FLUORIDE USE IN
DENTISTRY
DR BAKARE
Outline
•
•
•
•
•
•
•
•
•
•
•
Introduction
History
Natural Sources Of Fluoride
Physiology and metabolism of fluoride
Fluoride in Dentistry
Control of dental caries
Fluoride toxicity
Dental fluorosis
Fluorosis indices
Water defluoridation
Conclusion
Introduction
• Fluoride is a mineral and Fluoride ion comes from the element
fluorine.
• Fluorine is 17th most abundant element in the earths crust.
• Highly reactive, hence never encountered in its free state in nature.
• Exits only in combination with other elements as a fluoride
compound
• Constitutes about 0.032% in earth’s crust
• The name Fluorine is derived from
• The Latin word “fluore” meaning “to flow”.
• Greek “floris”- destruction
Brief History of Fluoride in Dentistry
• Frederick McKay in 1901 noted characteristic mottling stains on teeth
of children who had spent all their life in Colorado known as Colorado
brown stain
• G.V Black and others found that other regions in the USA has similar
mottling, and histological exam show that enamel was imperfectly
calcified. No difference in caries incidence compared with normal
teeth.
• Mackay suspected the cause to be from the water supply
• Similar findings in a community formed by house workers of an
aluminium company prompted the chief chemist anxious that
aluminium should not be blamed, to analyse the water and found a
higher than normal concentration of fluoride (about 13.7ppm)
• HT Dean in 1938 showed a relationship between tooth mottling and
water fluoride level and that mottling disappear or minimal as
fluoride fall below 1ppm.
• FA Arnold 1953 reported a 50% fall in caries in Grand Rapids
compared with control group after 6years of artificially fluoridating
water.
• 1969 --- WHO recommended first time 1 ppm fluoride in drinking
water for a practicable and effective public health measure.
• 1994 ----- WHO has recommended optimum level of fluoride in
drinking water as 0.5-1.0ppm.
Fluoride in Nigeria
• Data from Nigeria is sparse. Two studies from Plateau state found a
prevalence of 26.1% in langtang with 20.6% classified as mild. It
reported Fl conc of 2.39-3.96ppm in streams and 1.26-2.82ppm in
wells(1997)
• In 2008, a prevalence of 12.9% was recorded. This study also found
higher prevalence in high altitude areas which had lower Fl content
of 0.76+/- 0.04 than the lower altitude areas
Natural Sources of Fluoride
• In rock and soil-
• Fluorspar ( fluorite CaF2)
• Fluorapatite {Ca10F2 (PO4 )6}
• Cryolite ( Na3AlF6)
• In Soil, the fluoride concentration increases with depth.
• In Water:
• Sea water - 0.8- 1.4mg/L.
• Lakes, rivers or artesian wells - below 0.5mg/L.
• Concentrations as high as 95mg/L have been recorded in the United Republic
of Tanzania.
• In Air:
•
•
•
•
•
Fluoride is widely distributed in the atmosphere as;
dusts of fluorides-containing soils
gaseous industrial waste
domestic burning of coal fires
gases emitted in areas of volcanic activity
• In Foods And Beverages:
•
•
•
•
Unprocessed foods -low (0.1-2.5 mg/kg).
In plants - 2-20mg/g of dry weight.
Leafy vegetables -11-26 mg on dry weight basis.
Fish -20-40 ppm on dry weight basis.
• In Animals
•
•
•
•
Beef, pork and mutton-0.3ppm
Higher in Chicken- contained in bone and cartilage fragments
Fish products- up to 20ppm
Dried sea foods also fluoride rich 84.5ppm (South East Asia)
• In beverages
• Juice, beverages,
• Infant formula
• Fluoride content in liquid beverages generally reflects that of water used.
Total daily intake of Fluoride
• Fluoride from Air
• Minimal
• Fluoride from Water
• Most important single source of fluoride
• Dependent on fluoride concentration and amount
• Fluctuation –climatic and geographical areas
• Fluoride from food
• 0.3 to 0.6 mg/day
• Fluoride intake 6months of life-bottle/breast fed
• Breast fed infant receives 0.003 to 0.004mg/day- formula fed infants (1.2ppm)
fluoride intake increased 50 times
Physiology of fluoride
• Ingested fluoride is absorbed mainly from the upper G.I.T.
• F ingested on an empty stomach reaches peak plasma level in 30
minutes
• Up to 95% of ingested F may be absorbed
• Absorbed fluoride is transported in plasma and is either excreted or
deposited in the calcified tissues
• Most absorbed fluoride is excreted in urine.
• Single ingestion of 5mg fluoride by an adult is absorbed and cleared
from the blood in 8-9 hrs.
• Approx. 75% – 90% of ingested F¯ is absorbed
• More in liquid diet than in solid (80% in solid, up to 97% in water)
• Half-time for absorption is 30 min
• Peak plasma concentration – 30 – 60 min.
• Ionic form-- relevant to health
• Fat soluble form
• Calcium in diet reduces absorption
• 99% of body burden is assoc. with calcified tissues
• 50% will be assoc. within 24 hr – Rest is excreted through urine
Distribution of Fluoride
• Teeth and skeleton have the highest concentrations of fluoride -affinity of fluoride to calcium.
• Fluoride content of teeth increases rapidly during early
mineralization periods and continues to increase with age, but at
a lower rate.
Fluoride in Dentistry
• The application of fluoride in dentistry can be
considered under the following:
• Control of dental caries
• Fluoride toxicity
• Dental fluorosis
Fluoride in Caries Control
• The effect of fluoride in caries prevention can be
considered under two headings.
• Pre-eruptive effect
• Post – eruptive effect
Pre-Eruptive Effect
• Improved crystallinity - Changes the crystalline structure of enamel to
make it less soluble.
• Increased Crystal size
• Less acid solubility
• More rounded cusps and fissures
• Overall effect is small because discontinuation of fluorides leads to
increased caries – constant servicing!!!
Pre-Eruptive Effect
• Changes the crystalline
structure of enamel to make it
less soluble.
OLD CONCEPT
• That major inhibitory effect was
thought to be due to its
incorporation in tooth mineral
during the development of the
tooth prior to eruption
• Recent evidences shows that the main effect of fluoride in caries
prevention are the post-eruptive - through Topical effect.
• Fluoride incorporated during mineral development at normal levels of
20- 100ppm does not alter the solubility of the mineral.
• Fluoride incorporated developmentally into the normal tooth mineral is
insufficient to have a measurable effect on acid solubility.
• Only when fluoride is concentrated into a new crystal surface during Remineralization, is it sufficient to alter solubility beneficially.
Post-Eruptive Effect
• Effect is seen when fluoride is present in plaque and saliva.
• There is now clear evidence that caries reduction is most effective
when a low conc. Of Fl is maintained consistently in the oral
environment.
• This is in contrast to earlier concept
• Attributed the major benefit of Fl to pre-eruptive maturation of forming
enamel
• Predominant effect is TOPICAL rather than systemic
• Interferes with glycolysis – Bacteria metabolizing sugars to acid by
inhibiting enolase and proton pump ATPase.
• Inhibit the glycolytic pathway of oral microorganisms reducing acid
production and interfering with the enzymatic regulation of carbohydrate
metabolism.
• Also reduces the accumulation of intracellular and extra-cellular
polysaccharides
• This bactericidal action occurs only at higher concentrations.
• These inhibitory mechanisms are affected by the hydrogen ion
concentration of plaque.
• A decrease in pH results in a greater inhibitory action on bacterial
carbohydrate metabolism
which occurs due to
• Unionized hydrofluoric acid formed at lower pH values
• Fluoride can not cross the cell wall and
membrane in its ionized form(F-) but can
rapidly travel through the cell wall and into
the cariogenic bacteria in the form of HF.
• Fluoride in the presence of plaque bacteria
generated acid, travels with the acid into
the subsurface of the tooth, adsorb to the
crystal surface and protect it from being
dissolved.
• Once inside the cell ,the HF dissociates
again acidifying the cell and releasing
fluoride ions that interfere with enzyme
activity in the bacterium.Interferes with
glycolysis
Summary of Fluoride Anti-caries Activities
• Fluoride prevents demineralization.
• Formation of fluorohydroxyapatite and inhibition of mineral loss from enamel.
• Fluoride enhances remineralization
• Through formation of a fluoride reservoir and creation of supersaturated solutions.
• Fluoride alters the action of plaque bacteria.
• At low pH, fluoride combines with hydrogen ions and diffuses into oral bacteria as
hydrogen fluoride (HF) Inside the cell HF dissociates, acidifying the cell and releasing
fluoride ions that inhibit glycolysis.
• Fluoride aids in post eruptive maturation of enamel.
• Fluoride reduces enamel solubility.
Fluoride Application
Systemic fluoride
Sources
• Water and other beverages.
• Food
• Fluoride drops
• Fluoride tablets
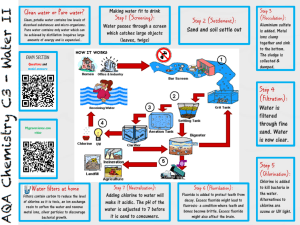
Water Fluoridation
• It is the controlled addition of fluoride to public water supply to bring its fluoride
concentration up to an optimal level to prevent dental caries.
• Also defined as controlled adjustment of the concentration of fluoride in a
communal water supply so as to maximize caries reduction and a
clinically insignificant level of fluorosis.
• It is also an upward adjustment of the concentration of fluoride ion in a public
water supply in such way that the concentration of fluoride in the water may be
consistently maintained at 1 ppm by weight to prevent dental caries with
minimum possibility of causing dental fluorosis.
• Most effective, safest and cheapest way of reducing caries.
• Recommended level of fluoride for community water supply ranges
from 0.7-1 ppm depending on the mean maximum temperature.
• At this level, fluoridated water is odourless and tasteless.
• It results in 20-40% reduction of caries over a life time
• It does not confer life time immunity
• The adsorption of fluoride to the
enamel surface is greatly
influenced by concentration and
temperature.
• Hence the, fluoride concentration
in public water supply is adjusted
according to the average
atmospheric temperature
(temperate /tropical region)
• WHO recommended (1994)- 0.5 to
1.0 ppm
Simple
modified
method
to
determine
optimum
fluoride
concentration
and
mean
annual
temperature. Richard et.al
• The use of water fluoridation dates back to the 1900 following the
discovery of the a mystery staining of teeth by Dr. Fredrick Mckay in
Colorado Boulder.
Advantages
• Most economical and cost effective measure for reduction of dental
caries
• It is practicable because it requires no individual effort.
• Offers both pre-eruptive and post-eruptive effects
• Topical effect through release in saliva
Disadvantage
• It requires an effective and central water supply system
• Freedom of choice is removed
• Requires a complex infrastructure
• Initial capital outlay
School Water Fluoridation
• Suitable alternative to community water fluoridation
• 4.5 to 6.3 ppm
Advantages
• Effective public health measure-when community water supply is not
possible
Disadvantages
• 5 to 6 years old upon starting school- will not provide
pre-eruptive contact
• Intermittent fluoride exposure-less than 180 days in a year
Salt Fluoridation
• The controlled addition of
fluoride to domestic salt during
manufacture for the purpose of
preventing caries.
• Concentration is based on
estimate of salt consumption
and evaluated by studies of
urinary fluoride concentration
• 1st used in Switzerland in 1955
• Concentration of 250mg/kg salt
recommended (250ppm for
adults and less for children)
• Caries protection may be as
good as water fluoridation
• Commonly used material is
Potassium Fluoride
Salt Fluoridation
Advantages
•
•
•
•
Low cost
Negligible waste
Ease of implementation
Freedom of choice for individuals
Disadvantages
• Fluoride dosages of different age
in different regions
• Lower salt consumption during
tooth forming years
• In conflict with general health
message of low salt intake for
prevention of coronary heart
disease
Milk Fluoridation
• First mentioned by Ziegler in 1956
• Limited Effect as a public measure
• Topical fluoride effect less than
water because of binding to
calcium or protein in the milk.
Advantages
• Need to drink under 14 years of
age
Disadvantages
• Incompletely ionized in milk
• Lower absorption from milk than
water
• Variation in intake
• Requires parental or school efforts
• Technical difficulties
• Problem in distribution
• High cost
Dietary Supplement
• Can be in form of tablets, drops,
in 1.0mg, 0.5mg and 0.25mg
preparations
• Most of them contain neutral
NaF.
• Dose is 0.5mg F/day in children ≥
3yrs
• Results in 40-50% reduction in
caries experience
Advantages
• Effective
• Freedom of choice
Disadvantages
• Compliance needed for
consistency
• Risk of over dose is high
Topical Fluoride
• These are placed directly on the teeth.
• Some preparations provide a high concentration of fluoride over a
short period of time.
• Other preparations such as dentifrices provide continuous low
concentration of fluoride on the teeth.
• Topical fluorides allow for the interaction of fluoride with minerals in
the teeth.
Indications for Topical Fluoridation
• Caries active individuals
• Children shortly after the period
of teeth eruption.
• Those who are on medication
which decrease the salivary flow
or who have received radiation
to head and neck.
• After periodontal surgery when
the roots of the tooth are
exposed.
• Patients with fixed or removable
prosthesis after placement or
replacement of restorations.
• Mentally and physically
challenged patients.
• Patients with an eating disorder
or who are undergoing a change
in lifestyle which may affect their
oral hygiene habits.
Rationale for Topical Fluoridation
• To speed the rate and increase the concentration of the fluoride
acquisition above the level which occurs naturally.
• The initial caries lesion characterized by a white spot is porous and
accumulates fluoride at a much higher concentration than the
adjacent sound tooth enamel.
Topical fluorides are divided broadly into 2 main categories
Professionally Applied
• Introduced by Bibby in 1942.
• Dispensed by dental professionals in the dental office and usually
involve the use of high fluoride concentration products ranging from
5000-19000 ppm which is equivalent to 5-9mgF/ml.
• The three agents currently in use are:
1) Neutral Sodium Fluoride (NaF)
2) Acidulated Phosphate Fluoride (APF)
3) Stannous Fluoride (SnF2)
Advantages
• Effective and useful for individuals at high risk of dental caries
• Freedom of choice
Disadvantages
• Need for personnel
• Time consuming
• Requires access to service
Indications
•
•
•
•
•
•
•
•
Caries prone children >6 years of age
Patients with initial carious lesions
For nervous patients, varnish is easy to apply
Medically and physically disabled
For early childhood caries
Fluoride varnish can reduce hypersensitivity in root caries
Patients with orthodontic appliances who cannot or will not use fluoride rinses
Patients with reduced salivary flow due to salivary gland dysfunction, drugs or
radiotherapy
Contraindications
• Due to high fluoride concentration, it is not ideal for home use
• Not for children < 6 years who cannot spit out
Forms of Topical Fluoride
• Aqueous Solutions And Gels
• The gel adheres to the teeth for a considerable amount of
time and eliminates the continuous wetting of the enamel
surfaces required when solutions are used.
• When gels are applies using trays, it is possible to treat two or four quadrants
simultaneously and saves time.
• Each application is loaded by using a thin layer, thereby reducing the risk of
accidentally ingesting a large quantity of fluoride.
• Thixotropic solutions are more stable at lower pH and do not run off the tray as
readily as conventional gels.
• FOAMS
• Foam based agents were developed to minimize the risk of fluoride
over dosage as well as to maintain the efficacy of topical fluoride
treatment.
• Advantages of foam based APF agents are:
• It is much lighter than a conventional gel and therefore only a small amount
agent is needed for topical application.(4gm of gel/mouth while less than 1gm
of foam/mouth).
• The surfactant in the foaming agent has cleansing action by lowering the
surface tension.
• It may also facilitate the better penetration of the material into inter
proximal surfaces where its action is most needed.
• Since APF foams does not require suctioning, it offers advantages for
home use as well as treatment of young children and disabled
persons where saliva evacuation may not be feasible.
• FLUORIDE VARNISH
• It was first developed by Schimdt in Europe in 1964.
• Increasing the time of contact between enamel surface and topical fluoride
agents favors the deposition of fluoro-apatite and fluorohydroxyapatite.
• Technique Used:
• After prophylaxis, the teeth are dried but not isolated since varnish can stick to
cotton.
• 0.3-0.5ml of varnish is required to cover full dentition.
• Application is done first on lower arch then upper, using single tufted small brush,
starting with the proximal surfaces.
• Patient is asked to sit with mouth open for 4 min to let it set.
• The patient is asked not to rinse or drink for 1 hour.
• Examples of Fluoride varnish preparations:
• Duraphat
• It is the first fluoride varnish developed in Germany.
• It is a viscous yellow material containing 22,600 ppm fluoride as sodium fluoride
in aneutral colophonium base.
• It has shown 30%-40% caries reduction in permanent dentition and 7%-44%
reduction in primary dentition.
• Carex
• It is also a fluoride varnish containing low fluoride concentration than Duraphat
(1.8% fluoride).
• It has the efficacy equal to that of Duraphat as caries preventive agent
Technique of Application
• Knutson’s techniques
• At the initial appointment the teeth
are cleaned with aqueous pumice
slurry and then isolated with cotton
rolls and dried with compressed air.
• Using cotton tipped applicator sticks,
2% sodium fluoride solution is
painted on the air dried teeth so that
all tooth surfaces are visibly wet. The
solution is
allowed to dry for 3-4 minutes.
• Advice patient not to eat or drink for
the next 30 minutes
• The procedure is repeated for each of
the isolated segments until the teeth
are treated.
• A 2nd ,3rd and 4th fluoride
application, each not preceded by a
prophylaxis, is scheduled at intervals
of approx. 1 week.
• The four-visit procedure is
recommended for 3, 7, 11 and 13
years, coinciding with the eruption of
different groups of primary and
permanent teeth.
• MUHLER’S TECHNIQUE
• commonly for Stannous fluoride
application
• Each tooth surface is cleaned with
pumice or any other dental cleaning
agent for 5-10 seconds.
• Unwaxed floss is passed between the
interproximal areas.
• Teeth are isolated and dried with air.
• SnF2 is applied using paint-on
technique and the solution is kept for
4 minutes.
• Repeat applications are made every 6
months or more frequently if the
patient is susceptible to caries.
• Tray technique
• The patient should sit upright in the
chair.
• Oral prophylaxis is done.
• The teeth to be treated are completely
isolated and dried with air.
• Clinical application of APF gels should be
done using trays that fit into the patient’s
upper and lower arches.
• A disposable foam-lined tray is preferred.
• To reduce ingestion of fluoride, a
minimum amount of fluoride gel that will
permit complete coverage of the tooth
surfaces should be dispensed. Usually,
the amount is less than 5 ml
• After the trays have been properly positioned,
saliva ejector is used to evacuate the stimulated
saliva and excess fluoride.
• It is repeated every 15-30 seconds so as to keep
the teeth most with the fluoride solution
throughout the four minute period.
• The patient should be told not to swallow the
gel but to exert slight pressure using the cheeks
and tongue as well as light biting force in order
to cause the gel to flow interproximally.
• The fluoride gel should be in the mouth for 4
minutes and then the remaining oral fluid must
be expectorated.
• The patient is instructed not to eat, drink or
rinse mouth for 30 minutes.
Self Applied
• Low concentration fluoride agents
• Dentrifices
• Fluoridated toothpaste
• Mouthrinses
Fluoride toothpaste
• The commonest and most widely used.
• The simplest method of fluoride delivery.
• World wide decline in caries experience
has been attributed to widespread use of
toothpaste.
• Many of the toothpastes contain Sodium
monofluorophosphate.
• First fluoride dentrifice accepted by ADA
in 1964
• Demonstrated caries reduction of
about 30%
• The concentration of fluoride in
toothpaste varies
• The standard and most frequently
used toothpaste contains 1,000 to
1,100ppm of fluoride
• Toothpastes containing 500 to
550ppm fluoride (pediatric
toothpastes)
Recommendations
• Containers should be labeled with
the concentration of fluoride in
ppm
• Containers should be designed to
limit the amount of paste
dispensed
• Individuals should brush twice daily
Fluoride Mouth rinse
Recommendations
• Usually formulated at
concentrations of either 0.2% for • Should not be used in children
younger than 6 years
weekly use or 0.05% for daily
use.
• Should only be used in high risk
children
• They are intended to be used by • Appropriate for patients with
orthodontic appliances or
forcefully swishing 10ml of liquid
radiotherapy treatments
around the mouth for 60
seconds before expectorating it.
Fluoride Toxicity
• Fluoride toxicity can be
• Acute
• Chronic
Factors that affect toxicity of fluoride
• Concentration
• Duration of exposure
• State of nutrition (calcium, magnesium)
Acute toxicity
• Acute fluoride toxicity results from rapid excessive ingestion of fluoride at a
given time.
• Children younger than 6 years account for the vast majority of the cases.
• The acute lethal dose for an adult is suggested to be 32-64 mg F/kg, and in
children it is 5mg F/kg.
• Certainly lethal dose (CLD): Amount of drug likely to cause death.
• Adult = 5-10 g NaF taken at one time or 32-64 mg F / Kg body weight.
• Children = 2.5 g of NaF
•
Once absorbed, fluoride binds calcium ions and may lead to
hypocalcemia.
• Fluoride has direct cytotoxic effects and interferes with a number of
enzyme systems:
• It disrupts oxidative phosphorylation, glycolysis, coagulation, and
neurotransmission (by binding calcium).
• Fluoride inhibits Na+/K+ -ATPase, which may lead to hyperkalemia by
extracellular release of potassium.
• Fluoride inhibits acetylcholinesterase, which may be partly responsible for
hypersalivation, vomiting, and diarrhea (cholinergic signs).
Acute toxicity
• Signs and symptoms
1.Gastrointestinal signs predominate
• Hypersalivation
• Nausea
• Vomiting
• Diarrhea
• Abdominal pain
• Dysphagia
• Mucosal injury
2. Electrolyte abnormalities
Hypocalcemia
Hypomagnesemia
Hyperkalemia
3. Neurologic effects
•
•
•
•
•
•
•
Headache
Tremors
Muscular spasm
Tetanic contractions
Hyperactive reflexes
Seizures
Muscle weakness
4. Cardiovascular
• Widening of QRS
• Various arrhythmias
• Shock
Management of Acute Fluoride Toxicity
Immediate cases:
• Aimed at reducing fluoride absorption
by inducing vomiting, fluid
replacement, monitoring levels of
plasma calcium and potassium.
More than 5mg/kg fluoride ingested
• Empty the stomach by inducing
vomiting.
• Give milk, 5% calcium gluconate orally
and hospitalization.
Less than 5mg/kg fluoride ingested
• Give milk.
More than 15mg/kg fluoride ingested
• Immediate Hospitalization, Induce
vomiting, Cardiac monitoring, Slow
administration of 10% calcium
gluconate-IV.
• Maintain urinary output-using
diuretics if necessary, supportive
measures for shock.
Chronic toxicity
• Fluoride ingested in small doses over a long period time results in
changes in the teeth and bone.
• These changes are called fluorosis.
Fluorosis
• Dental fluorosis
• Skeletal fluorosis
Dental Fluorosis
• Occurs as a result of hypo-mineralization of enamel due to the
ingestion of excess fluoride during tooth development.
• The severity of fluorosis is dose, duration and time dependent.
• The occurrence of enamel fluorosis is most strongly associated with
cumulative fluoride intake during enamel development
• This is especially during the early maturation stage of enamel
development.
• The time for early maturation (enamel calcification) varies from tooth
to tooth
• Upper central incisor has the most sensitive period for fluorosis as 1524 months for boys and 21-30 months for girls
• Risk of enamel fluorosis is limited to children aged 8 years and below (
6 years and above, teeth are spared)
• Children aged 6 years (posterior teeth can be affected at this period).
• By age 6 years, most children can control inadvertent swallowing of
fluoride rinses and gel.
Measurement of fluorosis: indices
• Various indices have been developed to measure dental fluorosis. This
includes:
• Deans Fluorosis Index(original-1934 and modified-1942)
• Thylstrup and Fejerskov index for fluorosis
• Fluorosis risk index
• Tooth surface index of fluorosis.
Deans Fluorosis Index(original-1934 and modified-1942)
• Formulated by H. Trendley Dean in 1934
• The first Fluorosis Index for categorizing dental fluorosis.
• Based on a 7-point ordinal scale: normal, questionable, very mild,
mild, moderate, moderately severe, and severe.
• Was modified in 1942 in which moderately severe" and "severe"
categories were combined.
• A new 6-point ordinal scale was released and it is extensively used
today.
• It is also this version that is still recommended by the World Health
Organization (WHO) in its basic survey manual (Burt and Eklund,
1999; World Health organization.1997)
• Assessment to be done under good sunlight facing the
window.
Thylstrup and Fejerskov index(TFI) for fluorosis 1978
It is the most sensitive of the indices since it calls for drying which accentuates the appearance of fluorosis
Water De-fluoridation
• De-fluoridation means to improve the quality of water with high fluoride
concentration by adjusting the optimal level in drinking water.
Methods of water defluoridation
• Absorption and ion exchange method
• Exchange negative ions such OH- group for fluoride ions depends up on PH,
temperature, flow rate, grain size of the material.
• Commonly used materials: activated alumina, activated bauxite, Zeolite,
Tricalcium phosphate, activated bone char, magnesite, magnesite etc
Precipitation method:
• In a high PH condition, coprecipitation of several elements in
water with fluoride ions forms
fluoride salts- flocculation
• Examples:
• Alum
• Alum and lime
• Lime softening
• Calcium chloride
Membrane separation
• Reverse osmosis process
• Expensive developing countries
• 30% of raw water is lost in the process
Nalgonda Technique
• Invented in India in 1975
• Most simple
• Least expensive
• Easiest to operate
• Can be applied at the domestic and
community levels
• Cost effective
• Flexible design to use in different
location
Conclusion
• Fl when used appropriately fluoride is a safe and effective agent that
can be used to prevent dental caries.
• Appropriate fluoride intake in different population groups in different
areas has to be ascertained on the basis of fluoride concentration in
food and water resources taken by the local population.
References
• Fejerskov, J. Ekstrand, Brian. Fluorides in dentistry. 2nd edition.
• Mellberg and Ripa. Fluorides in preventive dentistry. 1st edition.
• John Murray, Rugg. Fluorides in caries prevention. 3rd edition.
• Update on the use of fluoride-S.Joyston-Bechal and E.A.M Kidd
• European Academy Of Paediatric Dentistry-guideline on the use of
fluoride in children
• Lauer WC. Water Fluoridation Principles and Practices. 5th ed. Vol.
M4. American Water Works Association
• 2017 August WACS Update
• Hussain J and Sharma KC. Environmental Monitoring and Assessment.
March 2010, Volume 162, Issue 1, pp 1-14.
• Textbook of community Dentistry, TR Gururaja Rao. 2004 edition.
• Rajan et al 1987,1988, Use of fluoridated toothpaste - Blood fluoride
levels in children, International society of fluoride research.
• American Academy of pediatric dentistry,1967, revised in 2014.
Reference manual , Vol 37 No.6.
Question
• The sensitive year for fluorosis is fouth year.
• Indication for topical fluoride application.
• Concentration of fluorde in Naf, SnF, APF
• Is prophylaxis needed before topical fluoride
• Content of a dentrifices