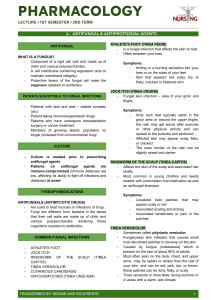
Mycosis & Antifungal medications • Agents used to treat mycosis (fungal infection) • Most fungal infections are superficial yet they can lead to serious complications especially in HIV patients as well as patients receiving immunosuppressants or cancer chemotherapy. • Antifungal drug discovery lagged behind leading to a rising resistance to current agents • Development of antifungal agents was overshadowed by antibacterial drug discovery • Most antifungal agents are superficial and self-limiting Systemic mycoses Opportunistic mycoses Superficial Mycoses Cutaneous mycoses Subcutaneous mycoses Classifications of Mycosis I – Infection of internal organs as lung via the inhalation of fungal spores – Example: Histoplasmosis, aspergillosis and systemic candidiasis – Excessive use of antibiotics affects normal flora balance within the body causing the overgrowth of fungi with low inherit virulence – Immuno-compromised patients are at risk of contracting such infections – Example: Fungal infection of GIT, mucosal lining of the vagina Classifications of Mycosis II – Infection of the outermost layer of skin and hair – Examples: Tinea infections – Infection of mucosal lining of mouth, lips and vagina – Infection of keratinized epidermal tissues as nails and hair (dermatophytic infection) – Diffuse cutaneous infection involving the skin and the subcutaneous tissues – Chronic and harder to treat – Results from skin trauma – Example: Mycetoma 1 Polyenes • Macrocyclic lactones containing conjugated double bonds that act as membrane disruptive agents • They preferentially bind to ergosterol embedded in fungal cell membrane creating pores in euokaryotic membrane allowing the leakage of important nutrient outside fungal cell which finally leads to cell death • They display lower binding to mammalian cholesterol yet they can lead to serious complications • Polyenes are amphoteric analogs which are sparingly soluble in water Ergosterol and Cholesterol: Ergosterol displays a flatter configuration as it contains 2 extra double bonds Amphotericin B Nystatin • Conjugated heptaene analog that displays lower toxicity relative to nystatin (WHY?), nevertheless it is considered nephrotoxic and patient receiving IV amphotericin B deoaxycholate formulation might require hospitalization • These side effects can be ameliorated by liposomal amphotericin B • Liposomal amphotericin preparation (AmBisome) are self-sealing vesicles (carriers) consisting of a phospholipid bilayer/cholesterol that contains amphotericin B. • AmBisome releases the drug at the site of action • Conjugated tetraene analog • Used topically as cream or ointment formulation for superficial mycosis or orally for mouth and GIT mycosis since nystatin has limited systemic absorption from the GIT tract. • Nystatin displays considerable side effects on mammalian host cells by binding to cholesterol. Agents Interfering with Ergosterol Biosynthesis There are some key enzymes involved in the biosynthesis of ergosterol, their inhibition will disrupt the process of ergosterol biosynthesis 2 1. Azoles • Analogs possessing an imidazole or triazole moiety • They bind to the heme prosthetic group of (Cytochrome P450 enzyme) CYP51 (14α- demethylase enzyme) inhibiting ergosterol biosynthesis • Accumulation of lanosterol which have different physical properties relative to ergosterol leads to increased cellular permeability and loss of important ions and molecules • Azoles exert better selectivity towards fungal enzymes yet they inhibit the mammalian isoform at higher concentrations Ketoconazole Fluconazole Posaconazole • Imidazole antifungal agent • Either can be used orally for systemic infections or topically for localized infections • Agents that increase stomach pH as H2-anatagonists will decrease systemic absorption of ketoconazole after oral administration. • Ketoconazole is a substrate as well as inhibitor CYP3A4 enzyme • CYP3A4 inducers as phenytoin will decrease ketoconazole plasma concentration • Drug that are metabolized by CYP3A4 will experience prolonged half-life and increased plasma concentration as macrolide antibiotics, tricyclic antidepressant and selective serotonin reuptake inhibitors • A triazole antifungal agent. • It has the advantage of having better oral bioavailability relative to ketoconazole. • Medications metabolized by CYP2C9 enzyme will require adjustment to the administered dose (Especially drugs with narrow therapeutic index like warfarin and phenytoin) as fluconazole is a strong inhibitor of CYP2C9 enzyme. • Fluconazole has limited aqueous solubility. (How possible its water solubility can be improved?) • A recently introduced triazole analog which is used orally for systemic fungal infections • Very effective against fungi that are resistant to other azoles as Aspergillus • Posaconazole inhibits Aspergillus two CYP51 isoforms (CYP51A and CYP51B). Thus it prevents the salvage pathway used for ergosterol biosynthesis. 3 • Posaconazole and ketoconazole inhibit P-glycoprotein(multi drug resistant protein). Econazole • Used as 1% cream for topical treatment of local tinea infections and cutaneous candidiasis 2. Squalene Epoxidase Inhibitors • First enzyme involved in ergosterol biosynthesis, it introduces an epoxide group at C2-C3 position. • Inhibition of squalene epoxidase leads to: 1- Changing physical properties of the cell membrane allowing the leakage of important nutrients 2- Accumulation of squalene which is considered by itself toxic to the fungal cell • These inhibitors primarily inhibit fungal squlene epoxidase enzyme with weak effect on human enzyme • These analogs have narrow spectrum of activity mostly against dermatophytes and superficial infections Allylamines • Used as a cream formulation for topical ringworm and athlete's foot tinea infections • Used orally or topically for dermatophytic infections • Effective for the treatment of onychomycosis (ringworm tinea infection of the nails) • Soluble in polar organic solvent (How its aqueous solubility can be increased?) • Bioisostere of naftifine (No allylamino group) • Used for superficial Candida infections • Thiocarbamate analog • The first squalene epoxidase inhibitor medication to be used in the pharmaceutical market • Used for superficial infections 4 3. Δ7, Δ8-Isomerase and Δ 14 -Reductase Inhibitors Morpholine analog interfering with ergosterole biosynthesis process by inhibiting Δ7, Δ8-Isomerase and Δ 14 Reductase altering physical properties of the cell membrane. Inhibitors of Cell Wall Biosynthesis Echinocandins • Semi synthetic cyclic lipopeptides (contain lipophilic side chain) • Echindocandins decrease strength of fungal cell wall by inhibiting β-1,3-glucan synthase. Caspofungin Micafungin • Considerably safe medications as they target organelle not found in the mamlian host • Used for life threatening funal infections • Only administered by IV route (Why?) 5 Miscellaneous Agents Griseofulvin Flucytosine • Inhibits mitotic division in fungi, thus it is considered a fungistatic agent. • It act on the metaphase stage by interfering with mitotic spindles • It is administered orally where it is carried by systemic circulation to keratin rich tissue. • Used for treatment of fungal infection of nail and hair • Prodrug converted in vivo to the active form (can it affect the human host?) • Incorporation of false nucleotides interfering with protein and RNA synthesis. • Also it is considered as an irreversible inhibitor of thymidylate synthase • Used for systemic serious fungal infections 6 Fluconazole Synthesis Econazole 7 Synthesis of Naftifine Tolnaftate 8