds produced by intestinal bacteria, not cleared by liver Spider angiomas palmar erythema gynecomastia - elevated estrogen levels Ecchymoses(easy bruising) - decreased synthesis of clothing factors Xanthomas(yellow skin plaques / nodules) - elevated cholesterol levels Hypoglycemia –- decreased liver glycogen stores, decreased liver glucose production Splenomegaly - portal hypertension Encephalopathy asterixis (hand-flapping tremor) - portosystemic shunt (digestive products bypass liver and are not detoxified) INDIRECT BILIRUBIN (unconjugated) increased ➢ Hemolytic anemia ➢ Physiologic jaundice of the newborn HBs-Ag ➢ Earliest marker of hepatitis B ➢ Indicates infective state (hepatitis B) JAUNDICE ➢ Skin looks yellow if serum bilirubin > 2mg/dL PREHEPATIC ➢ Hemolysis: sickle cell anemia, Hemolytic anemias (antibodies against RBC’s) HEPATIC ➢ Hepatitis: impaired conjuction of bilirubin by liver cells POSTHEPATIC ➢ Cholestasis: impaired excertion by liver cells (estrogens, some drugs), Bile duct obstruction DRUG INDUCED LIVER DISEASE CHLORPROMAZINE ➢ Reversible cholestasis ETHANOL ➢ Fatty liver, Cirrhosis ACETAMINOPHEN/ CARBON TETRACHLORIDE ➢ Acute liver cell necrosis ESTROGENS ➢ Hepatocellular adenoma (benign) AFLATOXIN HEPATITIS B AND C ➢ Hepatocellular carcinoma IMPLEMENTATION 1. Check skin, gums and stool for bleeding 2. Avoid aspirin 3. Monitor weight 4. Monitor abdominal cicumference 5. If ascites interferences with breathing > high Fowler’s DIET: 1. High carbohydrate, high calorie, vitamins (low protein diet if client has hepatic encephalopathy) 2. Provide counseling if client abuses alcohol GALLBLADDER CHOLELITHIASIS ➢ presence of gallstones in the gallbladder ➢ Usually asymptomatic (70%) ➢ May cause biliary colic (20%) ______________________________________________________________ ➢ May cause cholecystitis (10%) BILIARY COLIC ➢ ➢ ➢ Steady, cramplike pain in epigastrium Murphy’s sign (inspiratory arrest during palpation of liver margin) Pain does not subside spontaneously Implementation 1. No oral food during acute cholecystitis Diagnosis 1. X-ray, ultrasound, scan to visualize stones 2. ERCP to visualize ducts Medications 1. Analgesics 2. Antibiotics 3. Ursodiol: (resolves small cholesterol stones, but does not help in acute attack) Post Operative 1. Monitor T-tube drainage (up to 500ml in first 24h is normal) Client Education 1. Reduce dietary fat and cholesterol intake PANCREATITIS ACUTE PANCREATITIS ➢ Causes – Alcohol abuse, cholelithiasis ➢ Features – Elevate lipase, amylase ➢ Mortality rate – 10% CHRONIC PANCREATITIS ➢ Causes – Alcohol abuse, rarely due to cholelithiasis ➢ Features – pancreatic calcifications Assessment 1. 2. 3. 4. 5. Nausea Severe abdominal pain around umbilicus Abdominal rigidity Signs of shock Dark urine, clay-colored stools if due to bile duct obstruction (stones) Laboratory 1. Elevate amylase, lipase 2. If serum calcium low> poorer prognosis Implementation 1. Keep client NPO 2. Assist with nasogastric tube 3. Monitor vital signs 4. Monitor input/output 5. Assess for respiratory difficulties and base of lungs Client Education 1. Strict avoidance of alcohol MALDIGESTION Dysfunction of pancreas ➢ Chronic pancreatitis ______________________________________________________________ ➢ Cystic fibrosis Lack of specific enzymes ➢ Lactase deficiency Lack of bile salts ➢ Biliary cirrhosis ➢ Resected terminal ileum ➢ Bacterial overgrowth MALABSORPTION Dysfunction of small bowel ➢ Short bowel syndrome ➢ Bacterial overgrowth ➢ Celiac disease ➢ Tropical sprue Note: Diarrhea often leads to transients lactase deficiency: Teach client to avoid milk when having diarrhea of any cause. DIARRHEA Secretory ➢ Large volume watery stools ➢ Persists with fasting ➢ (cholera, dysentery) Osmotic ➢ Bulky, greasy stools ➢ Improves with fasting ➢ (lactase deficiency, pancreatic insufficiency, short bowel syndrome) Inflammatory ➢ Frequent but small stools ➢ Blood and/or pus ➢ (inflammatory bowel disease, irradiation, shigella, amebiasis) Dysmotility ➢ Diarrhea alternating with constipation ➢ (irritable bowel syndrome, diabetes mellitus) LOWER ABDOMINAL PAIN Appendicitis ➢ Vague periumbilical pain, nausea ➢ Later localizes to lower right quadrant ➢ Perforation: high fever and leukocytosis Diverticulitis ➢ Elderly patients ➢ Steady pain ➢ Localized to lower left quadrant ➢ Left sided appendicitis Inflammatory bowel disease ➢ Chronic, cramping pain ➢ Diarrhea, blood and pus in stool Intestinal obstruction ➢ Hyperactive bowel sounds ______________________________________________________________ Intestinal infraction ➢ Absent bowel sounds ➢ Gross or occult blood in stool APPENDICITIS Assessment 1. Nausea, anorexia 2. Initially periumbilical pain 3. Later localizes to McBurney’s point 4. Mild fever, elevated WBC count 5. Abdominal rigidity 6. Rebound tenderness Implementation 1. Maintain bed rest 2. Keep client NPO if surgery is likely 3. Semi-Fowler’s position decreases pain 4. Monitor for signs of perforation and systemic infection Post Operative 1. Monitor vital signs 2. Monitor fluid intake and output 3. Monitor bowel sounds 4. Monitor dressing for drainage or signs of infection DIVERTICULITIS Diverticula - bulging pouches of mucosa through sorrounding muscle Diverticulosis - presence of diverticula Diverticulitis - inflammation of diverticula Assessment 1. Pain in lower left quadrant 2. May be relieved by bowel movement 3. Bowel irregularities 4. Rectal bleeding 5. Mild fever 6. Elevated WBC Diagnosis: 1. Barium enema 2. Sigmoidoscopy 3. Colonoscopy Implementation 1. NPO if peritonitis or massive bleeding 2. Liquid or soft diet during acute phase 3. High fiber and bulk-forming diet after pain subsides 4. Stool softeners 5. Temporary colostomy necessary: perforation, peritonitis or obstruction Post Operative 1. Monitor vital signs 2. Monitor fluid intake and output 3. Watch for bleeding: hemoratic and hemoglobin 4. Watch for signs of infection: pus or foul odor HEMORRHOIDS ➢ Varicosities of anal and rectal veins Predisposing factors ______________________________________________________________ 1. 2. 3. 4. Hereditary Chronic constipation Pregnancy Liver cirrhosis Assessment ➢ Rectal pain and itching ➢ Bleeding (bright red blood on stool) Implementation 1. Warm sitz baths to ease pain and swelling 2. Stool softeners, high fiber diet 3. Avoid straining 4. Surgery: ligation, sclerotherapy or surgical excision Topical Medications 1. Anti-inflammatory: hydrocortisone cream 2. Astringents: witch hazel cream Post Operative 1. Watch for rectal bleeding 2. Good anal hygiene – keep dry INFLAMMATORY BOWEL DISEASE CROHN’S DISEASE(regional enteritis) ➢ Cramping abdominal pain ➢ Fever, anorexia, weight loss Pathology 1. Transmural thickening 2. Granulomas 3. Usually involves ileum 4. Rectum often spared 5. Affects several bowel segments Complications 1. Perianal disease 2. Fistulas 3. Perforation Outcome ➢ Many patients will have disease recurrence a few years after surgery ULCERATIVE COLITIS ➢ Less abdominal pain ➢ More bloody diarrhea Pathology 1. Mucosal ulceration 2. Begins at rectum and progresses 3. Towards ileocecal junction 4. Limited to colon (but involve terminal ileum) Complications 1. Increased risk for colon carcinoma Outcome ➢ Surgery is curative ______________________________________________________________ Note: The cause of Crohn’s disease and ulcerative colitis are unknown. These patients often have additional chronic inflammations such as sacroiliitis, iritis or conjunctivitis. Assessment 1. Abdominal pain and cramping 2. Malaise, weakness 3. Anxiety 4. Chronic diarrhea with blood, pus or mucus 5. Fever , elevated WBC count 6. Weight loss Diagnosis 1. Baruim enema 2. endoscopy with biopsy Implementation 1. Watch for dehydration 2. Monitor stool frequency and consistency 3. Monitor hemoglobin and hematocrit 4. Watch for signs of gastrointestinal obstruction 5. Provide psychological support and counseling Diet 1. Acute phase: bowel rest > NPO > low-residue diet 2. Low-fat diet for steatorrhea 3. Avoid milk (lactose deficiency of chronic diarrhea) Medications 1. Sulfasalazine 2. Steroids 3. Analgesics Surgery ➢ Indicated it perforation, obstruction or cancer develops INTESTINAL OBSTRUCTION MECHANICAL OBSTRUCTION ➢ Due to adhesions, tumors, vovulus (twisting) ➢ Increased bowel sounds PARALYTIC ILEUS ➢ Due to toxins, infections or postoperative ➢ Absent bowel sounds Assessment 1. Nausea 2. Colicky pain 3. Constipation 4. Vomiting (fecal vomiting in severe lower bowel obstruction) Diagnosis 1. abdominal film: intestinal gas 2. endoscopy Implementation 1. Maintain NPO 2. Monitor vital signs 3. Turn client supine to prone (helps passing flatus and relief abdominal pressure) 4. Monitor patency of decompression tube Post Operative ➢ Encourage coughing, turning, deep breathing ______________________________________________________________ ➢ Monitor bowel sounds (return of peristalsis) PERITONITIS ➢ Acute inflammation of peritoneum Bacterial 1. Perforated duodenal ulcer 2. Ruptured appendicitis 3. Volvulus (twisting of bowel , strangulation, obstruction) 4. Abdominal trauma Chemical 1. Pancreatitis 2. Perforated gastric ulcer Note: Mortality dramatically decreased with antibiotics! Assessment 1. Constant, intense, diffuse abdominal pain 2. Nausea 3. Weakness 4. Abdominal rigidity 5. Absent bowel sounds 6. Signs and symptoms of shock 7. Diagnostic paracentesis: cytology, bacterial culture Implementation 1. NPO to reduce peristalsis 2. Monitor vital signs 3. Maintain bed rest 4. Semi-Fowler’s position 5. IV electrolytes and antibiotics are ordered COLORECTAL CANCER ➢ Second most common cancer in US ➢ 5 year mortality about 50% ➢ Early diagnosis significantly improves survival Assessment 1. Vague abdominal discomfort 2. Nausea, loss of appetite 3. Weakness, fatigue 4. Family history of colorectal cancer 5. Ribbon – or pencil – shaped stools 6. Black of tarry stools 7. Anemia 8. Signs of intestinal obstruction Diagnosis 1. sigmoidoscopy, 2. colonoscopy with boipsy 3. CEA blood test to detect recurrence after surgery Implementation 1. Monitor intake and output 2. Monitor consistency and color of stool 3. Prepare client for surgery ______________________________________________________________ COLOSTOMY CARE 1. Remove pouch when 1/3 full 2. Cleanse stoma with soft cloth and water or mild soap 3. Dry skin thoroughly before applying pouch 4. Use skin barrier powder or paste to protect from fecal drainage 5. Irrigaton of stoma - never force catheter 6. Allow client to verbalize feelings about colostomy ______________________________________________________________