Foodborne Illness & Public Health: Epidemiology & Outbreak Guide
advertisement

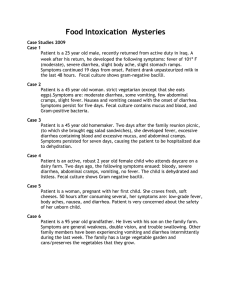
Organism, name of illness, onset time after ingesting, signs/symptoms, duration, food sources Foodborne Illness-Causing Organisms --- Bacillus Cereus- B. cereus food poisoning. 10-16 hrs. Abdominal Cramps, Watery Diarrhea, nausea. 24 -48 Hours. Meats Stews Gravies Vanilla Sauce Campylobacterjejuni - Campylobacteriosis, 2-5 days. Diarrhea, Cramps, Fever, and vomiting. 2-10 days, Raw and undercooked poultry, unpasteurized milk, and contaminated water. Clostridium botulinum - Botulism. 12-72 hours. Vomm, Diarrhea, double vision, Blur Vision, hard swallow, weak, could result in respiratory failure/death. Variable. Bad canned foods, home-canned veggies, fermented fish, Clostridium Perfringens - Perfringens Food Poisoning. 8-16 hrs. Intense abdominal cramps, watery diarrhea. 24 hrs. Meats, poultry, gravy, dried or pre-cooked meals, time/temp abused foods. Baked Potatoes in aluminum foil. Cryptosporidium - Intestinal cryptosporidiosis. 2-10 days. Diarrhea, cramps, slight fever. May relapse over weeks/months. Uncooked food, or food handled by an infected producer after cooking. Contaminated water. Cyclospora cayetanensis - Cyclosporiasis, 1-14 days usually at least 1 week. Diarrhea (watery), loss of appetite, substantial loss of weight, cramps, nausea. Possibly months. Fresh Produce E. coli producing toxin - e. Coli infection (travelers diarrhea). 1-3 days. Watery Diarrhea, Abdominal cramp, some vomiting. 3-7 or more days. Water or food contaminated with human feces. E. coli 0157:H7 - Hemorrhagic colitis. 1-8 days. Bloody diarrhea, abdominal pain, vomit, little to no fever, 4 or younger, can lead to kidney failure. 5-10 days. Undercooked beef, unpasteurized milk/juice, raw fruits/veggies. Hepatitis A - Hepatitis. 28 days on average (15-50 days). Diarrhea, dark urine, flu-like symptoms, fever, headache, abdominal pain. 2 weeks-3 month. Raw produce, shellfish, water. Listeria Monocytogenes - Listeriosis. 9-48 hrs for gastro-intestinal symptoms, 2-6 wks for invasive disease. Fever, Sore, diarrhea, nausea, threat to pregnant. Variable. Milk, soft cheese, ready to eat deli meats, contaminated water. Noroviruses - Viral gastroenteritis. winter diarrhea, food poisoning. 12-48 hours. Nausea, vom (kids), abdominal cramps, dia (adults), fever, headache. 12-16 hrs. Raw produce, contaminated drinking water, uncooked food, food reheated after contact with infected food handler, Shellfish. Clinical Approach Vs. Public Health Approach to Health Care - Clinical Approach - Primary roll is to diagnose and treatment of illness in individuals, preventive medicine. Focus remains on individuals, Public Health Approach - Primary Roll is in control and prevention of disease in populations or groups of individuals. Primary Focus. Emphasis. Paradigm. Organizational Lines of Specialization. Public Health - Populations. Prevention, Health Promotion, Whole Community. Interventions aimed at the environment, Human Behavior, and lifestyle. Analytical (Epidemiology) Setting and population (occupational health), Substantive Health Problems (Nutrition), and skills in assessment, policy development, and Assurance. Clinical Medicine - Individuals. Diagnosis, treatment, whole patient. Medical Care. Organ (Cardiology), Patient Group (Pediatrics), Etiology (oncology, infectious disease), technical skill (Radiology) Public Health Problems Include - Infectious disease, chronic diseases, emergencies, injuries, environmental health problems, other healthy threats. Public Health Approach - Surveillance (what or is there a problem) , Risk Factor Identification (What is the Cause), Intervention Evaluation (what works), Implementation (How do you do it). Clinical Care - Prevention, treatment, and management of illness and the preservation of mental and physical well-being through the services offered by medical and allied health professions (Health Care). Determinant - factor that contributes to the generation of a trait. Epidemic or outbreak - occurrence in a community or region of cases of an illness, specific health-related behavior. Both terms are used interchangeably, however, epidemic usually occurs to a larger geographic. Health Outcome – result of a medical condition. Epidemiology - The study of the distribution and determinants of health related States or events in specified populations, and the application of the study to the control of health problem. Steps in solving health problems - Step 1: Collect Data - Surveillance, determine the time and place and person. Step 2: Assessment - Inference. Step 3: Hypothesis Testing - Determine how and why. Step 4: Actions - Intervention. Epidemiology Terms - Endemic - Present among a population at all times. Outbreak - Localized Epidemic. Epidemic - Large # of people over a large geographic area infected. Pandemic An Epidemic over a very wide are (countries). Cluster - An aggression of cases over a particular period (Birth defects closely grouped together) Sporadic - a disease that occurs infrequently. Risk - The probability an individual will be affected. Rate - # of cases occurring during a specific period. RATE (%) = NUMBER OF CASES / POPULATION AT RISK times 100 Symbiotic relationships between organisms - Normal Flora - Many microbes have a positive symbiotic relationship with other organisms. Mutualism - Both organisms benefit. Commensalism -One organism benefits, the other is not harmed or helped. Parasitism - One organism benefits while the other is harmed. Takes Place when humans are invaded by infectious microbes. A Parasite-Host relationship is created. (Infectious Agent). Fomite - A physical Object that serves to transmit an infectious agent from person to person (Hairbrush with lice). Zoonosis - Infectious disease that is transmitted from animals to humans. Vector - Organisms who allow the infecting agent to thrive. Disease - when the cumulative effects of the infection cause tissue damage Infection - When infectious agents begin to attack Contamination - When a potentially infectious agent exists in the host but has not yet invaded the tissues of the host. Infectivity – refers to the proportion of exposed persons who become infected. Pathogenicity -Refers to the proportion of infected persons who develop clinical disease. Virulence - refers to the proportion of persons with clinical disease who become severely ill or die. How to compare Scientific Method to The Steps in Outbreak Investigation - Obtain background Info, Define a problem, Formulative Hypothesis, Develop a study to test the Hypothesis, Collect data and observations, Evaluate results, Determine of Hypothesis is true/modify - Do lab verification to prove hypothesis, Formulative conclusions, Report results. Steps of an Outbreak Investigation - Step 1: Prepare for field work. Research Supplies and equipment. Follow protocol and contact all parties to determine roles. Step 2: Consider the severity, potential for spread, public concern, and the availability of resources. Find out the expected # of cases for an area. Step 3: Verify a diagnosis. Step 4: Construct a working case definition. 1. Case definition - Establish with The four components or standard criteria for determining who has a disease or condition. A. Clinical Information - about the disease or condition. B. Characteristics - of the affected people. C. Location or Place - as specified as possible as restaurant, country. D. Time sequence - Specific time during which the outbreak occurred. 2. Identification of specific cases - kind and # - count specific cases. A. Confirmed - have diagnosis with case definition plus lab verification. B. Probable - many factors point to diagnosis but may lack lab verification. C. Possible - Some factors point to the diagnosis. 3. LINE LISTING. Step 5: Find cases systematically and record information. Case findings ,ay be done through passive reporting, screening, records review. Should include 1. Identifying Information - A name, address, and telephone # is essential if investigators want to contact patients for additional questions. 2. Demographic Info - Age, Sex, Race, Occupation, etc. 3. Clinical Information - Signs and symptoms. Date of onset is needed to chart the time course of the outbreak. Did death occur? 4. Risk factor info - This info must be tailored to the specific disease in question. (Since food and water are common vehicles in Hepatitis A but not Hepatitis B, exposure to water and foods show the outbreak) 5. Reporter Info - The case report must include the reporter or source of the report. Investigators will sometimes need to contact the reporter to seek more information, or to report back their findings. Step 6: Perform descriptive epidemiology. describe some of the key characteristics of those persons. Incidence Rate = # of new cases of disease during a specific time period / # of people at risk Prevalence (total number of existing cases at a point in time) = Total number of cases (old and new) / # of people at risk Types of epidemic Point source-An epidemic in which all cases are infected at the same time, usually from a single source or exposure. Continuous source-An epidemic in which the causal agent (e.g. polluted drinking water, spoiled food) is infecting people who come into contact with it, over an extended period of time. Person-to-Person(a.k.a. Propagated) -An epidemic in which the causal agent is transmitted from person to person, allowing the epidemic to propagate Path of infection Reservoir: Susceptible Host: Portal of Entry:Portal of exit: