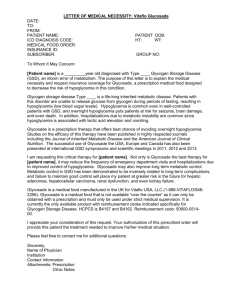
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/8173694 Hypoglycemic Brain Damage Article in Metabolic Brain Disease · January 2005 DOI: 10.1016/j.forsciint.2004.08.001 · Source: PubMed CITATIONS READS 182 3,019 1 author: Roland N Auer University of Saskatchewan 219 PUBLICATIONS 10,197 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Brain Injury View project Missed diagnoses in alleged child abuse View project All content following this page was uploaded by Roland N Auer on 29 October 2018. The user has requested enhancement of the downloaded file. P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) pp1311-mebr-492105 September 17, 2004 3:6 C 2004) Metabolic Brain Disease, Vol. 19, Nos. 3/4, December 2004 ( Hypoglycemic Brain Damage Roland N. Auer1 Received November 26, 2003; accepted December 4, 2004 Hypoglycemia was long considered to kill neurons by depriving them of glucose. We now know that hypoglycemia kills neurons actively rather than by starvation from within. Hypoglycemia only causes neuronal death when the EEG becomes flat. This usually occurs after glucose levels have fallen below 1 mM (18 mg/dL) for some period. At that time abrupt energy failure occurs, the excitatory amino acid aspartate is massively released into the limited brain extracellular space and floods the excitatory amino acid receptors located on neuronal dendrites. Calcium fluxes occur and membrane breaks in the cell lead rapidly to neuronal necrosis. Significant neuronal necrosis occurs after 30 min of electrocerebral silence. Other neurochemical changes include energy depletion to roughly 25% of control, phospholipase and other enzyme activation, tissue alkalosis, and a tendency for all cellular redox systems to shift towards oxidation. Hypoglycemia often differs from ischemia in its neuropathologic distribution, in that necrosis of the dentate gyrus of the hippocampus can occur and a predilection for the superficial layers of the cortex is sometimes seen. Cerebellum and brainstem are universally spared in hypoglycaemic brain damage. Hypoglycemia constitutes a unique metabolic brain insult. Key words: Hypoglycemia; metabolism; brain; necrosis; excitatory amino acids. HISTORICAL ASPECTS OF HYPOGLYCEMIA Manfred Sakel introduced hypoglycemia as a therapy in psychiatry (Sakel, 1933, 1934), published in the English literature in the late 1930s (Sakel, 1937). At that time, insulin was given to people for treatment of schizophrenia and drug addiction. The desired period of coma, after some experience with this procedure, was 30 min, since it was discovered if the patient remained in coma for longer than 30 min coma would be transformed from a “reversible coma” to an “irreversible coma” (Baker, 1938; Fazekas et al., 1951). Our present day understanding of hypoglycaemic brain damage now indicates that this was due to the relatively scant neuronal necrosis that occurs within 30 min, contrasting with widespread virtual decortication that occurs after 60 min of hypoglycaemic coma (Auer et al., 1984a). Over the years, insulin-induced hypoglycemia as a therapy for psychiatric disease or drug addiction fell out of favor. After the Second World War, this treatment was phased out (Mayer-Gross, 1951). It should be noted that prior to the introduction of Sakel’s therapy (and prior to the discovery of insulin in 1921), hypoglycemia must have been seen with islet cell adenoma, the β-cell, insulin-secreting pancreatic tumor (Terbrüggen, 1932). However, hypoglycemia 1 Departments of Pathology and Clinical Neuroscience, University of Calgary, 3330 Hospital Drive N.W., Calgary, Alberta, Canada T2N 4N1. E-mail: rauer@ucalgary.ca 169 C 2004 Plenum Publishing Corporation 0885-7490/04/1200-0169/0 P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) pp1311-mebr-492105 September 17, 2004 3:6 170 Auer was not clearly recognized until it was brought to the fore by the discovery of insulin in 1921, and the ensuing widespread use of insulin in the treatment of diabetes. Today, hypoglycemia is seen in the context of numerous metabolic and medical diseases. But profound hypoglycemia, accompanied by EEG isoelectricity and neuronal necrosis, occurs mainly when insulin or oral hypoglycaemic agents are administered. Hypoglycemia is commonly seen today in situations of medication error, homicide attempt, and suicide attempt (Auer et al., 1989; Kalimo and Olsson, 1980). We begin with a brief review of the electroencephalogram (EEG), since disappearance of brain electrical activity is a necessary prerequisite for hypoglycaemic brain damage. THE EEG IN HYPOGLYCEMIA EEG is important in hypoglycemia because it determines the presence of brain damage. The EEG normally consists of waves in the alpha range of 8–13 Hz (ααaves) and beta range of 13–25 Hz (β waves). Normally, the theta range of 4–8 Hz (θ waves) constitutes a very minor component of the EEG and delta activity in the range of 1–4 Hz (δ waves) is absent. As the blood glucose levels progressively drop in hypoglycemia to the range of 1– 2 mM, θ waves increase and coarse δ waves appear. These are accompanied by clinical stupor or drowsiness (see Table 1). Changes in the brain monoamines dopamine, noradrenaline, and serotonin already occur at this stage (Agardh et al., 1979), probably explaining at least partly, the changes in cerebration that occur in the early, precoma stages of hypoglycemia. Free fatty acids increase over six times (Agardh et al., 1980) due to phospholipid breakdown, and there is inhibition of plasma membrane function and contained ion pumps (Agardh et al., 1982). Metabolically, this also corresponds to progressive carbohydrate depletion in cerebral tissue, until energy failure occurs in a threshold manner when brain glucose has fallen by over 97% (Feise et al., 1976). The cerebellum suffers a lesser metabolic insult (Agardh et al., 1981b; Agardh and Siesjö, 1981), probably due to the greater efficiency of the cerebellar glucose transporter (LaManna and Harik, 1985), explaining the relative resistance of the cerebellum to hypoglycaemic brain damage. As the duration of hypoglycemia increases, coma finally supervenes when the threshold of energy failure is reached. The blood glucose is by now in the range of <1 mM. Over time, this is accompanied electroencephalographically by isoelectricity, a flat EEG in common parlance. The signs and stages of hypoglycemia are outlined in the Table 1. The absolute level of the blood sugar is unimportant once it reaches asymptotic low levels. It is the fact of cerebral EEG isoelectricity that is the harbinger of neuronal necrosis. Table 1. Stages of Hypoglycemia Clinical EEG Blood glucose (mM) Normal Anxiety (adrenergic discharge) Normal ↑amplitude ↓frequency (θ, δ waves) waves Flat >3.5 2–3.5 Stupor Coma, Cushing response (↑ BP) 1–2 <1.36 P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) pp1311-mebr-492105 Brain in Hypoglycemia September 17, 2004 3:6 171 In experimental studies, a flat EEG was in fact seen over one log variation in blood glucose levels, from 1.36 down to 0.12 mM (Auer et al., 1984a). The controlled experimental data thus indicate that hypoglycemia in this range is at risk of producing a flat EEG, which then in turn heralds the onset of necrotizing brain damage. Before we discuss hypoglycaemic neuronal necrosis, however, we will review the altered metabolism that accompanies hypoglycemia, and tease out those aspects of pathological cerebral metabolism that give rise to neuronal death in hypoglycemia. NEUROCHEMISTRY Glycolytic flux through the Embden-Myerhof pathway is obviously decreased in hypoglycaemia, contributing to a decreased cerebral metabolic rate for glucose (CMRgl) (Abdul-Rahman and Siesjö, 1980). Transamination reactions occur, and the aspartate– glutamate transaminase reaction is shifted to the left (Fig. 1). Oxaloacetate increases due to the shortage of acetate with which it condenses to form citrate in the Krebs cycle. It is this primary increase in oxaloacetate that secondarily drives Figure 1. Metabolism in the tricarboxylic acid cycle and Embden-Meyerhof glycolysis. Alterations caused by hypoglycemia are shown with arrows, with the relative thickness of the arrows representing the quantitative flow of metabolites along the pathways. Since oxaloacetate has little acetate to condense with to form citrate, it builds up and by mass action drives the aspartate-glutamate transaminase reaction to the left. P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) 172 pp1311-mebr-492105 September 17, 2004 3:6 Auer Figure 2. Hypoglycemia causes an increase in tissue aspartate and decrease in glutamate, while both amino acids flood the extracellular space of the brain. GABA similarly floods the extracellular space, but its inhibitory effects are often insufficient to prevent hypoglycaemic convulsions in the face of the excitatory amino acids released. Data from Norberg and Siesjö (1976) for whole tissue and extracellular data from Sandberg et al. (1986). this reaction to the left, according to Le Chetalier’s principle (chemical law of mass action). Aspartate in the tissue increases fourfold (Agardh et al., 1978). The increased aspartate spills over from the intracellular to the extracellular space of the brain, where aspartic acid level increase to 1600% of control (Sandberg et al., 1985). Excitatory and inhibitory amino acid changes are shown in Fig. 2. These are the salient neurochemical features of hypoglycaemic brain damage that result in neuronal death. But there are other biochemical alterations that occur, and these are most interesting in that many are the opposite of those that occur in ischemia. One of these is the consistent development of a profound tissue alkalosis. The cause is twofold. Increased ammonia production as the cell catabolizes protein and deaminates amino acids is one cause. Ammonia is a very strong base and its tissue production powerfully drives up cellular pH. The second reason for alkalosis in hypoglycemia is lactate deficiency. The normally acidifying production of lactic acid is mitigated in profound hypoglycemia. Lactate has a pKa of 3.83, and it tends to pull the tissue pH towards its own pKa . Tonic production of lactate is reduced due to the decreased glycolytic flux in hypoglycemia. One morphologic consequence of this is that infarction is impossible in hypoglycemia due to the impossibility of increasing tissue lactate and lowering pH. This, combined with the absence of ischemia explains why selective neuronal necrosis, but not infarction, is seen in hypoglycemia. The above events conspire to increase cellular pH to roughly 7.5 from a normal of 7.3 (Pelligrino and Siesjö, 1981). This hypoglycaemic alkalosis contrasts with the acidosis engendered by brain tissue in ischemia. Energy failure occurs in hypoglycemia, with the energy charge falling abruptly to roughly 25% of normal. Oxidative phosphorylation is decreased and inorganic phosphate is increased (Behar et al., 1985). Adenosine triphosphate (ATP), the chief player in determining the cellular energy state, is reduced, and adenosine monophosphate, is increased. Brain energy metabolism can be sustained not only by consumption of endogenous substrates such as proteins and fatty acids (Agardh et al., 1980), but also through exogenous molecules which still circulate through the blood in hypoglycemia. These include glycerol P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) pp1311-mebr-492105 Brain in Hypoglycemia September 17, 2004 3:6 173 (Sloviter et al., 1966), lactate (McIlwain, 1953), and ketone bodies (β-OH butyrate and acetoacetate). Lactate alone can substitute for roughly 1/4 of glucose use (Nemoto and Hoff, 1974). Oxidation is favored during hypoglycemia, and cellular redox pairs all tilt their reactions toward oxidation in hypoglycemia. Thus, lactate/pyruvate, NAD/NADH, GSG/GSSG, and NADP/NADPH all shift their equilibria toward the oxidized compound of the pair (Agardh et al., 1978). Whether the oxidized cellular state of hypoglycemia leads to oxidative damage to DNA or proteins is still unknown. Hypoglycemic brain damage is characterized by an increase in cerebral blood flow (CBF) (Abdul-Rahman et al., 1980) but interestingly also a relatively upheld cerebral metabolic rate for oxygen (CMRO2 ) (Eisenberg and Seltzer, 1962). To account for upheld CMRO2 with decreased CMRgl the use of endogenous substrates by the brain must be invoked (Agardh et al., 1981a). The use of brain tissue fatty acids and protein catabolic products explain the stoichiometric discrepancy between glucose consumed and CO2 produced during hypoglycemia. It should be noted that the increased CBF is nonspecific, and occurs in many brain insults: the increase in blood pressure represents an attempt by the body to maintain the brain (the Cushing response) in the face of an insult to the brain. NEUROPATHOLOGY Once the EEG goes flat, neuronal necrosis appears over the ensuing minutes as aspartate floods the extracellular space (Sandberg et al., 1986). These necrotic neurons can be stained with any acid histological stain, and the increased affinity for acid dyes will cause them to be acidophilic (Auer et al., 1984b). Since most histologic stains of the brain involve a pink or red acid dye, acidophilic neurons are invariably red in routinely stained tissue sections. A conspicuous feature of hypoglycaemic brain damage in the rat is neuronal necrosis in the dentate gyrus of the hippocampus (Auer et al., 1985). This seems to be due to the proximity of the NMDA receptors of the molecular layer of the dentate to the CSF spaces containing the excitatory amino acid aspartate. One of the mysteries of hypoglycaemic brain damage has been its asymmetry. It seems impossible a priori for a metabolic insult to cause an asymmetric pattern of damage in the brain. However, with the understanding that a flat EEG is necessary for brain damage to occur, and the discovery that this is occasionally asynchronous between the hemispheres (Harris et al., 1984; Wieloch et al., 1984), this is easily explained. If one hemisphere should develop a flat EEG 10 min before the other, then a duration of 20 min of flat EEG for the entire brain would really amount in that case to 30 min for one hemisphere but only 20 min for the other, as assessed by an interhemispheric EEG. There is another practical implication of this besides theoretically explaining hypoglycaemic asymmetry in brain damage. The neuropathologist should never use asymmetry as a criterion favoring either ischemic or hypoglycaemic brain damage over the other, since both can be asymmetric. The early lesion of the neuron is marked electron microscopically by dendritic swelling (Auer et al., 1985). This spares the intervening neuropil. The lesion is the electron microscopic hallmark of an excitotoxin. The reason for this is the selective dendritic location of receptors. Thus, amino acids bind to neuronal dendrites, open ion channels which leads to P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) pp1311-mebr-492105 174 September 17, 2004 3:6 Auer water fluxes, too, across the membrane, leading to swelling of dendrites, sparing intervening axons. Hypoglycemia may be summarized as a novel insult that has a number of features unsuspected several decades ago. These include a positive mechanism of neuronal death, not merely neuronal death by starvation. An often seen asymmetry is explained by the asynchronous onset of electrocerebral silence between the hemispheres. And selective necrosis of the dentate gyrus is not seen in cerebral ischemia, the dentate being the last structure within the hippocampus to be destroyed by ischemia. REFERENCES Abdul-Rahman, A., Agardh, C.-D., and Siesjö, B.K. (1980). Local cerebral blood flow in the rat during severe hypoglycemia and in the recovery period following glucose injection. Acta Physiol. Scand. 109:307– 314. Abdul-Rahman, A., and Siesjö, B.K. (1980). Local cerebral glucose consumption during insulin-induced hypoglycemia, and in the recovery period following glucose administration. Acta Physiol. Scand. 110:149–159. Agardh, C.-D., Carlsson, A., Lindqvist, M., and Siesjö, B.K. (1979). The effect of pronounced hypoglycemia on monoamine metabolism in rat brain. Diabetes 28:804–809. Agardh, C.-D., Chapman, A.G., Nilsson, B., and Siesjö, B.K. (1981a). Endogenous substrates utilized by rat brain in severe insulin-induced hypoglycemia. J. Neurochem. 36:490–500. Agardh, C.D., Chapman, A.G., Pelligrino, D., and Siesjö, B.K. (1982). Influence of severe hypoglycemia on mitochondrial and plasma membrane function in rat brain. J. Neurochem. 38:662–668. Agardh, C.-D., Folbergrová, J., and Siesjö, B.K. (1978). Cerebral metabolic changes in profound insulin-induced hypoglycemia, and in the recovery period following glucose administration. J. Neurochem. 31:1135–1142. Agardh, C.-D., Kalimo, H., Olsson, Y., and Siesjö, B.K. (1981b). Hypoglycemic brain injury: Metabolic and structural findings in rat cerebellar cortex during profound insulin-induced hypoglycemia and in the recovery period following glucose administration. J. Cereb. Blood Flow Metab. 1:71–84. Agardh, C.-D., and Siesjö, B.K. (1981). Hypoglycemic brain injury: Phospholipids, free fatty acids, and cyclic nucleotides in the cerebellum of the rat after 30 and 60 minutes of severe insulin-induced hypoglycemia. J. Cereb. Blood Flow Metab. 1:267–275. Agardh, C.D., Westerberg, E., and Siesjö, B.K. (1980). Severe hypoglycemia leads to accumulation of arachidonic acid in brain tissue. Acta Physiol. Scand. 109:115–116. Auer, R.N., Hugh, J., Cosgrove, E., Curry, B. (1989). Neuropathologic findings in three cases of profound hypoglycemia. Clin. Neuropathol. 8:63–68. Auer, R.N., Kalimo, H., Olsson, Y., and Wieloch, T. (1985). The dentate gyrus in hypoglycemia. Pathology implicating excitotoxin-mediated neuronal necrosis. Acta Neuropathol. (Berl.) 67:279–288. Auer, R.N., Olsson, Y., and Siesjö, B.K. (1984a). Hypoglycemic brain injury in the rat. Correlation of density of brain damage with the EEG isoelectric time: A quantitative study. Diabetes 33:1090–1098. Auer, R.N., Wieloch, T., Olsson, Y., and Siesjö, B.K. (1984b). The distribution of hypoglycemic brain damage. Acta Neuropathol. (Berl.) 64:177–191. Baker, A.B. (1938). Cerebral lesions in hypoglycemia. II. Some possibilities of irrevocable damage from insulin shock. Arch. Pathol. 26:765–776. Behar, K.L., den Hollander, J.A., Petroff, O.A.C., Hetherington, H.P., Prichard, J.W., and Shulman, R.G. (1985). Effect of hypoglycemic encephalopathy upon amino acids, high-energy phosphates, and pHi in the rat brain in vivo: Detection by sequential 1 H and 31 P NMR spectroscopy. J. Neurochem. 44:1045–1055. Eisenberg, S., and Seltzer, H.S. (1962). The cerebral metabolic effects of acutely induced hypoglycemia in human subjects. Metabolism 11:1162–1168. Fazekas, J.F., Alman, R.W., and Parrish, A.E. (1951). Irreversible posthypoglycemic coma. Am. J. Med. Sci. 222:640–643. Feise, G., Kogure, K., Busto, R., Scheinberg, P., and Reinmuth, O. (1976). Effect of insulin hypoglycemia upon cerebral energy metabolism and EEG activity in the rat. Brain Res. 126:263–280. Harris, R.J., Wieloch, T., Symon, L., and Siesjö, B.K. (1984). Cerebral extracellular calcium activity in severe hypoglycemia: Relation to extracellular potassium and energy state. J. Cereb. Blood Flow Metab. 4:187–193. Kalimo, H., and Olsson, Y. (1980). Effect of severe hypoglycemia on the human brain. Acta Neurol. Scand. 62:345–356. LaManna, J.C., and Harik, S.I. (1985). Regional comparisons of brain glucose influx. Brain Res. 326:299–305. P1: KVK mebr2004.cls (04/22/2004 v1.1 LaTeX2e MEBR document class) Brain in Hypoglycemia pp1311-mebr-492105 September 17, 2004 3:6 175 Mayer-Gross, W. (1951). Insulin coma therapy of schizophrenia: Some critical remarks on Dr. Sakel’s report. J. Ment. Sci. 97:132–135. McIlwain, H. (1953). Glucose level, metabolism, and response to electrical impulses in cerebral tissues from man and laboratory animals. Biochem. J. 55:618–624. Nemoto, E.M., and Hoff, J.T. (1974). Lactate uptake and metabolism by brain during hyperlactatemia and hypoglycemia. Stroke 5:48–53. Norberg, K., and Siesjö, B.K. (1976). Oxidative metabolism of the cerebral cortex of the rat in severe insulin induced hypoglycemia. J. Neurochem. 26:345–352. Pelligrino, D., and Siesjö, B.K. (1981). Regulation of extra- and intracellular pH in the brain in severe hypoglycemia. J. Cereb. Blood Flow Metab. 1:85–96. Sakel, M. (1933). Neue Behandlungsart Schizophreniker und verwirrter Erregter. Wien. Klin. Wchnschr. 46:1372– 1373. Sakel, M. (1934). Schizophreniebehandlung mittels Insulin-Hypoglykämie sowie hypoglykämischen Schocks. Wien. Med. Wchnschr. 84:1211. Sakel, M. (1937). The methodical use of hypoglycemia in the treatment of psychoses. Am. J. Psychiatry 94:111– 129. Sandberg, M., Butcher, S.P., and Hagberg, H. (1986). Extracellular overflow of neuroactive amino acids during severe insulin-induced hypoglycemia: In vivo dialysis of the rat hippocampus. J. Neurochem. 47:178–184. Sandberg, M., Nyström, B., and Hamberger, A. (1985). Metabolically derived aspartate—Elevated extracellular levels in vivo in iodoacetate poisoning. J. Neurosci. Res. 13:489–495. Sloviter, H.A., Shimkin, P., and Suhara, K. (1966). Glycerol as a substrate for brain metabolism. Nature 210:1334– 1336. Terbrüggen, A. (1932). Anatomische Befunde bei spontaner Hypoglykämie infolge multipler Pankreasinseladenome. Beitr. z. Path. Anat. u. Allg. Path. 88:37–59. Wieloch, T., Harris, R.J., Symon, L., and Siesjö, B.K. (1984). Influence of severe hypoglycemia on brain extracellular calcium and potassium activities, energy and phospholipid metabolism. J. Neurochem. 43:160–168. View publication stats