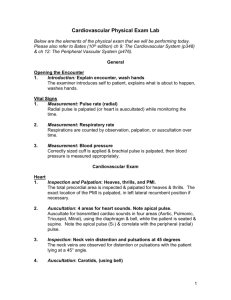
306 Final Script Atmosphere “Good afternoon, my name is Angela. I am going to be your nurse today. Can I please get you’re your name and date of birth? Today, we are going to be conducting a general physical assessment. The information I will be obtaining will be put into your electronic health record which can only be accessed by your healthcare provider and you. Before I begin, I want to ensure safety of the environment and privacy by pulling the curtains. Do you feel safe? Great. Also, before I begin, I am going to perform hand hygiene.” Quick General Survey 3 subjective questions “What brings you in today?” “Any recent pain?” “Have you had any changes in your weight?” “At this point, I would ask the patient to walk 10 feet away and back to her start point. I would note that gait is smooth and rhythmic. I am noting that her posture is upright, normal. I am also noting that the patient’s dressing, grooming, and hygiene are appropriate to the setting as well. I am noting that the patient appears well-developed in relation to nutritional status.” “Can you tell me what today’s date is? And where we are? Great.” “The patient appears conscious, alert and oriented, and her facial expression, mood, and affect is neutral and appropriate to the setting.” “Upon the general survey, there are no abnormal findings to note for this patient.” 3 findings in older adult impaired gait redistribution of body fat wide stance, shuffling feet Neuro and Musculoskeletal (equipment: penlight) 3 subjective questions o “Do you have any pain in your joints or muscles? o “Any limited ROM?” o “Any numbness or tingling in any part of your body?” “I am going to shine this light in your eye on each side, just please look off in the distance while I do this. Both pupils constrict directly and indirectly.” o PERRLA patient’s pupils appear equal, round, react to light, and accommodate.” o “Now, I am going to have you focus on this pen as I pull it closer to your eyes. Both eyes converge and constrict which is normal.” Next, we are going to do your musculoskeletal assessment. o o “I am going to assess muscle tone and strength with bilateral hand grasps. Please squeeze my fingers. Muscle tone and strength of upper extremities appear to be equal bilaterally, and normal Next, we will do the plantar flexion test. o “Can you extend your legs and push against my hands with your feet like a gas pedal, please? Point toes to the sky” Muscle tone and strength are normal and equal in both lower extremities upon bilateral plantar flexion.” 3 findings in older adults for neuro and musculoskeletal o limited ROM o decrease strength o kyphosis Respiratory “Next we will I will assess your respiratory system” 3 subjective questions o “Do have any difficulty breathing?” o “Any pain?” o “History of asthma?” “Respiration appears easy, even, and unlabored.” “I’m going to auscultate your anterior chest wall using 10 landmarks.” “Normally this would be done under the clothing, but for the sake of school, it is done on top of the shirt” o “Breathe normally as I’m doing this” “I’m now going to auscultate the posterior chest wall.” (18 landmarks) “Upon auscultation, there are no abnormal findings to note in this patient.” 3 older adult findings: o decreased tidal volume o decreased chest expansion o decreased gas exchange Cardiac “Next I will assess your cardiac system” 3 subjective questions o “Any chest pains?” o “Swelling in the extremities?” o “Do you tire easily?” Auscultate Apical Pulse & Respiration o I’m going to auscultate the apical pulse which is in your 5th intercostal space, midclavicular line for 60 seconds. Just breathe normally. o extra 30 seconds for respiratory rate State apical pulse & Respiratory rate Perform auscultation of 5 landmarks of heart with diaphragm o Next, I will assess your 5 cardiac points o I’m going to start at your 2nd intercostal space, the right sternum border where your aortic pulse is. o 2nd intercostal space left sternal border pulmonic valve o 3rd intercostal space left sternal border for your Erb’s point o 4th intercostal space left sternal border for your tricuspid valve o 5th intercostal, midclavicular line for mitral valve “Now I’m going to flip this around and use my bell to do the same 5 points.” “Heart sounds appear normal, there are no abnormal findings to note” 3 older adult findings o dysrhythmias o increased systolic blood pressure o orthostatic hypertension Peripheral Vascular “Now I’m going to assess your peripheral vascular system.” 3 subjective questions for peripheral vascular o “Any swelling?” o “Any skin changes or discolorations” o “Any leg pain or cramps?” “Upon looking at your upper extremities I can see that they are of normal color for your ethnicity, your temperature is warm and normal. There is no excess moisture, which is normal. “ “Now I am going to assess capillary refill of both hands. Color returns under two seconds which is normal.” “Now I will assess the presence of a radial pulse. It is present and normal in both arms.” “I am also checking for edema in the lower extremities, noting there is no pitting which is normal.” “Upon inspection, I am noting the presence of normal and even color throughout the lower extremities. I am going to assess temperature and note warmth to the touch as well. Moisture on the lower extremities is normal. There is absence of varicosities in both legs. Capillary refill is normal, less than 2 seconds” o Dorsalis pedis pulse, posterior tibial pulses. Bilaterally equal, normal. 3 older adult findings o hair loss in lower extremities o presence of varicose veins in lower extremities o weaker pedal pulse GI “Last assessment we will do is your Gastrointestinal system.” 3 subjective questions o “Any stomach pains?” o “Changes in your eating habits?” o “Last bowel movement?” “Can you lie down on the bed now.” “Upon inspection of the abdomen, I am noting for smooth, even, and symmetrical contour.” Perform auscultation of abdomen (moving in a clockwise direction I will begin in the RLQ, RUQ, LUQ, LLQ) o “There is presence of normal bowel sounds” Perform percussion using ring finger and middle finger of non-dominant hand on abdomen, and striking with same fingers of dominant hand (RLQ, RUQ, LUQ, LLQ) o “There is normal-pitched hallow sounds upon percussion” “At this point I would assess skin turgor by lightly pinching the skin, noting the absence of tenting, indicating adequate hydration.” Perform palpation in RLQ, RUQ, LUQ, LLQ (“please tell to stop if you feel any pain”) o “There are no lumps or hernias to note.” Upon assessment of abdomen, there are no abnormal findings to note.” 3 older adult findings o Increased Sub Q around stomach and hips o constipation o decreased sense of taste Conclusion “That concludes the physical assessment for today. You can get up and sit in your seat. I will document the absence of abnormal findings in your electronic health record. Do you have any questions for me?”