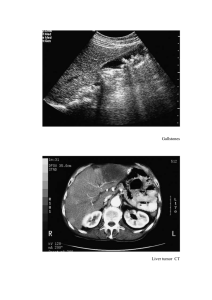
8.1. Liver disease. Methods of radiation examination. To diagnose diseases of the digestive system in children, the entire arsenal of radiation diagnostic methods is used. This is determined by both an extremely wide range of diseases and various possibilities of radiation visualization of different organs. In general, the principles of radiation diagnosis of diseases of the digestive system can be schematically remembered as follows: • to assess the condition of the parenchymal organs (liver, spleen, pancreas) and gallbladder, ultrasound is primarily used; • x-ray methods are more often used to assess the condition of the gastrointestinal tract and esophagus (hollow organs). However, there are many exceptions to these general rules. Indications for radiation examination of the digestive system in children are many, the main of which are: • abdominal pain syndrome; • palpable tumor syndrome; • nausea, vomiting, choking when swallowing; • regurgitation and vomiting syndrome; • disorder of the stool, pathological impurities in the stool; • hepato- and / or splenomegaly; • jaundice syndrome; • decreased appetite, weight loss or poor weight gain; • unmotivated temperature rise. For the purpose of medical examination, the digestive organs in children are examined echographically. Ultrasound screening of the digestive system is not strictly mandatory and may be recommended: • before the start of the visit to the children's institution; • before the start of the visit to the sports section; • in the period of rapid growth (pre- and puberty period); • before planned surgical intervention. The main method of radiation examination of the liver in children's practice is ultrasound. The relatively small size of the child's body and the unexpressed subcutaneous fat layer allow echographically visualizing the liver fundamentally better than is possible in adult practice. Doppler blood flow assessment is widely used, which becomes especially significant in the assessment of portal hypertension. X-ray methods are used infrequently: for example, angiographic methods are used for portal hypertension, CT - for volumetric processes and focal changes. In almost all cases, radiation examination of the liver begins with the use of ultrasound, and the remaining methods are used according to strict individual indications. The main indications for ultrasound of the liver are: • pain in the upper abdomen; • jaundice syndrome; • hepato- (spleen-) megalius; • skin rashes; • violations of the nature of the stool; • nausea, vomiting; • Unmotivated temperature rises . 8.1.1. Normal ultrasound anatomy and variants of the structure of the liver ■■ Normally, the liver is easily visualized from the right hypochondrium, its echogenicity is "average"; it is with the echogenicity of the liver that the echogenicity of other organs of the abdomen is compared. The normal ultrasound anatomy of the child's liver is not fundamentally different from that of an adult. One of the main criteria for the echographic assessment of the liver is its size (see appendix), in all age groups the anteroposterior size of the left lobe is slightly more than half of the right. Clearly the vessels of the liver are visualized already in the Bmode, while due to the location of the vessels of the portal and hepatic systems in different planes, it is impossible to simultaneously visualize them in one scan (Figure 8.1.1.1). Doppler examination of the vessels of the liver in children is technically easier to perform than in adult patients, also due to the small size of the child's body. Normally, the blood flow in the main vessels of the liver is clearly traced. In accordance with the direction of blood flow, the left branch of the portal vein is stained red (to the sensor), and the right one is blue (from the sensor). The type of blood flow in the portal vein and its large branches is usually monophasic, the velocity in the trunk of the portal vein in most children is from 20 to 40 cm / s (Figure 8.1.1.2). In the hepatic veins, the blood flow is different - the so-called W-shaped, i.e. blood moves then to the liver, then from the liver. Therefore, in the mode of color Doppler, the hepatic veins have an inconstant color: according to the phases of the cardiac cycle, the blood flow changes direction and therefore the color from red to blue and vice versa. Blood flow in the hepatic veins becomes monophasic in severe parenchymal liver disease. There are three hepatic veins: left, middle and right. They open into the inferior vena cava very high, in the immediate vicinity of its confluence with the right atrium, which explains the W-shaped type of blood flow in the hepatic veins. Fig. 8.1.1.1. Anatomy of the liver in children: 1 - gallbladder; 2 – portal vienna; 3 - hepatic veins; 4 - inferior vena cava; 5 - abdominal aorta; a - optimal visualization of the right hepatic vein; b - optimal visualization of the left branch of the portal vein; c, g - optimal visualization of the arch of the portal vein in the epigastrium Fig. 8.1.1.2. Vascular anatomy of the liver in children: a, b, c, d - portal vein (trunk outside the scan). The left branch is shown by an arrow, the blood flow in it is directed to the sensor, the flow is colored red, the spectrum is monophasic, located above the isoline (c). In the right branch (double arrow), the blood flow is directed from the sensor, the flow is colored blue, located below the isoline (g); d, e, g, z - hepatic veins. A change in the direction of blood flow and, accordingly, its staining is determined; W-spectrum blood flow (H) An infrequent anatomical variant is an elongated left lobe that extends into the left subdiaphragmatic space and "tongue" envelops the spleen. Such an anatomical variant has diagnostic value in abdominal trauma, since it can echographically resemble a subcapsular hematoma of the spleen. A very rare anatomical variant is an additional lobe of the liver, the atypical location of which determines significant diagnostic difficulties. Such an additional lobe may be almost completely isolated from the main hepatic mass or connected to it by a thin cord (Figure 8.1.1.3). Fig. 8.1.1.3. Atypical location of the liver in children: 1 - additional lobe of the liver; 2 abdominal aorta; 3 - inferior vena cava; 4 - left kidney; 5 - vertebral body: a, b - the elongated left lobe of the liver (dotted line), "tongue" covering the spleen; c, g - additional, extensed lobe of the liver in the epigastrium liver parenchyma ■■ Hepatomegaly in children is very common and accompanies various pathological conditions. Of great importance is the assessment not only of the actual size of the liver, but also of the state of its parenchyma, fragments of hepatic and portal vessels, biliary tract. An isolated increase in the size of the liver can be both an individual feature of the child ahead of the pace of physical development, and the body's reaction to almost any disease, for example, SARS. Diffuse increase in the echogenicity of the liver parenchyma in children is relatively rare and is usually accompanied by an increase in the size of the organ. In young children, such echographic changes can be observed in fetal hepatitis, in older children - with fatty hepatosis. In the latter case, there are also irregularly shaped foci of increased echogenicity in the liver parenchyma (Fig. 8.1.2.1). Diffuse uneven increase in the echogenicity of the liver parenchyma against the background of an increase in its size, it is observed in diseases of accumulation (Gaucher disease, etc.). Fig. 8.1.2.1. Increasing the echogenicity of the liver parenchyma: a - a child of 3 months with galactosemia (arrow shows a clot in the biliary gland bubble); b - a child of 8 years with fatty hepatosis; c - focal changes in alimentary hepatosis. Reactive changes in the liver in children are often accompanied by a pronounced increase in the echogenicity of the walls of the vessels of the portal system, while the liver parenchyma acquires a coarse-stiff character. These are nonspecific changes that can be observed in any diseases with manifestations of intoxication, in intestinal infections (Fig. 8.1.2.2). At the same time, very similar changes are characteristics for chronic hepatitis, metabolic liver diseases, liver fibrosis, reliable pathognomonic echographic symptoms that have not yet been found. In septic conditions, as well as in some specific infections (primarily yersiniosis, mononucleosis), hypoechoic foci of various sizes are determined in the liver parenchyma. In dynamics, the foci either disappear without a trace, or first acquire a hyperechoic center, or are calcified. More often, these foci have a diameter of 3-5 mm and are few. In rare cases, the foci are multiple - "without counting" - and have as low, and increased echogenicity. The formation of large liver abscesses in children is rare and is observed, in particular, in severe appendicular peritonitis (Figure 8.1.2.3). Fig. 8.1.2.2. Diffuse changes in the liver parenchyma in the form of increased echogenicity of the walls of the portal vein (2), hepatic veins (3), gallbladder (1) in children with ARVI with abdominal pain syndrome Fig. 8.1.2.3. Septic foci in the liver: a, b - a child of 2 months with osteomyelitis. Septic foci (arrows) in the liver; b - the same child after 2 weeks against the background of conservative therapy; d - multiple (without counting) hyperechoic foci (fungal sepsis); d, e - abscess of the edge of the liver (dotted line) with appendicular peritonitis in a child of 8 years; f, z - yersiniosis, course. Focus with hyperechoic center (arrow) 8.1.3. Hepatitis ■■■ In childhood, there are various hepatitis, while the scarcity of anamnesis determines significant difficulties in the clinical diagnosis of the disease. Of course, the main diagnostic criteria for hepatitis are the data of laboratory research methods. It is impossible to exclude hepatitis on ultrasound. The only type of hepatitis that has a fairly vivid echographic picture is acute hepatitis A. It should, however, be remembered that its echographically can only be suspected with a high degree of certainty. It is noteworthy that the actual changes in the liver are non-specific and non-demonstrative: moderate hepatomegaly and impoverishment, the "blurriness" of the parenchyma pattern are determined. The most characteristic changes are noted on the part of the gallbladder in the form of a sharp swelling of its walls. In this case, the walls of the bubble acquire a "layered" structure, the wall thickness can reach 10-15 mm or more. The lumen of the bladder is sometimes practically absent. In some cases, the swelling of the walls of the gallbladder reaches such a degree of severity that the bladder may echographically look like a "tumor". In some cases, a zone of decreased echogenicity around the gallbladder is determined - periveral edema. Another typical change is a significant increase in lymph nodes in the liver gate, in the projection of the head and body of the pancreas. Often, such echographic changes are detected in the prodromal period of hepatitis, before the appearance of jaundice syndrome (Fig. 8.1.3.1). Fig. 8.1.3.1. Acute hepatitis A in children: a - liver parenchyma: depletion of intraorgan vascular pattern; b, c, d - different children, gallbladders (dotted line). A sharp thickening of the bladder wall, the lumen is closed; d, e - lymph nodes (arrows) in the gate of the liver, in the projection of the pancreas 8.1.4. Liver cysts of various etiologies ■■ Echinococcal liver cysts in children are currently relatively rare and mainly in endemic areas. Diagnosis of echinococcosis of the liver in children is mainly echographic, but CT and MRI can be used to more accurately determine the relationship of cysts with the bile ducts and large vessels. Depending on the stage of development of the parasite in pain. Fig. 8.1.4.1. Echinococcal liver cyst: a, b - ultrasound determines the huge size of the cyst in the right lobe of the liver, vascular, in its lumen - multiple curved shapes of the structure - exfoliated membranes of the parasite; c similar changes are detected by CT Fig. 8.1.4.2. Calcified echinococcal liver cysts: a - overview radiography; b, c - a cyst with a dense wall is located next to the portal vein; d - same child, different scan: daughter cysts in the lumen; d - CT. The cyst is shown by an arrow The cyst contains suspension, fragments of the exfoliated chitinous membrane, the parasite itself (Figure 8.1.4.1). In such cases, the cyst has a relatively dense and clearly visible membrane. Less often, the cyst is thin-walled with purely liquid contents. Cysts can be single or multiple, can also occur in other organs. This determines the mandatory of a comprehensive radiation examination of a patient with echinococcosis. The X-ray method in the diagnosis of liver cysts is uninformative. The exception is calcified echinococcal cysts. Impregnated with calcium salts, the wall of such a cyst becomes radiopaque. Usually such a radiation picture is characteristic already with the death of the parasite. Echographic evaluation of calcified cysts is difficult: the dense wall is little or impermeable to ultrasound rays, and it is very difficult to assess the condition of the cyst contents (Figure 8.1.4.2). Congenital liver cysts are relatively common, usually diagnosed echographically in children older than 3 years, but can also occur in newborns. Liver cysts in most cases are small, "festoon", are thin-walled. The contents of cysts are more often purely liquid, very rarely - finely dispersed suspension. Sometimes septa are distinguishable in the lumen of the cysts. In rare cases, cysts can reach huge sizes, occupying most of the organ and significantly deforming it (Figure 8.1.4.3). It is noteworthy that even in these cases, subjective complaints in children may not be, laboratory manifestations of hepatic dysfunction are also usually not observed. Fig. 8.1.4.3. Congenital liver cysts: a - a congenital liver cyst with typical edges of a festoon shape; b - liver cyst with a septa in the lumen; b, g - a giant liver cyst in a child of 12 years. The right lobe is almost entirely made by a cyst, the vascular pattern in the preserved parenchyma can be traced reliably Fig. 8.1.4.4. Diaphragm cysts: a, b - a cyst of large sizes, accurate organ differentiation is impossible; b, d - a cyst of medium size; the liver parenchyma "skirts" the cysts (dotted line); e, e - small cyst, analogous echographic changes Often significant diagnostic difficulties are caused by diaphragm cysts. Localized in the costodiaphragmatic angle, they are "pressed" into the liver parenchyma, echographically projected onto the liver and are traditionally mistakenly regarded as liver cysts. The sizes of cysts are often small - rarely larger than 3 cm in diameter, as an exception there are cysts of the diaphragm of large and giant sizes, when a sharp displacement of organs significantly complicates topical diagnosis (Fig. 8.1.4.4). When dynamically observed for several years for cysts of small sizes, in most cases, significant dynamics are not detected. Sometimes these cysts progressively decrease in size. Differential diagnosis is based on knowledge of the typical localization of diaphragm cysts and targeted evaluation of the edges of the cyst: especially when scanning from the back, it is noticeable that the cyst is "indented" Fig. 8.1.4.5. Diaphragm cyst on ultrasound and CT: a, b - diaphragm cyst (arrows) on CT; b, g - cyst of the diaphragm (dotted) "pressed" into the liver parenchyma, scanning from the back. A typical septa in the lumen; e, e - same child, ultrasound from subhepatic access. The cyst of the diaphragm is "pressed" into the liver parenchyma (dotted line) into the liver tissue, but does not emanate from it. It is also possible to use the CT method to assess the mutual arrangement of organs. With CT, it can be reliably seen that the cyst is located outside the liver tissue, especially when examined on the left side (Fig. 8.1.4.5). 8.2. Diseases of the biliary tract ■■■ The main method of radiation examination of the gallbladder and biliary tract (BT) in children is currently ultrasound. In rare cases, if surgical pathology is suspected or present, radiopaque studies of BT are performed: endoscopic retrograde cholecystopancreatography, transvesical contrast of the biliary tract. In recent years, it has become possible to perform magnetic resonance pancreatocholangiography with volumetric reconstruction of BT. Ultrasound examination of BT should be carried out STRICTLY ON AN EMPTY STOMACH (DO NOT EAT ANYTHING, DO NOT DRINK ANYTHING), i.e.: - a newborn with suspected pathology of BT is examined after skipping 1 feeding; - infants (sometimes toddlers) are examined after 6-8 hours of fasting (if ultrasound is scheduled for 10.00 h, you can feed the child with milk formula at night (2.00-3.00); - the rest of the children receive food the night before, in the morning on the day of the study strictly on an empty stomach. The exception is newborns who are given ultrasound screening: in such cases, special training is not provided. Normally, the Gallbladder with ultrasound is visualized reliably in children of any age. Usually it has a pear-shaped, less often - cylindrical shape. Moderate, labile (changing with respiratory movements or with a change in body position) inflection in the cervical region of the LP is a variant of its normal structure. The wall of the gallbladder in children is normally very thin - less than 1 mm. From the BT in a healthy child, only choledoch can be echographically visualized. Its diameter should not exceed half the diameter of the portal vein. The remaining fragments of BT are normally not able to visualize echographically, and it is not possible to reliably judge the architectonics of the BT from ultrasound data. The size of the gallbladder in childhood is very variable. Indicative data are presented in the annex. Thickening of the gallbladder wall to 2 mm and an increase in its echogenicity occurs in children's practice often and is usually interpreted as "reactive changes". The absence of perifocal edema and dispersed suspension in the lumen allows you to exclude acute cholecystitis, and often the changes in the pancreas, stomach and liver parenchyma can be regarded as reactive. They are found in abdominal pain syndrome of almost any etiology, as well as in toxic conditions of various genesis. Thickening and increased echogenicity of the walls of the gallbladder is also found in cholecystolithiasis, anomalies of the BT without acute inflammation at the time of examination. Actually, acute cholecystitis in children is rare and occurs against the background of calculosis of the gallbladder, anomalies in the development of BT. Echographically acute cholecystitis is characterized by a significant thickening of the walls of the gallbladder, edema of perifocal tissues, finely dispersed suspension or sediment in the lumen of the gallbladder (Fig. 8.2.1). Very often in childhood, various variants of deformities of the gallbladder are revealed. Of clinical importance are gross deformities, as well as pronounced S-shaped deformities in the cervical region. With an elongated shape of the cervical region of the gallbladder and a rounded bottom of the gallbladder, there are grounds to echographically suspect siphonopathy. A rare option is a malformation of the gallbladder in the form of multiple septa in the lumen. Such gallbladder are usually small in size, it is not easy to judge their functional state, when conducting choleretic tests, the contraction of such blisters is practically not observed (Fig. 8.2.2). Dispersed suspension in the gallbladder in children is relatively common and can be a consequence of a general serious condition, previous intoxication, observed with prolonged fasting, parenteral nutrition, against the background of tissue decay of any etiology. In general surgical pediatric practice, finely dispersed suspension in the lumen of the gallbladder is often observed in children with appendicular peritonitis, with destructive pneumonia, etc., i.e. is not an independent disease, but reflects the overall severity of the child's condition. Fig. 8.2.1. Changes in the walls of the gallbladder: a - unchanged gallbladder, the walls are practically not differentiated; b - moderately pronounced thickening and increase in echogenicity of the walls of the gallbladder "reactive" in nature; b - acute calculous cholecystitis. Wall thickness of the gallbladder - between the black-white arrows, in the cervical region - fixed calculus (arrow) with a clear acoustic shadow (double arrow) Fig. 8.2.2. Deformities of the gallbladder: a - pronounced inflection in the body; b - pronounced S-shaped deformation in the cervical region; b - multiple kinks in the cervical region, rounded shape of the bottom (siphonopathy); d - multiple septa in the lumen of the bladder Actually cholecystolithiasis in children in recent years is much more common than before and is no longer casuistic rare. Even in infancy. The echographic picture is very characteristic and consists in the detection in the lumen of the bubble of single or multiple echodense inclusions with an acoustic shadow. Usually these inclusions are mobile and move in the lumen of the gallbladder when the position of the child's body changes. Relatively often in childhood, cholecystolithiasis develops in the presence of gross deformities of the gallbladder, intraluminal membranes, etc. In such cases, the stones are fixed. Stones in a disconnected gallbladder look unusual: in the absence of liquid contents in the lumen of the gallbladder, the calculus looks like an echo-dense inclusion in the liver itself. (figure 8.2.3). Fig. 8.2.3. Calculosis of the gallbladder in children: a - single calculus (arrow); b - multiple stones (arrows); b - calculus (arrow) against the background of the intraluminal membrane of the gallbladder; d - calculosis of the disconnected gallbladder (arrow) Stones can be so small that each of them is practically not differentiated as a separate inclusion, and in the pro-light of the gallbladder a coarse sediment is determined. The acoustic shadow of such small stones may not be determined, and with a large number of stones, a single, continuous shadow is formed. Unlike stones, the polyps of the gallbladder are stationary and do not form an acoustic shadow (Fig. 8.2.4). It is very difficult, and sometimes impossible, to differentiate gallbladder polyposis from cholesterosis: in both cases, the formations are fixed to the wall of the bladder, have an average echogenicity, do not form an acoustic shadow and do not shift when the position of the child's body changes. Fig. 8.2.4. Diseases of LP in children: a - polyp of gallbladder in a child of 12 years old; b - multiple (without counting) small stones in the lumen of the gallbladder; b - same child, intraoperative image Among the anomalies of the development of BT, the most frequent option in childhood is the cystic transformation of the choledoch. Usually, the defect is diagnosed in 3-7 years, when the child has periodic complaints of abdominal pain and an ultrasound is performed on him. However, this disease is congenital, and ultrasound diagnosis is possible already in the neonatal period. In a typical case, in the projection of the liver gate, an irregularly rounded thinwalled formation with liquid contents is determined. The diameter of the formation can reach 10 cm or more, but in most cases it is 3-5 cm. Sometimes the cyst has not a rounded, but a cubicshaped or cylindrical shape. There are frequent cases of detection of a cyst of dense inclusions in the lumen, sometimes with an acoustic shadow, which indicates the presence of choledochocystolithiasis. Often, the cystic transformation of the choledoch is combined with a pronounced deformation of the gallbladder in the form of its multiple kinks and atypical location. When the inflammatory process is attached, the walls of the cyst thicken to 3-5 mm, become "layered", echoesymptoms of acute cholecystitis are also determined. There are often changes in the form of dilatation of fragments of the intrahepatic bile ducts, which indicates the presence of biliary obstruction (figure 8.2.5). For the final clarification of the state and architectonics of the BT, endoscopic retrograde cholecystocholangiogram, MRI, less often computed tomography are used. These studies can more accurately than ultrasound determine the condition of undilated fragments of BT, to clarify the structure of the BT. Modern technologies for magnetic resonance cholecystocholangiography or pancreatocholangiography make it possible to carry out a threedimensional reconstruction of dilated fragments of BT, which greatly simplifies the perception of the spatial location of pathologically altered fragments of BT (Fig. 8.2.6). Fig. 8.2.5. Cystic transformation of choledoch in a child of 6 years: 1 - the cyst of the choledoch proper; 2 - the left lobar bile duct; 3 - the right lobe bile duct; 4 - the gallbladder; a - in the gate of the liver, a cystic formation up to 4 cm in diameter is determined; b - pronounced dilatation of the lobe bile ducts, deformation of the gallbladder Fig. 8.2.6. CT and MRI of the same child as in Figure 1 - cystic choledoch; 2 - left lobar duct; 3 right lobar duct; 4 - gallbladder; a - CT: dilatation of intrahepatic fragments of BT; b - MRI, similar changes; c - MRI, volumetric image reconstruction Traditionally, one of the first among the currently existing methods of visualization of BT is intraoperative transvesical cholecystocholangiography. The invasive imaging method has an undoubted advantage in assessing not only the BT, but also the virsung duct, the architectonics of the bile ducts. The difficulty of interpreting the resulting image arises when dilated fragments of BT are superimposed on each other (Fig. 8.2.7). Treatment of cystic transformation of choledoch surgical: perform cholecystectomy, removal of cystically altered common bile duct and formation of bileodigestive anastomosis, more often total - hepaticoejunoanastomosis on the disconnected intestine according to Ru. In the postoperative period, the control of the patency of the anastomosis and the state of the BT is carried out in pediatric practice with the help of ultrasound, when the intestine fixed in the gate of the liver, sewn to the common hepatic duct, is visualized. Relatively often, aerobylia is observed - the flow of air from the intestine into the BT. With significant preoperative dilatation of the lobe bile ducts, a complete reduction in their lumen usually does not occur after surgery, and residual dilation of the BT persists for many years (Fig. 8.2.8). Fig. 8.2.7. Intraoperative transvesical cholecystocholangiography: 1 - cystically modified choledoch; 2 - gallbladder; a - according to the catheter (arrow) installed in the gallbladder, contrasted with BT: the shadow of the gallbladder was superimposed on the shadow of the cystically modified choledoch; a double arrow shows the virsung duct; b - another child: on the catheter (arrow) contrasted BT Fig. 8.2.8. Condition after removal of choledoch cyst, cholecystectomy, imposition of bileodigestive anastomosis: 1 - common hepatic duct; 2 - fragments of the left lobe duct; 3 sutured; a - reliably traced the message between the common hepatic duct and intestine (arrow); b - the same child; dilation of the left lobe duct is preserved; c - the same child after 6 months. Pronounced aerobilia (gas in the lumen of the bile ducts), it is impossible to reliably assess the dilatation of BT during ultrasound 8.3. Diseases of the pancreas ■■■ Diseases of the pancreas are diagnosed in pediatric practice mainly by ultrasound. The organ is located deep in the abdominal cavity, for its optimal visualization it is necessary to carry out some compression on the anterior abdominal wall, and children, especially young children, react negatively to this, so the study is sometimes technically difficult. Only if significant structural changes in the organ are detected on ultrasound, CT scans are performed on children. Anatomically, ultrasound distinguishes 3 parts of the pancreas: the head, body and tail. Normally, in a newborn, the size of these three parts is approximately the same, at an older age, the body becomes significantly thinner than the head and tail. Approximate sizes of organ fragments are given in the appendix. In a newborn, the echogenicity of the parenchyma of the gland is much higher than the echogenicity of the liver, subsequently the echogenicity of the pancreatic parenchyma decreases and only slightly exceeds the echogenicity of the liver parenchyma. The structure of the parenchyma of the gland is homogeneous without inclusions, the virsung duct is not dilated, its lumen is not visualized. Sometimes only its closed walls can be visualized in the form of 2 thin parallel lines. In the projection of the head, the pancreatic part of the choledoch can be visualized (Fig. 8.3.1). Fig. 8.3.1. Ultrasound of unchanged pancreas: a - the pancreas of the newborn (dotted line), all fragments of the same size; b - the pancreas of a child of 9 years (dotted line), the body is much thinner than other fragments; b - virsung duct (arrows) Among the pathological conditions of the pancreas, an increase in its size and diffuse changes in the organ parenchyma with the appearance of "granularity" of the tissue are very common (Fig. 8.3.2). Such changes are non-specific, can occur in many pathological conditions: with intoxication of any genesis, intestinal syndrome of various etiologies, allergic manifestations, skin diseases, helminthic invasion, infectious and inflammatory diseases, chronic constipation, etc. Often such reactive changes are called "reactive pancreatitis", which is fundamentally wrong: pancreatitis is primarily characterized by clinical manifestations, enzymemia, fermenturia. The identified reactive changes are an indication primarily for the clinical and laboratory additional examination of the child, after which the question of the need for the appointment of therapy should be decided. Fig. 8.3.2. Reactive changes in the pancreatic parenchyma In diabetes mellitus, changes in the pancreas are nonspecific. Often, some increase in the size of the gland and its diffuse changes that do not have any specific features are determined. Only with a long-term, severe course of diabetes mellitus in some adolescents there is a decrease in the pancreas in size and a pronounced increase in the echogenicity of the gland parenchyma. Acute pancreatitis in children is rare, there is always a pronounced fermentemia. In the edematous form, a significant increase in the size of the gland is characteristic, sometimes a diffuse decrease in the echogenicity of the parenchyma, an increase in intraorgan vascular pattern. The Virsung duct becomes more noticeable. The absence of perifocal fluid accumulations and effusion in the abdominal cavity is prognostically favorable: fermentemia is usually short-lived, children recover relatively quickly, and the disease itself can be secondary, for example, against the background of a severe intestinal infection (Fig. 8.3.3). The pseudotumorous form of acute pancreatitis is extremely rare in childhood. With this form of the disease, a fragment of the pancreas (more often the head) is sharply enlarged in size, its contours may be uneven and really resemble a volumetric formation (Fig. 8.3.4). A moderate amount of free fluid is determined in the pelvic cavity. A few days after the start of treatment, moderate dilatation is possible as the acute inflammation subsides. Moderate dilatation is possible as the acute inflammation subsides. Virsungov duct. Fig. 8.3.3. Acute pancreatitis in a child of 18 months with hemolytic-uremic syndrome. Gland size: head - 22 mm, body - 18 mm, tail - 21 mm: a - a significant increase in the size and decrease in the echogenicity of the gland parenchyma; b - strengthening of intraorgan vascular pattern; b - underlined virsung duct (arrow) Fig. 8.3.4. Pseudotumorous form of acute pancreatitis in a boy of 12 years old. The contours of the pancreas are shown on the dotted line The destructive form of acute pancreatitis sometimes develops against the background of anomalies in the development of BT, calculosis of the gallbladder and is combined with echographic signs of acute cholecystitis. Characterized by a significant increase in the size of the pancreas, an uneven increase in its echogenicity; against this background, foci of decreased echogenicity (zones of tissue autolysis) are detected. In most cases, there is swelling of the tissue near the pancreas, liquid contents in the pelvic cavity. Moderate stasis of the contents in the lumen of the dilated duodenum is possible. With a favorable current against the background of massive conservative therapy, these changes disappear relatively quickly (2 weeks). In the most severe cases, the accumulation of pathological contents in the cavity of the small omentum is possible, which may require surgical treatment (Fig. 8.3.5). Fig. 8.3.5. Acute destructive pancreatitis in children: 12-p.k. - duodenum; 1 - cavity of the small omentum; 2 - liquid contents retrovesical; 3 - bladder; a, b - a child of 4 years. In the parenchyma of the enlarged pancreas (dotted line), a site of decreased echogenicity is determined, the duodenum is moderately dilated; b - a child of 12 years with acute pancreatitis. On the 4th day of the disease, an increase in the pancreas (dotted line), an uneven decrease in the echogenicity of the parenchyma and a pronounced paraorgan edema (arrows) are determined; d - the same child, on the 14th day of the disease, a defect in the parenchyma of the gland (arrow) and a paraorgan edema (double arrow) are clearly visible; d - after another 4 days in the cavity of the small omentum a significant amount of liquid contents in the cavity of the small omentum, the defect of the parenchyma persists (arrow); e - liquid contents retrovesically Chronic pancreatitis is even more rare and is observed mainly in adolescents. Characterized by an uneven increase in the pancreas, unevenness of its contours, pronounced unequal increase in the echogenicity of the gland parenchyma and dilatation of the Virsungov duct. The latter can be traced fragmentarily or almost throughout. Sometimes the Virsung duct acquires a convoluted character. A decrease in the size of the pancreas against the background of gross changes in the structure of the parenchyma is a prognostically very serious sign (Fig. 8.3.6). Fig. 8.3.6. Chronic pancreatitis: 1 - bladder; 2 - liquid contents retrovesically; a, b, c - a child of 12 years (arrows - virsungov duct); g, d, e - child 14 years old. Virsung duct (arrow) is sharply convoluted, dilated, the size of the pancreas is reduced, the parenchyma with a pronounced increase in echogenicity Fig. 8.3.7. Pancreatic abscess in a child with hemolytic-uremic syndrome: against the background of a sharp increase in the size of the pancreas (dotted line) in its head, a large abscess is determined, up to 3 cm in diameter (between the arrows) Fig. 8.3.8. Tumor lesions of the pancreas in children: a, b, c - hypervascularized volumetric formation of the pancreas (dotted) in a child 6 years old with tuberous sclerosis; g, d - massive metastatic lesion of the pancreas (dotted line) in a child with lymphosarcoma Pancreatic abscess in children is very rare. In the projection of the organ, an irregularly rounded formation with formed walls and hypoechoic heterogeneous contents in the lumen is determined. There is no vascular pattern in the formation. With an abscess of the pancreatic head, a violation of the patency of the duodenum, its dilatation and the presence of stagnant contents in it are often noted (Fig. 8.3.7). Volumetric formations and cysts of the pancreas in childhood are rare. Actually, tumor lesions of the pancreas in children are practically not found, volumetric formations of the pancreas are known in tuberous scleros. Metastatic lesions of the gland are also very rare. The pancreas is unevenly enlarged in size, the vascular pattern can be enhanced (Fig. 8.3.8). Cysts of the subventricular gland are more often of a post-traumatic nature, as a rare option - with polycystic disease. 8.4. Pathology of the spleen■■■ Most often, the pathology of the spleen is diagnosed by ultrasound. Typically formed and localized in the left hypochondrium, the organ is easily visualized; in a standard study, the length and thickness of the organ is measured. Approximate age norms of the size of the spleen are given in the appendix. The atypical position of the spleen is rare. Displacement of the organ into the chest cavity is observed with left-sided false diaphragmatic hernia. Also, atypical location and shape of the organ can occur with embryonic hernia and gastroschisis. A change in the shape and structure of the organ in the form of additional lobules is often observed. Usually, additional lobules are located in the gate of the organ or at the poluses. There may be both single and multiple additional lobules. They have no independent clinical significance. In rare cases, the entire spleen has a fragmented, lobed structure (Figure 8.4.1). The absence of a spleen (asplia) occurs more often as an integral part of syndromic pathology. Fig. 8.4.1. Atypical structure of the spleen: a, b - additional lobule of the spleen (italics) in the gate of the organ; b, d - large additional lobe (italics); e, e - spleen in the form of two fragments An increase in the size of the spleen without structural changes in its parenchyma is often found against the background of a variety of diseases. Moderate splenomegaly is observed in any diseases with intoxication syndrome, in childhood infections. Pronounced spleen nomegaly with displacement and deformation of internal organs can occur in diseases of accumulation, portal hypertension, hematological diseases. With critically pronounced splenomegaly in children with systemic and hematological diseases, cases of spontaneous rupture and infarction of the organ are known (Fig. 8.4.2). Spleen infarction on ultrasound looks like a triangular-shaped hypoechoic avascular focus located along the periphery of the organ, while the top of the triangle faces the gate of the organ, and the base - along the contour of the organ. With spontaneous ruptures of the organ, which are usually in the nature of subcapsular, irregularly shaped, sometimes confluent, hypoanechoic foci of various sizes, are determined in the parenchyma of the organ. Fig. 8.4.2. Splenomegaly in children: a, b - spleen in portal hypertension. The size of the organ exceeds the scanning zone; b, g - pronounced splenomegaly (187 * 83 mm) in a 4-year-old child with hematological disease. Spleen infarction (dotted line); d, e - spontaneous subcapsular rupture of the spleen in a child of 2 years with cytomegalovirus infection. Spleen dimensions approx. 22(M05 mm) Focal changes in the structure of the spleen are observed relatively often in infectious diseases, toxic conditions and are usually accompanied by splenomegaly. Multiple (without counting) small-point hypoechoic foci in all parts of the parenchyma are observed in infectious and inflammatory diseases and are a nonspecific sign. Against the background of treatment, these foci disappear without a trace. Small single (rarely more than 10) hypoechoic foci of 3-7 mm in diameter more often appear with specific infections (yersiniosis, mononucleosis). Against the background of treatment, such foci can either disappear without a trace, or calcifications can form from them in the spleen parenchyma, which persist for many years (Fig. 8.4.3). Fig. 8.4.3. Changes in the spleen in infectious diseases: a, b - spleen and its fragment in severe appendicular peritonitis; b - spleen in yersiniosis; d - spleen in mononucleosis (the focus is shown by a dotted line); d, e - single and multiple calcifications after infectious diseases Spleen cysts are infrequent. In most cases, these are small, rounded-shaped single inclusions that tend to spontaneously disappear. larger cysts often have festoon-like edges, spontaneous regression of a large cyst usually does not occur. (figure 8.4.4). Fig. 8.4.4. Spleen cysts: a, b - small size of the spleen cyst (arrow) in a newborn; b, d - medium-sized spleen cyst in a child of 8 years; d, e - a large cyst of the spleen in a child of 11 years In rare cases, spleen cysts can reach gigantic sizes. In this case, there is a sharp deformation of the spleen itself, a pronounced displacement of other abdominal organs, there may be significant difficulties with the differentiation of the organ affiliation of the cyst. In such cases, the entire arsenal of radiation diagnostic methods using X-ray, radiopaque techniques, CT, MRI (Fig. 8.4.5) is used. Fig. 8.4.5. Giant cyst of the spleen in a girl of 14 years: a - overview radiograph: massive darkening in the upper abdomen, the loops of the intestine are pushed down; b - on irrigography, the displacement of the colon is determined; c - MRI: the huge size of the cyst along which the spleen tissue is spread; g - ultrasound: a huge cyst of the spleen (spleen tissue is spread out on the cyst, circled with a dotted line), deforming the spleen; the left kidney is deformed and pushed back; e - the cyst is removed into the surgical wound, the contents are partially removed; e - the cyst is opened. Its volume was about 4 liters. 8.5. Portal hypertension Portal hypertension (PH) in children occurs infrequently, but is one of the most serious diseases, the accurate radiation diagnosis of which determines both the tactics (including surgical) of patient management and the possible prognosis of the disease. Suprahepatic PH in connection with Budd-Chiari syndrome or disease in children is extremely rare. The bulk of patients with PH are children with a hepatic form that has developed against the background of severe parenchymal liver lesions (hepatitis of various genesis, including fetal with an outcome in cirrhosis of the liver) and a subhepatic form that develops with cavernous transformation of the portal vein. It is this last option that is the most promising regarding the possibility of surgical correction of the defect, and the relative safety of the functional state of the liver makes the long-term prognosis of the disease of such patients favorable. The main radiation method for diagnosing PH is currently ultrasound with Doppler assessment of portal blood flow. Before the advent of this method, angiography was often used. Both before and currently, splendid and / or mesenteric portography is used, which is performed in most cases intraoperatively to clarify the angioarchitectonics of the portal bed. 8.5.1. Portal hypertension against the background of diffuse liver diseases (hepatic form of portal hypertension) ■■ Diffuse liver diseases leading to the development of PH syndrome are diverse. A significant proportion are children with fetal hepatitis. At the same time, an increase in the size of the liver, a diffuse increase in the echogenicity of its parenchyma, and often a reduced gallbladder with thickened walls and inclusions in the lumen (Figure 8.5.1.1) are characteristic. Usually, PH develops in children with severe fetal hepatitis over the age of 3 months. For PH syndrome in children against the background of diffuse liver diseases, the attachment of ascites is characteristic, pronounced in terminal stages of the disease. The amount of fluid in the abdominal cavity in adolescents can reach several liters. In the color Doppler mode, you can fix the movement of free fluid in the abdominal cavity. Fluid is defined as anechoic contents, first of all it accumulates and is visualized in the pelvic cavity, then in the lateral canals, with a further increase in the number - under the domes of the diaphragm and above the loops of the intestine (Figure 8.5.1.2). An accurate echographic estimate of the amount of fluid in the abdominal cavity is impossible, but there is a scheme that allows you to approximately estimate its amount: • in the presence of fluid only in the cavity of the small pelvis, its amount is less than 8 ml / g of the patient's body weight; • in the presence of fluid in the pelvic cavity and in the lateral canals of the abdominal cavity, the amount of fluid leaves from 8 to 24 ml / kg of body weight; • in the presence of fluid in all parts of the abdominal cavity, its amount exceeds 24 ml / kg of the patient's body weight. Fig. 8.5.1.1. Fetal hepatitis in infants: a - against the background of an increase in the size of the liver and an increase in the echogenicity of the parenchyma in the lumen of the gallbladder, a clot (arrow) is determined; b swelling of the perifocal tissues around the gallbladder (arrows) with similar changes in the liver parenchyma in another child; b - another child, a dense sediment in the lumen of the gallbladder (arrows). Hepatomegaly and a significant increase in the echogenicity of the liver parenchyma Chronic hepatitis in remission has practically no specific echographic signs. The size of the liver remains within normal limits or there is a small hepatomegaly. It is possible to increase the echogenicity of the walls of the vessels of the portal system. Sometimes the "coarse-grained" structure of the parenchyma is noted, but the last sign depends to a great extent on the quality of the equipment used and cannot always be considered diagnostically significant. Fig. 8.5.1.2. Ascites in PH on the background of the terminal stage of fetal hepatitis: a - ascitic fluid around the left lobe of the liver; b - ascitic fluid in the lateral canal (arrows - intestinal loops); b - ascitic fluid around the spleen; d - ascitic fluid above the surface of the liver (arrow - sickle ligament); e - appearance of the child Cirrhosis of the liver in children is rare, reliable echographic diagnosis of this disease is often impossible: the development of large foci of regeneration is uncharacteristic for childhood, and small foci can be difficult to fix. Sometimes they are echographically distinguishable only by the ventral surface of the liver. Typical is a change in the shape of the edge of the liver - it becomes rounded. The size of the liver is usually slightly increased, and in the later stages - reduced (figure 8.5.1.3). Fig. 8.5.1.3. Cirrhosis of the liver in children: a, b - a child of 11 years with morphologically confirmed cirrhosis of the liver of unclear etiology, small regeneration nodes along the ventral surface of the liver (arrows), the edge of the liver is rounded (double arrow); c, d - a large focus of regeneration (arrows) in a child of 15 years Congenital fibrosis of the liver has a fairly specific echographic picture, but these changes are detected reliably only in the later stages of the disease. The coarse-hard structure of the liver parenchyma, confluent foci of increased echogenicity of the parenchyma, located mainly in the peripheral parts of the organ, are determined. Pronounced changes in periportal tissues are also characteristic in the form of a significantly extended increase in echogenicity (Figure 8.5.1.4). Fig. 8.5.1.4. Congenital liver fibrosis: a, b - sudden changes in the structure of the liver; c recanalization of the umbilical vein (arrow) In the presence of small cystic inclusions in the parenchyma, cystofibrosis can be judged. Cysts can be located both in all parts of the liver parenchyma and in its individual segments, be single or multiple (Figure 8.5.1.5). The size of the cysts is usually small (2-7 mm). In addition to the presence of cysts, changes in the liver parenchyma are reduced to an increase in the echogenicity of the parenchyma, especially the periportal zone, and the coarse-grained structure of the parenchyma. The disease is an integral part of polycystic disease, in which cysts occur in the kidneys, much less often - in the spleen and pancreas. In some cases, cysts in the kidneys appear several years earlier than in the liver. The prognosis of the disease depends on the predominant progression of organ failure. Diseases of accumulation, primarily Gaucher disease, are characterized by pronounced hepatomegaly and diffuse increase of echogenicity of the liver parenchyma. Sometimes the parenchyma looks heterogeneous with inclusions of increased density of small sizes (Figure 8.5.1.6). The vascular pattern of the liver parenchyma is significantly impoverished. In rare cases, it is possible to isolate relatively specific echoesymptoms; thus, for Wilson-Konovalov's disease (violation of copper metabolism) against the background of a diffuse-heterogeneous increase in echogenicity and "heaviness" of the parenchymal pattern, the appearance of small, rounded hypoechoic foci is characteristic. Rice. 8.5.1.5. Polycystic disease: a, b, c - a child of 5 years, gross structural changes in the liver parenchyma, cysts (arrow) are clearly visible only when scanned with a high-frequency sensor (b). The kidney parenchyma (dotted, c) contains a large number (without counting) of point cysts; g, d, e - a child of 3 months, single small cysts (arrows in the liver parenchyma, cysts are not visible in the superficial layers of the organ (d). In the kidney parenchyma (e - a fragment of the organ) multiple cysts Rice. 8.5.1.6. Gaucher disease in a 6-year-old child: a, b - diffuse-heterogeneous increase in the echogenicity of the liver parenchyma; b - the blood flow in the hepatic veins is close to monophasic, which indicates severe parenchymal liver damage The development of PH syndrome is always accompanied by the appearance of splenomegaly. It is the increase in the size of the spleen that is often the first reason for examining the child and performing an ultrasound. The parameters of the splenic blood flow change. Normally, the blood flow in the splenic vein has a monophasic character, i.e. its speed is constant throughout the entire cardiac cycle. With PH, a propulsive type of blood flow appears in the splenic vein, i.e. its speed changes and the curve takes on a "pulsating" appearance. In the most severe cases, reverse blood flow is observed in the splenic vein, i.e. the blood in it moves not from the spleen, but into the spleen, respectively, with a Doppler color study, the vein will also be colored red, like the artery running next to it (Fig. 8.5.1.7 g). It is also characterized by an increase in peripheral resistance in the splenic artery. If the normal RI of blood flow in the splenic artery is about 0.6-0.7, then with PH this indicator rises to 0.85 or more, in critical cases it reaches 1.0 (Figure 8.5.1.7). Rice. 8.5.1.7. Spleen in PH: a - pronounced splenomegaly, the left kidney is pushed back and deformed; b, c - pronounced tortuosity of the splenic vein (arrow); g - reverse blood flow in the splenic vein (arrow, artery – double arrow); e - propulsive blood flow in the splenic vein; e - reverse blood flow in the splenic vein; g - a sharp increase in RI to 1.0 in the splenic artery (the norm is about 0.6-0.7); z - varicose veins in the stomach wall In rare cases, children develop large spontaneous splenoretroperitoneal shunts. They have a different localization and shape, the diameter can reach 5-9 mm. Large spontaneous spleonretroperitoneal shunts usually provide a fairly good discharge of portal blood into the systemic circulation; massive varicose veins of the esophagus and stomach in these children often does not happen (Fig. 8.5.1.8). In the later stages of the disease, recanalization of the umbilical vein appears, in which hepatofugal ("from the liver") blood flow is fixed. The umbilical vein can have both linear and convoluted course, diameter reaches 10 mm or more in adolescents. It is not difficult to trace the course of the umbilical vein already under the skin of the anterior abdominal wall (Figure 8.5.1.9). A massive discharge of blood through the umbilical vein is a mechanism for compensating for increased pressure in the portal system; in such children, bleeding from the veins of the esophagus and stomach usually does not occur. The size of the liver in the terminal stage of the disease decreases. Fig. 8.5.1.8. Large spontaneous shunts in portal hypertension: a - large splenoretroperitoneal shunt of linear shape; b - spontaneous splenorenal shunt in the gate of the spleen; c splenoretroperitoneal convoluted shunts In isolated cases, in addition to recanalization of the umbilical vein, the development of large intrahepatic portosystemic veno-venous shunts occurs. Such shunts are characterized by a high-speed turbulent flow of blood, which is directed from the portal system to the system of the hepatic veins and further to the inferior vena cava. They are visualized as a tubular form of the structure of low echogenicity, better defined in the mode of color Doppler (Fig. 8.5.1.10). According to the high-speed turbulent nature of the blood flow in the shunt in the color Doppler mode, the shunt has a multi-colored bright color. Fig. 8.5.1.9. Recanalization of the umbilical vein in PH: a - type of patient: dilated veins in the navel; b, c - recanalization of the umbilical vein in the thickness of the liver (arrow); d, d umbilical vein throughout, under the skin of the anterior abdominal wall; e - liver parenchyma, the walls of the branches of the portal vein are sharply compacted; zh, z - distal part of the umbilical vein in the thickness of the liver, the direction of blood flow - to the sensor (i.e. from the liver) - the flow is colored red; and - with pulsed Dopplerography in umbilical vein is determined by venous hepatofugal (from the liver) blood flow Fig. 8.5.1.10. Intrahepatic portosystemic shunt in a child 6 years old with cirrhosis of the liver: a - the edge of the liver is rounded, the contour is uneven; b - in the left lobe of the liver, moderately dilated left branch of the portal vein and the left hepatic vein are visualized; b - the high-speed turbulent flow in the left hepatic vein and in the shunt between it and the portal vein is determined; g - multidirectional blood flow at the junction of the vessels; d - turbulent high-speed blood flow in the left renal vein, the direction of blood flow - from the portal vein; e, f, z, and, k - throughout the entire cardiac cycle in the shunt high-speed turbulent blood flow 8.5.2. Subhepatic portal hypertension I ■■■ The subhepatic form of PH develops due to a block of portal blood flow at the level of the trunk of the portal vein, which is absent in such children, and in its place there is a cavernoma - a conglomerate of convoluted vessels. The size of the cavernoma is different, can reach 6x4 cm.The diameter of individual fragments of vessels is usually 3-4 mm, rarely - up to 6 mm. In some cases, the cavernoma can spread to the region of the head of the pancreas, while in the projection of its head, multiple abnormally convoluted anechoic inclusions with a venous type of blood flow are determined during the Doppler study. For PH against the background of cavernous transformation of the portal vein, significant changes in the walls of the gallbladder are also characteristic: they are sharply thickened - up to 7-10 mm, the bladder often has an irregular shape with multiple deformities. In rare cases, multiple venous vessels - portoportal anastomoses - can be differentiated in the walls of the bladder (Figure 8.5.2.1). Typical are the thickening of the small omentum and the appearance of multiple vessels in it. In the event of PH against the background of cavernous transformation of the portal vein, as with PG against the background of diffuse liver damage, splenomegaly, tortuosity of the splenic vein and changes in splenic hemodynamics in the form of propulsive blood flow in the splenic vein and high-resistive in the artery are characteristic. Of fundamental importance are the diameter of the splenic vein and its "surgical length", since this determines the possibility of portosystem splenorenal bypass grafting. Normally, the diameter of the splenic vein in children 3-5 years old is 3-5 mm, by the age of 10 - 6-8 mm. Rice. 8.5.2.1. Polyorganic changes in portal hypertension: a, b - cavernoma (dotted line) in the liver gate, the walls of the LP are significantly thickened (between the arrows); b, g - cavernoma in the liver gate (dotted line), a sharp deformation of the gallbladder; d, e - portoportal anastomoses in the wall of the gallbladder (arrows); f, z - venous vessels in the head of the pancreas (arrows) The most formidable manifestation of PH in children is acute bleeding from the dilated veins of the esophagus and stomach. At the same time, varicose veins of the esophagus and stomach are very rarely seen during ultrasound, endoscopy is used to establish its presence and severity; these changes are also visible on X-ray examination - spleen or mesenterocoportography. Splenoportography is performed more often intraoperatively for the final decision on the type of anastomosis. Sufficient length and width of the splenic vein make it possible to use this vessel. In addition, the presence of a discharge of a contrast agent through the veins of the esophagus and stomach is evaluated. In the absence of a surgically sufficient trunk of the splenic vein, mesenteric portography is performed: contrast is injected into the superior mesenteric vein; both the actual anatomy of the vessel and the presence of a discharge of blood into the systemic circulation through the veins of the esophagus and stomach are observed (Fig. 8.5.2.2). Rice. 8.5.2.2. Splenoportography and mesentericoportography a - splenoportography: a contrast agent is injected into the lower pole of the spleen, the trunk of the splenic vein (arrow) is contrasted, the cavernoma is visualized, a massive discharge of contrast through the varicose veins of the stomach and esophagus; b - by splenoportography, no splenic vein trunk suitable for splenorenal shunting was found. With mesenteric portography by injecting contrast into the superior mesenteric vein (arrow), its surgical length is sufficient for surgery 8.7.1. Structural features and liver diseases and biliary tract in newborns ■■■ Indications for radiation examination of the liver in newborns are: - jaundice syndrome - hepato-(spleen-) megalius; - regurgitation and vomiting syndrome; - stool disorders; - hyperthermia; - melena; - and more. The main method of radiation diagnosis of pathology of the liver and biliary tract in newborns is ultrasound. Preparation for the study - a state strictly on an empty stomach (skipping one feeding). Basically, the structure of the liver in an infant is the same as in children of other age groups. The vascular system of the liver has fundamental features associated with the transient preservation of the fetal pathways of blood flow. The vessels of the liver already in newborns are visualized clearly. In the first 3 days of life, the patency of the umbilical vein, flowing into the left branch of the portal vein, is preserved. With deep breathing or with the cry of a child, parietal blood flow is often traced in it (Figure 8.7.1.1). Fig. 8.7.1.1. Anatomy of the portal and umbilical vein in newborns: a - portal vein of a newborn; b - sleeping umbilical vein of a child for 2 days of life. The lumen of the vein is not determined, there is no blood flow in it (white arrow); b, d - umbilical vein of another child 2 days of life. At rest, there is no blood flow in the umbilical vein, with a deep breath - the parietal blood flow (arrow) is determined. Another feature of children of the early neonatal period is the unobliterated ductus venosus, which runs from the recessus of the left branch of the portal vein to the inferior vena cava and flows into it directly near the right atrium, sometimes together with the left hepatic vein (Figure 8.7.1.2). This duct is a fetal commune. In utero, it ensures the flow of umbilical cord blood into the systemic circulation of the fetus. Persistence of the umbilical vein and ductus venosus determines the possibility of some complications during manipulations on the vessels of the umbilical cord of the newborn. Blood flow in the ductus venosus is determined in almost all children of the first day of life, in most - for 2-3 days, very rarely - in infants older than 6 days. The speed of blood flow in the ductus venosus can reach 1 m / s. Fig. 8.7.1.2. Ductus venosus in newborns: 1 - recessus of the left branch of the portal vein; 2 heart; a - the ductus venosus (arrow) is clearly visible in gray scale mode; b – the ductus venosus (arrow) flows into the inferior vena cava with a single trunk with the middle hepatic vein (double arrow) immediately near the right atrium; b - obliterated ductus venosus (arrow); d, d- ductus venosus in gray scale mode is not visible, in color doppler scanning is determined reliably (arrow); e - the spectrum of blood flow in the ductus venosus - the speed reaches 1 m / s The shape of the liver in newborns is fundamentally the same as in older children. In rare cases, when the organs of the abdominal cavity are sharply displaced, for example, with an embryonic hernia, the liver can take bizarre shape. At the same time, a significant part of it moves from the abdominal cavity to the hernial protrusion itself, sometimes filling it almost entirely. In such cases, the liver takes the form of an "hourglass". The vascular bed of the liver is deformed, but the trunk of the portal vein is preserved and can be traced reliably (Figure 8.7.1.3). Fig. 8.7.1.3. Atypical liver structure in an infant with an embryonic hernia: a - the type of organ on ultrasound. The sensor is installed on the hernial membranes; b - patient's type, the membranes of the embryonic hernia are treated with a solution potassium permanganate. The dotted line shows the location of the liver Also, a significant displacement of the liver and its atypical form is observed with frenopericardial hernia, with an anterior diaphragmatic hernia on the right (Larrey's hernia). With these defects, the liver is located in a significant mass in a typical place, but the left lobe is elongated and in the form of a "tongue" moves into the chest cavity, adjacent directly to the heart or to the pericardium (Figure 8.7.1.4). An unusual shape of the right lobe is also possible. Variants of the structure of the vascular system of the liver relate mainly to the portal vein. So, in children with embryonic hernias and an atypical form of the liver, agenesis of the left branch of the portal vein can occur with the formation of an atypical vessel in the parenchyma of the organ that goes through the thickness of the liver tissue. Such a variant of the structure of the portal system in an isolated form is rare. In this case, the trunk of the portal vein can be traced reliably, but the division into right and left branches missing. All blood flow is directed along the "right" branch of the portal vein, which describes a wide arc in the liver parenchyma, ending in a typical projection of the distal part of the left branch (recessus). Clinical and laboratory manifestations of hepatic pathology are not observed (Fig. 8.7.1.5). Rice. 8.7.1.4. True Larrey's anterior diaphragmatic hernia on the right side of newborn: PP - right atrium; a - a survey radiograph of the organs of the chest cavity, the dotted line indicates a fragment of the liver displaced into the chest cavity; b, c - ultrasound determines the displacement of a fragment of the left lobe of the liver into the chest, which is adjacent directly to the heart; d - contact of the right lobe of the thymus with a displaced fragment of the liver; d, e - a study of the heart, in which a fragment of the liver adjacent to the heart is well differentiated. An arrow shows a catheter passing through an open oval window A rare vascular pathology of the liver is a congenital portosystemic veno-venous shunt. In most cases, in newborns, such a pathology is detected by screening ultrasound examination or in the presence of clinical signs of hepatic or abdominal pathology (Fig. 8.7.1.6). This variant is congenital shunts are relatively favorable, the presence of congenital arterioportal shunts quickly leads to the development of portal hypertension. In rare cases, a massive discharge of blood through a portosystemic shunt leads to metabolic disorders in the form of hyperammonemia, hypergalactosemia without enzymatic deficiency. In most cases, such shunts close on their own in the second half of the child's life. Fig. 8.7.1.5. Anomaly of the structure of the portal vein in a newborn: a - the trunk and right branch of the portal vein are determined reliably; b, c - there is no left branch of the portal vein, the right branch passes into a large intrahepatic vessel describing an "arc" in the liver parenchyma (arrow, a fragment of the hepatic vein is shown with a double arrow) and ending in the recessus (R) projection of the left branch Gas in the portal system in infants is very rare and in most cases is observed in the prodromal period of ulcerative-necrotizing enterocolitis, less often in severe cases of the same disease. In the most pronounced cases, the movement of small gas bubbles can be recorded in the trunk of the portal vein. It is also possible that this phenomenon occurs in newborns who have undergone infusions into the umbilical cord veins. The phenomenon is short-lived, the duration of its existence is calculated in a few hours or days. It is noteworthy that in most cases it is not possible to confirm the roentgenological presence of gas in the portal system, ultrasound is a more sensitive method for detecting this phenomenon (Fig. 8.7.1.7). Calcifications in the liver parenchyma are usually formed as a result of intrauterine infectious lesions, nature which is not always clear. In particular, such changes are observed in congenital syphilis. Foci can be single or multiple, the criterion for echographic evaluation of the focus as a calcification is the presence of an acoustic shadow behind it (8.7.1.8). Fig 8.7.1.6. Congenital intrahepatic portosystemic shunt: a - left lobe of the liver in B-mode; b - the same scan, color Doppler mode. The direction of blood flow in the portal vein - to the sensor (red color), in the hepatic vein - from the sensor (blue); b, g, d - spectral characteristics of blood flow at various points of the shunt; e - color Doppler examination of the shunt in another scan; f, z, and - polypositional scanning. Between the portal and hepatic veins, multiple subtle communications can be traced. Also, multiple hypoechoic foci in the liver can be observed with angiomatosis of the organ, often combined with hemangiomas localized on the surface of the child's body. Hemangiomatous foci can be both single and multiple (without counting), occupying all fragments of the organ. The size of individual foci reaches 20 mm already in newborns. A pathognomonic echographic symptom is a sharp increase in the vascular pattern in the foci: either along their periphery or throughout the focus (Figure 8.7.1.9). In some cases, there is a tendency for foci to disappear. Fig. 8.7.1.7. Gas of the portal system in newborns: a, b - gas of the portal system in a child of 18 hours of life who underwent infusions into the umbilical cord vein in the delivery room; b, d, d - gas of the portal system and gas in the pyramids of the kidney in a newborn in the prodromal period of enterocolitis; e - a pronounced phenomenon of the gas of the portal system; f - the same child, on the radiograph gas in the portal system is not traced; z, and, k - the same child, gas bubbles in the left branch of the portal vein; with dopplerography, characteristic short-term interference is determined Fetal hepatitis in infants also does not have pathognomonic echographic symptoms, it can only be suspected on ultrasound with a certain degree of probability, but it is impossible to diagnose or exclude it absolutely accurately echographically. Hepatomegaly, a diffuse increase in the echogenicity of the liver parenchyma; sometimes splenomegaly are determined. Typical is pronounced ascites, but this symptom is not always found. Very often changes in the gallbladder are determined: it is reduced in size, its wall is thickened, there may be clots, sediment, suspension in the lumen (Figure 8.7.1.10). Very similar echographic changes are observed in galactosemia, when, in addition to changes in the structure of the liver and gallbladder, they are characteristic pronounced manifestations of ascites. Significant changes in the parenchyma of the liver and gallbladder can be a manifestation of severe toxicosis of various genesis, and clots in the lumen of the bladder are often found in cholepathies in young children. Fig. 8.7.1.8. Liver of a newborn with intrauterine infection (syphilis): a - in the parenchyma of the right lobe of the liver, more - multiple (without counting) hyperechoic inclusions of 3-4 mm in diameter without a clear acoustic shadow are determined along the periphery of the organ; b - same child, different sensor. Fuzzy acoustic shadows are determined; c, g - another scan. A parietal thrombus (arrows) is defined in the recessus left branch ports and a large calcification (9 mm) with a clear acoustic shadow (double arrow) A distinctive echographic sign of atresia of the bile ducts is the absence of a gallbladder. Along with this, there are hepatomegaly and an increase in the echogenicity of the liver parenchyma, as in fetal hepatitis. Strictly speaking, it is the presence or absence of the gallbladder that is the echographic differential diagnostic sign of these diseases, which are essentially considered as different stages of the course of the same process. Sometimes with atresia of the bile ducts, dilatation of the intrahepatic bile ducts can be observed; moderate expansion of the common hepatic duct in the liver gate is prognostically favorable, since it determines the probability of the effectiveness of Portoenteroanastomosing according to Kasai. Rice. 8.7.1.9. Hemangiomatosis of the liver in young children: a, b, c - a child of 1 month, one of the foci of the right lobe of the liver: a sharp increase in the vascular pattern in the projection of hypoechoic foci; g, d - the same child, another part of the right lobe of the liver, similar changes; e-k - baby G., 2 months. In all parts of the liver parenchyma, multiple (without counting) hypoechoic foci with uneven fuzzy contours, irregularly rounded shape, up to 11 mm in diameter, with a sharply enhanced vascular pattern along the periphery were revealed. Fig. 8.7.1.10. Fetal hepatitis (a-d) and cholepathy (e-z) of newborns: a - appearance of a child with fetal hepatitis; b, c - the same child, the gallbladder is reduced in size (15x5 mm on an empty stomach), deformed, its walls are thickened, the echogenicity of the walls of the bladder is increased; d - another child, a bladder with a small amount of liquid contents, the walls of the bladder are thickened and compacted, swelling of peribladder tissues is pronounced; e - another child, the lumen of the bladder is filled with echogenic inclusions (double arrow), does not contain liquid bile; e, f - cholepathy in a child of 6 days of life against the background of complete parenteral nutrition. In the lumen of the choledoch, a clot (arrows) is determined, clots in the bottom of the bladder; h - another child with a similar history. Clot (double arrow) in the lumen of the gallbladder