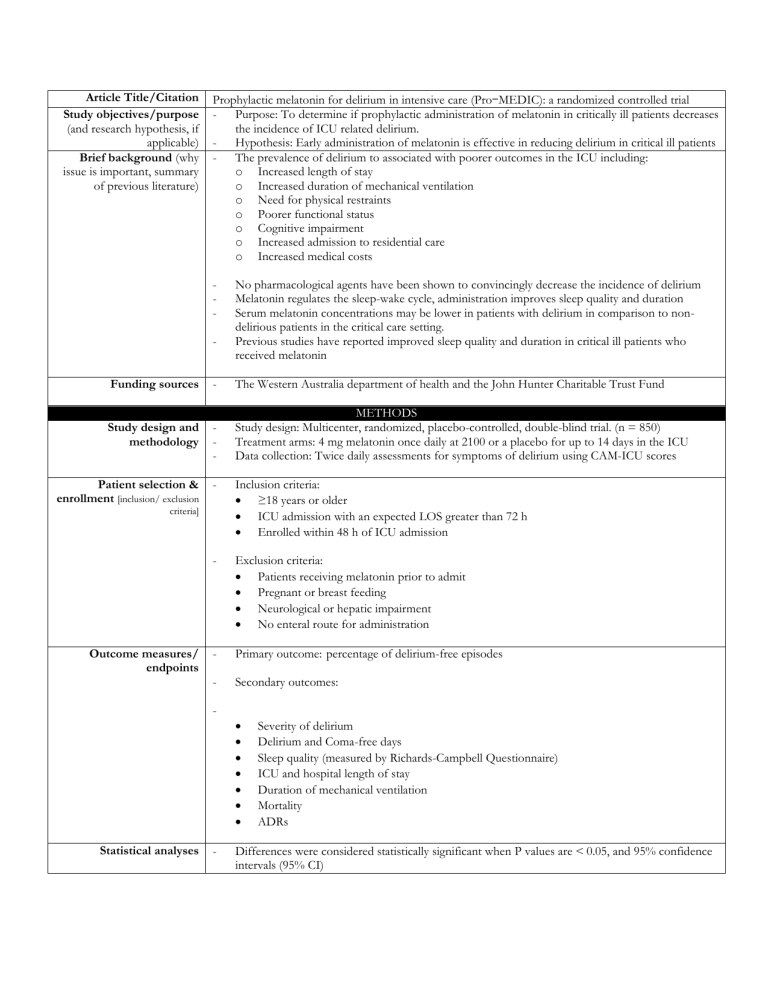
Article Title/Citation Study objectives/purpose (and research hypothesis, if applicable) Brief background (why issue is important, summary of previous literature) Prophylactic melatonin for delirium in intensive care (Pro-MEDIC): a randomized controlled trial - Purpose: To determine if prophylactic administration of melatonin in critically ill patients decreases the incidence of ICU related delirium. - Hypothesis: Early administration of melatonin is effective in reducing delirium in critical ill patients - The prevalence of delirium to associated with poorer outcomes in the ICU including: o Increased length of stay o Increased duration of mechanical ventilation o Need for physical restraints o Poorer functional status o Cognitive impairment o Increased admission to residential care o Increased medical costs - No pharmacological agents have been shown to convincingly decrease the incidence of delirium Melatonin regulates the sleep-wake cycle, administration improves sleep quality and duration Serum melatonin concentrations may be lower in patients with delirium in comparison to nondelirious patients in the critical care setting. Previous studies have reported improved sleep quality and duration in critical ill patients who received melatonin Funding sources - The Western Australia department of health and the John Hunter Charitable Trust Fund Study design and methodology - METHODS Study design: Multicenter, randomized, placebo-controlled, double-blind trial. (n = 850) Treatment arms: 4 mg melatonin once daily at 2100 or a placebo for up to 14 days in the ICU Data collection: Twice daily assessments for symptoms of delirium using CAM-ICU scores Patient selection & enrollment [inclusion/ exclusion - Inclusion criteria: ≥18 years or older ICU admission with an expected LOS greater than 72 h Enrolled within 48 h of ICU admission - Exclusion criteria: Patients receiving melatonin prior to admit Pregnant or breast feeding Neurological or hepatic impairment No enteral route for administration - Primary outcome: percentage of delirium-free episodes - Secondary outcomes: criteria] Outcome measures/ endpoints Statistical analyses - Severity of delirium Delirium and Coma-free days Sleep quality (measured by Richards-Campbell Questionnaire) ICU and hospital length of stay Duration of mechanical ventilation Mortality ADRs Differences were considered statistically significant when P values are < 0.05, and 95% confidence intervals (95% CI) - Enrollment & baseline characteristics Summary of primary and secondary outcomes including subgroup analysis, etc. Be sure to include both efficacy and safety parameters, if appropriate Author’s conclusions - - Study strengths - Study limitations - Applicability and impact on pharmacists/healthcare providers Resident Conclusions and recommendations RESULTS Average age of 62 Male (59.1% vs 66.4% control group) Apache score of 17.3% vs 17.5% CAM positive baseline 9.6% vs 8.3% Admission etiology was mostly Emergency at 81.9% vs 80.1% And their diagnosis type for being in the ICU was respiratory at 27% followed by cardiovascular at 22% No significant difference in the average proportion of delirium-free assessments per patient between the melatonin and placebo groups (79.2 vs 80% respectively, p = 0.547) No significant difference in any secondary outcomes including ICU LOS (median: 5 vs 5 days, p = 0.135), hospital LOS (median: 14 vs 12 days, p = 0.816), mortality at any time point including at 90 days (15.5 vs 15.6% p = 0.948) No significant difference in the requirement of anti-psychotics, sedatives or physical restraints, or in the duration of mechanical ventilation No serious adverse events reported in either group AUTHORS’ DISCUSSION & CONCLUSIONS Short LOS Dose of melatonin may be too low Limited ICU setting Study consistent with critical ill patients having low to non-existent melatonin levels. Using melatonin early and continued throughout the ICU for a maximum of 14 consecutive days did not resulting a reduction in the prevalence of delirium compared to placebo. These findings do not support the routine use melatonin to prevent delirium in the critically ill. RESIDENT’S DISCUSSION & CONCLUSIONS Comparable baseline characteristics between the two groups Included LOS, mortality outcomes, and use of rescue medications GOLD standard study design Adequately powered study, large population, less than expected loss to follow-up resulting in >95% power Subgroup analysis with baseline delirium assessment with a priori groups - Brief summary of authors’ main discussion points Alpha value of 0.05 and a power of 80%, sample size was increased by 15% to account for potential losses to follow-up, incidences of coma, or inability to perform CAM, 850 patients with 425 patients in each arm Poisson regression was used to compare the count of delirium and coma-free days between the treatment groups using an offset of number of days in ICU Hospital mortality was analyzed with Cox proportional hazards models and presented with Kaplan Meyer curves. 17.1% of assessments were missed and around 20% were non-assessable CAM-ICU assessments were not standard in most sites, which could explain some of the missed assessments Dose was on the medium to low range of studied doses CAM scores were checked twice daily, flexibility was allowed in timing and de-sedation was encouraged (nurse managed) Study based in Australia. Melatonin is not effective for prevention of delirium in the ICU so we would not be using it in the ICU for the prevention of delirium. I would not recommend melatonin for preventing delirium in the ICU. Reference: Wibrow B, Martinez FE, Myers E, et al. Prophylactic melatonin for delirium in intensive care (Pro-MEDIC): a randomized controlled trial. Intensive Care Med. 2022;48(4):414425. doi:10.1007/s00134-022-06638-9