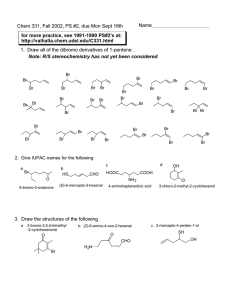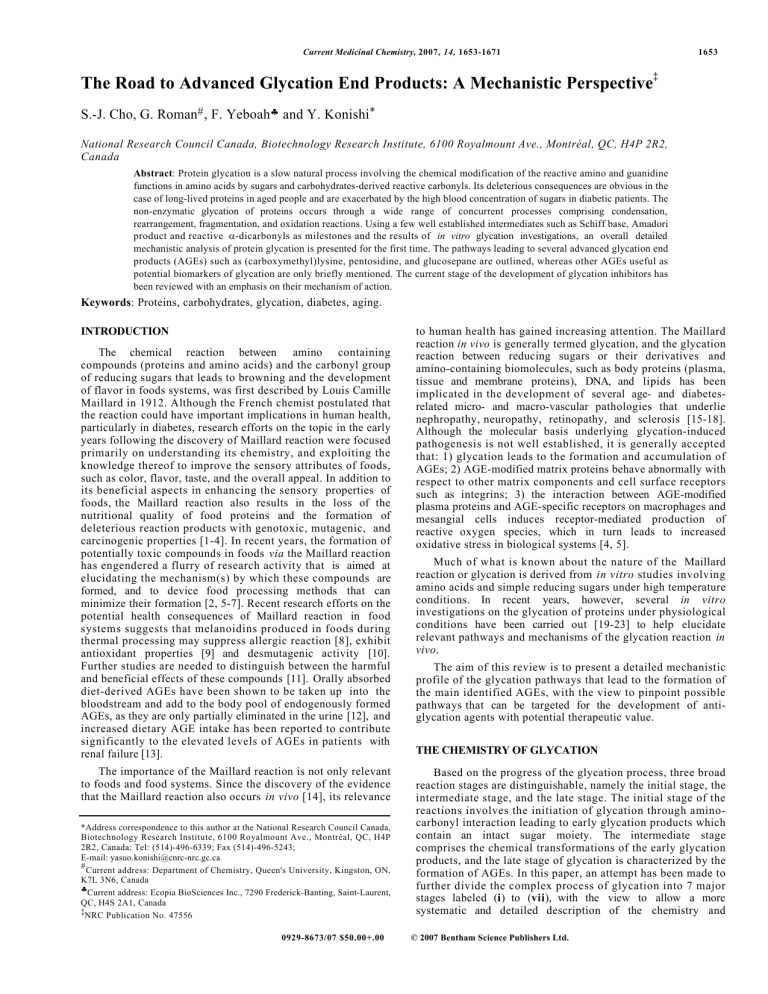
Current Medicinal Chemistry, 2007, 14, 1653-1671 The Road to Advanced Glycation End Products: A Mechanistic Perspective 1653 ‡ S.-J. Cho, G. Roman# , F. Yeboah♣ and Y. Konishi* National Research Council Canada, Biotechnology Research Institute, 6100 Royalmount Ave., Montréal, QC, H4P 2R2, Canada Abstract: Protein glycation is a slow natural process involving the chemical modification of the reactive amino and guanidine functions in amino acids by sugars and carbohydrates-derived reactive carbonyls. Its deleterious consequences are obvious in the case of long-lived proteins in aged people and are exacerbated by the high blood concentration of sugars in diabetic patients. The non-enzymatic glycation of proteins occurs through a wide range of concurrent processes comprising condensation, rearrangement, fragmentation, and oxidation reactions. Using a few well established intermediates such as Schiff base, Amadori product and reactive α-dicarbonyls as milestones and the results of in vitro glycation investigations, an overall detailed mechanistic analysis of protein glycation is presented for the first time. The pathways leading to several advanced glycation end products (AGEs) such as (carboxymethyl)lysine, pentosidine, and glucosepane are outlined, whereas other AGEs useful as potential biomarkers of glycation are only briefly mentioned. The current stage of the development of glycation inhibitors has been reviewed with an emphasis on their mechanism of action. Keywords: Proteins, carbohydrates, glycation, diabetes, aging. INTRODUCTION The chemical reaction between amino containing compounds (proteins and amino acids) and the carbonyl group of reducing sugars that leads to browning and the development of flavor in foods systems, was first described by Louis Camille Maillard in 1912. Although the French chemist postulated that the reaction could have important implications in human health, particularly in diabetes, research efforts on the topic in the early years following the discovery of Maillard reaction were focused primarily on understanding its chemistry, and exploiting the knowledge thereof to improve the sensory attributes of foods, such as color, flavor, taste, and the overall appeal. In addition to its beneficial aspects in enhancing the sensory properties of foods, the Maillard reaction also results in the loss of the nutritional quality of food proteins and the formation of deleterious reaction products with genotoxic, mutagenic, and carcinogenic properties [1-4]. In recent years, the formation of potentially toxic compounds in foods via the Maillard reaction has engendered a flurry of research activity that is aimed at elucidating the mechanism(s) by which these compounds are formed, and to device food processing methods that can minimize their formation [2, 5-7]. Recent research efforts on the potential health consequences of Maillard reaction in food systems suggests that melanoidins produced in foods during thermal processing may suppress allergic reaction [8], exhibit antioxidant properties [9] and desmutagenic activity [10]. Further studies are needed to distinguish between the harmful and beneficial effects of these compounds [11]. Orally absorbed diet-derived AGEs have been shown to be taken up into the bloodstream and add to the body pool of endogenously formed AGEs, as they are only partially eliminated in the urine [12], and increased dietary AGE intake has been reported to contribute significantly to the elevated levels of AGEs in patients with renal failure [13]. The importance of the Maillard reaction is not only relevant to foods and food systems. Since the discovery of the evidence that the Maillard reaction also occurs in vivo [14], its relevance *Address correspondence to this author at the National Research Council Canada, Biotechnology Research Institute, 6100 Royalmount Ave., Montréal, QC, H4P 2R2, Canada; Tel: (514)-496-6339; Fax (514)-496-5243; E-mail: yasuo.konishi@cnrc-nrc.gc.ca # Current address: Department of Chemistry, Queen's University, Kingston, ON, K7L 3N6, Canada ♣Current address: Ecopia BioSciences Inc., 7290 Frederick-Banting, Saint-Laurent, QC, H4S 2A1, Canada ‡NRC Publication No. 47556 0929-8673/07 $50.00+.00 to human health has gained increasing attention. The Maillard reaction in vivo is generally termed glycation, and the glycation reaction between reducing sugars or their derivatives and amino-containing biomolecules, such as body proteins (plasma, tissue and membrane proteins), DNA, and lipids has been implicated in the development of several age- and diabetesrelated micro- and macro-vascular pathologies that underlie nephropathy, neuropathy, retinopathy, and sclerosis [15-18]. Although the molecular basis underlying glycation-induced pathogenesis is not well established, it is generally accepted that: 1) glycation leads to the formation and accumulation of AGEs; 2) AGE-modified matrix proteins behave abnormally with respect to other matrix components and cell surface receptors such as integrins; 3) the interaction between AGE-modified plasma proteins and AGE-specific receptors on macrophages and mesangial cells induces receptor-mediated production of reactive oxygen species, which in turn leads to increased oxidative stress in biological systems [4, 5]. Much of what is known about the nature of the Maillard reaction or glycation is derived from in vitro studies involving amino acids and simple reducing sugars under high temperature conditions. In recent years, however, several in vitro investigations on the glycation of proteins under physiological conditions have been carried out [19-23] to help elucidate relevant pathways and mechanisms of the glycation reaction in vivo. The aim of this review is to present a detailed mechanistic profile of the glycation pathways that lead to the formation of the main identified AGEs, with the view to pinpoint possible pathways that can be targeted for the development of antiglycation agents with potential therapeutic value. THE CHEMISTRY OF GLYCATION Based on the progress of the glycation process, three broad reaction stages are distinguishable, namely the initial stage, the intermediate stage, and the late stage. The initial stage of the reactions involves the initiation of glycation through aminocarbonyl interaction leading to early glycation products which contain an intact sugar moiety. The intermediate stage comprises the chemical transformations of the early glycation products, and the late stage of glycation is characterized by the formation of AGEs. In this paper, an attempt has been made to further divide the complex process of glycation into 7 major stages labeled (i) to (vii), with the view to allow a more systematic and detailed description of the chemistry and © 2007 Bentham Science Publishers Ltd. 1654 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 Cho et al. mechanism(s) of the reaction. The first stage (i) refers to the condensation of a terminal amino group of a protein and the carbonyl group of the acyclic form of a reducing carbohydrate to form a Schiff base, which then undergoes Amadori rearrangement to form an Amadori product. Stage (ii ) deals with non-oxidative and oxidative cleavage reactions of Amadori products, leading to several identifiable AGEs. Stage (iii) involves Schiff base degradation through the Namiki pathway to produce glyoxal and glyoxal-protein adducts, the latter being subsequently converted into two specific AGEs, Nε(carboxymethyl)lysine (CML) and pentosidine, by a route that circumvents Amadori rearrangement. Stage (iv ) reactions feature autoxidative glycosylation, which describes the formation of glyoxal and a novel carbohydrate having a carbon chain one atom shorter than the initial sugar. Stage (v) reactions describe the formation of pentosidine from the Schiff base derived from arabinose generated in stage (iv ). Stage (vi ) deals with the formation of several α-dicarbonyls through the autoxidation of glucose. The production of α-dicarbonyls triggers stage (vii), which describes the formation of a large array of AGEs different from CML and pentosidine and mainly including proteinprotein crosslinks. The overall illustration of these stages occurring during protein glycation is summarized in Scheme (1). The Maillard reaction requires the existence of a primary amino group in the structure of an organic compound (a protein in the specific case of the in vivo glycation) to be reacted with the carbonyl group of a reducing sugar. Several simple ω-amino acids have been shown to react swiftly with glucose to produce in a direct manner the expected Amadori products [24]. The initiation of the glycation process depends primarily on the nucleophilicity of the amino group. In the case of proteins, glycation takes place preferentially at a ω-amino group of the amino acids sequenced in the protein, and at the α-amino group of the amino-terminal residue of the proteins. Although the ε- amino group of lysine bears primary importance with respect to its reactivity in the formation of Amadori products and AGEs, the relevance of hydroxylysine residues in the collagens should not be underestimated [25]. Furthermore, a recent paper has disclosed the formation of ornithine residues from arginine on the protein backbone in substantial quantities during aging of collagen and lens crystallins, which subsequently contributes to the formation of AGEs through glycation and glycoxidation with age [26]. Although a recent paper reports an equal distribution of the glycation sites in a certain protein [27], proofs for the existence of preferential sites of glycation in a protein have been recurrently reported [28-33]. All reducing carbohydrates can potentially be involved in the Maillard reaction, and pentoses such as arabinose or ribose, as well as hexoses such as glucose, fructose, or galactose, and even disaccharides as lactose or maltose have been encountered in studies related to protein glycation. The physiologically relevant D-glucose is one of the least reactive of the common sugars in protein glycation, a reason possibly leading to its evolutionary selection as the main free sugar in vivo [34]. On the other hand, D-ribose is the sugar counterpart in most of the in vitro studies of protein glycation. In spite of the fact that its levels in humans are not elevated, D-ribose is preferred for in vitro experiments because it is known to be more reactive in the Maillard reaction than D-glucose, probably due to a higher fraction of the more reactive acyclic form [35-37]. Formation of Schiff Base and its Amadori Rearrangement (Stage i) The glycation reaction starts with the nucleophilic attack of the nitrogen atom of a primary amino group of a lysine residue at the carbonyl group of a reducing sugar such as glucose (1) to form the hemiaminal (2), which spontaneously dehydrates to give the Schiff base (3), as depicted in Scheme (2). Generally, the glucose Lys-NH2 (i) (vi) (iii) glyoxal-Lys adduct Schiff base (i) (ii), (iv) α-dicarbonyls 1,2-enaminol (iv) (i) (iii) Amadori product ara binose (vii) (ii) (v) CML, pentosidine Scheme 1. -dicarbonyl-de rived AGEs Reaction Mechanisms in the Formation of AGEs Current Medicinal Chemistry, 2007 Vol. 14, No. 15 formation of Schiff base is reversible, and both addition and elimination reaction rates are maximized at slightly acidic pH. With aromatic aldehydes, the equilibrium is shifted in favor of Schiff base formation, but aliphatic aldehydes that possess a hydrogen atom on the carbon adjacent to the carbonyl group do not generally yield Schiff bases [38]. In the case of reducing sugars, the intermediate Schiff base can undergo rapid cyclization to form the N-substituted glycosylamine (4) [39], which is unstable in aqueous medium and can either undergo hydrolysis to yield the starting substrates, or undergoes Amadori rearrangement to produce the relatively stable 1amino-1-deoxy-D-fructose (7), also known as Amadori product. Amadori rearrangement normally involves an acid-catalyzed ring opening of glycosylamine (4) to give the iminium ion (5). The iminium ion then undergoes deprotonation to form the enaminol (6), which upon tautomerism produces the Amadori product (7). Amadori rearrangement can also be catalyzed by transition metal ions, via the same mechanism as protons. The empty d orbitals of transition metal ions readily accept a pair of electrons to form transition-state complexes with compounds containing electron-donating groups [40]. Consequently, examples of Lewis acid-catalyzed Amadori rearrangement have also been reported [41-43], in which the transition metal ions are more efficient than protons, as they are usually polyvalent and can form multiple bonds to the substrate. With regards to the cyclic glycosylamine (4), metal ions such as Fe 2+ , Fe 3+ , or Cu 2+ accelerate the formation of the reactive acyclic iminium ion (5), thus increasing the reaction rate of the Amadori rearrangement. Non-Oxidative and Oxidative Degradation of Amadori Products (Stage ii) Amadori products are fairly stable, but with time and under appropriate conditions they can either decompose to form AGEs or undergo a reverse reaction to the starting substrates (sugars and the free amines) [21]. The degradation of Amadori products may occur both under non-oxidative and oxidative conditions. At pH 7.4 and 37°C, the reversal of Amadori product to the starting substrates accounts for more than 90% of its degradation under non-oxidative conditions [21]. In the pH range of 4-7, the transformation of the sugar moiety of Amadori products into α-dicarbonyl compounds, including 1HC O HO CH NH 1655 deoxyglucose (1-DG) (9), 3-deoxyglucosone (3-DG) (10 ), and 1amino-1,4-dideoxy-2,3-oxo-glucosone (11 ) is a major degradative pathway [44]. As shown in Scheme (3), the enediol (8) derived from Amadori product (7) undergoes a lysine residue elimination to give 1-DG, whereas 3-DG is a result of the lysine moiety removal from the enaminol (6) [45]. Further degradation of 3-DG via a retro-aldol reaction generates methylglyoxal (12 ) and glyceraldehyde (13 ) [46]. Presumably, the acid-catalyzed dehydration of enediol (8) leads to 1-amino-1,4-dideoxy-2,3oxo-glucosone (11 ), whose formation in vivo is still uncertain, as this compound has not been isolated and characterized. One of the major consequences of protein-bound dicarbonyl moieties is the formation of inter- and intra-protein cross-links, a process responsible for many age and diabetes related health complications. To the best of our knowledge, no cross-linked AGEs derived from 1-DG have yet been reported. 3-DG has long been considered as the major α-dicarbonyl intermediate derived from the non-oxidative degradation of Amadori products. 3-DG rapidly reacts with protein amino groups to form AGEs such as CML (14 ) or representative cross-links, such as imidazolone (15 ), pyrraline (16 ), and pentosidine (17 ) presented in Fig. (1) [47]. However, in a recent study, Biemel et al. have showed that the hitherto unknown 1-amino-1,4-dideoxy-5,6-oxo-glucosone (19 ) is the major α-dicarbonyl intermediate generated when glucose was incubated with Boc-lysine, as shown in Scheme (4) [48]. Starting from Amadori product (7), the migration of the 2,3-enediol function in enediol (8) to the 5,6 position as a result of successive β-elimination reactions and the final dehydration at C4 of the 1-amino-5,6-enediol (18 ) leads to 1-amino-1,4dideoxy-5,6-oxo-glucosone (19 ), which is the key intermediate in the formation of glucosepane (21 ). Glucosepane is an acid labile lysine-glucose-arginine crosslink that has identified in in vitro bovine serum albumin (BSA)-glucose incubation mixtures [49], in human serum albumin and lens proteins [50], and in senescent human cellular matrix [51]. The intramolecular condensation between the amino group and the terminal aldehyde function in 1-amino-1,4-dideoxy-5,6-oxo-glucosone (19 ) affords the seven-membered ring compound (20 ), which yields the bicyclic heterocycle upon further condensation with arginine and ring closure [52]. This mechanism is not well established, as it is only based on the identification of (19 ) from which all four diastereoisomers of glucosepane (21 ) could result in model incubation mixtures [48]. Because the stage at which Lys HC N Lys OH H C OH H C OH HO C H HO C H H C OH H C H C OH H C Lys-NH2 H C OH HO C H OH H C OH OH H C OH –H2 O CH2 OH CH2 OH CH2 OH 1 2 3 O HO HO NHLys OH 4 H+ or Mn+ H2 C C NH HO C H H C OH H C L ys O OH HC NH C OH HO C H H C OH H C OH Lys –H+ HC NH H C OH HO C H H C OH H C OH CH2 OH CH2 OH CH2OH 7 6 5 Scheme 2. Lys OH H O HO HO NHLys OH 1656 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 Cho et al. H2C NH C OH C OH H C+ H C Lys H2C - H+ OH Lys H2C NH O C O C OH C O H C H C CH2 OH NH C Lys CH2 OH H C CH2 OH OH CH2 OH 11 + H+ H2 C NH C H2 C NH C OH O HO C H H C OH H Lys C 2,3-e noliza tion H OH + H2 O H C OH C OH C L ys H - H2 N Lys H OH CH2 OH CH2 OH 7 8 CH3 CH2 H OH C O C O C O C OH C OH HC OH C C H OH CH2OH CH2 OH 9 1,2-enolization HC NH C OH HO C H H C OH H C OH Lys + H+ - H2 O HC NH C OH C H H C OH H C OH CH 2OH Lys + H2 O - H2N - H+ O HC O C O CH3 12 retro-aldol H C OH H C OH CH2 OH O C CH2 Lys HC HC H C CH2 OH 6 O OH CH2 OH 10 13 Scheme 3. the guanidine function is introduced in the reaction it is still unclear, the same authors proposed another hypothetical course of reaction, in which the closure of the five-membered ring occurs first [49]. The aldimine (22 ) could be derived from Amadori product (7) by water elimination from its enaminol tautomer (6). The reaction of (22 ) with the guanidine function of an arginine side chain affords the deoxyglucosone-derived imidazoline cross-link DOGDIC (23 ), which upon dehydration and prototropic rearrangement leads to glucosepane (21 ), as presented in Scheme (5). The rationale for this pathway relies on the similarity of this sequence to that proposed for the formation of imidazolinone derivatives [53, 54] and on the isolation of DOGDIC distereoisomers from a model incubation mixture [52]. However, the absence of glucosepane (21 ) in the 3COOH O NH NH H2 C (CH2 )4 H2 N CO OH The oxidative cleavage of Amadori product has been proposed as a major pathway for CML formation [55, 56]. CML is one of the central AGEs and it is used as a biomarker for CO OH N CH2 deoxyosone incubation mixtures, including those with BSA, definitely rules out DOGDIC (23 ) as a precursor for glucosepane and invalidates this pathway [52]. Despite its structural homology with pentosidine (17 ), glucosepane (21 ) is unique amongst AGEs because it is primarily formed under nonoxidative conditions. As for 1-amino-1,4-dideoxy-2,3-oxoglucosone (11 ), although its formation has not been confirmed experimentally, this α-dicarbonyl compound is considered as a primary intermediate in the formation of CML (14 ) in vivo through the oxidative cleavage of the C2-C3 carbon-carbon bond of 1-amino-1,4-dideoxy-2,3-oxo-glucosone. N (CH2 )3 N NH 2 HOH2 C 14 CHO N N H (H2 C) 3 (CH2 )4 CHO H HOOC CHO H H2N COOH CH2 OH Fig. (1). HN 15 16 N (CH2) 4 NH2 H2N 17 COOH Reaction Mechanisms in the Formation of AGEs H2 C NH Current Medicinal Chemistry, 2007 Vol. 14, No. 15 Lys H2 C NH C OH C O HO C H HO C H C OH H C OH H C OH H C OH CH 2OH CH2OH 7 8 Lys N HO O H2 C NH H C OH HO C H Lys HO NH C OH HO C H Lys H C OH OH C H CH C H CH HC C H HO O HO OH OH HC OH CH2 OH NH C NH C C C O H2 C H OH H2 C C L ys C H CH2 - H2 O H 2C H Lys - H2 O H2 C NH C OH HO C H H C OH C OH HC OH O 19 20 Lys OH H OH 1657 L ys 18 HN - H2O NH H2 N Arg Lys L ys N N HN NH HO N HO Arg - H+ Lys H N N NH HO N HO N NH HO N Arg HO Arg H 21 Scheme 4. oxidative stress and long-term protein damage in normal aging and diabetes. It can be derived from a combination of glycation and oxidation reactions [25, 57]. Although the oxidative degradation of Amadori product accounts for its formation during protein glycation, CML can be produced through several other pathways such as Schiff base degradation through the Namiki pathway [58, 59], the “autoxidative glycosylation” comprising the reaction between lysine and glyoxal [58, 60, 61], the reaction between lysine and ascorbate [62], or the metalcatalyzed oxidation of polyunsaturated fatty acids in the presence of proteins [63]. Attempts to establish the relative contribution of each of these pathways to the generation of CML have so far been unconvincing and even contradictory. The conclusion that the oxidative cleavage of Amadori product is responsible for most of the CML produced is based on the observation that aminoguanidine, a compound known to trap glyoxal, only partially inhibited the formation of CML in vitro, indicating that the contribution of the autoxidative glycosylation to the formation of CML is negligible [56]. On the other hand, in a model system using labeled glucose most of the CML produced originated either from glucose autoxidation or the Namiki pathway [64]. At low glucose and buffer concentrations all three major pathways (cleavage of Amadori product, Namiki and autoxidative pathways) afforded comparable amounts of CML, whereas the production of CML through the fragmentation of Amadori product was partially inhibited at high glucose concentrations [64]. The oxidative cleavage of Amadori product (7) having two enolizable protons at positions C1 and C3 may occur via two competing pathways featuring either 1,2-enaminol (6) or 2,3ene-diol (8) as the key intermediates. These enolic intermediates result from a base-catalyzed (hydroxide, phosphate) reaction, although the formation of 2,3-ene-diol may also be catalyzed via an intramolecular deprotonation by an amino group [65, 66]. Both 1,2-enaminol (6) and 2,3-ene-diol (8) undergo spontaneous autoxidation in the presence of molecular oxygen and under metal ion catalysis to produce superoxide anion, enediol oxy radicals, and hydrogen peroxide [67-70]. At high pH and in the presence of a suitable electron acceptor, 1,2-enaminol (6) loses a proton to form the enolate anion (24 ), which is oxidized to the enaminol radical (25 ), as illustrated in Scheme (6). Subsequent oxidation to the imine (26 ) followed by hydrolysis yields 2-glucosone (27 ) as the oxidative cleavage product through this pathway [71]. Under physiological conditions, the Amadori product derived from fructose and lysine forms CML (14 ) and erythronic acid (30 ) by oxidative cleavage between C2 and C3 of the sugar residue [55]. 2,3-Enediol (8) has been suggested as an intermediate in CML formation, and based on its structural homology with ascorbic acid, a radical mechanism has been proposed [72]. Trace amounts of metals in the buffer could be responsible for the generation of the alkoxy radical (28 ) from 2,3-ene-diol (8), the former being further oxidized to 1-amino-1,4-dideoxy-2,3-oxoglucosone (11 ), a putative α-dicarbonyl intermediate also allegedly formed under non-oxidative cleavage of Amadori 1658 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 H2 C NH C O HO C H H C H C Cho et al. Lys HC NH C OH HO C H +H+ OH H C OH - H2 O OH H C OH CH2OH CH2 OH 7 6 H HN Lys HN NH C OH C H H C OH H C OH CH2 OH A rg N H2 C HN H OH H OH N H2 C H O CH2 C OH H C OH H CH OH N H OH H OH Arg CH2 OH Lys H N N H Arg - H2 O OH NH HO N H H C Lys N H2 C - H2 O NH H N NH Arg H N N - H+ HC H L ys CH2 OH Lys L ys NH HO - H2 O HC 22 H N NH H2 N L ys OH CH2 OH Arg H OH 21 23 Scheme 5. product. As noted before, the presence of (11 ) in glycation mixtures is still uncertain, and it should be emphasized that the failure of aminoguanidine to inhibit CML formation does not only suggest that autoxidative glycosylation is not the major pathway leading to CML, but also provides evidence that the dicarbonyl (11 ) is not an intermediate in the oxidative degradation of Amadori product, as it should have been trapped by aminoguanidine. Based on the fact that experimental protein glycation yields hydrogen peroxide as a by-product [73], Elgawish et al. proposed [70] the Baeyer-Villiger oxidative cleavage of the C2C3 bond in diketone (11 ) as the pathway leading to CML and erythronic acid via the anhydride (29 ), as presented in Scheme (6). However, the participation of Baeyer-Villiger oxidation in the formation of CML is unlikely, because the incubation of glycated human serum albumin with 1mM H2 O2 failed to generate CML in a model system [56]. Moreover, because no accumulation of hydrogen peroxide in the incubation mixtures was observed, it is reasonable to assume that H 2 O2 is further reduced to free hydroxyl radicals [61]. Indeed, Nagai et al. showed that hydroxyl radicals produced through a Fenton reaction between Fe2+ and Amadori product-derived endogenous hydrogen peroxide play an important role in the oxidative cleavage of Amadori product into CML [74]. In connection to this, a study involving the incubation of Amadori products in the presence of scavengers of H2 O2 , superoxide, and hydroxyl radicals found the formation of CML to be inhibited by 88%, 100%, and 30%, respectively [55]. In another study, it was reported that superoxide promoted CML formation more efficiently than hydrogen peroxide and hydroxyl radicals [75]. A recent study using labeled glucose [76] has shed some light on the mechanism of formation of CML. The mechanism proposed implies tautomerization of the 3-deoxyosone formed from the Amadori compound into a 2,4-dioxo compound (31 ) followed by hydration to lead to CML (14 ) and 3,4-dihydroxy2-butanone (32 ), as shown in Scheme (7). It has also been reported that, although C1 and C2 contributed mostly to the formation of CML, C5 and C6 in glucose become more and more involved in CML formation with prolonged reaction times due to the shifting of the oxo group along the sugar backbone. Furthermore, evidence that the formation of CML via glyoxal is not the main pathway has been provided [76]. Schiff Base Degradation and CML Formation by Namiki Pathway (Stage iii) The Schiff base formed during the initial stage of the glycation reaction can also undergo degradation by retro aldol cleavage reactions via the Namiki pathway to form short chain carbonyl compounds such as glyoxal, glycoaldehyde, and their corresponding imine analogs [56, 77]. The rate of Schiff base degradation via the Namiki pathway increases with increasing pH, as retro-aldolization is favored under basic conditions. Although Namiki’s initial studies were conducted with basic aliphatic amines in a heated reaction system, Glomb et al. have shown that lysine derivatives of glyoxal and glycolaldehyde are also formed under physiological conditions [56]. In a tentative mechanism according to Scheme (8), the degradation may be triggered by intramolecular hydrogen bonding between the imine nitrogen atom and the C3 hydroxyl group hydrogen atom to form a chair conformer of the Schiff base (3), in which the retro-aldol cleavage of the C2-C3 bond is facilitated and Reaction Mechanisms in the Formation of AGEs H2C NH C O HO C H H C OH H C OH Current Medicinal Chemistry, 2007 Vol. 14, No. 15 Lys 1,2-enolization HC NH C OH HO C H H C OH H C OH Lys HC - H+ C NH O HO C H H C OH H C OH CH2 OH CH2 OH CH2 OH 7 6 24 Lys HC NBT2+ NH Lys . C O HO C H H C OH H C OH NBT+ . 1659 CH2 OH 25 N BT2+ 2,3-enolization NBT+ H2C NH C OH H H C OH C OH C Lys OH HC O HC N C O C O HO C H HO C H H C OH H C OH H C OH H C OH + H 2O - H 2N Lys CH2 OH Lys CH2 OH CH2 OH 8 27 M n+ 26 M (n-1)+ H2 C C NH. H2 C H L ys H2C C OH C O C O C O C OH C OH O2 - O2 H NH C OH H H CH2 OH C H 2C Lys NH C O C O C OH L ys Baeyer-Villiger H H OH CH2 OH 14 + H2O COOH OH H C OH CH2 OH H C OH C Lys O OH O + H2 O2 NH CH2 OH 28 29 11 30 Scheme 6. produces the Schiff base of glycolaldehyde (34 ). This intermediate could undergo hydrolysis to glycolaldehyde (35 ), which is subsequently oxidized to glyoxal (36 ), or could rearrange to produce aminoaldehyde (37 ) which forms pyrazine (38 ) upon cyclocondensation with a second molecule of aminoaldehyde [56]. Oxidation of pyrazine (38 ) yields a N,Ndialkylpyrazinium radical cation which fragments to glyoxal or di- and mono-Schiff bases of glyoxal (39 ) and (40 ) respectively. H2 C NH C O HO C H H C OH H C OH Lys 1,2-enoliz ation CH2 OH HC NH C OH HO C H H C OH H C OH Glomb and Monnier have suggested that glyoxal and glycoaldehyde generated in the Namiki pathway can lead to the Lys HC - H2 O CH2 OH 7 Glyoxal and its corresponding imine analogs are responsible for the formation of several AGEs including CML, (carboxymethyl)arginine (CMA), Nε-(carboxyethyl)lysine (CEL), glyoxal-lysine dimer GOLD, arginine-lysine-glyoxal crosslink GODIC and pentosidine. N C OH L ys C O HO + H2O CH2 H C O C OH CH2OH H C H C OH H C OH H C OH H C OH CH2OH H2C NH C CH2 OH OH Lys C H NH Lys O OH CH2 14 CH3 C O C OH CH2 OH 31 Scheme 7. Lys OH C H2C NH NH C H 6 H2 C HC H C O C OH CH2OH 32 Lys 1660 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 HC N H C OH HO C H H C OH H C OH Cho et al. Lys L ys N HO HOHC O retro-aldol HC H CH OH O H C OH H C OH - CH 2OH CH2 OH HC NH HC OH Lys HC N H2 C 33 L ys OH 34 + H2 O CH2OH - H2 N L ys 3 H2 C NH HC Lys O 37 HC O H2C OH 35 O2 dimerization O2 Lys N N HC O HC O 36 Lys 38 + H2 O - H2 N - eLys HC N N HC O fragmentation L ys Lys 39 N HC N Lys Lys HC N Lys 40 Scheme 8. formation of CML [56]. Although there is no clear experimental evidence of this, aminoaldehyde (37 ) seems to be the most obvious intermediate from which CML can be derived through either oxidative or non-oxidative pathways. As shown in Scheme (9), the oxidation of aminoaldehyde (37 ) could be achieved by any of the oxygen reactive species present in the glycation mixture, or even by molecular oxygen under metal ion HC N H C OH HO C H H C OH H C OH It is noteworthy to mention that Schiff base degradation through the Namiki pathway is not the only way to generate short chain carbonyl compounds such as glycolaldehyde or L ys Namiki pathway H2 C NH HC O H2 C Lys Cannizz aro C OH 37 CH2OH 14 3 oxidation H2 C C OH 14 Scheme 9. catalysis. Alternatively, aminoacetaldehyde (37 ) may lead to CML (14 ) via a Cannizzaro reaction under non-oxidative conditions, a hypothesis that is supported by complementary experiments conducted with aminoacetaldehyde at pH 9 [56]. NH O L ys NH O Lys H2 C + CH 2 OH NH Lys Reaction Mechanisms in the Formation of AGEs Current Medicinal Chemistry, 2007 Vol. 14, No. 15 glyceraldehyde in vivo. For example, the former can be produced by the action of myeloperoxidase–hydrogen peroxide–chloride system on serine [78], whereas the latter could arise from the glycolysis pathway. incubation of glucose with RNase under oxidative conditions [58]. A hypothetical mechanism for the formation of arabinose and glyoxal through autoxidation, according to Scheme (10 ), shows that the enol form of glucose-derived Schiff base or Amadori product (7) can react with C1 of another molecule of glucose via the enamine reaction to form the intermediate (41 ), which rapidly rearranges to (42 ). Enolization of the aminoketose (42 ) at the amino tethered α-carbon generates the enaminol (43 ), whose chair conformation can drive a retro-aldol reaction that is initiated by intramolecular hydrogen abstraction to form arabinose. The cleavage of arabinose leaves behind the iminoketoheptose (44 ) which rearranges to aminoaldoheptose (45 ), an intermediate from which a second molecule of arabinose splits off via a retro-aldol reaction to finally give the enaminol (33 ), a precursor of glyoxal. According to this mechanism, the ratio of arabinose to glyoxal formed during autoxidative Formation of Arabinose from Glucose-Derived Amadori Products (Stage iv) A closer look at the structure of pentosidine clearly shows that a pentose is required to generate its pyridine ring. However, pentosidine can also be readily produced during the postAmadori stage of the glycation reaction when the starting sugars are hexoses such as glucose or fructose [79]. Elucidation of the mechanism of formation of pentosidine from glucose incubation systems was a difficult challenge until Wells-Knecht et al. reported the formation of glyoxal and arabinose during the HC NH L ys C OH HO C H H C OH H C OH H CH2 OH HO C H H C OH enamine reac tion HC 6 H C C Lys N CH2 OH CH2OH (CHOH) 4 (CH2OH) 4 H C OH CH C OH HO C H C O H C OH HO C H H C OH H C OH CH2 OH H C OH H O OH OH CH2 OH OH OH HN C C NH Lys C H H C OH H C OH HO O4H9 C 4 OH HO NH H2 C (CH2 OH)4 C OH Lys 42 1 H C HC CH2OH 41 CH2O H Lys C4 H9 O4 O H - HC O HO C H H C OH H C OH OH C N Lys H C OH HO C H H C OH H C OH CH2 OH 44 CH2 OH CH2 OH 43 HC OH C NH H C OH HO C H L ys O HC NH H C O HO C H H C OH H H C OH H CH2 OH HC C C L ys H O HO C H H C OH H C OH HC OH HC NH OH CH2 OH H2 C O NH 36 H2C OH HC N 34 CH2 OH HC Scheme 10. Lys 33 - 45 HC OH 1661 L ys Lys 1662 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 Cho et al. glycosylation is 2:1, which is in good agreement with the experimental observation that the incubation of glucose with RNase produced arabinose and glyoxal in the ratio of about 2.5:1. The difference between the experimental results and the theoretical value may be explained by the fact that the aminoaldehyde (36 ) can undergo a wide range of transformations leading to many other substances besides glyoxal. In addition, the Girard-T reagent that was used to detect the amount of glyoxal formed does not detect glycoaldehyde and its imine derivatives (34 ), also arising from the tautomerization of the enaminol (33 ). identified in incubations of D-arabinose with lysine [48]. The identification of (48 ) enabled the mechanistic elucidation of the generation of pentosidine from arabinose as shown in Scheme (11 ). The reaction begins with the formation of Amadori product (46 ), which then undergoes enolization to yield 2,3-ene-diol (47 ), which in turn undergoes sequential β-elimination reactions that cause the double bond to migrate to the end of the carbohydrate backbone to form a 5,6-ene-diol. Subsequent dehydration and tautomerization of this 5,6-ene-diol leads to the formation of the lysine-linked dideoxyosone (48 ), which then undergoes intramolecular condensation between the amino group and the terminal aldehyde to form the cyclic β-keto iminium ion (49 ). Condensation of (49 ) with arginine leads to pentosinane (50 ), an isolated intermediate which yields the crosslink end product pentosidine (17 ) at the end of a reaction sequence comprising oxidation, dehydration, and aromatization [52]. Despite the obvious necessity of molecular oxygen for the transformation of pentosinane into pentosidine, a study found that the formation of pentosidine from arabinose proceeds even under non-oxidative conditions (absence of oxygen and in the presence of metal ion chelators) with a yield of about 50% [84]. The authors inferred that the formation of pentosidine either occurs via a mechanism that is difficult to inhibit by antioxidative conditions, or that the oxidative mechanism might involve intermolecular redox processes rather than oxygen-dependent reactions. The results of this study is in agreement with the observation made by Biemel et al. that the partial transformation of pentosinane to pentosidine could not be prevented by applying antioxidative conditions as employed in the synthesis of pentosinane from pentoses [52]. Pentosidine Formation from Schiff Base via Biemel’s Pathway (Stage v) Pentosidine is a fluorescent protein crosslink AGE that can be derived from lysine-sugar-arginine interaction. It accumulates in collagenous tissues with age and its accumulation is accelerated in diabetic patients [80]. It is also the first AGE used as a biomarker for the assessment of glycation in biological systems [81]. Like other glycoxidation products, pentosidine can result from a plethora of pathways, the starting point being either the Schiff base (3) or the Amadori product (7). For example, pentosidine can result from the reaction between lysine, arginine and glyceraldehyde or glycoaldehyde during the early stage of the glycation reaction. Farboud et al. [82] demonstrated that pentosidine was generated in significant amounts in a time and concentration dependent manner when BSA was incubated under physiological conditions with glycoaldehyde, a product of Schiff base degradation through Namiki pathway. Recently, Chellan and Nagaraj [83] have shown that glyceraldehyde resulting from the fragmentation of glucose [46] also produces high levels of pentosidine in a model system, and proposed that the mechanism of pentosidine formation may be initiated by glyceraldehyde-arginine condensation reaction. However, the major pathway for pentosidine formation presumably involves the ring closure with arginine residues of the novel dideoxyosone (48 ), a reasonable α-dicarbonyl precursor HC N HO C H H C H C Lys HC NH HO C OH H C OH OH H C OH CH2 OH Generation of -Dicarbonyls from Glucose (Stage vi) The production of reactive α-dicarbonyls involved in the formation of AGEs occurs beyond protein glycation. Simple monosaccharides autoxidise at pH 7.4 and 37°C to produce βketoaldehydes via a process involving free radicals, as illustrated in Scheme (12 ). Enolization is a prerequisite for monosaccharide autoxidation, and trace metal ions may catalyse L ys H 2C HO H CH2 OH NH L ys H2 C C HO C H C OH C OH C OH C OH CH2 OH 46 NH CH2 OH 47 H 2C NH HO C H H C OH C OH HC OH L ys H2 C HO C NH Lys H2 C H HO CH C HC C NH OH O L ys Lys H N + H+ CH2 - H2O C O HC O + - H2 O HO 48 HN L ys NH H2 N N Arg - H+ N+ N NH N HO H 50 Arg O 49 Lys - H2 O Scheme 11. L ys H N NH - H2 O N - H17 Arg Reaction Mechanisms in the Formation of AGEs Current Medicinal Chemistry, 2007 Vol. 14, No. 15 monosaccharide autoxidation, but only up to a maximum rate limited by the rate of monosaccharide enolisation [85]. Spontaneous degradation of glucose in buffered solution at 37°C leads to glyoxal, methylglyoxal and 3-DG [46]. Glyoxal (36 ) is formed in the degradation of glucose by retro-aldol condensation reactions activated by deprotonation of the 2- or 3-hydroxy groups, along with erythrose (51 ) or erythrol (52 ). Deprotonation of C-2 is a common initial activation step in the formation of glucosone (54 ) and 3-deoxyglucosone (3-DG) (10 ). Re-distribution of the electron density between C-1 and C-2 leads to the formation of 1,2-ene-diol (53 ), whereas redistribution of the electron density between C-2 and C-3 followed by dehydration leads to 2,3-enol (55 ) and thereby 3DG (10 ). Methylglyoxal (12 ) is formed by fragmentation of 3DG (10 ), along with glyceraldehyde (13 ). The initial rates of formation of glyoxal, methylglyoxal and 3-DG were dependent on phosphate buffer. This may be due to the catalytic action of phosphate dianion HPO4 2- in the activation of the deprotonation of glucose [85]. The marked inhibition of - glyoxal formation by a metal ion chelator is consistent with redox active metal ions (Fe3+ and Cu 2+ ) catalysing the autoxidation of glycoaldehyde leading to the formation of glyoxal and hydroxyl radical [85]. 3-DG formation was also decreased by a metal ion chelator, suggesting that trace metal ion–phosphate complexes may be involved in the activation of glucose for 3-DG formation [46]. AGEs Derived from -Dicarbonyls (Stage vii) Despite their relatively low concentration in reaction mixtures compared to the concentration of the parent carbohydrates, α-dicarbonyls are a class of intermediates responsible for most of the AGE formation, including a significant number of crosslinks, due to their high reactivity. Besides the AGEs already shown in Fig. (1), a series of other compounds, mainly crosslinks resulting from α-dicarbonyls are presented in Fig. (2) and Fig. (3). Glyoxal was identified as an H2 C OH H C OH H C OH CH2 OH 52 retro-aldol HC O H C OH HO C H H H C C HC H retro-a ldol C O OH + H OH C OH HC OH HC O HC OH H2C OH OH 35 51 1 1,2-enolization HC OH HC O C OH C O HO C H HO C H H C OH H C OH H C OH H C OH M n+ O2 O2 CH2O H CH2 OH 53 54 –H2 O HC O OH C O C H CH2 C OH H C OH OH H C OH HC C H H Scheme 12. C O re tro-aldol CH2 OH CH2O H 55 10 Mn+ O2 CH2 OH CH2 OH 1663 HC O C O CH3 12 HC H C O OH CH2OH 13 HC O HC O O2 36 1664 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 Cho et al. HN HN COOH (CH2) 4 O CH2 (CH2 )4 HN N N NH NH C (CH2 )4 N (CH2) 3 (CH2) 3 HN CO NH NH (CH2 )3 CO HN CO N NH NH N HN CO CO HN 56 58 57 HN COOH H3C NH N (CH2 )4 (CH2) 4 60 OH H3 C H3 C CH3 N CH3 H3C OH N O N NH NH NH HN CO 59 OH N CH2 HN CO (CH2 )4 CH2 CO (CH2) 3 (CH2 )3 CO N HN 61 O CO CO H 3C 62 63 CO HN (CH2 )4 H3 C O O H3 C H3 C N HN N N H3C NH 2 N NH O (CH2 )3 NH (CH2 )3 (CH2 )3 CO HN HN CO CO 64 NH NH2 N (CH2 )3 HN N N HN 65 66 CO 67 Fig. (2). intermediate able to react with the ε-amino group of lysine residues in proteins to form CML [58] and an imidazolium crosslink known as glyoxal-lysine dimer (GOLD) (56 ) [86-88], which has been detected in human serum and lens protein. The modification of the guanidine function in arginine residues by glyoxal leads to N ω-(carboxymethyl)arginine (CMA) (57 ) [89, 90], which was found in skin collagen and human serum protein, and an imidazolone designated as Glarg (58 ) [91, 92]. Lederer et al. identified an arginine-lysine-glyoxal crosslink tagged GODIC (59 ) from a D-glucose-BSA incubation mixture [93], which was found later in human material [50, 51]. Methylglyoxal irreversibly modifies lysine residues in proteins under physiological conditions to give a higher homologue of CML, CEL (60 ) [94, 95], and an imidazolium crosslink labeled methylglyoxal-lysine dimer (MOLD) (61 ) [96] which has been found in human lens protein [87, 97] and human serum [98]. Several adducts of methylglyoxal with arginine residues have been reported as well. Argpyrimidine (62 ) was acknowledged as a major fluorescent AGE in glycated bovine lenses [99] and discovered later in tissue proteins [100], human lens proteins [101, 102], and even in amyloid deposits [103] and in human cancer tissues [104]. A methylglyoxal-arginine adduct having a tetrahydropyrimidine structure (63 ) was also identified as a non-fluorescent product in a BSA incubation [105], along with methylglyoxal-derived hydroimidazolone MG-H1 (64 ) [106]; the isomeric hydroimidazolones MG-H2 (65 ) and MG-H3 (66 ) have also been reported [107]. The arginine-lysinemethylglyoxal crosslink coined as MODIC (67 ) is an analog of Reaction Mechanisms in the Formation of AGEs Current Medicinal Chemistry, 2007 Vol. 14, No. 15 Besides α-dicarbonyls, hydroxyaldehydes such as glycoladehyde and glyceraldehyde have also been shown to be the starting materials for the recently discovered AGEs GApyridine (73 ) [120, 121], OP-lysine (74 ) [122] and GLAP (75 ) [123-125]. GODIC, and was synthesized and detected in a D-glucose-BSA incubation mixture [93], human serum albumin and lens protein [50], and senescent human extracellular matrix [51]. The acid labile pyrraline (16 ) [108, 109] and imidazolone (15 ) [110] are the most representative AGEs with a 3-DG-modified lysine structure, the former being detected in human diabetic lenses [111]. Skovsted et al. have isolated a derivative of the imidazolium crosslink 3-deoxyglucosone-lysine DOLD (68 ) from the reaction between N2 -hippuryl-lysine and 3-DG [112], but the actual crosslink has not yet been detected in vivo. Along with imidazolone (15 ), hydroimidazolone (69 ) was reported to result from 3-DG and arginine derivatives [113, 114], the former being immunohistochemically detected in diabetic patients [115]. DOGDIC (23 ), the corresponding arginine-lysine crosslink derived from 3-DG was also prepared [93] and identified in vivo [50, 51]. Other crosslinks that have been only scarcely reported in the literature are the acid-stable cationic fluorophores vesperlysines A (R = H) and B (R = CH 3 ) (70 ), vesperlysine C (71 ) [116, 117] and crosslines (72 ) [118, 119]. CO HN H H HOH 2C H (CH2 )4 HN (CH2 )4 HN CO OH N NH N (CH2 )3 (CH2 )4 HN 68 OC N N OH OH HN O OH OH N H Immunological approaches using monoclonal and polyclonal antibodies specific for AGE-modified proteins have been developed and have been used to confirm the presence of AGEs in vivo [126]. Furthermore, antibody libraries for AGE structures are important tools for the discovery of novel AGE structures in vitro and in vivo. The initial studies in this realm proved the existence of a common structure among AGEs derived from different glycated proteins and the specificity of these antibodies for AGEs, but not for early-stage glycation products such as Schiff base or Amadori product [127, 128]. CML (14 ) was shown to be a major immunological epitope among AGEs [129, 130], and the use of AGE-modified BSA as an antigen allowed the preparation of a monoclonal anti-AGE antibody (6D12) in mice specific for CML [128]. The carbonyl HOH2 C (CH2 )4 CO HN R CO 70 69 HN OC NH (H2 C) 4 (H2 C)4 CO CH2OH N N HN HN OH CO (CH2 )4 OC OH (CH2) 4 N HO N CH HO - HOH2 C (CH2 )4 (CH2 )4 CO OH HN CO 73 HN HO H N O COOH O Fig. (3). HN OH + N 74 OH 72 + N H2 N (CH2) 4 CH2 OH 71 O + N OH H H OH CH2 OH H N H N NH OH OH HO N H O 75 1665 76 1666 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 group in CML plays an important role in its recognition by the antibody, and it has recently been found that 6D12 and conventionally prepared polyclonal anti-CML antibody crossreact with CEL (60 ) because of its structural similarity to CML [131]. A novel monoclonal antibody specific for CML (CMS-10) has been prepared, and its reactivity was highly correlated with the CML content determined by high performance liquid chromatography [131]. Several polyclonal anti-AGE antibodies specific for other epitopes (non-CML) have also been prepared and characterized [132], but the structure of these epitopes remains unknown. The antibodies developed for glyoxalmodified proteins were able to recognize GOLD (56 ) [133], whereas the ones prepared for methylglyoxal-modified proteins identified argpyrimidine (62 ), MOLD (61 ), and GOLD (56 ) [105, 134]. Another series of non-CML anti-AGE antibodies that recognize a broad range of serum proteins modified by 3-DG (10 ), glyceraldehyde (13 ), glycolaldehyde (35 ), methylglyoxal (12 ), glyoxal (36 ), and glucose (1) has also been developed [135, 136]. Using immunochemical methods, pentosidine (17 ) was detected in biological samples [137] and in vitro [138], 3DG-imidazolone (15 ) was identified in brain tissues [139] and atherosclerotic lesions [110], pyrraline (16 ) was evidenced in diabetic tissues [140] and in familial amyotrophic lateral sclerosis patients [141], and CEL (60 ) was recognized by its antibody in diabetic rats [142], spinal cord astrocytes [143], and corneas [144]. Novel AGEs such as the non-fluorescent, acidlabile, imidazole-based arginine-lysine cross-link ALI (76 ) [145] or GA-pyiridine (73 ) [120] have also been evidenced through immunochemical studies. Finally, the issue of recognition of AGEs by the receptor for advanced glycation end products (RAGE) has to be briefly addressed. Receptors binding AGEs were initially thought to be scavenger receptors implicated in the removal of AGEs, and faulty disposal of AGE-modified proteins was believed to be relevant in aging and diseases such as diabetes or atherosclerosis [146, 147]. The cloning and subsequent characterization of RAGE [148] provided evidence that binding of AGEs to RAGE did not lead to an accelerated clearance and degradation with all the expected beneficial effects. Instead, ligand–receptor interaction resulted in post-receptor signalings that comprise but are not limited to activation of p21 ras, MAP kinases, and the NF-κB pathway [149-151]. Therefore, the concept of RAGE as a scavenger/clearance receptor for AGEs has to be amended and extended. Nevertheless, the precise chemical nature of AGE structures mediating RAGE binding have not been identified, but some evidence supports a role for CML as a RAGE ligand [152]. In addition, one study [153] reported that RAGE binding affinity for AGEs showed some dependence on the CML content, whereas fluorescence and pentosidine content did not robustly predict RAGE binding, suggesting that fluorescent AGEs and pentosidine do not bind to RAGE. Glyceraldehyde- and glycolaldehyde-derived AGEs were shown to bind to RAGE with estimated K d values of 300 nM and 1.4 µM, respectively, whereas glucose-derived AGEs exhibited a lower ability to bind to RAGE [154]. Inhibition of Protein Glycation Protein glycation is a complex natural process involving a cascade of reactions dependent on the pH of the medium and the presence of reactive oxygen species and metal ions. A series of intermediates that are very often more reactive towards proteins than the starting carbohydrates are generated through multiple pathways and at different stages of the reaction. Because protein glycation can not be avoided, strategies involving its prevention or even its reversal are to be envisaged. To the best of our best knowledge, no positive biological effects of glycation have been reported. This makes the inhibition of glycation by a selective inhibitor a rather unique approach in Cho et al. the sense that no negative effects are to be expected. The thorough understanding of the chemistry of glycation under physiological conditions could prove to be a useful tool in the successful discovery of safe and effective anti-glycation agents for use as therapeutic agents. One of the current therapeutic strategies for the prevention, cure and management of age and diabetes related health complications involves the use of anti-glycation agents. These are chemical compounds that can slow down, inhibit the glycation process, or even reverse its negative consequences [155, 156]. Generally, anti-glycation agents can suppress the formation of AGEs, either through preventing glycoxidations or by sequestering the reactive α-dicarbonyls. Recently, compounds that break down the protein cross-links have also been included in this category. The design of drugs to inhibit AGEs formation considerably challenges the pharmaceutical industry, because these inhibitors must react stoichiometrically with a wide range of structures, trap low molecular weight soluble reactive intermediates, which they must intercept in the presence of much higher concentrations of reactive functional groups on proteins. Lysine residues are the major site of chemical modification of proteins by sugars, and a concentration near 50 mM of plasma proteins requires that an AGE formation inhibitor (whose concentration in plasma during therapy is much lower) be significantly more reactive than lysine. Alternatively, the inhibitor may intercept the formation of AGEs at a stage either preceding the formation of the reactive carbonyl intermediates or after the formation of a reactive adduct with protein. The inhibitor should display in the same time all these activities without interfering with the normal metabolism of aldehydes or ketones in vivo. The structures of the currently known anti-glycation inhibitors are shown in Fig. (4). Aminoguanidine (77 ), the prototype AGE inhibitor [157], is one of the most studied anti-glycation agents that have been evaluated for their potential use as therapeutic agents. The antiglycation property of aminoguanidine is based on its ability to scavenge α- and β-dicarbonyl species formed during glycation to produce stable hydrazones or 3-amino-1,2,4-triazine compounds [158]. In spite of the beneficial effects of aminoguanidine in reducing the deleterious effects of glycation, its clinical trial was terminated due to safety concerns. Like most of anti-glycation agents that act as reactive carbonyls trappers, aminoguanidine also sequesters pyridoxal phosphate and may adversely affect vitamin B6 metabolism [159] and inhibit nitric oxide synthase [160] and semicarbazide sensitive amine oxidase [161] at the pharmacological concentration required for its anti-glycation activity [162]. Designed based on the structural motif of aminoguanidine, the novel inhibitor ALT-946 (78 ) proved to be a more potent inhibitor of AGEderived protein modification than aminoguanidine and devoid of nitric oxide synthase inhibitory action [163]. Metformin (79 ), a bisguanidine which has been used in the treatment of type II diabetes was shown to reduce blood glucose levels via a serine–threonine protein kinase termed LKB1, which phosphorylates and activates adenosine monophosphateactivated protein kinase [164]. Metformin is a moderate AGE inhibitor due to its ability to trap methylglyoxal and form the corresponding dihydroimidazolone derivative, although it is not as reactive as aminoguanidine [165]. Pyridoxamine (80 ) was reported as a novel, less toxic AGE inhibitor in studies evaluating analogs of vitamins involved in the metabolism of carbonyl compounds such as thiamine or pyridoxine [20, 166]. Like aminoguanidine, pyridoxamine inhibited the modification of lysine residues and the loss of enzymatic activity of RNase in the presence of glyoxal and glycolaldehyde, as well as the formation of BSA-derived CML [167]. In contrast to aminoguanidine, pyridoxamine proved to Reaction Mechanisms in the Formation of AGEs Current Medicinal Chemistry, 2007 Vol. 14, No. 15 1667 H2 N NH NH NH H N H2 N H2 N N H N H N H2 HO CH3 CH3 H2 N N H N H N N 78 79 80 O H3C O O H3C N N Br C6 H5 S NH Br O H3 C S S 81 H3C 82 N CH 3 83 O CH3 O O CH3 COOH H3C N H CH3 N N H Br O HOOC CH3 CH3 O 77 OH NH N H N H Cl N H Cl 84 N N N HN N N N HN CH3 N O H3 C N N O HOOC O NH2 N H H3 C HOOC O CH3 CH3 OH O O N O HN 86 85 87 NH2 CH3 O O N S N N H2 HN NH 88 PO3H O N CHO S H3C N H2 89 90 Fig. (4). be a potent inhibitor of AGE formation from glycated proteins, which granted it the name of “Amadorin”, a post-Amadori inhibitor of AGE formation [168]. Besides its ability to trap αdicarbonyl intermediates, evidence that pyridoxamine blocks Amadori product-to-CML conversion by interfering with the catalytic role of redox metal ions that are required for this glycoxidative reaction has been provided [169]. The acknowledgment that pyridoxamine has a limited potential to react with dicarbonyl precursors of AGE fueled a rational mechanism-based approach to design second-generation low- nucleophilicity Amadorins with improved specificity only for inhibiting post-Amadori pathway. This effort has successfully produced prototypical compounds such as BST-4997 [170]. An overview of the results of animal model studies concerning the use of pyridoxamine for inhibiting AGE formation and the development of complications of diabetes [171] and its hypothetical mechanism of action have been recently reviewed [172, 173]. A relatively novel potential therapeutic approach for the AGE-derived pathologies is the development of a class of 1668 Current Medicinal Chemistry, 2007, Vol. 14, No. 15 compounds capable of breaking already existing AGE–protein crosslinks, and thus reverse cardiovascular and dermatological stiffness related to aging and diabetes. This constitutes an exciting approach since it would address the issue of preaccumulated AGEs and subsequently allow their clearance via the kidney. The prototype compound in this class is N(phenacyl)thiazolium bromide, which has been shown to cleave glucose-derived protein crosslinks both in vitro and in vivo [174]. Doubts raised about the effectiveness of N(phenacyl)thiazolium bromide due to its hydrolysis under physiological conditions [175] have led to the development of a stable analog, ALT-711 (Alagebrium) (81 ). The exact mechanism of crosslink breaking is not clearly understood at the present time. Based on the structural characteristics of the AGE–protein breaker compounds and the predicted dicarbonyl structural motif of the crosslinks, a mechanism for breaking AGE–protein crosslinks has been proposed in vivo [174]. This mechanism precludes the action of crosslink breakers on other AGE–protein crosslinks such as MOLD, GOLD, glucosepane, DOGDIC, MODIC, and GODIC, and whether these crosslink motifs are amenable to breaking by crosslink breakers is not clear at present. Thiazolium salts are among the most potent inhibitors of ascorbate oxidation [176], showing that their antioxidant characteristics can contribute, at least in part, to their AGE-inhibiting properties through the attenuation of glycoxidation. Regardless of its mechanism of action, the results of pre-clinical and clinical studies [177] show that ALT711 offers a potential therapy for the pathological conditions caused by AGE–protein crosslinks. The emergence of these thiazolium halides has paved the way for the design of other AGE-breakers such as C16 (82 ) [178]. Another inhibitor of advanced glycation, OPB-9195 (83 ) belongs to a group of thiazolidine derivatives known as hypoglycemic drugs, but its action of inhibiting both AGEderived cross-linking and the formation of AGEs does not involve the lowering of blood glucose levels but rather an interaction with carbonyl groups and prevention of the initial Schiff base formation [179]. The use of OPB-9195 decreased pentosidine yield in uremic plasma from unspecified carbonyl compounds (“carbonyl stress”) in a similar manner to aminoguanidine, allowing a structure–activity supposition based on the fact that both inhibitors share a hydrazine function (available in the case of OPB-9195 after hydrolysis) capable of forming hydrazones with the carbonyls [180]. Furthermore, the concentrations of three major glucose-derived reactive carbonyl compounds (glyoxal, methylglyoxal and 3-DG) have been significantly reduced in the presence of OPB-9195 [181], and CML accumulation in diabetic nephropathy has also been deterred [182]. However, at milimolar concentration, OPB-9195 and other AGE inhibitors used in studies in vitro have very strong metal ion binding activity, and their inhibition of AGE formation is likely to be the result of their chelating or antioxidant activity rather than their carbonyl trapping activity [176]. A large series of phenoxyisobutyric acid derivatives initially developed as allosteric effectors of hemoglobin for lowering oxygen affinity of human blood [183] have been reported to be potent inhibitors of glycation [184]. The mechanism of action of this class of compounds is unknown. Evidence suggests that that they act in the early stage, but mostly inhibit the post-Amadori glycation, and a good number of them are inhibitors of AGE–protein crosslinking. Structure–activity relationship investigations have shown that compounds with an additional aryl- and heteroaryl-ureido or aryl- and heteroaryl-carboxamido structure show higher inhibitory effects, leading to inhibitors which are approximately 40 times more potent than aminoguanidine, and in the same time 2 to 3 times more effective than pyridoxine. Cho et al. From a second series of compounds, including several substituted aryl and heteroaryl carboxylic acids and substituted phenoxyacetic acids, LR-90 (84 ) has emerged as a potent in vitro inhibitor of AGE–collagen crosslinks formation [185]. LR90 manifested the same inhibitory effects in vivo, presumably by inhibiting the autoxidation pathways before and after the formation of reactive carbonyl species due to its strong metal chelating property [186]. Carnosine (β-alanyl-L-histidine) (85 ) is a naturally occurring non-toxic dipeptide and a commercially available drug that acts both as an antioxidant and an anti-glycation agent [187]. It inhibits protein glycation and crosslinking by acting as an alternative and competitive glycation target [188, 189] as it directly reacts with glycating agents through its primary amino group, whereas its imidazole moiety plays a supportive role either by stabilizing the pyrazinium adduct formed between the glycating agent and carnosine or by chelation to ion metals [190]. The antioxidant properties of carnosine [191], which are directed towards scavenging hydroxyl radicals [192, 193] and peroxyl radicals [194], also contribute to its anti-glycation activity. The most striking antiglycation property of carnosine is its ability to reverse preexisting glycation [195], possibly through a transglycation reaction involving the Schiff bases of sugars [196]. Other protective processes may involve “carnosylation”, carnosine’s reaction with glycated and oxidized proteins having carbonyl functions [197], and subsequent facilitation of the inactivation/removal of such deleterious proteins [198]. However, the AGE-inhibitory action of carnosine is not comparable with that of aminoguanidine. N-Acetylcarnosine, a prodrug for carnosine is useful for age-related cataract management and prevention in human and canine eyes [199]. Several other compounds such as the angiotensin II receptor antagonists olmesartan (86 ) [200] and valsartan (87 ) [201], antiinflammatory drug tenilsetam (88 ) [202, 203], 2,3diaminophenazine (89 ) [204, 205], and the liposoluble thiamine derivative benfotiamine (90 ) [206] were also reported to inhibit the formation of AGEs in vitro or in vivo, but their application in therapeutics appears to be limited. The screening of a large library of drugs yielded over a hundred hits [207], most of them being anti-inflammatory drugs with antioxidant activity. Among these drugs, catechins, tetracyclines and adrenalines are the most potent with the IC50 values around 20 µM. CONCLUSIONS Nonenzymatic glycation of proteins in vivo and its resulting advanced glycation end products have been implicated in the development of several health complications associated with the normal aging process and diabetes. Studies conducted to elucidate the chemistry of the glycation reaction and the mechanisms by which glycation induces protein damage that results in health complications have led to the general consensus that protein glycation in vivo involves a complex cascade of reactions including condensations, rearrangements, fragmentations, and oxidative steps. Several AGEs, such as CML and pentosidine, have been identified as biomarkers that can be used to indicate the extent of the glycation in biological systems. Most in vitro glycation investigations conducted under physiological conditions with the view to elucidate the reaction pathways leading to these biomarkers have only presented generalized schemes focusing on a certain stage of glycation, without placing the findings in a larger context, nor showing clear details on the multitude of pathways involved in the formation of AGEs. Due to the complexity of the processes involved in glycation, the redundancy of some stages, and in several cases the multiples possibilities for the generation of the same AGE, it is difficult to conceive that a unique successful Reaction Mechanisms in the Formation of AGEs inhibitor could be designed. The critical review of the current stage of the development of glycation inhibitors not only clearly shows that several types of inhibitors such as carbonyl trapping compounds, antioxidants and metal ions chelators had a limited efficiency but also hints to the long road ahead. The overall detailed mechanistic analysis of the glycation reaction pathways leading to the formation of AGEs presented in this paper definitely sets the stage for the development of mechanism-based chemical agents to prevent and manage the glycation related health complications. REFERENCES [1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16] [17] [18] [19] [20] [21] [22] [23] [24] [25] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] [37] [38] [39] [40] [41] Yaylayan, V.A.; Machiels, D.; Istasse, L. J. Agric. Food Chem., 2003, 51 , 3358. Monti, S.M.; Ritieni, A.; Sacchi, R.; Skog, K.; Borgen, E.; Fogliano, V. J. Agric. Food Chem., 2001, 49 , 3969. Skog, K.I.; Johansson, M.A.; Jägerstad, M.I. Food Chem. Toxicol., 1998, 36 , 879. Persson, E.; Graziani, G.; Ferracane, R.; Fogliano, V.; Skog, K. Food Chem. Toxicol., 2003, 41 , 1587. Kato, T.; Harashima, T.; Moriya, N.; Kikugawa, K.; Hiramoto, K. Carcinogenesis, 1996, 17 , 2469. Tsai, S.J.; Jenq, S.N.; Lee, H. Mutagenesis, 1996, 11 , 235. Weisburger, J.H.; Jones, R.C. Basic Life Sci., 1990, 52 , 105. Hayase, F.; Usui, T.; Watanabe, H. Mol. Nutr. Food Res., 2006, 50 , 1171. Usui, T.; Shizuuchi, S.; Watanabe, H.; Hayase, F. Biosci. Biotechnol. Biochem. , 2004, 68 , 247. Chuyen, N.V. Adv. Exp. Med. Biol., 1998, 434, 213. Somoza, V. Mol. Nutr. Food Res., 2005, 49 , 663. Koschinsky, T.; He, C.-J.; Mitsuhashi, T.; Bucala, R.; Liu, C.; Buenting, C.; Heitmann, K.; Vlassara H. Proc. Natl. Acad. Sci. USA, 1997, 94 , 6474. Uribarri, J.; Peppa, M.; Cai, W.; Goldberg, T,; Lu, M.; Baliga, S.; Vassalotti, J.A.; Vlassara, H. Am. J. Kidney Dis., 2003, 42 , 532. Trivelli, L.A.; Ranney, H.M.; Lai, H.T. N. Engl. J. Med., 1971, 284, 353. Thorpe, S.R.; Baynes, J.W. Drugs Aging, 1996, 9, 69. Friedman, E.A. Nephrol. Dial. Transplant., 1999, 14 (Suppl. 3), 1. Beisswenger, P.J.; Makita, Z.; Curphey, T.J.; Moore, L.L.; Jean, S.; Brinck-Johnsen, T.; Bucala, R.; Vlassara, H. Diabetes, 1995, 44 , 824. Brownlee, M. Nature, 2001, 414(6865), 813. Chiou, Y.J.; Tomer, K.B.; Smith, P.C. Chem. Biol. Interact., 1999, 121, 141. Booth, A.A.; Khalifah, R.G.; Todd, P.; Hudson, B.G. J. Biol. Chem., 1997, 272, 5430. Zyzak, D.V.; Richardson, J.M.; Thorpe, S.R.; Baynes, J.W. Arch. Biochem. Biophys., 1995, 316, 547. Hunt, J.V.; Bottoms, M.A.; Mitchinson, M.J. Biochem. J., 1993, 291, 529. Le Guen, C.A.; Jones, A.F.; Barnett, A.H.; Lunec, J. Ann. Clin. Biochem. , 1992, 29 , 184. Mossine, V.V.; Glinsky, G.V.; Feather, M.S. Carbohydr. Res., 1994, 262, 257. Dunn, J.A.; McCance, D.R.; Thorpe, S.R.; Lyons, T.J.; Baynes, J.W. Biochemistry, 1991, 30 , 1205. Sell, D.R.; Monnier, V.M. J. Biol. Chem., 2004, 279, 54173. Vrdoljak, A.; Trescec, A.; Benko, B.; Hecimovic, D.; Simic, M. Clin. Chim. Acta, 2004, 345, 105. Watkins, N.G.; Thorpe, S.R.; Baynes, J.W. J. Biol. Chem., 1985, 260, 10629. Iberg, N.; Flückiger, R. J. Biol. Chem., 1986, 261, 13542. Reiser, K.M.; Amigable, M.A.; Last, J.A. J. Biol. Chem., 1992, 267, 24207. Calvo, C.; Ulloa, N.; Campos, M.; Verdugo, C.; Ayrault-Jarrier, M. Clin. Chim. Acta, 1993, 217, 193. Lapolla, A.; Fedele, D.; Reitano, R.; Arico, N.C.; Seraglia, R.; Traldi, P.; Marotta, E.; Tonani, R. J. Am. Soc. Mass Spectrom., 2004, 15 , 496. Hinton, D.J.; Ames, J.M. Amino Acids, 2006, 30 , 425. Bunn, H.F.; Gabbay, K.H.; Gallop, P.M. Science, 1978, 200, 21. Valencia, J.V.; Weldon, S.C.; Quinn, D.; Kiers, G.H.; DeGroot, J.; TeKoppele, J.M.; Hughes, T.E. Anal. Biochem., 2004, 324, 68. Bunn, H.F.; Higgins, P.J. Science, 1981, 213, 222. Means, G.E.; Chang, M.K. Diabetes, 1982, 31 (Suppl. 3II), 1. Namiki, M. Adv. Food Res., 1988, 32 , 115. Neglia, C.I.; Cohen, H.J.; Garber, A.R.; Ellis, P.D.; Thorpe, S.R.; Baynes, J.W. J. Biol. Chem., 1983, 258, 14279. Dugas, H. Bioorganic Chemistry: A Chemical Approach to Enzyme Action , 3 rd ed., Springer-Verlag: New York, 1996, pp. 388. Current Medicinal Chemistry, 2007 Vol. 14, No. 15 [42] [43] [44] [45] [46] [47] [48] [49] [50] [51] [52] [53] [54] [55] [56] [57] [58] [59] [60] [61] [62] [63] [64] [65] [66] [67] [68] [69] [70] [71] [72] [73] [74] [75] [76] [77] [78] [79] [80] [81] [82] [83] [84] [85] [86] [87] [88] [89] [90] [91] [92] Kato, Y.; Watanabe, K.; Sato, Y. J. Agric. Food Chem., 1981, 29 , 540. [93] 1669 Hayase, F.; Shibuya, T.; Sato, J.; Yamamoto, M. Biosci. Biotechnol. Biochem. , 1996, 60 , 1820. Kolka, S. Pol. J. Chem., 1984, 58 , 689. Ledl, F.; Schleicher, E. Angew. Chem. Int. Ed., 1990, 29 , 565. Martins, S.I.; Marcelis, A.T.; van Boekel, M.A. Carbohydr. Res., 2003, 338, 1651. Thornalley, P.J.; Langborg, A.; Minhas, H.S. Biochem. J., 1999, 344, 109. Niwa, T. J. Chromatogr. B Biomed. Sci. Appl., 1999, 731, 23. Biemel, K.M.; Conrad, J.; Lederer, M.O. Angew. Chem. Int. Ed., 2002, 41 , 801. Lederer, M.O.; Bühler, H.P. Bioorg. Med. Chem., 1999, 7, 1081. Biemel, K.M.; Friedl, D.A.; Lederer, M.O. J. Biol. Chem., 2002, 277, 24907. Sell, D.R.; Biemel, K.M.; Reihl, O.; Lederer, M.O.; Strauch, C.M.; Monnier, V.M. J. Biol. Chem., 2005, 280, 12310. Biemel, K.M.; Reihl, O.; Conrad, J.; Lederer, M.O. J. Biol. Chem., 2001, 276, 23405. Henle, T.; Walter, A.W.; Haeßner, R.; Klostermeyer, H. Z. Lebensm. Unters. Forsch., 1994, 199, 55. Hayase, F.; Koyama, T.; Konishi, Y. J. Agric. Food Chem., 1997, 45 , 1137. Ahmed, M.U.; Thorpe, S.R.; Baynes, J.W. J. Biol. Chem., 1986, 261, 4889. Glomb, M.A.; Monnier, V.M. J. Biol. Chem., 1995, 276, 10017. Dyer, D.G.; Dunn, J.A.; Thorpe, S.R.; Bailie, K.E.; Lyons, T.J.; McCance, D.R.; Baynes, J.W. J. Clin. Invest., 1993, 91 , 2463. Wells-Knecht, K.J.; Zyzak, D.V.; Litchfield, J.E.; Thorpe, S.R.; Baynes, J.W. Biochemistry, 1995, 34 , 3702. Baynes, J.W.; Thorpe, S.R. Diabetes, 1999, 48 , 1. Al-Abed, Y.; Bucala, R. Bioorg. Med. Chem. Lett., 1995, 5, 2161. Wolff, S.P.; Dean. R.T. Biochem. J., 1987, 245, 243. Dunn, J.A.; Ahmed, M.U.; Murtiashaw, M.H.; Richardson, J.M.; Walla, M.D.; Thorpe, S.R.; Baynes, J.W. Biochemistry, 1990, 29 , 10964. Fu, M.-X.; Requena, J.R.; Jenkins, A.J.; Lyons, T.J.; Baynes, J.W.; Thorpe, S.R. J. Biol. Chem., 1996, 271, 9982. Wells-Knecht, M.C.; Thorpe, S.R.; Baynes, J.W. Biochemistry, 1995, 34 , 15134. Hodge, J.E. Adv. Carbohydr. Chem., 1955, 10 , 169. Coward, J.K.; Bruice, T.C. J. Am. Chem. Soc., 1969, 91 , 5339. Jones, A.F.; Winkles, J.W.; Thornalley, P.J.; Lunec, J.; Jennings, P.E.; Barnett, A.H. Clin. Chem., 1987, 33 , 147. Gillery, P.; Monboisse, J.C.; Maquart, F.X.; Borel, J.P. Diabetes Metab., 1988, 14 , 25. Azevedo, M.; Falcao, J.; Raposo, J.; Manso, C. Free Rad. Res. Commun., 1988, 4, 331. Elgawish, A.; Glomb, M.; Friedlander, M.; Monnier, V.M. J. Biol. Chem., 1996, 271, 12964. Baker, J.R.; Zyzak, D.V.; Thorpe, S.R.; Baynes, J.W. Clin. Chem. , 1994, 40 , 1950. Sakurai, T.; Tsuchiya, S. FEBS Lett., 1988, 236, 406. Jiang, Z.Y.; Woollard, A.C.; Wolff, S.P. FEBS Lett., 1990, 268, 69. Nagai, R.; Ikeda, K.; Higahi, T.; Sano, H.; Jinnouchi, Y.; Araki, T.; Horiuchi, S. Biochem. Biophys. Res. Commun., 1997, 234, 167. Smith, P.R.; Thornalley, P.J. Eur. J. Biochem., 1992, 210, 729. Kasper, M.; Schieberle, P. Ann. N.Y. Acad. Sci., 2005, 1043, 59. Hayashi, T.; Namiki, M. In Amino-Carbonyl Reactions in Food and Biological Systems, Fujimaki, M., Namiki, M., Kato, H., Eds.; Elsevier Science Publishers: Amsterdam, 1986; pp. 29. Anderson, M.M.; Requena, J.R.; Crowley, J.R.; Thorpe, S.R.; Heinecke, J.W. J. Clin. Invest., 1999, 104, 103. Grandhee, S.K.; Monnier, V.M. J. Biol. Chem., 1991, 266, 11649. Sell, D.R.; Monnier, V.M. J. Clin. Invest., 1990, 85 , 380. Sell, D.R.; Monnier, V.M. J. Biol. Chem., 1989, 264, 21597. Farboud, B.; Aotaki-Keen, A.; Miyata, T.; Hjelmeland, L.M.; Handa, J.T. Mol. Vision, 1999, 5, 11. Chellan, P.; Nagaraj, R.H. J. Biol. Chem., 2001, 276, 3895. Litchfield, J.E.; Thorpe, S.R.; Baynes, J.W. Int. J. Biochem. Cell Biol., 1999, 31 , 1297. Thornalley, P.J.; Wolff, S.P.; Crabbe, J.; Stern, A. Biochim. Biophys. Acta, 1984, 797, 276. Odani, H.; Shinzato, T.; Usami, J.; Matsumoto, Y.; Brinkmann Frye, E.; Baynes, J.W.; Maeda, K. FEBS Lett., 1998, 427, 381. Chellan, P.; Nagaraj, R.H. Arch. Biochem. Biophys., 1999, 368, 98. Wells-Knecht, K.J.; Brinkmann, E.; Baynes, J.W J. Org. Chem., 1995, 60 , 6246. Iijima, K.; Murata, M.; Takahara, H.; Irie, S.; Fusimoto, D. Biochem. J., 2000, 347, 23. Odani, H.; Iijima, K.; Nakata, M.; Miyata, S.; Kusunoki, H.; Yasuda, Y.; Hiki, Y.; Irie, S.; Maeda, K.; Fujimoto, D. Biochem. Biophys. Res. Commun., 2001, 285, 1232. Schwarzenbolz, U.; Henle, T.; Haebner, R.; Klostermeyer, H. Z. Lebensm. Unters. Forsch. A, 1997, 205, 121. Paul, R.G.; Avery, N.C.; Slatter, D.A.; Sims, T.J.; Bailey, A.J. Biochem. J., 1998, 330, 1241. Lederer, M.O.; Klaiber, R.G. Bioorg. Med. Chem., 1999, 7, 2499. 1670 [94] [95] [96] [97] [98] [99] [100] [101] [102] [103] [104] [105] [106] [107] [108] [109] [110] [111] [112] [113] [114] [115] [116] [117] [118] [119] [120] [121] [122] [123] [124] [125] [126] [127] [128] [129] [130] [131] [132] [133] [134] [135] [136] [137] Current Medicinal Chemistry, 2007, Vol. 14, No. 15 Ahmed, M.U.; Brinkmann Frye, E.; Degenhardt, T.P.; Thorpe, S.R.; Baynes, J.W. Biochem. J., 1997, 324, 565. Degenhardt, T.P.; Thorpe, S.R.; Baynes, J.W. Cell Mol. Biol. (Noisy-leGrand), 1998, 44 , 1139. Brinkmann, E.; Wells-Knecht, K.J.; Thorpe, S.R.; Baynes, J.W. J. Chem. Soc. Perkin Trans. I, 1995, 2817. Brinkmann, E.; Degenhardt, T.P.; Thorpe, S.R.; Baynes, J.W. J. Biol. Chem. , 1998, 273, 18714. Nagaraj, R.H.; Shipanova, I.N.; Faust, F.M. J. Biol. Chem., 1996, 271, 19338. Shipanova, I.N.; Glomb, M.A.; Nagaraj, R.H. Arch. Biochem. Biophys., 1997, 344, 29. Wilker, S.C.; Chellan, P.; Arnold, B.M.; Nagaraj, R.H. Anal. Biochem., 2001, 290, 353. Padayatti, P.S.; Ng, A.S.; Uchida, K.; Glomb, M.A.; Nagaraj, R.H. Invest. Ophthalmol. Vis. Sci., 2001, 42 , 1299. Ahmed, N.; Thornalley, P.J.; Dawczynski, J.; Franke, S.; Strobel, J.; Stein, G.; Haik, G.M. Invest. Ophthalmol. Vis. Sci., 2003, 44 , 5287. Gomes, R.; Sousa Silva, M.; Quintas, A.; Cordeiro, C.; Freire, A.; Pereira, P.; Martins, A.; Monteiro, E.; Barroso, E.; Ponces Freire, A. Biochem. J., 2005, 385, 339. van Heijst, J.W.; Niessen, H.W.; Hoekman, K.; Schalkwijk, C.G. Ann. N.Y. Acad. Sci., 2005, 1043, 725. Oya, T.; Hattori, N.; Mizuno, Y.; Miyata, S.; Maeda, S.; Osawa, T.; Uchida, K. J. Biol. Chem., 1999, 274, 18492. Lo, T.W.C.; Westwood, M.E.; McLellan, A.C.; Selwood, T.; Thornalley, P.J. J. Biol. Chem., 1994, 169, 32299. Ahmed, N.; Argirov, O.K.; Minhas, H.S.; Cordeiro, C.A.A.; Thornalley, P.J. Biochem. J., 2002, 364, 1. Nakayama, T.; Hayase, F.; Kato, H. Agric. Biol. Chem. , 1980, 44 , 1201. Hayase, F.; Nagaraj, R.H.; Miyata, S.; Njorogeg, G.; Monnier, V.M. J. Biol. Chem., 1989, 264, 3758. Jono, T.; Nagai, R.; Lin, X.; Ahmed, N.; Thornalley, P.G.; Takeya, M.; Horiuchi, S. J. Biochem. (Tokyo), 2004, 136, 351. Nagaraj, R. H.; Sady, C. FEBS Lett., 1996, 382, 234. Skovsted, I.C.; Christensen, M.; Breinholt, J.; Mortensen, S.B. Cell. Mol. Biol., 1998, 44 , 1159. Konishi, Y.; Hayase, F.; Kato, H. Biosci. Biotechnol. Biochem., 1994, 58 , 1953. Hayase, F.; Konishi, Y.; Kato, H. Biosci. Biotechnol. Biochem., 1995, 59 , 1407. Niwa, T.; Katsuzaki, T.; Ishizaki, Y.; Hayase, F.; Miyazaki, T.; Uematsu, T.; Tatemichi, N.; Takei, Y. FEBS Lett., 1997, 407, 297. Nakamura, K.; Nakazawa, Y.; Ienaga, K. Biochem. Biophys. Res. Commun., 1997, 232, 227. Tessier, F.; Obrenovich, M.; Monnier, V.M. J. Biol. Chem., 1999, 274, 20796. Nakamura, K.; Hasegawa, T.; Fukunaga, Y.; Ienaga, K. J. Chem. Soc. Chem. Commun., 1992, 992. Obayashi, H.; Nakano, K.; Shigeta, H.; Yamaguchi, M.; Yoshimori, K.; Fukui, M.; Fujii, M.; Kitagawa, Y.; Nakamura, N.; Nakamura, K.; Nakazawa, Y.; Ienaga, K.; Ohta, M.; Nishimura, M.; Fukui, I.; Kondo, M. Biochem. Biophys. Res. Commun., 1996, 226, 37. Nagai, R.; Hayashi, C.M.; Xia, L.; Takeya, M.; Horiuchi, S. J. Biol. Chem. , 2002, 277, 48905. Greven, W.L.; Waanders, F.; Nagai, R.; van der Heuvel, M.C.; Navis, G.; van Goor, H. Kidney Int., 2005, 68 , 595. Argirov, O.K.; Lin, B.; Ortwerth, B.J. J. Biol. Chem., 2004, 279, 6487. Usui, T.; Hayase, F. Biosci. Biotechnol. Biochem., 2003, 67 , 930. Usui, T.; Shimohira, K.; Watanabe, H.; Hayase, F. Biofactors, 2004, 21 , 391. Usui, T.; Shimohira, K.; Watanabe, H.; Hayase, F. Biosci. Biotechnol. Biochem. , 2007, 71 , 442. Makita, Z.; Vlassara, H.; Cerami, A.; Bucala, R. J. Biol. Chem., 1992, 267, 5133. Nakayama, H.; Taneda, S.; Kuwajima, S.; Aoki, S.; Kuroda, V.; Misawa, K.; Nakagawa, S. Biochem. Biophys. Res. Commun., 1989, 162, 740. Horiuchi, S.; Araki, N.; Morino, Y. J. Biol. Chem., 1991, 266, 7329. Reddy, S.; Bichler, J.; Wells-Knecht, K.J.; Thorpe, S.R.; Baynes, J.W. Biochemistry, 1995, 34 , 10872. Ikeda, K.; Higashi, T.; Sano, H.; Jinnouchi, Y.; Yoshida, M.; Araki, T.; Ueda, S.; Horiuchi, S. Biochemistry, 1996, 35 , 8075. Koito, W.; Araki, T.; Horiuchi, S.; Nagai, R. J. Biochem. (Tokyo), 2004, 136, 831. Ikeda, K.; Nagai, R.; Sakamoto, T.; Sano, H.; Araki, T.; Sakata, N.; Nakayama, H.; Yoshida, M.; Ueda, S.; Horiuchi, S. J. Immunol. Methods, 1998, 215, 95. Sady, C.; Jiang, C.L.; Chellan, P.; Madhun, Z.; Duve, Y.; Glomb, M.A.; Nagaraj, R.H. Biochim. Biophys. Acta, 2000, 1481, 255. Shamsi, F.A.; Partal, A.; Sady, C.; Glomb, M.A.; Nagaraj, R.H. J. Biol. Chem. , 1998, 273, 6928. Takeuchi, M.; Makita, Z.; Bucala, R.; Suzuki, T.; Koike, T.; Kameda, Y. Mol. Med., 2000, 6, 114. Takeuchi, M.; Yanase, Y.; Matsuura, N.; Yamagishi, S.; Kameda, Y.; Bucala, R.; Makita, Z. Mol. Med., 2001, 7, 783. Taneda, S.; Monnier, V.M. Clin. Chem., 1994, 40 , 1766. Cho et al. [138] [139] [140] [141] [142] [143] [144] [145] [146] [147] [148] [149] [150] [151] [152] [153] [154] [155] [156] [157] [158] [159] [160] [161] [162] [163] [164] [165] [166] [167] [168] [169] [170] [171] [172] [173] [174] [175] [176] [177] [178] [179] Miyazaki, K.; Nagai, R.; Horiuchi, S. J. Biochem. (Tokyo), 2002, 132, 543. Jono, T.; Kimura, T.; Takamatsu, J.; Nagai, R.; Miyazaki, K.; Yuzuriha, T.; Kitamura, T.; Horiuchi, S. Pathol. Int., 2002, 52 , 563. Miyata, S.; Monnier, V. J. Clin. Invest., 1992, 89 , 1102. Kato, S.; Horiuchi, S.; Liu, J.; Cleveland, D.W.; Shibata, N.; Nakashima, K.; Nagai, R.; Hirano, A.; Takikawa, M.; Kato, M.; Nakano, I.; Ohama, E. Acta Neuropathol. (Berlin), 2000, 100, 490. Ling, X.; Nagai, R.; Sakashita, N.; Takeya, M.; Horiuchi, S.; Takahashi, K. Lab. Invest., 2001, 81 , 845. Shibata, N.; Hirano, A.; Hedley-Whyte, E.T.; Dal Canto, M.C.; Nagai, R.; Uchida, K.; Horiuchi, S.; Kawaguchi, M.; Yamamoto, T.; Kobayashi, M. Acta Neuropathol. (Berlin), 2002, 104, 171. Kaji, Y.; Nagai, R.; Amano, S.; Takazawa, Y.; Fukayama, M.; Oshika, T. Br. J. Ophthalmol., 2007, 91 , 85. Al-Abed, Y.; Bucala, R. Bioconjug. Chem., 2000, 11 , 39. Vlassara, H.; Bucala, R.; Striker, L. Lab. Invest., 1994, 70 , 138. Vlassara, H.; Brownlee, M.; Cerami, A. Proc. Natl. Acad. Sci. USA, 1985, 82 , 5588. Neeper, M.; Schmidt, A.M.; Brett, J.; Yan, S.D.; Wang, F.; Pa, Y.C.E.; Elliston, K.; Stern, D.M.; Shaw, A. J. Biol. Chem., 1992, 267, 14998. Lander, H.M.; Taurus, J.M.; Ogiste, J.S.; Hori, O.; Moss, R.A.; Schmidt, A.M. J. Biol. Chem., 1997, 272, 17810. Basta, G.; Lazzerini, G.; Massaro, M.; Simoncini, T.; Tanganelli, P.; Fu, C.; Kislinger, T.; Stern, D.M.; Schmidt, A.M.; De Caterina, R. Circulation, 2002, 105, 816. Bucciarelli, L.G.; Wendt, T.; Rong, L.; Lalla, E.; Hofmann, M.A.; Goova, M.T.; Taguchi, A.; Yan, S.F.; Yan, S.D.; Stern, D.M.; Schmidt, A.M. Cell. Mol. Life Sci., 2002, 59 , 1117. Kislinger, T.; Fu, C.; Huber, B.; Qu, W.; Taguchi, A.; Du Yan, S.; Hofmann, M.; Yan, S.F.; Pischetsrieder, M.; Stern, D.; Schmidt, A.M. J. Biol. Chem., 1999, 274, 31740. Valencia, J.V.; Weldon, S.C.; Quinn, D.; Kiers, G.H.; DeGroot, J.; TeKoppele, J.M.; Hughes, T.E. Anal. Chem., 2004, 324, 68. Yonekura, H.; Yamamoto, Y.; Sakurai, S.; Yasui, K.; Petrova, R.G.; Abedin, M.J.; Li, H.; Watanabe, T.; Makita, Z.; Takeuchi, M.; Yamamoto, H. Int. Cong. Ser., 2002, 1245, 129. Thomas, M.C.; Baynes, J.W.; Thorpe, S.R.; Cooper, M.E. Curr. Drug Targets, 2005, 6, 453. Reddy, V.P.; Beyaz, A. Drug Discov. Today, 2006, 11 , 646. Nilsson, B.O. Inflamm. Res., 1999, 48 , 509. Thornalley, P.J.; Yurek-George, A.; Argirov, O.K. Biochem. Pharmacol., 2000, 60 , 55. Taguchi, T.; Sugiura, M.; Hamada, Y.; Miwa, Y. Biochem. Pharmacol., 1998, 55 , 1667. Tilton, R.G.; Chang, K.; Hasan, K.S.; Smith, S.R.; Petrash, J.M.; Misko, T.P.; Moore, W.M.; Currie, M.G.; Corbett, J.A.; McDaniel, M.L. Diabetes, 1993, 42 , 221. Yu, P.H.; Zuo, D.M. Diabetologia, 1997, 40 , 1243. Thornalley, P.J. Arch. Biochem. Biophys., 2003, 419, 31. Forbes, J.M.; Soulis, T.; Thallas, V.; Panagiotopoulos, S.; Long, D.M.; Vasan, S.; Wagle, D.; Jerums, G.; Cooper, M.E. Diabetologia, 2001, 44, 108. Shaw, R.J.; Lamia, K.A.; Vasquez, D.; Koo, S.H.; Bardeesy, N.; Depinho, R.A.; Montminy, M.; Cantley, L.C. Science, 2005, 310(5754), 1642. Battah, S.; Ahmed, N.; Thornalley, P.J. Int. Congr. Ser., 2002, 1245, 355. Booth, A.A.; Khalifah, R.G.; Hudson, B.G. Biochem. Biophys. Res. Commun., 1996, 220, 113. Voziyan, P.A.; Metz, T.O.; Baynes, J.W.; Hudson, B.G. J. Biol. Chem., 2002, 277, 3397. Khalifah, R.G.; Baynes, J.W.; Hudson, B.G. Biochem. Biophys. Res. Commun., 1999, 257, 251. Voziyan, P.A.; Khalifah, R.G.; Thibaudeau, C.; Yildiz, A.; Jacob, J.; Serianni, A.S.; Hudson, B.G. J. Biol. Chem., 2003, 278, 46616. Khalifah, R.G.; Chen, Y.; Wassenberg, J.J. Ann. N.Y. Acad. Sci., 2005, 1043, 793. Metz, T.O.; Alderson, N.L.; Thorpe, S.R.; Baynes, J.W. Arch. Biochem. Biophys., 2003, 419, 41. Voziyan, P.A.; Hudson, B.G. Ann. N.Y. Acad. Sci., 2005, 1043, 807. Voziyan, P.A.; Hudson, B.G. Cell Mol. Life Sci., 2005, 62 , 1671. Vasan, S.; Zhang, X.; Zhang, X.; Kapurniotu, A.; Bernhagen, J.; Teichberg, S.; Basgen, J.; Wagle, D.; Shih, D.; Terlecky, I.; Bucala, R.; Cerami, A.; Egan, J.; Ulrich, P. Nature, 1996, 382(6588), 275. Thornalley P.H.; Minhas H.S. Biochem. Pharmacol., 1999, 57 , 303. Price, D.L.; Rhett, P.M.; Thorpe, S.R.; Baynes, J.W. J. Biol. Chem., 2001, 276, 48967. Vasan, S.; Foiles, P.; Founds, H. Arch. Biochem. Biophys., 2003, 419, 89. Cheng, G.; Wang, L.L.; Qu, W.S.; Long, L.; Cui, H.; Liu, H.Y.; Cao, Y.L.; Li, S. Acta Pharmacol. Sin., 2005, 26 , 1460. Nakamura, S.; Makita, Z.; Ishikawa, S.; Yasumura, K.; Fujii, W.; Yanagisawa, K.; Kawata, T.; Koike, T. Diabetes, 1997, 46 , 895. Reaction Mechanisms in the Formation of AGEs [180] [181] [182] [183] [184] [185] [186] [187] [188] [189] [190] [191] [192] [193] Current Medicinal Chemistry, 2007 Vol. 14, No. 15 Miyata, T.; Ueda, Y.; Yamada, Y.; Izuhara, Y.; Wada, T.; Jadoul, M.; Saito, A.; Kurokawa, K.; van Ypersele de Strihou, C. J. Am. Soc. Nephrol., 1998, 9, 2349. Miyata, T.; Ueda, Y.; Asahi, K.; Izuhara, Y.; Inagi, R.; Saito, A.; van Ypersele de Strihou, C.; Kurokawa, K. J. Am. Soc. Nephrol., 2000, 11 , 1719. Nakamura, S.; Tachikawa, T.; Tobita, K.; Aoyama, I.; Takayama, F.; Enomoto, A.; Niwa, T. Am. J. Kidney Dis., 2003, 41 , S68. Lalezari, I.; Lalezari, P. J. Med. Chem., 1989, 32 , 2352. Rahbar, S.; Yernini, K.K.; Scott, S.; Gonzales, N.; Lalezari, I. Biochem. Biophys. Res. Commun., 1999, 262, 651. Rahbar, S.; Yerneni, K.K.; Scott, S.; Gonzales, N.; Lalezari, I. Mol. Cell Biol. Res. Commun., 2000, 3, 360. Figarola, J.L.; Scott, S.; Loera, S.; Tessler, C.; Chu, P.; Weiss, L.; Hardy, J.; Rahbar, S. Diabetologia, 2003, 46 , 1140. Reddy, V.P.; Garrett, M.R.; Perry, G.; Smith, M.A. Sci. Aging Knowledge Environ., 2005, pe12. Hipkiss, A.R.; Michaelis, J.; Syrris, P. FEBS Lett., 1995, 371, 81. Hipkiss, A.R.; Chana, H. Biochem. Biophys. Res. Commun., 1998, 248, 28. Hobart, L.J.; Seibel, I.; Yeargans, G.S.; Seidler, N.W. Life Sci., 2004, 75 , 1379. Guiotto, A.; Calderan, A.; Ruzza, P.; Borin, G. Curr. Med. Chem., 2005, 12 , 2293. Ukeda, H.; Hasegawa, Y.; Harada, Y.; Sawamura, M. Biosci. Biotehnol. Biochem. , 2002, 66 , 36. Babizhayev, M.A.; Sequin, M.C.; Gueyne, J.; Evstigneeva, R.P.; Ageyeva, E.A.; Zheltukhina, G.A. Biochem. J., 1994, 304, 509. Received: February 22, 2007 Revised: April 12, 2007 Accepted: April 13, 2007 [194] [195] [196] [197] [198] [199] [200] [201] [202] [203] [204] [205] [206] [207] 1671 Kang, J.H.; Kim, K.S.; Choi, S.Y.; Kwon, H.Y.; Won, M.H.; Kang, T.C. Mol. Cells, 2002, 13 , 498. Seidler, N.W.; Teargans, G.S.; Morgan, T.G. Arch. Biochem. Biophys., 2004, 427, 110. Szwergold, B.S. Biochem. Biophys. Res. Commun., 2005, 336, 36. Brownson, C.; Hipkiss, A.R. Free Radic. Biol. Med., 2000, 28 , 1564. Yeargans, G.S.; Seidler, N.W. Biochem. Biophys. Res. Commun., 2003, 300, 75. Babizhayev, M.A.; Deyev, A.I.; Yermakova, V.N.; Brikman, I.V.; Bours, J. Drugs R. D., 2004, 5, 125. Miyata, T.; van Ypersele de Strihou, C.; Ueda, Y.; Ichimori, K.; Inagi, R.; Onogi, H.; Ishikawa, N.; Nangaku, M.; Kurokawa, K. J. Am. Soc. Nephrol., 2002, 13, 2478. Forbes, J.M.; Thomas, M.C.; Thorpe, S.R.; Alderson, N.L.; Cooper, M.E. Kidney Int. Suppl., 2004, S105. Shoda, H.; Miyata, S.; Liu, B.F.; Yamada, H.; Ohara T.; Suzuki, K.; Oimomi, M.; Kasuga, M. Endocrinology, 1997, 138, 1886. Webster, J.; Urban, C.; Berbaum, K.; Loske, C.; Alpar, A.; Gartner, U.; De Arriba, S.G.; Arendt, T.; Munch, G. Neurotox. Res., 2005, 7, 95. Oturai, P.S.; Christensen, M.; Rolin, B.; Pedersen, K.E.; Mortensen, S.B.; Boel, E. Metabolism, 2000, 49 , 996. Soulis, T.; Sastra, S.; Thallas, V.; Mortensen, S.B.; Wilken, M.; Clausen, J.T.; Bjerrum, O.J.; Petersen, H.; Lau, J.; Jerums, G.; Boel, E.; Cooper, M.E. Diabetologia, 1999, 42 , 472. Karachialis, N.; Babaei-Jadidi, R.; Kupich, C.; Ahmed, N.; Thornalley, P.J. Ann. N. Y. Acad. Sci., 2005, 1043, 777. Yeboah, F.; Konishi, Y.; Cho, S.J.; Lertvorachon, J.; Kiyota, T.; Tomasz, P. WO 2003032969 (2003); Chem. Abstr. 2003, 138, 314635. Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.