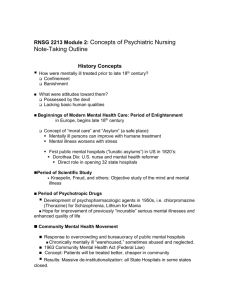
Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 What is mental health? No single definition of mental health exists o Is NOT separate from physical health. o Very Subjective because everyone has different symptoms, and it is different for everyone. Clinical manifestations are different for everyone. o Comprehensive nursing care—holistic nursing Deinstitutionalization o 1963 Deliberate shift from state hospitals to community-based facilities. o Community movement o Income for disabled—social security (SSDI, SSI) o Revolving door effect—take care of symptoms and discharge and send back into community only to have patient come back to facility. Does not have support at home and find support within the facility. Typically, this is the homeless population d/t lack of home, resources, food, income, availability to medications. AKA: Frequent Flyer, their disorder does NOT define them. Reaching staff—NRS follows patient after discharge and ensure they are adhering to their regimen and continue to follow until they are stable within the community. Challenges o Stigma Most wait 10-12 years for depression before seeking treatment. Wait 3-5 years before reaching out for anxiety help. Do not judge anyone when they seek care, avoid stereotypes and making them feel judged. o COST Managed care—designed to control balance between the quality of care provided and the cost of that care. Receive care based on need. Managed care organizations—control expenditure of insurance funds by requiring providers to seek approval before the delivery of care. Case management—case by case basis, represented an effort to provide necessary services while containing cost. Average admits for 3-5 days for inpatient hospitalization for mental health issues. Average cost is 25-30,000 per 3-5 day stay. We fix/stabilize their symptoms. Brief interventions and then sent home. They do not learn how to cope/live with symptoms/diagnosis. o SPECIAL POPULATION Homelessness, psychiatric boarding, arrest, incarceration (75-80% can be diagnosed with at least ONE psych condition), veterans, victimization, suicidality, familial violence, danger to others. o WORK FORCE Not enough NRSG staff available to fully staff psych facilities. Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Current theories and therapy o Combo of chapter 3, 4, & 5 most important topics o Ch 2 NOT on exam!!! Outline o Introduction Freud's psychoanalysis Freud is the father of psychoanalysis Developed theories in late 19th and early 20th centuries Body of knowledge has been used for developing other theories Psycho analytic theory supports the notion that all human behavior is caused and can be explained Personality components (pg 41): ID, Superego, Ego. Id: Reflects basic or innate desires such as pleasure-seeking behavior, aggression, and sexual impulses. ALL ABOUT ME, selfseeking. Has no regard for rules or social convention/norms Superego: Reflects moral and ethical values Behavior is within social expectations. It’s about others, NOT you. Ego: Balancing or mediating force between id and superego. This helps you make sound decisions. AKA: Defense mechanisms Defense Mechanisms (pg 42-43) -help protect our ego so that we are not stressed out or being emotionally vulnerable. o Aggression-behavior o Compensation- overachievement in one area to cover deficiencies in another area. Ex: overachievement in one area to offset real deficiencies in another area. o Conversion- Expression of emotional conflict through development of physical symptom. o Denial- failure to acknowledge unbearable condition; failure to admit the reality of a situation or how one enables the problem to continue. Ex: diabetic person eating chocolate candy. **MOST COMMONLY USED DEFENSE MECHANISM** o Displacement-being angry/upset with someone other than who caused those feelings. Ex: Person who is mad at the boss and yells at their spouse. o Dissociation- Dealing with emotional conflict by temporary alteration in consciousness or identity. o Fixation- Immobilization of portion of the personality resulting from unsuccessful completion of tasks in a developmental stage. o Identification- Modeling actions and opinions of influential others while searching for identity or aspiring to reach a person, social, or occupational goal. o Intellectualization- Separation of emotions of a painful event or situation from the facts involved, acknowledging the facts but not the emotions. o Introjection- Accepting another person’s attitudes, beliefs, and values as one’s own. o Projection- Unconscious blaming of unacceptable inclinations or thoughts on an external object. o Rationalization- Requires intentional thinking to figure out some of the root cause analysis. Ex: Student blames failure on teacher being mean. o Reaction formation-acting opposite of what one thinks/feels. Ex: women who never wanted to have children becomes supermom. Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Regression- Moving back to a previous development stage to feel safer for have needs met. Ex: 5-year-old asks for a bottle when new baby bro is being fed. o Repression- Excluding emotionally painful or anxiety provoking thought and feeling from conscious awareness. Brain automatically does this for you. o Resistance- Overt or convert antagonism toward remembering or processing anxiety-producing information. o Sublimation- Substituting a socially acceptable for an impulse that is unacceptable. o Substitution- Replacing desired gratification with one that is more readily available. o Suppression- Conscious exclusion of unacceptable thoughts and feelings from conscious awareness. Ex: student decides not to think about a parent’s illness to study for a test. o Undoing- Exhibiting acceptable behavior to make up for or negate unacceptable behavior. Erickson stages of development (pg 44-45) Foundation for psychosocial assessment o Infancy stage-birth to 12 months Trust vs Mistrust Want to view world as safe and reliable and nurturing and dependable. Virtue: Hope o Toddler stage-Autonomy vs shame & doubt Achieve sense of control and free will. Give 2 options to pick from. Virtue: Will (sense & freewill) o Preschool stage-Initiative vs guilt. (Shame and doubt) Beginning development of conscience, learning to manage conflict and anxiety Virtue: Purpose o School age-Industry vs inferiority Emerging confidence in own abilities, taking pleasure in accomplishments Virtue: Competence o Adolescence-Identity vs role confusion Formulating sense of self and belonging (act like the ones they want to be like) Virtue: Fidelity o Young adult-Intimacy vs isolation Forming adult, loving, long lasting relationships, and meaningful attachment to others Virtue: Love o Middle adult-Generativity vs stagnation Being creative and productive, establishing next generation Virtue: Care o Maturity-Ego integrity vs despair (regret their choices—depression) Accepting responsibility for oneself and life. Has been through different experiences. Virtue: Wisdom Know interventions and most likely possibly outcome. Will be given scenarios based on stage and determine the best/most appropriate option. Focus mostly on highlighted ones. Milieu (pg 46) Persona’s social environment basically. Involved clients’ interpersonal relationship skills, giving one another feedback about behavior, and working cooperatively as a group to solve day-to-day problems. A person's social environment Developed by Sullivan (1892-1949) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 involved clients’ interactions with one another Practicing interpersonal relationship skills Giving one another feedback about behavior Working cooperatively as a group to solve day today problems Peplau’s Nurse patient relationship (pg 47) o Nurse theorist. Think about today’s class. o Orientation-introduction, expectations, syllabus, assignements. Explained expectations, reviewed suggestions/questions, addressed corrections will be made (orientation phase) o Working phase is working together. Tylenol vs Ibuprofen. 200 vs 500 which would you like. What would you rate your pain at 9/10, give higher dose of medication. o Resoluation-terminate relationship. Understanding of what needs to happen after discharge (why we give discharge summary). Want client educated upon discharge. Maslow’s hierarchy (pg 49) o Physiological needs supersedes psychological needs. Physical needs first then psychological needs o Physiological Needs—food, water, sleep, shelter, sexual expression, freedom from pain. o Safety & Security Needs—include protection, security, freedom from harm or threatened deprivation. o Love & Belonging Needs-intimacy, friendship, acceptance. Empathy vs sympathy o Empathy—understanding. Trying to put yourself in their shoes to understand. (Feeling) o Sympathy—saying I feel bad or sorry for you. “I am here for you; we will figure this out together” Group therapy (pg 54) o 2 different types of groups o Open groups Anyone can walk in. There is NO criteria about anything with this group. Ex: AA meetings. Informal and no specific leader only identified leader. No training or certification needed. No limitations on # of individuals involved in group Sitting in circle facing one another. (No showing back to others in group) o Closed groups Only for certain individuals. They start group at same time and finish the curriculum at the same time (usually 8-12 weeks). Specific appointed leader for the group. Leads the session. MUST be trained for certified to do this type of group. Needs credentials. May require specific time of clothing, hide tattoos, avoid any triggers for anyone else involved in that specific group session. Keep it 5-15 individuals involved. May be like classroom settings. Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Chapter 1 Foundations of psychiatric mental health nursing Mental Health o Difficult to define-neurochemical imbalance. No single, universal definition Many components influenced by factors Dynamic, ever-changing state Influencing factors: o Individual (personal)—Way you were raised, growth & development, age, maturity—age & maturity level should match ideally, support level/system, socioeconomic status, genetics (HUGE), Anxiety is most common diagnosis Kids are concrete thinkers, must be direct and black/white. Neuron pathways developed by age:25. o Interpersonal (relationship)—Intimate zone (spouse, family, parents), work or school relationships (incivility) o Social/cultural (environmental)—Homelessness, sense of community, access to resources, intolerance of violence, support of diversity among people, and mastery of environment. Includes disorders that affect: o Mood o Behavior o Thinking These often indicate signs of distress and/or impaired functioning. General criteria for diagnosis: o Dissatisfaction with characteristics, abilities, accomplishments o Ineffective or unsatisfying relationships o Dissatisfaction with one’s place in the world o Ineffective coping with life events o Lack of personal growth Diagnostic and Statistical Manual of Mental Disorders DSM-5: Taxonomy published by the American Psychiatric Association Purposes: o Standardize nomenclature, language o Identify defining characteristics or symptoms o Assist in identifying underlying causes DSM Classification Allows the practitioner to identify all factors that relate to a patient’s condition: o Major psychiatric disorders o Medical conditions o Psychosocial and environmental problems Question Is the following statement true or false? The definition of mental health is standardized and universally accepted. Answer: False o Rationale: There is no single universal definition of mental health, which has many components and is influenced by myriad factors. Historical Perspectives Ancient times Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Sickness as displeasure of gods; punishment for sins; viewed as demonic or divine o Aristotle and imbalances of the four humors (blood, water, yellow and black bile); balance restoration via bloodletting, starving, and purging o Early Christians’ view as possession by demons Period of enlightenment (1790s) o Creation of asylums; moral treatment o Dorothea Dix Sigmund Freud: scientific study, treatment of mental illness Psychopharmacology (1950s): development of psychotropic drugs Community mental health movement o Deinstitutionalization o Legislation for disability income o Changes in commitment laws Mental Illness and the 21st Century Current state o More than 18.6% of Americans aged 18 years and older have diagnosable mental disorder (NIMH, 2008), 20.7 million have a substance use disorder, and 8.4 million of this population have a dual diagnosis. o 15 million adults and 4 million children and adolescents with impaired daily activities o Economic burden exceeds that of all types of cancer. o Leading cause of disability in the United States and Canada for those 15 to 44 years of age o Increasing number of both adults and children/adolescents are being treated for mental illness; yet only 1 in 4 adults and 1 in 5 children are treated. o Treatment still lagging in homeless and those with substance abuse problems Issues and concerns: o “Revolving-door” effect due to deinstitutionalization Often “boarded” in EDs while awaiting inpatient beds o Shorter hospital stays, decompensation, rehospitalization, dual diagnoses o Homelessness (42% estimated to have serious mental illness associated with substance abuse) o 33% have associated physical illness comorbidities. o Lack of adequate community resources Question: Which statement best reflects the current state of mental health and mental illness? Mental health-care costs exceed the costs for cancer care. Most adults and children receive adequate mental health care. Community resources for the homeless with mental illness are adequate. Deinstitutionalization has reduced the revolving-door effect. Answer: Mental health-care costs exceed the costs for cancer care. o Rationale: The economic burden of mental illness exceeds that for all types of cancer care. o Only 1 in 4 adults and 1 in 5 children receive the necessary mental health care. Community resources for homeless clients with mental illness are inadequate. Deinstitutionalization has led to the “revolving-door” effect. Objectives for the Future Healthy People 2020 objectives: o Increase the number of people identified, diagnosed, treated, helped to live healthier lives o Decrease rates of suicide, homelessness o Increase employment for those with serious mental illness o Provide more services for incarcerated persons with mental health problems Community-Based Care Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Lack of appropriate number of community mental health centers to provide services Development of community support programs o Availability, quality of services highly variable o Inaccurate anticipation of extent of people’s needs o Despite flaws, positive aspects make them preferable for treatment Cost Containment and Managed Care Managed care movement (early 1970s) Development of utilization review firms/managed care organizations (1990s); case management Separation of mental health care from physical care for insurance coverage Cost Containment and Managed Care (cont.) Mental health-care management through privately owned behavioral health-care firms o If no private insurance, reliance on counties of residence for payment HCFA: Medicare, Medicaid Mental health parity, insurance coverage Cultural Considerations Culturally diverse population Cultural differences influencing mental health, treatment of mental illness (see Chapter 7) Changes in family structure Question: Is the following statement true or false? Community-based programs are preferable for treating many people with mental illness. Answer True o Rationale: Although there are flaws in the system, community-based programs have positive aspects that make them preferable for treating many people with mental illness. Psychiatric Nursing Practice Linda Richards: first American psychiatric nurse McLean Hospital, Belmont, MA: site of first training for nurses to work with persons with mental illness Expansion of role with development of somatic therapies Psychiatric Nursing Practice (cont.) First psychiatric nursing textbook (Nursing Mental Diseases) published in 1920 Johns Hopkins: first school of nursing to include psychiatric nursing course (1913) National League for Nursing (1950) requiring schools to include psychiatric nursing experience Psychiatric Nursing Practice (cont.) H. Peplau: therapeutic nurse–client relationship; interpersonal dimension (foundation for current practice) J. Mellow: focus on client’s psychosocial needs, strengths American Nurses Association and Standards of Care Psychiatric–Mental Health Nursing Phenomena of Concern (see Box 1.2) Psychiatric Nursing Practice (cont.) Basic-level functions o Counseling o Milieu therapy o Self-care activities o Psychobiologic interventions o Health teaching o Case management o Health promotion, maintenance Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Advanced-level functions o Psychotherapy o Prescriptive authority for drugs o Consultation, liaison o Evaluation Student Concerns and Psychiatric–Mental Health Clinical Experience Saying the wrong thing Knowing what to do Being rejected or not talking to the student Asking personal questions Handling bizarre, inappropriate, or sexually aggressive behavior Handling feeling unsafe Student Concerns and Psychiatric–Mental Health Clinical Experience (cont.) Seeing someone known on the unit Dealing with similar problems or backgrounds Question: Is the following statement true or false? The National League for Nursing required schools to include a psychiatric nursing experience before the first nursing school included a psychiatric nursing course in its curriculum. Answer False o Rationale: Johns Hopkins was the first school of nursing to include a course in psychiatric nursing in its curriculum; this was done in 1913. It was not until 1950 that the National League for Nursing required schools to include an experience in psychiatric nursing. Self-Awareness Issues Everyone has unique or different values, ideas, and beliefs. Possible conflict between personal values/beliefs, those of client Need to accept differences; view each client as worthwhile regardless of opinions or lifestyle Self-awareness through reflection Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Chapter 2 Neurobiological theories and psychopharmacology Central Nervous System Brain (See Figures 2.1 and 2.2) o Cerebrum o Cerebellum o Brain stem o Limbic system Spinal cord Nerves that control voluntary acts (neurotransmitters) Cerebrum Two hemispheres Four lobes: o Frontal lobe (thought, body movement, memories, emotions, moral behavior) o Parietal lobe (taste, touch, spatial orientation) o Temporal lobe (smell, hearing, memory, emotional expression) o Occipital lobe (language, visual interpretation) Cerebellum Below cerebrum Center for coordination of movements, postural adjustments Reception, integration of information from all body areas to coordinate movement, posture Brain Stem Midbrain: reticular activating system (motor activity, sleep, consciousness, awareness) and extrapyramidal system Pons: primary motor pathway Medulla oblongata: vital centers for cardiac, respiratory function Nuclei for cranial nerves III through XII Locus ceruleus: norepinephrine-producing neurons (stress, anxiety, impulsive behavior) Limbic System Above brain stem o Thalamus (activity, sensation, emotion) o Hypothalamus (temperature regulation, appetite control, endocrine function, sexual drive, impulsive behavior) o Hippocampus (emotional arousal, memory) o Amygdala (emotional arousal, memory) Neurotransmitters Chemical substances to facilitate neurotransmission (see Figure 2.3) Important in right proportions to relay messages (see Figure 2.4) Play role in psychiatric illness and psychotropic medications, including their actions and side effects. Neurotransmitters (cont.) Excitatory or inhibitory (see Table 2.1) o Excitatory Dopamine: complex movements, motivation, cognition, regulation of emotional response Norepinephrine: attention, learning, memory, sleep, wakefulness, mood regulation Epinephrine: flight-or-fight response Glutamate: major neurotoxic effects at high levels Neurotransmitters (cont.) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Excitatory or inhibitory (see Table 2.1) (cont.) o Inhibitory • Serotonin: food intake, sleep, wakefulness, temperature regulation, pain control, sexual behaviors, regulation of emotions GABA: modulation of other neurotransmitters o Excitatory or inhibitory Acetylcholine: sleep-and-wakefulness cycle; signals muscles to become alert Histamine: neuromodulator Question Is the following statement true or false? The cerebellum consists of four lobes. Answer False Rationale: The cerebrum consists of four lobes. The cerebellum is located below the cerebrum. Brain Imaging Techniques Computed tomography (CT) Magnetic resonance imaging (MRI) Positron emission tomography (PET) Single photon emission computed tomography (SPECT) Limitations o Use of radioactive substances; expense of equipment; client’s inability to tolerate technique o Changes nondetectable with current techniques Neurobiologic Causes Genetics and heredity: play role but not solely genetic o Twin, adoption, and family studies are used. Psychoimmunology: compromised immune system possibly contributing, especially in at-risk populations Infections: particularly viruses during fetal development, possibly play role Nurse’s Role in Research and Education Ensure all clients, families are well informed. Help distinguish between facts and hypotheses. Explain if or how new research may affect client’s treatment or prognosis. Question Is the following statement true or false? Single photon emission computed tomography is considered the best type of brain imaging technique to diagnose disease. Answer False Rationale: Single photon emission computed tomography (SPECT) is not considered the major type of brain imaging used to diagnose disease. In fact, many of the changes in the brain are not currently detectable with any of the current techniques. Psychopharmacology Psychotropic drugs Efficacy (maximum therapeutic effect) Potency (amount of drug needed for maximum effect) Half-life Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Approved use Psychopharmacology (cont.) Off-label use (effective for disease different from one involved in original testing) Black box warning (serious or life-threatening side effects) Principles of Psychopharmacology Antipsychotic Drugs Antipsychotic agents—neuroleptics (see Table 2.3) o Conventional (e.g., chlorpromazine, fluphenazine, thioridazine, haloperidol, loxapine) o Second generation (e.g., clozapine, risperidone, olanzapine) o Third generation (dopamine system stabilizers; e.g., aripiprazole) Antipsychotic Drugs (cont.) Use: treatment of psychotic symptoms Mechanism of action: block dopamine receptors Antipsychotics: Side Effects Extrapyramidal syndrome (EPS): o Acute dystonia Torticollis, opisthotonus, oculogyric crisis Treatment: anticholinergic drugs or diphenhydramine (see Table 2.4) o Pseudoparkinsonism (stooped posture, mask-like faces, shuffling gait) o Akathisia (restlessness, anxiety, agitation) Antipsychotics: Side Effects (cont.) Neuroleptic malignant syndrome (NMS) Tardive dyskinesia (irreversible involuntary movements) Anticholinergic effects (dry mouth, constipation, urinary hesitancy or retention) Antipsychotics: Side Effects (cont.) Other side effects: o Increased prolactin levels o Weight gain (second-generation agents, except ziprasidone) o Prolonged QT interval (thioridazine, droperidol, mesoridazine) o Agranulocytosis (clozapine) Antipsychotics: Client Teaching Adherence to regimen Side effects, management o Thirst/dry mouth (sugar-free candy, liquids) o Constipation (dietary fiber, stool softeners) o Sedation (safety measures) Actions for missed dose (dose if within 4 hours of usual time) CBC, ANC with clozapine Question Which of the following drugs would be classified as a conventional antipsychotic? Clozapine Risperidone Fluphenazine Aripiprazole Answer Fluphenazine Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o • Rationale: Fluphenazine is classified as a conventionalantipsychotic. o Clozapine and risperidone are considered second-generation antipsychotics. Aripiprazole is considered a third-generation antipsychotic. Antidepressants Use: major depressive illness, anxiety disorders, depressed phase of bipolar disorder, psychotic depression Antidepressants (cont.) Four groups (see Table 2.5): o Tricyclic and related cycle antidepressants (TCAs) o Selective serotonin reuptake inhibitors (SSRIs) o MAO inhibitors (MAOIs) o Others (venlafaxine, bupropion, duloxetine, trazodone, nefazodone) Antidepressants (cont.) Mechanism of action: interact with monoamine neurotransmitter systems, especially norepinephrine and serotonin Preferred drugs for clients at high risk for suicide Antidepressants: Side Effects SSRIs o Anxiety, agitation, akathisia, nausea, insomnia, sexual dysfunction o Weight gain TCAs o Anticholinergic effects o Orthostatic hypotension, sedation, weight gain, tachycardia o Sexual dysfunction Antidepressants: Side Effects (cont.) MAOIs o Daytime sedation, insomnia, weight gain, dry mouth, orthostatic hypotension, sexual dysfunction o Hypertensive crisis (with foods containing tyramine) Antidepressants: Side Effects (cont.) Other agents o Sedation, headache (nefazodone, trazodone) o Loss of appetite, nausea, agitation, insomnia (bupropion, venlafaxine) o Priapism (trazodone) Antidepressants: Drug Interactions Serotonin syndrome o MAOI + SSRI o Agitation, sweating, fever, tachycardia, hypotension, rigidity, hyperreflexia o Coma, death (extreme reactions) Antidepressants: Client Teaching Time of dosage o SSRI first thing in morning o TCAs at night Actions for missed dose o SSRI up to 8 hours after missed dose o TCAs within 3 hours of missed dose Safety measures Dietary restrictions if taking MAOI (see Box 2.1) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Mood-Stabilizing Drugs Lithium, some anticonvulsants (carbamazepine, valproic acid; gabapentin, topiramate, oxcarbazepine, and lamotrigine) Use: treatment of bipolar disorders Mood-Stabilizing Drugs (cont.) Mechanism of action o Normalize reuptake of certain neurotransmitters (lithium) o Increase levels of GABA (valproic acid, topiramate) o Kindling process (valproic acid, carbamazepine) Mood-Stabilizing Drugs: Side Effects Lithium o Nausea, diarrhea, anorexia, fine hand tremor, polydipsia, polyuria, metallic taste, fatigue, lethargy; weight gain, acne (later in therapy) o Toxicity: severe diarrhea, vomiting, drowsiness, muscle weakness, lack of coordination Carbamazepine and valproic acid: drowsiness, sedation, dry mouth, blurred vision Mood-Stabilizing Drugs: Side Effects (cont.) Carbamazepine: rash, orthostatic hypotension Valproic acid: weight gain, alopecia, hand tremor Topiramate: dizziness, sedation, weight loss Mood-Stabilizing Drugs: Client Teaching Periodic monitoring of blood levels o 12 hours after last dose taken Drug with meals Safety measures Question Is the following statement true or false? A client who takes an SSRI with an MAOI is at risk for a hypertensive crisis. Answer False Rationale: A client who takes an SSRI with an MAOI is at risk for serotonin syndrome. o Hypertensive crisis occurs if the client is taking MAOI and ingests foods containing tyramine. Antianxiety Drugs Use: treatment of anxiety and anxiety disorders, insomnia, OCD, depression, posttraumatic stress disorder, alcohol withdrawal Benzodiazepines, buspirone (see Table 2.6) Mechanism of action o Mediation of GABA (benzodiazepines) o Partial agonist activity at serotonin receptors (buspirone) Antianxiety Drugs: Side Effects Benzodiazepines o Physical, psychological dependence o CNS depression o Hangover effect o Tolerance Buspirone o Dizziness, sedation, nausea, headache Antianxiety Drugs: Client Teaching Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Safety measures Avoidance of alcohol Avoidance of abrupt discontinuation Stimulants Amphetamines (methylphenidate amphetamine, dextroamphetamine) Use: treatment of ADHD in children and adolescents, residual attention-deficit disorder in adults, narcolepsy Stimulants (cont.) Mechanism of action o Cause release of norepinephrine, dopamine, serotonin presynaptically o Direct agonist effects postsynaptically o Block reuptake of neurotransmitters Stimulants: Side Effects and Client Teaching Side effects o Anorexia, weight loss, nausea, irritability o Growth and weight suppression Client teaching o Dose after meals o Avoidance of caffeine, sugar, chocolate o Proper storage out of reach of children Disulfiram Use: aversion therapy for alcoholism Mechanism of action: inhibition of enzyme involved with alcohol metabolism o Adverse reaction with alcohol ingestion Side effects: fatigue, drowsiness, halitosis, tremor, impotence Disulfiram (cont.) Drug interactions with phenytoin, isoniazid, warfarin, barbiturates, long-acting benzodiazepines Client teaching: avoidance of alcohol, including common products that may contain it o Shaving cream, deodorant, OTC cough preparations Question Which of the following drugs would the nurse expect to administer to a client with ADHD? Disulfiram Methylphenidate Buspirone Lithium Answer Methylphenidate Rationale: Methylphenidate is a stimulant used to treat ADHD. o Disulfiram is used to treat alcoholism. Buspirone is used to treat depression. Lithium is used to treat bipolar disorder. Cultural Considerations More rapid response to antipsychotics, TCAs for African Americans than whites o Greater risk of side effects Slower metabolism of antipsychotics, TCAs for Asians o Lower doses to produce the same effects Cultural Considerations (cont.) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Lower doses of antidepressants for Hispanics than whites to achieve desired effects Lower doses of lithium for Asians and African Americans than whites to produce desired effects Cultural Considerations (cont.) Increased frequency of herbal medicine use o St. John’s wort o Kava o Valerian o Ginkgo biloba Increased risk for interactions Common Barriers to Maintaining Medication Management Long-term, chronic illness requires ongoing treatment. Symptoms of poor insight and confusion “Faulty” thinking Major side effects/interactions of meds Stereotyping and discrimination against mental illness Self-Awareness Issues View chronic mental illness as having remissions and exacerbations, just as chronic physical illnesses do. Remain open to new ideas that may lead to future breakthroughs. Understand that medication noncompliance is often part of the illness, not willful misbehavior. Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Chapter 3 Psychosocial theories & therapies Psychosocial Theories Psychoanalytic (Freud) Developmental (Erikson, Piaget) Interpersonal (Sullivan, Peplau) Humanistic (Maslow, Rogers) Behavioral (Pavlov, Skinner) Existential (Beck, Ellis, Frankl, Perls, Glasser) Psychoanalytic Theories: Sigmund Freud All human behavior is caused, explainable Repressed sexual impulses, desires as motivation for behavior Personality components o Id o Ego o Superego Behavior motivation due to subconscious thoughts, feelings o Conscious, preconscious, unconscious o Subconscious Ego defense mechanisms (see Table 3.1) Psychosexual stages of development o Oral o Anal o Phallic/oedipal o Latency o Genital (see Table 3.2) Transference, countertransference Current Psychoanalytic Practice Psychoanalysis o Focus on discovering causes of patient’s unconscious, repressed thoughts, feelings, conflicts related to anxiety o Free association, dream analysis, behavior interpretation used to gain insight into and resolve these conflicts, anxieties Lengthy, expensive, practiced on limited basis today Freud’s defense mechanisms still current Question: Is the following statement true or false? Freud identified three stages of psychosexual development. Answer: False o Rationale: Freud identified five stages of psychosexual development: oral, anal, phallic/oedipal, latency, and genital. Developmental Theories Erik Erikson o Eight stages of psychosocial development (see Table 3.3) o Achievement of life’s virtues Jean Piaget o Cognitive, intellectual development o Four stages: sensorimotor, preoperational, concrete operations, formal operations Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Interpersonal Theories: Sullivan Five life stages: infancy, childhood, juvenile, preadolescence, adolescence (see Table 3.4) Three developmental cognitive modes o Prototaxic (infancy, childhood) o Parataxic (early childhood) o Syntaxic (school-aged children; more predominant in preadolescence) Significance of interpersonal relationships Therapeutic milieu or community Interpersonal Theories: Peplau Therapeutic nurse–patient relationship Four phases: orientation, identification, exploitation, resolution (see Table 3.5) Nurse’s roles to meet patient’s needs: stranger, resource person, teacher, leader, surrogate, counselor Four levels of anxiety: mild, moderate, severe, panic (see Table 3.6) Humanistic Theories Abraham Maslow o Hierarchy of needs o Basic physiologic, safety and security, love and belonging, esteem, self-actualization Carl Rogers o Client-centered therapy (focus on client’s role) o Unconditional positive regard, genuineness, empathetic understanding Behavioral Theories Behaviorism: focus on behaviors and behavior changes, not how mind works Ivan Pavlov: classical conditioning B. F. Skinner: operant conditioning o All behavior learned o Behavior with consequences (reward or punishment) o Recurrence of rewarded behavior o Positive reinforcement: increased frequency of behavior o Removal of negative reinforcers: increased frequency of behavior o Continuous reinforcement: fastest way to increase behavior; random intermittent reinforcement increasing behavior more slowly but with a longer-lasting effect Treatment modalities: behavior modification, token economy, systematic desensitization Question: Is the following statement true or false? Abraham Maslow was the first theorist to focus on the client’s role. Answer: False o Rationale: Carl Rogers was the first to focus on the client’s role in his client-centered therapy. Existential Theories Overall belief: deviations occur when person is out of touch with self or environment o Goal: to return person to authentic sense of self Cognitive therapy o Focus on immediate thought processing o Use by most existential therapists Rational emotive therapy (Albert Ellis) o 11 “irrational beliefs” leading to unhappiness o “Automatic thoughts”; use of ABC technique Logotherapy (Viktor Frankl): life with meaning; therapy as search for that meaning Gestalt therapy (Frederick “Fritz” Perls) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Emphasis on self-awareness o Identification of thoughts, feelings in the here and now Reality therapy (William Glasser) o Focus on person’s behavior and how that behavior keeps a person from achieving life goals Crisis Intervention Four stages of crisis o Exposure to stressor o Increased anxiety when usual coping ineffective o Increased efforts to cope o Disequilibrium, significant distress Categories of crises o Maturational o Situational o Adventitious Crisis Intervention (cont.) Duration: usually 4 to 6 weeks Outcome: resolution to functioning at precrisis level, higher level, or lower level Crisis intervention techniques o Directive interventions: assess health status, promote problem solving o Supportive interventions: deal with person’s needs for empathetic understanding Question Which of the following includes the concept of automatic thoughts? Cognitive therapy Rational emotive therapy Logotherapy Gestalt therapy Answer B. Rational emotive therapy Rationale: Rational emotive therapy focuses on 11 irrational beliefs and automatic thoughts. o Cognitive therapy focuses on immediate through processing. Logotherapy involves therapy as a search for life with meaning. Gestalt therapy emphasizes self-awareness. Cultural Considerations Major psychosocial theorists were o White o Born in Europe or United States o Seldom treated outside their cultural populations Assumptions of normal or typical may not apply equally well to different racial, ethnic, or cultural backgrounds. Treatment Modalities Community mental health treatment (primary mode of treatment) o Clients continue to work and are able to stay connected with family, friends, and other support systems. o Personality or behavior patterns gradually develop; unable to be changed in a relatively short inpatient course of treatment o Peer counseling, advocacy, and mentoring are showing positive results. Treatment Modalities (cont.) Hospital (inpatient) treatment (often last mode of treatment) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Indications: severe depression/suicidal; severe psychosis; alcohol or drug withdrawal; behaviors requiring close supervision in a safe, supportive environment Individual Psychotherapy Bringing about change in a person by exploring his or her feelings, attitudes, thinking, behavior One-to-one relationship between the therapist and the patient o Progression through stages o Relationship as key to success Therapist’s theoretical beliefs strongly influence style of therapy Groups and Group Therapy Therapist or leader and group of clients sharing common purpose Members contribute to group with expectations of benefiting from it. Stages of group development: o Pregroup stage o Beginning or initial stage o Working stage o Termination Groups and Group Therapy (cont.) Group leadership o Formal leader usually for therapy groups and education groups; informal leader usually for support groups and self-help groups o Focus on group process, group content to be effective Groups and Group Therapy (cont.) Group roles o Growth producing: information seeker, opinion seeker, information giver, energizer, coordinator, harmonizer, encourager, elaborator o Growth inhibiting: monopolizer, aggressor, dominator, critic, recognition seeker, passive follower Groups and Group Therapy (cont.) Therapeutic results (Yalom, 1995): o New information or learning, inspiration or hope o Interaction with others o Feelings of acceptance, belonging o Awareness of not being alone; others share same problems o Insight into problems, behaviors, and effects on others o Altruism Types of Therapy Groups Psychotherapy groups Family therapy Family education Education groups Support groups Self-help groups Question Is the following statement true or false? Self-help groups tend to have an informal or no definitive leader. Answer True Rationale: Support groups and self-help groups tend to have an informal leader or no leader at all. Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Therapy and education groups typically have a formal leader. Complementary and Alternative Therapies Alternative medical systems (homeopathy, traditional Chinese medicine) Mind–body interventions (meditation, art, music therapy) Biologically based therapies (herbs, foods, vitamins) Complementary and Alternative Therapies (cont.) Manipulative and body-based therapies (therapeutic massage, chiropractic manipulation) Energy therapies (therapeutic touch, qi gong, pulsed fields, magnetic fields) Psychiatric Rehabilitation Services to patients with persistent, severe mental illness in the community Also known as community support services or programs Focus on patient’s strengths Activities involving medication management, transportation, shopping, food preparation, hygiene, finances, social support, vocational referral Psychosocial Interventions Nursing activities that enhance patient’s social and psychological functioning and promote social skills, interpersonal relationships, communication Skills used in mental health, other practice areas Self-Awareness Issues No one theory or treatment approach is effective for all patients. Using a variety of psychosocial approaches increases nurse’s effectiveness. Patient’s feelings, perceptions most influential in determining his or her response Current theories and therapy Outline Introduction Freud's psychoanalysis Defense Mechanisms Erickson stages of development Milieu Peplau’s Nurse patient relationship Maslows hierarchy Group therapy Defense mechanism What is Milieu? A person's social environment Developed by Sullivan ( 1892-1949) involved clients interactions with one another Practicing interpersonal relationship skills Giving one another feedback about behavior Working cooperatively as a group to solve day today problems Groups Reference Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Chapter 4 Treatments settings & therapeutic programs Treatment Settings Inpatient hospital treatment o Rapid assessment, stabilization of symptoms, discharge planning Client-centered multidisciplinary approach to brief stay o Short inpatient stays Treatment Settings (cont.) Inpatient hospital treatment o Long-stay clients (severe, persistent mental illness requiring acute care services) o Case management o Discharge planning Partial hospitalization programs o Day treatment programs o Eight broad categories of goals (see Box 4.1) Treatment Settings (cont.) Residential settings o Vary in structure, level of supervision, services provided Group homes Supervised apartments Board, care homes Adult foster care Crisis resolution/respite care Treatment Settings (cont.) Residential settings (cont.) o Evolving consumer household Group-living situation Residents make transition from group home to residence where they fulfill own responsibilities and function without onsite supervision. Transitional care o Peer support o Bridging staff Question Is the following statement true or false? Board and care homes are an example of a partial hospitalization program. Answer False Rationale: A board and care home is an example of a residential treatment setting. o A day treatment program is an example of a partial hospitalization program. Psychiatric Rehabilitation and Recovery Programs Services to promote recovery process (see Box 4.3) o Emphasis on recovery, going beyond symptom control and medication management; includes personal growth o Reintegration into community o Empowerment, increased independence o Improved quality of life Psychiatric Rehabilitation Programs (cont.) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Clubhouse model o Four guaranteed rights of members A place to come to Meaningful work Meaningful relationships A place to return to (lifetime membership) o Physician–client relationship as key o Focus on health, not illness Psychiatric Rehabilitation Programs (cont.) Assertive community treatment (ACT) o One of the most effective approaches (see Box 4.5) o Problem-solving orientation No problem is too small o Direct provision of service rather than referral o Services intense; no time constraints Psychiatric Recovery Programs Recovery goes beyond symptom control and medication management Includes personal growth, reintegration into the community, empowerment, increased independence, and improved quality of life as the beginning of the recovery process. Higher-level goals and expectations characterize later stages of recovery (see Box 4.4). Creates and manages the change this requires, both for individual staff and throughout the organization. Question Is the following statement true or false? In the clubhouse model, the relationship between clients is most important. Answer False Rationale: With the clubhouse model, the physician–client relationship is the most important. Special Populations: Homeless Mentally Ill In comparison to homeless, not mentally ill: o Spend more time in jail o Are homeless longer o Spend more time in shelters o Have less family contact o Face greater barriers to employment PATH program ACCESS demonstration project Special Populations: Prisoners The rate of mental illness among the incarcerated is 5 times higher than the general population. Factors for placement in criminal justice system o Deinstitutionalization o More rigid criteria for civil commitment o Lack of adequate community support o Economization of treatment for mental illness o Attitudes of police, society Special Populations: Prisoners (cont.) Criminalization of mental illness Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Barriers to successful community reintegration o Poverty o Homelessness o Substance use o Violence o Victimization, rape, trauma o Self-harm Special Populations: Active Military and Veterans The prevalence of PTSD and major depression is greater than their civilian counterparts. Increased rates of: o Suicide o Homicide o Injury o Physical illness o Sleep disorders o Substance abuse o Marital and family dysfunction Special Populations: Active Military and Veterans (cont.) Reluctance to seek treatment Treatment may not be readily available Stigmatizing Sexual traumas widespread for both males and females Interdisciplinary Team Pharmacist (see Box 4.6) Psychiatrist Psychologist Psychiatric nurse Psychiatric social worker Occupational therapist Recreation therapist Vocational rehabilitation specialist Interdisciplinary Team (cont.) Core skills o Interpersonal skills (tolerance, patience) o Humanity (warmth, acceptance, empathy) o Knowledge base o Communication skills o Personal qualities (consistency, assertiveness, problem solving) o Teamwork skills o Risk assessment, risk management Question Which of the following disciplines most likely would be included as part of the interdisciplinary team? Physician’s assistant Physical therapist Pharmacist Dietician Answer Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Pharmacist Rationale: The pharmacist would be a member of the interdisciplinary team when medication, management of side effects, and/or interactions with nonpsychiatric medications are complex. o A physician’s assistant, physical therapist, and dietician are not typically involved as members of the psychiatric interdisciplinary team. Psychosocial Nursing in Public Health and Home Care Primary prevention: stress management education Secondary prevention: early identification of mental health problems Tertiary prevention: monitoring, coordinating psychiatric rehabilitation services Clinical practice issues such as substance abuse, domestic violence, child abuse, grief, depression, and many others Self-Awareness Issues Evolution of care away from inpatient settings into community Nontraditional settings such as jails or homeless shelters Empowering clients to make their own decisions Frustration of working with clients having persistent and severe mental illness Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Chapter 5 Therapeutic Relationships Therapeutic Relationship Components of Therapeutic Relationship Trust o Behaviors such as caring, interest, understanding, consistency, honesty, promise keeping, listening (see Box 5.1) o Congruence is essential. Genuine interest o Self-comfort, self-awareness of strengths and limitations, clear focus Components of Therapeutic Relationship (cont.) Empathy o Putting oneself in client’s shoes Client and nurse giving “gift of self” o Different from sympathy (feelings of concern or compassion; focus shifting to nurse’s feelings) Acceptance (no judgments; set boundaries) Positive regard (unconditional nonjudgmental attitude) Self-Awareness Know self o Values (sense of right and wrong, code of conduct for living) Values clarification Choosing Prizing Acting o Beliefs o Attitudes (see Boxes 5.2 and 5.3) Question Is the following statement true or false? A nurse displays empathy by showing feelings of concern and compassion. Answer False Rationale: Empathy is putting oneself into the client’s shoes. o Sympathy is showing feelings of concern and compassion. Therapeutic Use of Self Use of aspects of personality, experience, values, feelings, intelligence, needs, coping skills, perceptions to establish relationships beneficial to clients o Concept developed by H. Peplau Therapeutic Use of Self (cont.) Johari window: tool to learn about oneself o 4 quadrants: open/public self; blind/unaware self; hidden/private self; unknown o Goal: move qualities from quadrants 2, 3, 4 into quadrant 1 Therapeutic Use of Self (cont.) Patterns of Knowing Ways of observing, understanding client interactions Four patterns (Carper, 1978; see Table 5.1) o Empirical (derived from nursing science) o Personal (from life experiences) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Ethical (from moral nursing knowledge) o Aesthetic (from art of nursing) Patterns of Knowing (cont.) Fifth pattern : unknowing (Munhall, 1993) o Nurse admits lack of knowledge of client or understanding of client’s subjective world Types of Relationships Social o Purpose of friendship, socialization, companionship, or task accomplishment o Superficial communication; shifting roles; outcomes rarely assessed Intimate o Emotional commitment of two persons o Individual needs met; assistance with helping each other meet needs Types of Relationships (cont.) Therapeutic o Focus on needs, experiences, feelings, ideas of client only o Use of communication skills, personal strengths, understanding of human behavior by nurse o Joint agreement on areas to work on; outcome evaluation Question Is the following statement true or false? A social relationship involves superficial communication for the purposes of friendship or task accomplishment. Answer True Rationale: A social relationship occurs for friendship, socialization, companionship, or task achievement. It involves superficial communication with shifting roles. Establishing a Therapeutic Relationship Peplau’s model of three phases o Orientation o Working o Termination (see Table 5.3) Overlapping, interlocking of phases Establishing a Therapeutic Relationship: Orientation Phase Meeting nurse, client Establishment of roles Discussion of purposes, parameters of future meetings Clarification of expectations Identification of client’s problems Nurse–client contracts/confidentiality, duty to warn/self-disclosure Establishing a Therapeutic Relationship: Working Phase Problem identification: issues or concerns identified by client; examination of client’s feelings and responses Exploitation: examination of feelings and responses; development of better coping skills, more positive self-image, behavior change, independence Possible transference/countertransference Establishing a Therapeutic Relationship: Termination Phase Begins when client’s problems are resolved Ends when relationship is ended Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Deals with feelings of anger or abandonment that may occur; client may feel termination as impending loss. Behaviors Diminishing Therapeutic Relationships Inappropriate boundaries (relationship becomes social or intimate) Feelings of sympathy, encouraging client dependency Nonacceptance of client, avoidance (see Box 5.4) Question During the working phase of a nurse–client relationship, which of the following would occur? Expectations are clarified. Nurse–client contracts are established. Feelings of loss are addressed. Client’s feelings are examined. Answer Client’s feelings are examined. Rationale: During the working phase, the client identifies issues or concerns and his or her feelings and responses are examined. o Expectations are clarified and contracts are established during the orientation phase. Feelings of loss are addressed during the termination phase. Therapeutic Roles of the Nurse in a Relationship Teacher (coping, problem solving, medication regimen, community resources) Caregiver (therapeutic relationship, physical care) Advocate (ensuring privacy and dignity, informed consent, access to services, safety from abuse and exploitation) Parent surrogate (see Box 5.5) Self-Awareness Issues Nurse’s self-awareness: crucial to developing therapeutic relationships Helpful activities: values clarification, journaling, group discussions, reading Development of self-awareness: continual, ongoing process Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Chapter 6 Therapeutic Communication Communication Exchange of information Verbal o Content: literal words spoken o Context: environment, circumstances, situation in which communication occurs Nonverbal o Process: all messages used to give meaning, context to message o Congruent or incongruent message Therapeutic Communication Interpersonal interactions; focus on patient’s needs Need for privacy Encompasses goals that facilitate the nursing process Needed to effectively meet the standards of client care Therapeutic Communication (cont.) Goals of therapeutic communication o Establish therapeutic relationship o Identify patient’s most important concerns; assess patient’s perceptions o Facilitate patient’s expression of emotions o Teach patient, family necessary self-care skills o Recognize patient’s needs; implement interventions to address patient’s needs o Guide patient toward acceptable solutions Therapeutic Communication (cont.) Respect for boundaries o Distance zones Intimate (0 to 18 inches) Personal (18 to 36 inches) Social (4 to 12 feet) Public (12 to 25 feet) o Therapeutic communication: most comfortable when nurse and patient are 3 to 6 feet apart Therapeutic Communication (cont.) Touch o Five types: functional/professional; social–polite; friendship–warmth; love–intimacy; sexual– arousal o Comforting and supportive; also possible invasion of intimate and personal space o The nurse must evaluate use of touch based on the client’s preferences, history, and needs. For example, clients with a history of abuse Question Is the following statement true or false? A distance of 2 feet between the nurse and patient is adequate for promoting comfortable therapeutic communication. Answer False Rationale: For effective therapeutic communication, a distance of 3 to 6 feet between the nurse and patient would be most appropriate. Therapeutic Communication (cont.) Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Active listening (concentrating exclusively on what patient says) Active observation (watching nonverbal actions as speaker communicates) o Recognize the most important issue o Know what questions to ask o Use of therapeutic communication techniques o Prevents jumping to conclusions o Objectively respond to message Verbal Communication Skills Need for concrete, not abstract, messages Techniques (see Table 6.1) o Exploring, focusing, restating, reflecting promotes discussion of feelings or concerns in more depth o Other techniques useful in focusing or clarifying what is being said o Feedback via making an observation or presenting reality Verbal Communication Skills (cont.) Avoidance of nontherapeutic techniques (see Table 6.2) o Advising, belittling, challenging, probing, reassuring Interpretation of signals or cues o Overt o Covert (themes, metaphors, proverbs, clichés) Nonverbal Communication Skills Facial expression o Expressive o Impassive o Confusing Body language o Open body position o Closed body position Nonverbal Communication Skills (cont.) Vocal cues Eye contact Silence Question Is the following statement true or false? Nonverbal communication is often less accurate than verbal communication. Answer False Nonverbal communication is often more accurate than verbal communication when the two are incongruent. People can readily change what they say, but are less likely to be able to control nonverbal communication. Understanding Meaning, Context, and Spirituality of Communication Meaning: usually more meaning than just spoken word Context o Validation with client of verbal, nonverbal information o Who, what, when, how, why Understanding Meaning, Context, and Spirituality of Communication (cont.) Spirituality Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 o Self-awareness of own spiritual beliefs o Need for objectivity and nonjudgmental attitude about patient’s beliefs Cultural Considerations Need for awareness of cultural differences o Speech patterns, habits o Styles of speech, expression o Eye contact o Touch o Concept of time o Health, health care Question Which of the following would be a nontherapeutic communication technique? Reassuring Reflecting Focusing Exploring Answer Reassuring Rationale: Reassuring is a nontherapeutic technique because it attempts to dispel the patient’s feelings. o Reflecting, focusing, and exploring are examples of therapeutic communication techniques. Therapeutic Communication Session Goals o Establishing rapport o Identifying issues of concern o Being empathetic, genuine, caring, unconditionally accepting of the person o Understanding patient’s perception o Exploring patient’s thoughts, feelings o Developing problem-solving skills o Promoting patient’s evaluation of solutions Therapeutic Communication Session (cont.) Initiation of session o Introduction o Establishment of contract for relationship o Identification of major concern Nondirective role (broad-opening, open-ended questions) Directive role (direct yes/no questions; usually for patients with suicidal thoughts, in crisis, or who are out of touch with reality) Therapeutic Communication Session (cont.) Proper phrasing of questions o Clarification o Identification of patient’s avoidance of anxiety-producing topic Guidance in problem-solving, empowerment to change Assertive Communication Expression of positive and negative feelings/ideas in open, honest, direct way o Calm, specific factual statements o Focus on “I” statements Mental Health Exam 1 Outline Ch 1, 2, 3, 4, 5, 6 & ATI Ch 3, 7, 8, 9 Possible responses o Aggressive o Passive–aggressive o Passive o Assertive Community-Based Care Nurses increasingly caring for high-risk patients in homes; families becoming more responsible for primary prevention Therapeutic communication techniques and skills are essential for caring for patients in the community. Increased self-awareness, knowledge needed about cultural differences; sensitivity to beliefs, behaviors, feelings of others Collaboration with patient and family as well as other health-care providers Question Is the following statement true or false? Assertive communication focuses on identifying negative feelings. Answer False Rationale: Assertive communication focuses on the expression of positive and negative feelings or ideas in an open, honest, direct manner. Self-Awareness Issues Nonverbal communication: as important as verbal Therapeutic communication influential in effectiveness of interventions Awareness of own communication is first step in improving communication o Ask for feedback from colleagues o Examine own communication skills