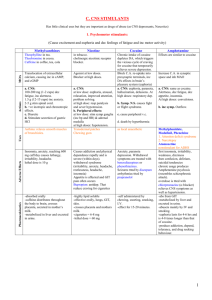
Heparin (Hepalean, Hep-Lock, Hep-Lock U/P) [SQ] Furosemide PO (Lasix) [PO] Indication: prophylaxis and treatment of various thromboembolic disorders: VTE, Pulmonary emboli, Afib with embolization, Acute/Chronic consumptive coagulopathies, Peripheral arterial thromboembolism. IV flush for access patency Indication: edema due to heart failure, hepatic impairment, or renal disease. Hypertension. Mechanism of Action: Increases inhibitory effect of antithrombin on factor Xa and thrombin. Low doses prevent conversion of prothrombin to thrombin. Higher doses prevent conversion of fibrinogen to fibrin. Mechanism of Action: Loop diuretic: inhibits reabsorption of Na+ and Clions at proximal and distal convoluted tubules and loop of Henle. Interferes with Cl-binding cotransport system. Increases renal excretion of H2O, Na+, Cl-, Mg+, K+, and Ca2+. Causes diuresis and removes excess fluid from the body, lowered BP as a result. Dose Range: IV: intermittent bolus 10,000 units followed by 5000-10,000 units Q4-6 hr. Continuous infusion: 5000u, followed by 20,000-40,000 units infused over 24 Dose Range: PO: 20-80 mg/single dose day initially, can increase to Q6-8 hr. For HTN: 40mg twice daily, adjust based on response. Hypercalcemia: 120mg/day in 1-3 doses. SQ (after IV): Initial dose 10,000-20,000 units, then Q8 8000-10,000 or Q12 15,000-20,000 IV: 20-40 mg, can repeat Q1-2 hr and increase dose by 20 mg every 1-2 hr until response is obtained. Continuous IV: Bolus 0.1 mg/kg followed by 0.1mg/kg/hr, max 0.4 mg/kg/hr. Common side effects: GI: drug-induced hepatitis. Derm: alopecia, rashes, urticaria. Local: pain at injection site. MuscSkel: osteoporosis (long term use) Misc: fever, hypersensitivity Life Threatening Side Effects: Hemat: bleeding, heparin-induced thrombocytopenia Nursing Considerations: assess for signs of bleeding and hemorrhage (bleeding gums, unusual bruising, hematuria, black stools, decreased hematocrit/BP. Monitor for hypersensitivity reactions. Observe injection site for hematomas, ecchymosis, or inflammation. Monitor platelet count every 2-3 days during use. Drug-Drug Interactions: Increased risk of bleeding if used with other medications that affect platelet function, i.e. NSAIDS, aspirin. Drug-Food Interactions: increased risk of bleeding with arnica, anise, chamomile, clove, dong quai, garlic, ginger, and panax ginseng. Common Side Effects: CNS: blurred vision, dizziness, headache, vertigo. EENT: Hearing loss, tinnitus. CV: hypotension. Fl/Elec: dehydration, hypocalcemia, hypocloremia, hypokalemia, hypomagnesemia, hyponatremia, hypovolemia, metabolic alkalosis. Life Threatening Side Effects: Stevens-Johnson Syndrome, Erythema multiforme, toxic epidermal necrolysis, aplastic anemia, agranulocytosis. Nursing Considerations: Assess fluid status. Obtain daily pt weight and strict I/O record. Note lung sounds, skin turgor, and assess mucous membranes for signs of dehydration. Monitor BP before and after administration. Assess pt skin frequently for skin rash during therapy. Drug-Drug Interactions: increased risk of hypotension with antihypertensives or nitrates. Increased risk of hypokalemia with other diuretics, laxatives, photericin B, and corticosteroids. Drug-Food Interactions: alcohol use increases risk of hypotension. Pantoprazole (Protonix IV) [IV] HYDROcodone/acetaminophen (Norco, Anexsia) [PO] Indication: erosive esophagitis associated with GERD. Pathologic gastric hypersecretory conditions. Unlabed use: supplemental treatment of duodenal ulcers caused by H. pylori. Indication: Management of pain that is severe enough to warrant daily, around-the-clock long-term opioid treatment where alternative options are not effective. Antitussive. Mechanism of Action: Proton Pump Inhibitor- binds to H+ and K+ exchanging ATPase in gastric parietal cells and prevents final transport of H+ ions into gastric lumen. Results in blocking of acid secretion. Mechanism of Action: Binds to opiate receptors in the CNS. Alters the perception of painful stimuli. Suppresses cough reflex. Acetoaminophen: acts on the hypothalamus to produce antipyresis. Inhibits prostaglandin synthetase. Hydrocodone: blocks pain perception in the cerebral cortex, decreases synaptic chemical transmission throughout the CNS and inhibits pain sensation into higher centers. Dose Range: IV for GERD: 40mg once daily for 7-10 days. IV for hypersecretory conditions: 80mg Q12 hr, max 240mg/day. Common Side Effects: headache, diarrhea, nausea, abdominal pain, vomiting, flatulence. Life Threatening Side Effects: C. difficile associated diarrhea (CDAD) Nursing Considerations: assess patient regularly for abdominal pain and bloody or black, tarry stools. May cause abnormal liver function tests. Monitor bowel function, watch closely for diarrhea to monitor risk for CDAD. Check for patient history of antiretroviral use or HIV/AIDS diagnosis. Drug-Drug Interactions: decreases levels of atazanavir and nelfinavir, avoid use with these antiretrovirals. Can decrease absorption of drugs needing an acidic pH. Increased risk of bleeding with warfarin. Increased hypomagnesemia risk with digoxin. Can raise methotrexate levels. Drug-Food Interactions: No restrictions on what food may be consumed, however patient might want to avoid caffeine, overly spicy foods, and meals high in saturated fat. Dose Range: PO Analgesic: 2.5-10 mg Q3-6 hours as needed. PO Antitussive: 5mg Q4-6 as needed. Common Side Effects: CNS: confusion, dizziness, sedation. CV: hypotension. GI: constipation, dyspepsia, nausea. Misc: physical/psychological dependence, tolerance. Life Threatening Side Effects: Overdose Nursing Considerations: assess BP, pulse, and respirations before and after administration. Assess bowel function to assist in prevention/treatment of constipation caused by administration. Assess pain before and 1hr after administration, aim to catch pain before breakthrough happens. Assess risk for opioid addiction, abuse, or misuse before administration. Drug-Drug Interactions: Exercise extreme caution when administering to a patient using MAOIs. Concurrent use with CYP3A4 inhibitors increase levels and risk of opiod toxicity. Use with benzodiazepines or other CNS depressants can cause profound sedation, respiratory depression, coma, death. Increased risk of serotonin syndrome with antidepressants. Drug-Food Interactions: Use of kava-kava, valerian, skullcap, chamomile or hops can increase CNS depression. Metoprolol (Lopressor, Toprol-XL) [PO] Lorazepam (Ativan) [PO] Indication: Hypertension, angina pectoris, prevention of MI, decreased mortality in patients with recent MI. Management of symptomatic heart failure. Unlabeled use: ventricular arrhythmias/tachycardia. Migraine prophylaxis. Tremors. Anxiety. Aggressive behavior, drug-induced akathisia. Indication: PO: anxiety disorders. IM/IV: status epilepticus, pre-anesthetic to produce sedation, decrease pre-op anxiety and induce amnesia. Mechanism of Action: Blocks response to beta-adrenergic receptors. Cardioselective for beta1 receptors at low doses, little to no effect on beta2 receptors. Dose Range: Antihypertensive/antianginal: 25-100mg/day as a signle dos initially or 2 divided doses, can be raised over 7 days to 450mg/day for immediate release or 400mg/day for extended release. MI: 25-50mg Q6 for 48 hrs, then 100mg 2x daily. Heart failure: 12.5-25mg once daily. Migraine prevention: 50-100mg 2-4x daily. Common Side Effects: CNS: weakness, fatigue. GU: Erectile dysfunction. Life Threatening Side Effects: Bradycardia, Heart Failure, Pulmonary edema Nursing Considerations: Monitor BP, EKG, and pulse frequently during therapy and dose adjustment. Monitor vital signs and EKG every 5-15min during and then for several hours after parenteral administration. Watch closely for a heart rate less than 40 bpm. Monitor I/O ratio. Perform daily weight checks. Assess lungs routinely for signs of heart failure. Drug-Drug Interactions: general anesthesia, IV phenytoin, and verapamil may cause increased myocardial depression. Increased risk of bradycardia if used in conjunction with digoxin, verapamil, diltiazem, or clonidine. Increased hypotension may occur if used with other antihypertensives or used with alcohol or nitrates. Use with amphetamines, cocaine, ephedrine, epinephrine/norepi, phenylephrine, or pseudoephedrine can cause excessive hypertension and bradycardia. Decreased effectiveness of thyroid medication if used in conjunction. Alters effectiveness of insulins/hypoglycemic agents. Mechanism of Action: Depresses the CNS by potentiating GABA (inhibitory neurotransmitter). Provides sedation, decreased anxiety, decreased seizures. Dose Range: epilepticus: 4mg IV, can repeat 10-15min. Preanesthetic: 0.05mg/kg body weight given IM, not to exceed 4 mg less than 2 hr before surgery. 0.044mg/kg given IV, not to exceed 2mg 15-20 min before surgery. Anxiety: 1-3 mg, 2-3 times daily, not to exceed 10mg/day. Insomnia: 2-4 mg given at bedtime. Common Side Effects: dizziness, drowsiness, lethargy. Life Threatening Side Effects: (rapid IV route) apnea, cardiac arrest Nursing Considerations: conduct regular assessment for continued need for treatment. Assess degree and manifestations of anxiety & mental status before and after administration. Assess location, duration, characteristics, frequency of seizures. Institute seizure precautions for seizure pts. Monitor pts on high doses for renal, hepatic, and hematologic function. Drug-Drug Interactions: Use with opioids, CNS depressants, and alcohol can cause profound sedation, respiratory depression, coma, death. Lowers efficacy of levodopa. Smoking with concurrent use raises metabolism and lowers effectiveness. Oral contraceptives can decrease medication levels. Drug-Food Interactions: use of kava-kava, valerian, or chamomile can increase CNS depression.