Mycosis Fungoides Case: Ulcerative Nodules & Fungal Infections
advertisement

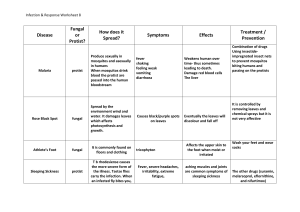
Case report Ulcerative nodules in a 40-year-old farmer with mycosis fungoides: a case report Sharina Macapagal, MD, Ma. Flordeliz Abad-Casintahan, MD, FPDS, FDSP-PDS and Catherine Go-Teodosio, MD, FPDS Jose R. Reyes Memorial Medical Center, Manila, Philippines Correspondence Sharina Macapagal, MD Jose R. Reyes Memorial Medical Center Manila Philippines Email: sharinamacapagal@gmail.com Funding source: None. Conflict of interest: None. doi: 10.1111/ijd.16204 from direct inoculation of the fungus through a break in the skin Introduction integrity. The clinical picture in affected individuals is variable Cutaneous T-cell lymphoma (CTCL) is a malignancy of skin- and can present as papules, nodules, and plaques. Once the homing T-cells. As a result of the loss of the normal T-cell diagnosis is established by histopathology and fungal culture, receptor (TCR) and the disruption of the normal skin barrier, management presents the next challenge as these organisms there is increased susceptibility to opportunistic fungal infec- are often highly resistant to most antifungal agents.5 tions, and mortality often results from infectious complications. The treatment of CTCL becomes a challenge when the disease is complicated with a mixed fungal infection as the latter must Case report be treated before the main problem can be addressed. Mycosis fungoides (MF), a cutaneous T-cell lymphoma, A case of a 40-year-old male is presented, with a 5-year his- impairs both the cutaneous barrier and the immune response. erythematous to hyperpigmented patches on anterior abdomen Patients with this condition are often at high risk for developing evolving to hypopigmented patches accompanied by weight opportunistic infections such as cutaneous aspergillosis and loss and inguinal lymphadenopathy. Findings of clinical and scopulariopsis.1 Aspergillus and Scopulariopsis are found in soil histopathologic examination were compatible with MF, plaque and organic wastes.2–4 Cutaneous deep fungal infection results stage. A skin punch biopsy and fungal culture were done (a) tory of generalized pruritus and diffuse hyperpigmentation with (b) Figure 1 Histopathologic findings of aspergillosis: (a) Acute angle branching hyphae within the granulomatous infiltrate (Periodic acid–Schiff stain, 9100), (b) Phialides with conidia radiating from the entire round surface of the vesicle (wet mount) ª 2022 the International Society of Dermatology. 1 International Journal of Dermatology 2022 2 Case report MF complicated by mixed deep fungal infection (a) (b) (c) (d) (e) (f) (g) (h) (i) (j) (k) (l) (m) (n) (o) Figure 2 Progress with treatment: (a-e) Diffuse xerosis of trunk and extremities with hyperpigmented and hypopigmented patches, ill-defined pink plaques with ulcerations on the face, neck, left axillary area and left hand, and yellow to brown discoloration and hyperkeratosis of nail plates of all the digits, (f-j) Complete response of lesions resulting in hypertrophic scars and ectropion of the left eye after 12 weeks of oral itraconazole 100 mg/tab twice daily, (k-o) Marked improvement of lesions after 4 weeks of amphotericin B 50 mg/vial once daily because of a suspicion of a possible fungal infection and revealed Aspergillus spp. (Fig. 1). The patient has commenced lesions. Hence, the patient was admitted and was started on amphotericin B 50 mg intravenously once a day for 4 weeks on itraconazole 100 mg twice daily. The ulcerations and nod- and showed marked improvement of the lesions (Fig. 2). The ules on the face and neck were completely responsive to medication was well tolerated despite moderate elevation in treatment, with significant residual scarring (Fig. 2). However, creatinine level. With the challenge in clearing the fungal infec- in the sixth month of treatment, there were recrudescent nod- tion as well as renal impairment, chemotherapy for MF was ules on the right and left lateral neck. A biopsy, fungal culture, significantly delayed. and matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) mass spectrometry were done and showed Scopulariopsis spp. (Fig. 3) which was sensitive to ampho- Discussion tericin B, itraconazole, posaconazole, and voriconazole. The As a result of profound immunosuppression and impaired skin patient was referred to the infectious disease specialist for barrier, patients with MF are prone to infectious complications therapeutic with Staphylococcus aureus as the most commonly identified evaluation. Itraconazole 200 mg daily was increased to 400 mg for 1 month with no improvement of International Journal of Dermatology 2022 pathogenic cause.6 ª 2022 the International Society of Dermatology. MF complicated by mixed deep fungal infection (a) Case report (b) Figure 3 Histopathologic findings of scopulariopsis: (a) Long thin septated hyphae with vesicular swellings found near granulomas (Periodic acid–Schiff stain, 9100), (b) Hyaline septate hyphae with brush-like annelides containing chains of conidia (Wet mount) Aspergillosis is the most frequent invasive mold infection in immunocompromised patients.7 For this patient, in particular, his long-term habitation in an orchard with probable exposure to high spore counts,4 frequent incidental cutaneous injuries, and impaired cutaneous barrier in MF were likely risk factors for developing this infection. Acknowledgment The authors thank the investigators who helped in the article: Dr. Deo Adiel F. Wong and Dr. Hester Gail Y. Lim-Bueser. Ethical approval: The Institutional Review Board (IRB) of the hospital approved the research protocol before commencing the study. The Infectious Disease Society of America guidelines specify three groups of antifungal agents for the treatment of aspergillosis, namely triazoles, amphotericin B, and echinocandin. Triazoles are the preferred agents for most patients.5 Amphotericin B is often reserved for use in resource-limited settings in which no alternative agents are available as in the case of our patient. Scopulariopsis is frequently isolated from onychomycosis patients. Cutaneous infection is rare but has been reported.4 Several drug susceptibility studies have shown that the organism is resistant to broad-spectrum antifungal agents including amphotericin B, flucytosine, fluconazole, itraconazole, voriconazole, and terbinafine.6,8,9 Decisions on when to proceed with chemotherapy for MF should involve both infectious disease specialists and hematologists/oncologists, as they must consider the progression of cutaneous infection during treatment versus the risk of death from the underlying malignancy if the treatment is delayed.10,11 In cases such as these, multiple biopsies, fungal cultures, and MALDI-TOF may be needed to establish the etiology of the opportunistic pathogens which can present as multiple coexisting infections in a single patient. Conclusion Treatment of aspergillosis and scopulariopsis remains difficult, especially for immunocompromised patients who need to start chemotherapy because of multiple drug interactions since most antifungal agents are nephrotoxic. Given the high resistance to antifungal agents and its potential to disseminate in immunocompromised hosts, treatment of a secondary opportunistic fungal infection serves as a roadblock to therapy. ª 2022 the International Society of Dermatology. References 1 Tsambiras PE, Patel S, Greene JN, et al. Infectious complications of cutaneous T-cell lymphoma. Cancer Control 2001; 8: 185–188. 2 Kelati A, Gallouj S, Tahiri L, et al. Defining the mimics and clinico-histological diagnosis criteria for mycosis fungoides to minimize misdiagnosis. Int J Women’s Dermatol 2017; 3: 100–106. 3 Bernardeschi C, Foulet F, Ingen-Housz-Oro S, et al. Cutaneous invasive aspergillosis. Medicine 2015; 94: e1018. 4 Liu X, Yang J, Ma W. Primary cutaneous aspergillosis caused by Aspergillus.Fumigatus in an immunocompetent patient. Medicine 2017; 96: e8916. 5 Patterson TF, Thompson GR, Denning DW, et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 2016; 63: e1–e60. 6 Rakita RM, Lease ED, Edelman JD, et al. Successful treatment of Scopulariopsis infection in a lung transplant recipient. Am J Transplant 2015; 15:2010. 7 Paredes K, Capilla J, Mayayo E, et al. Virulence and resistance to antifungal therapies of Scopulariopsis species. Antimicrob Agents Chemother 2016; 60: 2063–2068. 8 Sellier P, Monsuez J-J, Lacroix C, et al. Recurrent subcutaneous infection due to Scopulariopsis brevicaulis in a liver transplant recipient. Clin Infect Dis 2000; 30:820–823. 9 Shaver CM, Castilho JL, Cohen DN, et al. Fatal Scopulariopsis infection in a lung transplant recipient: lessons of organ procurement. Am J Transplant 2014; 14: 2893–2897. 10 Bruynzeel I, Starink TM. Granulomatous skin infection caused by Scopulariopsis brevicaulis. J Am Acad Dermatol 1998; 39: 365–367. zary 11 Kamijo H, Miyagaki T. Mycosis fungoides and Se syndrome: updates and review of current therapy. Curr Treat Options in Oncol 2021; 22: 10. International Journal of Dermatology 2022 3