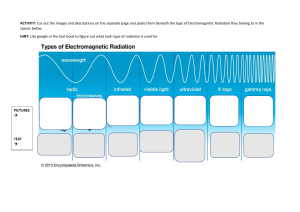
Radiation Emergencies Charles Stewart MD EMDM MPH Fears Media hype 1000’s will die Probably Crap! Cancer Mutations Special interest groups Terrorists Real threats Irradiation Contamination Incorporation Real threats Is the radiation exposure continuing? Irradiated patients pose no threat to the EMS system or the provider. Continued irradiation is a threat to the provider Gamma emitter or x-ray device Establish a safe exposure Real threats Is the patient or scene contaminated Contaminated patients can hurt you Leave the contaminated scene. Don’t bring anything with you. Irradiation The patient has been subjected to a high flux of gamma rays or neutrons This patient is not usually radioactive... An exception occurs with high neutron flux If irradiation continues, a tolerable dose for medical providers must be ascertained Exposure....Irradiation Dose = Duration Distance Defenses (shielding) Contamination A radioactive material is on the skin, tools, or clothes. This radioactive substance requires removal or it will continue to damage tissue. Decontamination Contamination Until the level of contamination is known, it may be wise to isolate contaminated patients. Incorporation Radioactive material is inhaled, ingested, or contaminates an orifice or open wound. The radioactive material can cause extensive cellular damage. Removal of the material may be an interesting problem.... A few definitions Ionizing radiation Electromagnetic radiation that “knocks off” electrons is ionizing This happens at about 100 electron volts Particulate radiation Radiation Alpha radiation A helium nucleus (2 protons, 2 neutrons) Easily stopped because the mass of the particle is so high Radiation Alpha radiation Alpha particles do not penetrate skin If incorporated, alpha particle emitters will cause significant damage Radiation Beta radiation An electron ejected at high speed The charge and energy of the beta particle depends on the nuclear reaction that occurred. Radiation Beta radiation Beta emitters represent both an internal and external threat to the patient (and to you!) Radiation Gamma radiation Exactly like X-rays X-rays - from added external energy Gamma rays - from nuclear decay Follows all laws of physics that pertain to light. Inverse square law Electromagnetic radiation (EMR) decreases with the square of the distance from the source As distance increases by 2, intensity falls off by 4 Neutron radiation Nuclear particles without a charge A product of nuclear fission Make other materials radioactive by capture of the neutron and subsequent decay of the new isotope Protons Nuclear particles with a positive charge A product of nuclear fission Van Allen belt Particle accelerators Not a problem for EMS providers Radiation measurement “Flux measurement” Measures the flux of the moment Geiger counter Scintillation counter Absorbed dose measurement Dosimeters Radiation measurement Dosimeters Film badge Permanent record Fog with temperature and humidity Ionization meter Sensitive to impact Thermoluminescent dosimeter No permanent record A few definitions.... RAD Radiation Absorbed Dose Deposition of 100 ergs of radiation per gram of tissue. A few definitions.... R Roentgen Deposition of 87 ergs of radiation per gram of air. A few definitions.... REM Roentgen Equivalent for Mammals RBE x RAD dose = REM (RBE = Relative Biological Effectiveness). A few definitions.... Banana Equivalent Dose Maximum exposure permitted Over age 18 5 REM / year for each year over 18 150 REM 1 time exposure in lifetime ever. 25 REM 1 time exposure in a year. Radiation bioeffects History Perspective Acute effects Long term effects Acute effects of radiation Localized Skin erythema Whole body Nausea and vomiting Malaise and fatigue Fever Hematologic changes Biological effects n Clinical dosimeters n n n Nausea and vomiting Lymphocyte counts Skin erythema Skin erythema Varies with the type of radiation Akin to sunburn Rapid development may indicate a severe exposure Not a particularly good dosimeter Nausea and vomiting Somewhat dose related Increased dose means quicker onset Absence of nausea implies minimal exposure Severity of symptoms varies immensely Poor correlation with dose Nausea and vomiting Nausea alone @ 5 or more hours - mild exposure Vomiting @ 5 or more hours - mild exposure Vomiting @ 1-5 hours - moderate exposure Vomiting within 1 hour - severe exposure Vomiting within minutes - probably lethal Lymphocyte count Best biological dosimeter < 500 lymphs/cc @ 48 hours is BAD > 1200 lymphs/cc @ 48 hours is good. Lymphocyte count Lymphs/cc @ 48 hours 1500 or more - good prognosis 1000 - 1500 - moderate exposure 500 - 1000 - severe exposure 100 - 500 - very severe exposure less than 100 - uniformly lethal Biological effects n Whole body exposure n n n n Mild exposure Hematopoietic syndrome GI syndrome Neurovascular syndrome Mild exposure Less than 200 rads Symptoms Nausea and vomiting Possible hair loss Prognosis - excellent Use contraception for 6 months Hematopoietic syndrome 200 - 1000 rads Symptoms Nausea and vomiting Diarrhea Pancytopenia Bone marrow suppression Prognosis - good to poor Gastrointestinal syndrome 1000 to 5000 rads Symptoms Intractable nausea and vomiting Bowel necrosis Bone marrow suppression Prognosis - poor Neurovascular syndrome 5000+ rads Symptoms Prodromal nausea and vomiting Rapid onset Listlessness Tremors and ataxia Convulsions Prognosis - hopeless Where can we intervene.... n n Intermediate exposure High level exposure Radiation exposure treatment No acute therapy Some pre-exposure treatment available Radiation injury team concept Protection from infection Control of bleeding Supportive therapy Intermediate Exposure 100 - 400 rads 5-50% death (untreated) Bone marrow suppression Nausea, vomiting and diarrhea Treatment helpful High level exposure 400- 1000 rads Combination of GI and hematologic syndromes Maximum lifesaving effort required About 1 week to arrange the consults Laminar airflow “clean” rooms Marrow transplant Long term effects Cataracts Shortened life span Genetic effects Cancers Leukemia Bone cancer (incorporation) Lung cancer (incorporation) Long term effects Dose related The minimum dose has not been established Lower incidence of disease ?? Lowered resistance to infection Exposure.... Measure the type and amount of the radioactive source. If the source cannot be shielded or removed, then the allowable radiation exposure times must be calculated. Decontamination Starts at the scene Treat patient first Medical therapy Remove contamination Wash patient Decontamination n Contamination can be reduced remarkably by simply removing the clothing Decontamination preparation Disposable equipment Makeshift ambulances Litters and gurneys Nondisposable equipment Cover all equipment with plastic Remove everything you can Don’t use expensive vehicles Decontamination preparation Establish a secured area Controlled access ? Cover with plastic sheeting Showers with a holding tank No “dirt” to leave the area Decontamination agents Soap and water Phosphate detergents Tide EDTA or DPTA Potassium permanganate and sodium bisulfate Establish protocols n n n Train Train Train Treat the patient first Keep in mind that the patient is not radioactive... You have to protect yourself from contamination not from the patient. PROTECT yourself Wear a dosimeter Dosimeters are not protective! They just tell you how much you got. Distance Increasing distance will decrease the dose by a factor calculated by the inverse square law Decontamination Estimates The amount remaining The amount removed Save all fluids/stools/tissues If the patient excretes it, uses it, or loses it... save it. Decontamination Flush... don’t scrub Scrubbing damages the skin May use soap or decontamination solutions Decontaminate highest radiation areas first.... if possible Decontamination May be augmented by... Prevention of uptake Enhancement of excretion Check with your friendly radiation biophysicist for further details! Chelation Blocking Isotope dilution Decontamination Hair Shower Cut Do not shave Decontamination After decontamination.... Bag it. Patient clothing Dressing materials Metal items Tools Label: Radioactive / do not discard Decontamination Staff Shower Fresh clothing Monitor for contamination Special problems Wounds Inhalation Ingestion / splash Wounds Cover with a self-adhesive surgical drape Prevents recurrent contamination Then decontaminate / irrigate Surgical debridement Inhalation Half will be returned to pharynx Do not swallow Save sputum ?? lung lavage Ingestion / splash Irrigate Mouth Eyes Ears ? Genitalia Save the irrigation for analysis Prophylaxis Evacuation from area Agents to decrease uptake Iodine Fluids ?? depends on contaminants Prophylaxis For radioactive iodine contamination a stable isotope of iodine is administered... SSKI For radioactive tritium, a stable isotope of hydrogen is used... water Prophylaxis Chelating agents may be used if the patient has internal contamination with any of the transuranic elements Plutonium, uranium, neptunium, americium.. ect. Exposure protective zones Three Mile Island Worst civilian US disaster No deaths Possibly 1-2 excess cancers over 20 years. The cleanup took 12 years and cost approximately US$973 million Small release of radiation, Equivalent to half the dose you get from an X-ray Fukushima Daini Nuclear Power Plant 4 reactor complex 14 meter tsunami Designed for 10 meters Destroyed ¾ of coolant pumps Grid destroyed Batteries for 8 hours only Fukushima Daini Nuclear Power Plant 6 reactor complex Declared a 20-kilometer (12 mi) restricted zone on April 19, 2011. All six reactors were decommissioned Completely shut down one year later. Chernobyl Nuclear Power Plant Massive explosion Supervisor did not follow checklist for a routine test Massive release of radioactivity 500,000 responders to area 31 Responder deaths China syndrome radioactive ‘lump’ Pripyat evacuated Long term effects Chernobyl Nuclear Power Plant Summary Radiation CAN be dangerous Multiple accidents have resulted in relatively few deaths or excess cancers Media ALWAYS overplays dangers Any Questions?