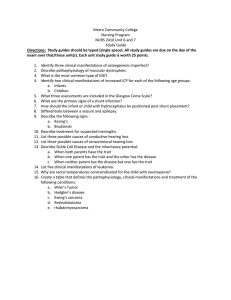
Pathophysiology Final Exam Blueprint: Renal, Immunity, Digestive
advertisement

Basic Pathophysiology Final Exam Blueprint 5/6/2022 Renal 5 Aging and renal function Elders are most prone to getting UTIs - Decrease in renal blood flow and GFR ● Altered sodium and water balance - Number of nephrons decrease due to renal vascular and perfusion changes - Response to acid base changes delayed - Increased risk for drug toxicity - Alterations in thirst and water intake - Why elderly Rennin-angiotensin-aldosterone system: cause for RAAS stimulation - Increased angiotensin II > releases aldosterone (promotes sodium and water retention to increase volume)> vasoconstriction from angiotensin ● ACE inhibitors and ARBs are used to reduced CVD risk and slows progression of CKD ● Drop-in blood pressure or when blood volume is low ● Kidney senses low pressure coming in Renal compensation for fluid loss & ADH - Kidneys are there to balance the amount of fluid when we are overloaded with fluid by drinking excessively we urinate more and when we are dehydrated the urine output is low - Causes the kidney to reabsorb the water and make the volume of urine less - If the pituitary gland releases too much ADH it will cause the kidney to reabsorb too much water making the urine output less when you are retaining water - But if ADH release its not enough like in Diabetes insipidous then the kidney will eliminate excess water because there's no ADH to help reabsorb water and so you tend to be hypovolemic because you’re losing too much water Patient education for clients with renal insufficiency - Sudden decline in kidney function ● Decrease in glomerular filtration ● Decrease in urine output ● Accumulation of nitrogenous waste products in blood - Prerenal ● Most common cause of AKI ● Caused by impaired renal blood flow ● GFR declines because of the decrease in filtration pressure - Intrarenal (intrinsic) ● Most commonly caused by acute tubular necrosis ❖ Postischemic or nephrotoxic ❖ oliguria - Postrenal ● Occurs with urinary tract obstructions that affect the kidneys bilaterally - The kidney cleanses the blood and removes waste when it doesn’t do that waste material will increase in the blood - Tell the patient to be mindful of protein intake because when protein is broken down it produces nitrogenous waste - The amount of sodium because you don’t want any fluid retention - Food that is rich in potassium Immunity/Infection/Inflammation 10 HIV infection; means of transmission; treatment; enzymes found carried within the HIV viral coat - Blood-borne pathogen - Heterosexual activity is most common route worldwide - HIV is transmitted through exchange of body fluids - Retrovirus: composed of RNA - Bodily fluids such as blood, semen, and breast milk - Requirements for HIV transmission from an infected host to an uninfected individual - HIV cannot survive outside the body - HIV targets are CD4- expressing T-lymphocytes and macrophages - CD4 lower than 200=AIDs - Antiretroviral Therapy (ART)- combination of: ● Chemokine receptor inhibitor: CCR5 antagonist prevents viral attachment ● HIV Fusion Inhibitors: Prevents CD4 ● Reverse Transcriptase: nucleoside reverse transcriptase; non-nucleoside reverse ● HIV integrase: inhibits of viral integration into host genome ● HIV protease: inhibits of the proteases HIV uses for assembly of new virus Types of immunity: Humoral and Cellular; manifestations and signs of deficiency Humoral immunity - Antibodies circulating in blood - Bind to antigens on bacteria and viruses - Bacterial infection Cellular immunity - T cells in blood and tissues - Defend against intracellular pathogens and abnormal cells - Becomes cytotoxic when activated Active immunity - Develops after exposure to antigen - Long lived Passive immunity - Preformed antibodies or T cells are administered - Temporary Correct definitions of allergy, autoimmunity, hypersensitivity reaction Allergy- Deleterious effects of hypersensitivity to environmental (exogenous) antigens Autoimmunity- disturbance in the immunologic tolerance of self antigens Alloimmunity- immune reactions to tissues of another individual Immune deficiency- reaction insufficient to protect the host Hypersensitivity- altered immunologic response to an antigen that results in disease or damage to the host - Type I ● IgE mediated (allergy) - Type II ● Tissue-specific reactions - Type III ● Immune complex-mediated - Type IV ● Cell-mediated Inflammation: characteristics; types of exudates Need histamine for inflammation Acute inflammation - Self-limiting - Lasts 8-10 days ● Local manifestations - Result from cellular and vascular changes and corresponding leakage of circulating components into the tissue - Heat, swelling, redness, pain, loss of function - Exudative fluid ❖ Serous exudate (watery) ❖ Fibrinous exudate (thick and clotted) ❖ Purulent exudate (pus) ❖ Hemorrhagic exudate (erythrocytes) - Systemic Manifestations ● Fever ● Caused by exogenous and endogenous pyrogens ● Act directly on the hypothalamus, which controls body’s thermostat - Leukocytosis ● Increased numbers of circulating leukocytes - Increased plasma protein synthesis ● Proteins are either pro or anti-inflammatory called acute phase reactants Chronic inflammation - Initiated if acute proves inadequate - Lasts weeks to months ● Unsuccessful acute inflammatory response - Characterized by pus formation, suppuration, and incomplete wound healing ● Other causes of chronic inflammation: - Microorganisms resistant to acute inflammation - Toxins causing tissue damage Immunoglobulins and common occurrences; occurrence in newborn IgG- transported across the placenta to protect the newborn child IgA- Bodily secretions IgM- largest of the immunoglobulins; first antibody produced during the primary response to an antigen; synthesized early in neonatal life IgE- Allergy IgD- Function as one type of B cell antigen receptor Autoimmunity – SLE; risk factors; pathophysiology of SLE - Most common autoimmune disease - Chronic multisystem inflammatory disease - Autoantibodies against ● Nucleic acids ● Histones ● Ribonucleoproteins ● Other nuclear materials - Symptoms the result of type II or III hypersensitivity reaction - More common in females - Clinical manifestations ● Arthralgias or arthritis ● Vasculitis and rash ● Renal diseases ● Hematologic changes ● Cardiovascular diseases - Manifestations may wax and wane and affect all body systems - Joints so they’ll be pain, attacks the kidney (nephritis) and the lining of the heart (pericarditis), blood, more common in young black women HLA (Human Leucocyte Antigen) impact on tissue transplant Has to be tested before giving a transplant - MHCs (HLAs) are major target - Classified according to time ❖ Hyperacute ● Immediate and rare ❖ Acute ● Days to months ● Cell-mediated immune response ❖ Chronic ● Months or years ● Weak cell-mediated reaction against minor HLA antigens Blood groups and transfusion - ABO blood groups (A,B, AB, O) - Antigens: proteins - Antibodies: protects the body from invaders - Type O is universal - Type AB is the universal recipient - Rh-=- Rh+=+- EBV and mononucleosis - Benign, acute, self-limiting infections of B lymphocytes transmitted by saliva through personal contact - Most common cause is EBV - Other viruses that cause similar symptoms: ● CMV ● Hepatitis ● Influenza ● HIV ● Rubella - Symptoms at time of diagnosis: ● Fever ● Fatigue ● Sore throat ● Swollen cervical lymph nodes ● Increased lymphocyte count ● Atypical (activated) lymphocytes - Serious complications are rare ● Splenic rupture is most common cause of death - Diagnosis ● >50% lymphocytes and at least 10% atypical lymphocytes ● Monospot qualitative test for heterophillic antibodies ● Antibodies for EBV antigens ● EBV is a ubiquitous herpes virus Digestive system 10 Cancers: gastric & colorectal Gastric - Presence of H. Pylori Use of alcohol smoking Colorectal - Ulcerative colitis is a risk factor smoking Crohn’s Disease: pathophysiology ● Granulomatous colitis, ileocolitis, or regional enteritis ● Idiopathic inflammatory disorder; affect any part of the digestive tract, from mouth to anus ● Causes “skip lesions” ● Can involve any part of the GI tract ● Ulcerations can produce fissures that extend into the lymphatics ● Symptoms similar to ulcerative colitis ● Anemia may result from malabsorption of vitamin B12 and folic acid ● Treatment similar to ulcerative colitis ● Lead to diarrhea PUD: Risk factors and patient education A break or ulceration in the protective mucosal lining - Usually in stomach or proximal duodenum - Sometimes in esophagus Acute and chronic ulcers Superficial - erosions Deep Zollinger- Ellison syndrome Duodenal ulcers - Most common of the peptic ulcers - Developmental factors ● H. Pylori ● Use of NSAIDS ● Stress ● Use of alcohol - Characterized by intermittent pain in the epigastric area - Management aimed at relieving the causes - Ingestion of food and antacids help relieve it too Intestinal obstruction: pathophysiology & complications Pairpheration and paraphrinitis - An intestinal obstruction is any condition that prevents the flow of chyme through the intestinal lumen - Simple obstruction ● Mechanical blockage of the lumen - Functional obstruction (paralytic ileus) ● Failure of intestinal motility ● Often occurs after intestinal or abdominal surgery, pancreatitis, or hypokalemia - Signs of small intestinal obstruction ● Colicky pains ● Nausea and vomiting - Signs of the large intestine obstruction ● Hypogastric pain and abdominal distention Ulcerative colitis & complications; impact on hematology ● Chronic inflammatory disease that causes ulceration of the colonic mucosa - Sigmoid colon and rectum - Begins in the rectum and may extend proximally to the entire colon - Intermittent periods of remission and exacerbation ● Symptoms - Diarrhea (10 to 20 days) - Urgency - Bloody stools - cramping ● Treatment is individualized and depends on severity of symptoms and extent of mucosal involvement Hiatal hernia: common symptom - Diaphragmatic hernia with protrusion of the upper part of the stomach through the diaphragm and into the thorax ● Sliding hiatal hernia- most common ● Paraesophageal hernia ● Mixed hiatal hernia - Conservative treatment - Cause reflux so they’ll be epigastric pain and they’ll also be… GERD: pathophysiology and symptoms - Reflux of acid and pepsin from the stomach to the esophagus causes esophagitis - Resting tone of the LES tends to be lower than normal - Conditions that increases abdominal pressure or delay gastric emptying can contribute to the development of reflux esophagitis - Manifestations ● Heartburn ● Acid regurgitation ● Dysphagia ● Chronic cough ● Asthma attacks ● Laryngitis ● Upper abdominal pain within 1 hour of eating - Protein pump inhibitors are the agents of choice for controlling symptoms and healing esophagitis Hepatobiliary system 10 Gall bladder dysfunction (Cholelithiasis) and fat absorption - Gallbladder stone- increases the hypercholesteremia because it is made up of cholesterol - When there is cholelithiasis it blocks bile from getting to the… where it should break down fat so it can be digested - Absorbtion of fat soluble vitamins so the stool will look clear lightly color - Risks ● Obesity ● Middle age ● Female ● Oral contraceptives ● Rapid weight loss ● Native american ancestry ● Genetic predisposition ● Gallbladder, pancreas or ileal disease - Gallstones ● Formed from impaired metabolism of cholesterol, bilirubin, and bile acids ● Types depend on chemical composition - Cholesterol - formed from bile that is supersaturated with cholesterol produced by the liver - pigmented brown - formed from calcium bilirubinate and fatty acid soaps that bind with calcium - black - compsed of calcium bilirubinate with mucin glycoproteins - associated with chronic liver disease and hemolytic disease - often asymptomatic or vague - epigastric and right hypochondrium pain - intolerance to fatty foods ● Cholecystitis - Inflammation of gallbladder or cystic duct - Almost always caused by a gallstone lodged in the cystic duct - Pain is similar to that caused by gallstones - Fever, leukocytosis, rebound tenderness, and abdominal muscle guarding are common findings Portal hypertension and manifestations: esophageal varices and hematemesis - Increase pressure within the liver, which will increase the capillary hydrostatic pressure within the liver forcing fluid out - Abnormally high blood pressure in the portal venous system caused by resistance to portal blood flow ● Intrahepatic ● Posthepatic - Varices - Splenomegaly ● Hepatopulmonary syndrome ● Portopulmonary syndrome - Vomiting of blood from bleeding esophageal varices is the most common clinical manifestation Liver cell damage: clinical manifestations including Jaundice ● Jaundice (icterus) - Caused by hyperbilirubinemia - Obstructive jaundice ● Extrahepatic obstruction - Hemolytic jaundice ● Prehaptic jaundice ● Excessive hemolysis of RBC - Characterized by dark urine, yellow discoloration of sclera and skin, and light colored stools; ascites, hepatic encephalopathy - Viral infection or nonviral - Tylenol (acetaminophen) Cirrhosis: Pathophysiology; Hepatic encephalopathy, ascites - Tissue is fibrotic so it is affecting the blood vessels so it can not do its job - Irreversible inflammatory, fibrotic liver disease - Biliary channels become obstructed and cause portal hypertension - Severity and rate of progression depend on the cause - Many causes ● Ascites - Accumulation of fluid in the peritoneal cavity - Most common cause is cirrhosis - Development associated with ● Portal hypertension ● Decrease synthesis of albumin by the liver ● Splanchinc vasodilation ● Renal sodium and water retention - 25% mortality in 1 year if associated with cirrhosis - Causes abdominal distention and increased abdominal girth and weight gain - Paracentesis ● Hepatic encephalopathy - A neurologic syndrome of impaired behavioral, cognitive, and motor function - Early symptoms ● Subtle changes in personality, memory loss, irritability, disinhibition, lethargy, and sleep disturbances - Later symptoms ● Confusion, disorientation to time and space, flapping tremor of the hands, slow speech, stupor, convulsions and coma Acute Pancreatitis; risk factors - Inflammation of the pancreas - Usually mild and resolves spontaneously - May result from direct cellular injury from alcohol, drugs, or viral infection - Cardinal manifestation is epigastric or midabdominal constant pain Musculoskeletal & Mobility 10 Fractures - types -Complications (ex. Compartment syndrome; muscular atrophy; bleeding) Compartment syndrome - Result of increase pressure within a muscle compartment - Can be caused by any condition that disrupts the vascular supply to an extremity - Muscle ischemia causes edema, rising compartment pressure and tamponade that lead to muscle infarction and neural injury - 6 Ps of compartment syndrome - Volkmann ischemic contracture - Diagnosis confirmed by measurement of intracompartmental pressure Muscular Atrophy - Muscle degeneration and weakness -Serious complication – fat embolism; risk for pulmonary embolism Rheumatoid arthritis: clinical manifestations – swelling, increase in synovial fluid - Inflammatory autoimmune joint disease - Systemic autoimmune damage to connective tissue, primarily in the joints - Similar symptoms to posteoarthritis - Cause unknown; multifactorial with strong genetic predisposition ● Rheumatoid factors - Cartilage damage from three processes ● Neutrophils and other cells in the synovial fluid become activated ● Inflammatory cytokines induce enzymatic breakdown of cartilage and bone ● T cells also interact with synovial fibroblasts, converting synovium into a thick, abnormal layer of granulation tissue - Insidious onset - Systemic manifestations ● Inflammation, fever, fatigue, weakness, anorexia, weight loss, and generalized aching and stiffness ❖ painful , tender, stiff joints ❖ Joint deformities ❖ Rheumatoid nodules - Caplan syndrome ● Diagnosed by presence of autoantibodies ● Early treatment with disease- modifying antirheumatic drugs Osteoarthritis – pathophysiology – loss of cartilage ● Characterized by - Loss and damage of articular cartilage - Inflammation - New bone formation of joint margins - Subchondral bone changes - Variable degrees of mild synovitis - Thickening of the joint capsule ● Prevalence increases with age ● Risk factors - Increased age - Joint trauma, long term mechanical stress - obesity ● Characteristics - Local areas of damage and loss of articular cartilage - New bone formation of joint margins - Subchondral bone changes - Variable degrees of mild synovitis and thickening of the joint capsule ● Manifestations - Pain - Stiffness (diminishes with activity) - Enlargement of the joint - Herbeden and bouchard nodes in hands - Tenderness - Limited motion - Muscle wasting - Partial dislocation - Deformity Gout & renal disease ● Inflammatory response to excessive quantities of uric acids - Blood (hyperuricemia) - Other body fluids, including synovial fluid ● Elevated levels lead to formation of monosodium urate crystals in joints - Cause acute, painful inflammation - Joint damage: gouty arthritis ● Crystals under subcutaneous tissues - Tophi ● Risk factors - Male sex - Increased age - High intake of alcohol, red meat, and fructose ● Manifestations - An increase in serum urate concentration (hyperuricemia) - Recurrent attacks of monoarticular arthritis (inflammation of a single joint) - Deposits of monosodium urate monohydrate (tophi) in and around the joints - Renal disease involving glomerular, tubular, and interstitial tissues and blood vessels - Formation of renal stones ● Clinical stages - Asymptomatic hyperuricemia - Acute gouty arthritis - Tophaceous gout ● Trauma is most common aggravating factors ● Primary symptom is severe pain ● Approximately 50% of the initial attacks occur in the metatarsophalangeal joint of the great toe ● 1000 times more likely to develop renal stones than general population ● Manifestations of acute gouty attack - Severe, pain, especially at night - Hot, red, tender joint - Signs of systemic inflammation Aging & osteoporosis; risk factors – smoking, sedentary lifestyle ● Postmenopausal osteoporosis - Middle aged and older women - Estrogen deficiency and secondary causes - Remodeling imbalance between the activity of osteoclasts and osteoblasts ● Age- related bone loss - Cause unclear - Reduced physical activity is likely a factor - Men have 30% greater bone mass than women ● Men have later involvement with osteoporosis - Manifestations ● Pain and bone deformity because of fracture ● Kyphosis - Endocrine System Hunchback caused by vertebral collapse 20 Diabetes mellitus – Types; management; Complications – DKA, neuropathy, hypoglycemia, HHNK (hyperosmolar hyperglycemic nonketotic syndrome) ● Type 1 DM ● Types - idiopathic type 1 - autoimmune type 1 ● immunologically mediated Beta cell destruction and apoptosis - 80-90% cells lost, insulin synthesis declines, hyperglycemia develops ● Alterations in insulin, amylin, glucagon ● genetic and environmental factors involved ● manifestations result from insulin deficiency - Hyperglycemia - polydipsia - polyuria - polyphagia - weight loss - fatigue - recurrent infections - prolonged wound healing ● Type 2 DM ● insulin resistance and decreased insulin secretion by beta cells ● caused by genetic environmental interaction ● risk factors are family history, age, obesity, hypertension, poor diet, and physical inactivity - diet during pregnancy may increase long term risk for child ● initial insulin resistance - compensatory hyperinsulinemia prevents clinical appearance ● later loss of beta cells causing deficiency of insulin activity ● GI hormones play role in insulin resistance ● manifestations(nonspecific): fatigue, pruritis, recurrent infections, visual changes, or symptoms of neuropathy; often overweight, dyslipidemic, and hypertensive ● Hypoglycemia - sometimes called insulin shock or insulin reaction - Type 1 is more at risk for hypoglycemia than type 2 ● Diabetes Ketoacidosis (DKA) - serious complication related to a deficiency of insulin and an increase in the levels of insulin counterregulatory hormones - DKA is much more common in type 1 DM because insulin is more deficient - kussmaul respirations, postural dizziness, CNS depression, ketonuria ● HHNKS - uncommon but significant complication of type 2 DM - more often in elderly ● neuropathy - damage to nerves due to buildup of fructose and sorbitol Diagnostic tests & monitoring tests ● Elevated glucose - take insulin ● low glucose - do not take insulin ● management - avoid milk and alcohol - high carb, low protein diet - small frequent meals ● monitoring - random blood sugar test - should be <200 mg/dl - Fasting blood sugar test - should be <126 mg/dl Implications of gestational diabetes - Any degree of glucose intolerance with onset of first recognition during pregnancy - hormones that aid the baby’s growth block the mothers insulin causing insulin resistance - management ● medical nutrition therapy ● avoid simple sugars ● injectable insulin if blood glucose control isn’t achieved with diet alone - complications ● enlarged baby ● risk of later developing type 2 DM Thyroid dysfunction in adults and infants; complications ● Hypothyroidism - Decreased function at birth, it is called cretinism. Causes mental retardation in children which reversible if instituted early ● Onset at adolescence and older leads to myxedema ● Weakness, fatigue, weight gain, cold intolerance, constipation and abdominal distention, accumulated fluid in the face; basically everything slows down. Grave’s Disease and clinical manifestations ● Autoimmune disease caused by stimulation of thyroid by autoantibodies against TSH receptor ● Prertibial myxedema ● Tachycardia, angina, CHF Cushing’s disease & infection - Manifestations resulting from chronic excess cortisol, regardless of cause - Excessive anterior pituitary secretion of ACTH - Manifestations ● Weight gain in trunk, facial, cervical areas ● Glucose intolerance and protein wasting Diabetes insipidus & SIADH ● Production of large quantities of dilute urine. Kidney is unable to concentrate urine. May be due to hyposecretion or absence of ADH ● If not controlled will lead to hypovolemia and hypernatremia ● Polyuria 5 to 20L of urine/ 24 hrs osmolality of <100mmol/kg ● Nocturia, dehydration, increased thirst, decreased weight loss, increase heart rate ● Constipation, decreased BP, shock ● Urine with low SG <1.005 urine SIADH - Occurs when ADH secretion continues w/o regard to the serum osmolality ● Fluid retention ● Delusional hyponatremia ● Increased serum hypoosmolality ● Anorxeia, nausea, vomiting ● Abdominal muscle cramps and weakness ● Irritabily, confusion, disorientation and seizures usually due to water intoxication ● No edema is present Parathyroidism and serum calcium level ● hyperparathyroidism - Increased secretion of parathyroid hormone - Classified as: ● Primary- excess secretion of PTH from one or more parathyroid glands ● Secondary- increased in PTH secondary to chronic hypocalcemia ● Tertiary- develops after long period pf hypocalcemia - Hallmark manifestations are hypercalcemia and hypophosphatemia ● hypoparathyroidism - Abnormally low PTH levels - Usually caused by parathyroid damage in thyroid surgery - Manifestations are primarily those of hypocalcemia Primary hyperfunction related to gland enlargement Neurologic, Spinal Cord & Brain Injury/Disorders 10 Parkinson’s disease_ Pathophysiology, risk for fall - Characteristically produces progressive muscle rigidity, akinesia and involuntary tremor. Death may result from complications, such as aspiration pneumonia or other infection - Common crippling disease - Affects men more often than women - A degenerative process that involves the dopaminergic neurons in the substantia nigra… this area plays an important role in the extrapyramidal system, which controls posture and coordination of voluntary motor movements - Normal coordinated movement requires a balance of dopamine and acetylcholine. In parkinson’s disease, dopamine level is low but acetylcholine level is high. Seizure – Pathophysiology & Types - sudden, transient alteration of brain function caused by abnormal excessive discharges of cortical neurons - epilepsy ● disease of recurrent unpredictable seizures - convulsions ● Tonic-clonic (jerky, contract- relax) movements associated with some seizures - stages ● prodromal - when symptoms start to appear prior to the big event (hence the seizure) - depression, anger, issues sleeping, anxiety, GI and urinary issues etc - can start days before a seizure ● Aura - doesn’t happen with all types (Focal seizures or tonic-clonic) - happens at the very beginning - lose conscious - Altered vision or hearing anxiety - weird taste or smell - dizzy unable to speak - happens within seconds or minutes ● Ictus - actual seizure… about 1-3 minutes ● status epilepticus - needs immediate medical treatment to make the seizure stop - continuous seizures state that can occur in all seizures type - accompanied by respiratory distress - patients in danger of hypoxia, hypoglycemia, acidosis and exhaustion ● Post Ictus - after the seizure… recovery - time for the brain to recover - takes hours to days - very tired - confused - headache - injury (tongue, cheek, body) Stroke (CVA): types, most common and most fatal; complications- speech impairment such as dysarthria - Leading cause of disability - Third (females) and fifth (males) leading cause of death in the U.S. - 25% of strokes are recurrent - classified Ischemic stroke ● Transient ischemic attacks (TIAS) - ISCHEMIC event causing neurological dysfunction <1 hour ● Thrombotic stroke - obstruction by thrombus in arteries supplying the brain ● Embolic stroke - thrombus fragments obstructing small brain vessels ● Lacunar strokes - occlusion of single, deep perforating artery of brain ● Hypoperfusion - systemic hypoperfusion decreases blood supply to brain Hemorrhagic stroke ● bleeding occurs in brain tissue or subarachnoid/ subdural spaces ● hypertension is primary cause ● mass of blood causes compressed brain tissue, leading to ischemia, edema, and increased ICP and necrosi Multiple sclerosis - Causes destruction of myelin sheath of neurons of the white matter of the brain and the spinal cord. The damage slows, blocks, or distarts transmission of nerve impulses in affected nerve cells - Manifestation of this condition depend on the extent and site of myelin destruction the disease can progress rapidly disabling the patient by early adulthood or causing death within months of onset, or advance slow. Each flare varies in duration and intensity - Causes ● Etiology unknown ● Autoimmune response to a viral infection ● Environmental or genetic factors - MS is mainly due to axon demyelination which occurs in patches throughout the CNS. this subsequently results in various neurological dysfunction - Diplopia, blurred vision, nystagmus - Burning sensations, pins and needles - Fatigue - Weakness - Signs and symptoms ● Paralysis ● Urinary incontinence ● Changes in bowel movement ● Slurred and poorly articulated speech ● dysphagia Myasthenia gravis - Weakness of skeletal muscle; symptoms are exacerbated by exercise and repeated movement and relieved by drugs that enhance acetylcholine levels. Frequently myasthenia gravis affects muscles of the face, lips, tongue, neck, throat, and any other skeletal muscle group - Exact cause is unknown but possible mechanisms include autoimmune response, ineffective acetylcholine release from nerve terminals, inadequate muscle fiber response to acetylcholine - Causes a failure in transmission of nerve impulses of the neuromuscular junction - Antibodies to the receptor prevent or reduce interaction between the post synaptic membrane receptors and acetycholine - 20-40 years old common in women - Ptosis and diplopia - Skeletal muscle weakness - Lack of fascial expression - When the disease involves the respiratory system, resulting in respiratory failure. Intubation and mechanical ventilation may be needed during emergencies Autonomic dysreflexia a syndrome in which there is a sudden onset of excessively high blood pressure. It is more common in people with spinal cord injuries that involve the thoracic nerves of the spine or above (T6 or above). Cardiovascular System 5 Renal disease and cardiovascular complication Heart failure management and patient education; Manifestations ❖ heart is unable to generate adequate cardiac output ➢ inadequate perfusion of tissues ➢ increased diastolic filling pressure of left ventricle ➢ pulmonary capillary pressures increase Left Heart Failure systolic heart failure Right Heart Failure ❖ inability of right ventricle to - - - ejection fraction less than 40% inability of the heart to generate adequate cardiac output to perfuse tissues stroke volume: contractility, preload, afterload ● disruptions decrease cardiac output ● falling cardiac output ng progressively worsens heart failure manifestations: ● dyspnea, orthopnea, cough of frothy sputum, fatigue, decreased urine output, and edema ● pulmonary edema, hypotension/hypertension, S3 gallop ● diastolic heart failure - pulmonary congestion despite normal stroke volume and cardiac output - major causes include hypertension induced myocardial hypertrophy and myocardial ischemia induced ventricular remodeling - decreased compliance of left ventricle - abnormal diastolic relaxation - manifestations: ➢ dyspnea on exertion, fatigue ➢ pulmonary edema may develop over time, S4 gallop provide adequate blood flow at a normal venous pressure ❖ can result from an increase in left ventricular filling pressure that is reflected back into the pulmonary circulation ❖ most commonly caused by a diffuse hypoxic pulmonary disease Vascular disease: Atherosclerosis and the risk factors - Form of arteriosclerosis - Thickening and hardening caused by accumulation of lipid-laden macrophages in the arterial wall - Plaque development - Risk factors include diabetes, smoking, hyperlipidemia/ dyslipidemia, hypertension, autoimmunity Myocardial infarction and cardiomyopathy ● Manifestations ❖ sudden severe chest pain; may radiate ❖ nausea, vomiting ❖ diaphoresis ❖ dyspnea ● complications ❖ sudden cardiac arrest due to ischemia, left ventricular dysfunction, and electrical instability Cardiomyopathy - a disease of the heart muscle that makes it harder for the heart to pump blood to the rest of the body. Cardiomyopathy can lead to heart failure. The main types of cardiomyopathy include dilated, hypertrophic and restrictive cardiomyopathy. Valvular dysfunction ● mitral valve prolapse syndrome ● acute rheumatic fever and rheumatic heart disease ● infective endocarditis Respiratory system 5 COPD: emphysema, chronic bronchitis COPD: - characterized by persistent airflow limitation - usually progressive - most common chronic lung disease in world - risk factors ❖ tobacco smoke ❖ occupational dusts and chemicals Emphysema: - abnormal permanent enlargement of the gas exchange airways accompanied by destruction of alveolar walls without obvious fibrosis - inherited deficit of a1- antitrypsin - loss of elastic recoil - air trapping - pink puffers Chronic bronchitis: - hypersecretion of mucus and chronic productive cough that lasts for at least 3 months of the year and for at least 2 consecutive years - inspired irritants increase mucus production and the size and number of mucous glands - the mucus is thicker than normal - bronchodilators, expectorants, and chest physical therapy used to treat - blue bloaters Chronic hypoxia & polycythemia - Hypoxia can also result from lung damage due to trauma. Other things can cause hypoxia include: Lung diseases such as chronic obstructive pulmonary disease (COPD), emphysema, bronchitis, pneumonia, and pulmonary edema (fluid in the lungs) Strong pain medicines and other drugs that hold back breathing. - increase production of erythropoietin in the kidney → increase RBC production → polycythemia (excessive RBC) - Cause • hypoxia in individuals in high attitudes, smokers w/ increased CO, and individual w/ chronic obstructive pulmonary disease or coronary heart failure or both Relative polycythemia - Hemoconcentration of blood due to dehydration - Fluid loss results in relative increases of red cell counts and Hgb and Hct values Absolute polycythemia - Primary (PV) - Secondary: increase in erythropoietin as a normal response to chronic hypoxia or an inappropriate response to erythropoietin secreting tumors Polycythemia vera (primary) - Slowly growing blood cancer in which bone marrow makes too many RBCs - WBCs and platelets are also often increased - Manifestations due to increased RC mass and hematocrit - Increased blood volume and viscosity Pulmonary edema & impact on oxygenation - excess fluid in the lungs ARDS - Acute respiratory distress syndrome (ARDS) is a life-threatening lung injury that allows fluid to leak into the lungs. Breathing becomes difficult and oxygen cannot get into the body. Most people who get ARDS are already at the hospital for trauma or illness. - The most common cause of ARDS is sepsis, a serious and widespread infection of the bloodstream. Pneumonia - lower respiratory tract infection - caused by bacteria, viruses, fungi, protozoa, or parasites - types: ❖ community-acquired (CAP) ● Streptococcus pneumoniae ● influenza ❖ Healthcare acquired (HCAP) ❖ Ventilator-associated (VAP) Acid-Base balance 5 Kidney’s role in acid-base balance The kidneys play a major role in the regulation of acid-base balance by - reabsorbing bicarbonate filtered by the glomeruli and excreting titratable acids and ammonia into the urine. Signs and symptoms of fluid overload - weight gain, swelling, shortness of breath and high blood pressure ABG analysis; potassium and hydrogen ion exchange Hematology 5 Anemias Pernicious - A form of vitamin B12 Aplastic Blood-loss Sickle cell A hematopoietic Acute blood lossposthemorrhagic Abnormal hemoglobin on the failure or bone deficiency anemia marrow aplasia with a reduction in that is an the effective autoimmune production of condition where mature cells by the body does the bone marrow not produce causing peripheral enough intrinsic pancytopenia (anemia, factor neutropenia, and - low amount of thrombocytopenia) oxygen going which is a through the deduction or blood and the absence of all three blood cells body suffers type anemia is a normocytic normochromic anemia. Acute blood loss is mainly a loss of intravascular volume, and the effects depend on the rate of hemorrhage that can lead to cardiovascular collapse, shock and death Chronic blood lossanemia occurs if the loss is greater than the replacement capacity of the bone marrow Manifestations: - early symptoms nonspecific and vague - when hemoglobuin a 7-8 g/dl: weakness, fatigue, difficulty walking, paresthesia, loss of appetite, abdominal pain, weight loss, sore tongue Manifestations: classic cardiovascular and respiratory manifestations with thrombocytopenia hemorrhage into tissues, leukopenia an infection rbc (hemoglobulin’s) very sensitive to low amounts of oxygen in the body; change shape - sickle shape, stiff and sticky - RBCs weak, lifespan is 20 days instead of 120 days - homozygous disease; genetic blood disorder - hemoglobulin S - Autosomal recessive disease - cause circulation problems Manifestations: significant blood loss - illness - hyper hemolytic increase death of RBCs - Spleen not working swells, congestions, infection - dactylitis - pain: opioids around clock - anemic: tired - shortness of breath - decreased RBCs Hemolytic Chronic Disease Premature accelerated destruction of erythrocytes, either episodically or continuously - caused by infections, systemic disease, drugs or toxins, liver disease, kidney disease, abnormal immune responses - hereditary: caused by abnormalities of RBC membrane or cytoplamic contents present at birth - increased destruction of RBCs - also called anemia of inflammation - decreased erythropoiesis and impaired iron utilization in chronic disease or inflammation - common in hospitalized patients Results from: decreased erythrocyte life span - suppressed production of erythropoietin - ineffective bone marrow response - altered iron metabolism in macrophages initially normocytic normochromic becomes microcytic hypochromic - treatment is aimed at underlying disorder - if inflammatory/ infectious conditions are not found, patients is screened for malignancies - Renal failure Manifestations: splenomegaly, jaundice, aplastic hemolytic, or megaloblastic crisis can develop with viral infection; with severe disease, bones become deformed and pathologic fractures occur; cardiovascular and respiratory manifestations correspond with severity of anemia Thrombocytopenia - Glycoprotein hormone produced by the liver and kidney which regulates the production of platelets DVT Blood transfusion - Transfusion reaction occurs when person with one blood type receives another TOTAL 100