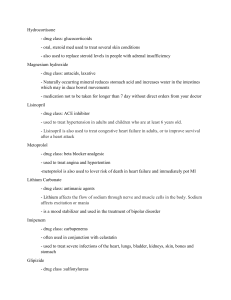
Case Reflection By: Thanuja, Nora, Ju Yu, and Imaad Overview Presenting Complaint Investigations Management Reflection Case Vignette 12 year-old girl presented with generalised abdominal pain and vomiting. History taken on 25/1/2022 Any differentials? History Of Presenting Complaint (HOPC) ● ● ● Abdominal pain and vomiting happened at night around 8.30pm Vomited ○ 12 times. ○ Mainly food content. ○ No blood/bile. (She ate at 4.30, started vomiting around 8.30) Abdominal Pain ○ Generalized ○ Continuous ○ Pain scale 9/10 ○ Nothing worsened/relieved the symptoms ○ Felt burning sensation but it reduces after each vomiting episode HOPC ● Next day did not go to school. Straight to clinic. Was given antiemetics, pain relievers and ORS ● Condition deteriorated further later that day. Started experiencing dyspnoea, dizziness, palpitations. Urine output decreased. ● No diarrhea and said mouth was not dry ● Father brought her to hospital kluang ED. She was immediately warded on that day. ● Blood tests taken. Child has high glucose and acidosis ● First day of admission, glucose reading was 24.8mmol (as of 23/1/2022) ● Further questioning, mom admitted polydipsia and polyuria since December Birth History :● ● ● ● 2.9kg Full term baby born at 38 weeks Vaginal delivery with labour induction Admitted to NICU for 2 days for Jaundice Immunization History :● Up to date. Completed COVID-19 vaccines. Diet History :● ● ● ● ● ● Mom said child used to be a picky eater and had to give appetite stimulating vitamins (started around 4 years old and stopped it when she turned 7) Generally eats home cooked food Prefers to eat rice based foods Admits to snacking a lot as parents are in the vending machine business Loves canned drinks Has the freedom to buy whatever she likes in school canteen Social History :● ● ● ● ● Total 5 people at home . She lives with both parents and her two younger sisters Father works in the vending machine business Mother is a housewife Household income is roughly RM8000 per month. No financial difficulties. At school, she is able to cope with studies. Interacts with teachers fine. Generally talks to her classmates but does not have any close/best friends. Mom says she has a shy personality. Past Medical History :● ● Was previously admitted at hospital Kluang when she was 1 years old for swallowing a coin. Was given liquid paraffin and passed the coin through faeces No surgical Hx Drug History :- NIL/NKDA Family History :- Mom has HTN. Maternal grandfather has T2DM. ICE : NIL Systemic Enquiry: NIL Diagnosis: Diabetic Ketoacidosis (DKA) Currently Weight : 31kg Height : 145cm 3rd day on ward. (Day of clerking 25/1/2022) ● ● ● ● On insulin actrapid On fluids 10% NaCl/dextrose +KCl Fasted for 3 days. Started eating a little on day of clerking Glucose reading on day of clerking 6.8mmol Follow up next day (26/1/2022) ● ● ● ● ● ● Followed ward round Consultant decided to start child on subcutaneous insulin (Insulatard if not mistaken) He was stopping her fluids. Just on KCl twice daily on that specific day Pharmacist was instructed to explain insulin regimens to mom and child (Counselling) Dietician was scheduled to meet mom and child on that day to discuss meal plans (Carbo-counting) Child appears less weak and pale on this day Examination General Inspection : She looked weak and slightly pale. Was on fluids and IV insulin. Continuous BP monitoring and catheter was inserted Vitals :BP 114/85 HR:80 RR:14, warm peripheries, no cyanosis Cardiovascular: Dual Rhythm No Murmur (DRNM) Respiratory: Vesicular breathing. No added breath sounds Neurological : (Ideally should have done) Abdominal : Soft Abdomen, No pitting edema Investigation Blood ● ● ● ● ● FBC U’s & E’s Blood Glucose Blood Ketones HBA1c for monitoring Others ● Strict Fluid Input/Output Chart Management ● Biological ○ ○ ○ ● Psychological ○ ● Insulin ■ 1 long acting dose + 1 short acting dose Fluids (Normal Saline +KCl) Diet Control ■ Regular Meal Timings Referral to therapeutic counselling to ease patient anxiety and worries avout their condition Social ○ Informing school about diagnosis and procedures involved in cases of emergencies (i.e, hypoglycaemia episode) REFLECTION Dose Reduction ● Aimed due to the hormonal imbalances that occur during puberty ○ ○ ● High insulin levels -> more testosterone from ovaries -> more facial hair and acne High insulin levels -> lower sex hormone binding globulins -> oestrogen excess -> heavy menses, fibroids May cause variability in blood sugar readings Other considerations when Prescribing 1. Psychosocial ○ ○ ○ ○ Age - Patient is 12 years old and therefore, attends school. i. She might not want to take medication at school in front of her peers How does this condition affect her mental and physical state Cost of medication Drug interactions 2. Patient counselling and check knowledge ○ ○ The doctor understood what the patient was experiencing and adjusted the dosage to suit her Good patient understanding improves compliance and patient-doctor relationship 3. Patient’s ability to live a normal life Counselling ● Provides opportunity to assess ○ ○ ○ ● Patient Understanding Laying out the procedures and intricacies involved Clarifying patient and caretaker’s ideas, concerns and expectations in regards to the management Allows information about support groups and other MDT members to achieve optimal control of patient symptoms Thank You for Listening