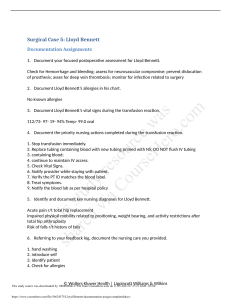
Surgical Case 5: Lloyd Bennett Documentation Assignments 1. Document your focused postoperative assessment for Lloyd Bennett. VS were as follows: BP- 106/68, HR-95, RR-17, T-99F, O2-95% on RA. Patient had normal heart sounds and lungs sounds were clear to auscultation. Respirations were even and normal with no distress noted. IV was patent with no redness or swelling. Patient’s dressing was dry and intact. Patient is A&Ox4. 2. Document Lloyd Bennett’s allergies in his chart. No known allergies. 3. Document Lloyd Bennett’s vital signs during the transfusion reaction. BP- 114/74, HR-94, RR-19, T-99F, O2-94% on RA 4. Document the priority nursing actions completed during the transfusion reaction. Priority is to stop the infusion. Check vital signs and monitor patient. Inform the provider and perform the new orders that were put in (urine culture and venous blood sample). Administer normal saline. Communicate situation with blood bank. Continue to manage symptoms and monitor the patient. 5. Identify and document key nursing diagnoses for Lloyd Bennett. Impaired physical mobility r/t recent surgery, frequent fatigue, and difficulty with changing positions Risk for falls d/t recent surgery Risk for skin breakdown d/t lack of mobility 6. Referring to your feedback log, document the nursing care you provided. I started by verifying my patient, allergies, signed consent, and blood type. I then got an initial set of vitals, all of which were WNL. I then auscultated the patient’s heart and lungs. I then began the administration of the packed RBCs, but the patient began to have a transfusion reaction. I immediately stopped the transfusion. I then notified the provider. I began going through the orders the provider put in following the reaction including a urine culture, calling the blood bank, and beginning an infusion of normal saline at 100ml/hr. I then got another set of vital signs. I also performed patient education. © Wolters Kluwer Health | Lippincott Williams & Wilkins