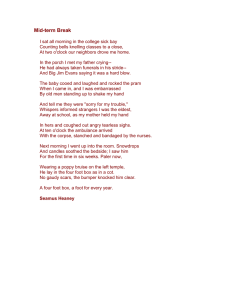
The 15th International Conference on Advanced Robotics Tallinn University of Technology Tallinn, Estonia, June 20-23, 2011 Foot Bone Kinematics at Half and Three Quarters Body Weight: A Robotic Cadaveric Simulation of Stance Phase Patrick M. Aubin, Member, IEEE, Eric C. Whittaker, and William R. Ledoux attaching marker clusters to individual bones of interest [3]. This technique is more accurate but also a highly invasive procedure with associated surgical risks. These limitations have motivated the development of dynamic robotic cadaveric models of the stance phase of gait [2],[4-8]. A cadaveric model is advantageous because invasive bone pins can be used to accurately measure bone kinematics without the ethical considerations associated with living subjects. Dynamic robotic cadaveric gait simulators animate a lower limb cadaveric specimen with the same motion, tendon forces, and vertical ground reaction force (vGRF) that occurs in vivo. Simulating a full body weight (BW) vGRF has proved difficult however due to challenges associated with building high force robotic devices and because the acquired cadaveric specimens from older donors often fail easily due to their low bone density. Previous studies have measured the bony motion of the foot and ankle when the applied vGRF was reduced to a BW of approximately 31 kg to 54 kg [7], or in some cases simply 50% BW [5],[9]. Other investigators have simulated 100% BW but used very light weight donors, i.e., BWs ranging from 35 to 50 kg [2]. It is unknown however how a reduced BW simulation affects foot kinematics. The purpose of this study therefore is to determine if the range of motion (ROM) of the bones in the foot is significantly different between 50% BW and 75% BW simulations of the stance phase of gait. Abstract—Lower limb cadaveric robotic gait simulators have been employed to model foot bone kinematics during the stance phase of gait. Often the simulations are performed at reduced body weight (BW) but the effect of this limitation on foot bone kinematics has not been quantified. In this study we utilized the robotic gait simulator (RGS) to measure in vitro foot bone kinematics at different applied ground reaction forces (GRFs) (50% BW and 75% BW). The RGS simulated gait by replicating in vivo tibial kinematics, GRFs, and tendon forces. A six-camera motion analysis system recorded the in vitro motion of ten bones in the foot. Linear mixed effects regression was used to test for differences in range of motion (ROM) by BW (75% vs. 50%) for 12 bone-to-bone relationships. Statistically significantly (p < 0.05) differences in ROM by BW were found for six of the 12 angles investigated. On average the ROM for the 75% BW simulations were systematically higher than that for the 50% BW simulations (p < .0001), but the magnitude of the difference was small (1.2˚). These results indicate that reduced BW in vitro simulations approximately model the ROM and temporal characteristic of foot bone kinematics. I. INTRODUCTION U nderstanding foot bone kinematics during the stance phase of gait is useful to further our knowledge of foot function, disease etiology, and surgical intervention efficacy. Accurately measuring foot bone kinematics in vivo is difficult however, and each method has its limitations. Motion capture of retro-reflective markers adhered to the skin is one approach but often results in grouping several bones together into one “rigid” body. For example, A. Leardini et al. grouped the navicular, lateral, middle and medial cuneiforms, and the cuboid bones into a single midfoot segment resulting in an inability to measure the motion that occurs between these bones [1]. Surface marker techniques also suffer from skin movement artifact where motion of the underlying bone can differ from the soft tissue covering it [2]. Surgical bone pins avoid these limitations by II. METHODS A. Living Subject Gait Analysis Ten healthy subjects were recruited and asked to perform five gait trails each after providing informed consent for this institutional review board approved study. A 12-camera motion analysis system (Vicon, Lake Forest, CA) sampling at 120 or 250 Hz recorded the motion of the three retroreflective markers attached to the tibia and fibula while a force plate (Bertec Corporation; Columbus, Ohio) sampling at 600 or 1500 Hz recorded the GRF. Rigid body motion of the tibia (i.e., TIB, a coordinate system constructed from anatomical landmarks of the tibia and fibula consistent with the proposed ISB standards [10]) with respect to the laboratory ground (i.e., GND, a coordinate system parallel to the force plate reference frame but with an origin located underneath the medial malleolus at heel strike) was calculated and decomposed into sagittal, frontal and transverse plane fixed angles and translations. In vivo tendon forces during stance phase were estimated Manuscript received March 21, 2011. This work was funded in part by the VA RR&D, grants A3923 and A4843C. P. M. Aubin was with the VA RR&D Center of Excellence for Limb Loss Prevention and Prosthetic Engineering, Seattle, WA 98108 USA and the Department of Electrical Engineering, University of Washington, Seattle, WA 98195 USA. He is now with the Department of Biomechanics, Vilnius Gediminas Technical University, Vilnius, Lithuania LT-03224. Eric Whittaker is with the VA RR&D Center of Excellence for Limb Loss Prevention and Prosthetic Engineering, Seattle, WA 98108 USA. William R. Ledoux is with the VA RR&D Center of Excellence for Limb Loss Prevention and Prosthetic Engineering, Seattle, WA 98108 USA and the Departments of Orthopaedics & Sports Medicine, and Mechanical Engineering, University of Washington, Seattle, WA 98195 USA. e-mail: wrledoux@u.washington.edu; phone: (1) 206-768-5347; fax (1) 206-2773963. 978-1-4577-1159-6/11/$26.00 ©2011 IEEE 653 from literature values of each muscle’s physiological cross sectional area (PCSA cm2), maximum specific isometric tension (MST N/cm2), and electromyography activity during gait (EMG % of maximum voluntary contraction) [11-14]. Muscle EMG to excitation (E) electromechanical delay dynamics were modeled by a second-order discrete linear difference equation given by (1): E(t ) EMG(t d ) 1E(t 1) 2 E(t 2) analyzed from the kinematics of the ten segment foot model. We focused on twelve clinically important angles - six in the sagittal plane, three in the frontal plane, and three in the transverse plane. For these angles, the bone-to-bone ROM was calculated as the difference between their maximum and minimum value from heel strike to toe off. (1) with coefficients, α = 0.9007, β1 = -0.0982, β2 = -0.0012, and electromechanical delay (d) = 42 ms [15]. Tendon force (FT) was calculated as the product of E, MST, PCSA, and a gain (G) equal to one (2). FT (t ) G PCSA MST E(t ) (2) B. In Vitro Kinematic Foot Model Six cadaveric specimens transected approximately 10 cm proximal to the malleoli were acquired for this study. The Achilles (Ach), tibialis anterior (TA), extensor hallucis longus (EHL), extensor digitorum longus (EDL), peroneus brevis (PB), peroneus longus (PL), posterior tibialis (PT), flexor hallucis longus (FHL) and flexor digitorum longus (FDL) tendons were dissected two cm proximal to the malleoli and their proximal ends were attached to tendon clamps. A 40-marker kinematic foot model, which has been previously described [8], was attached to the cadaveric foot (Fig. 1). Briefly, retro-reflective markers (6.4 mm) placed at specific sites with bone pins where used to create anatomical coordinate systems for the tibia (TIB), calcaneus (CAL), first metatarsal (MET1), third metatarsal (MET3), fifth metatarsal (MET5), and hallux (HAL). Quad clusters of retro-reflective markers were attached to bone pins and secured to the talus (TAL), navicular (NAV), cuboid (CUB), and medial cuneiform (CUN), with screws. For these four bones a four-marker digitizing wand was used to create embedded anatomical coordinate systems by registering the location of bony anatomical land marks to their respective quad clusters coordinate systems. During the simulation the motion of the retro-reflective markers was recorded with a six-camera motion analysis system (Vicon, Lake Forest, CA). A custom Body Builder (Vicon, Lake Forest, CA) program was written to calculate the zxy fixed angle pose of each child-segment (bone) with respect to (wrt) their parent-segment (bone) from the retroreflective marker positions, e.g., the angular pose of the HAL wrt the MET1. The kinematic data was filtered with a 10 Hz zero phase low pass Butterworth filter. A large number of bone-to-bone relationships can be Fig. 1. A cadaveric foot with the 40 marker kinematic foot model attached. Four retro-reflective markers were attached to the tibia (TIB), talus (TAL), calcaneus (CALC), navicular (NAV), medial cuneiform (CUN), first metatarsal (MET1), third metatarsal (MET3), fifth metatarsal (MET5), cuboid (CUB), and hallux (HAL) in order to track their motion via a 6camera motion analysis system during the in vitro simulation of stance phase. C. The Robotic Gait Simulator The RGS consists of a 6-DOF parallel robot (the R2000, Mikrolar Inc., Hampton, NH), nine brushless DC linear tendon force actuators (SR21 & GSX40, Exlar Corp., Chanhassen, MN), a force plate (model 9281CA, Kistler Instrument Corp.; Amherst, NY), a 6-camera motion analysis system (Vicon; Lake Forest, CA), a real time embedded controller (PXI, National Instruments Corp.; Austin, TX), and a PC with a graphical user interface (Fig. 2). To simulate gait the TIB was held fixed in space while the R2000 moved a mobile “ground” in order to recreate the relative tibia to ground motion. The R2000 is a 6-DOF parallel robot similar to a Stewart platform with six legs that actuate a mobile platform (Fig. 2, top right inset). The robot has a 2.4 m by 1.7 m footprint and net weight of 1450 kg. The mobile platform has an asymmetric working volume of roughly ± 100 mm translation in the x-, y-, and z-axis and ± 15° rotation around the x-, and y-axis and ± 360° rotation around the z-axis. The manufacturer specified accuracy and repeatability are approximately 50 μm and 25 μm, respectively. Its parallel construction provides high stiffness and allows for a 227 kg payload. A robust steel frame surrounding the R2000 mechanically grounds the base of the robot to the laboratory floor and also acts as a rigid support for the tibial mounting frame. Attached to the mobile platform via a 654 Fig. 2. The robotic gait simulator with surrounding frame (A), R2000 parallel robot (top right inset), R2000 motor (B, one of six), mobile force plate (C), cadaveric foot (D), mobile top plate (E), tibia mounting device (F), force control tendon actuators (G), 6-camera motion analysis system (H, only one camera shown), tendon pull control cable (I), and tendon freeze clamp (J). custom steel frame is a force plate that acts as the “ground” and moves relative to the static cadaveric TIB. Six brushless DC motors control the pose of the mobile platform. Unlike a traditional Stewart platform, the R2000’s legs have a fixed length; the position and orientation of the mobile platform are controlled by the legs rotating around a circular steel rim attached to the base of the robot. Tendon force was provided by a nine axis tendon actuation system which consists of nine linear actuators (SR21 & GSX40, Exlar Corp., Chanhassen, MN) in series with nine load cells (Transducer Techniques Inc., Temecula, CA). Control cables were routed from the load cells to custom tendon clamps (Fig. 2). The tendon actuation system operated in force control mode. A PID controller operating on the PXI controller measured tendon force in real time and made appropriate adjustments to the motor current in order to track the target tendon forces. The in vitro vGRF was controlled by a fuzzy logic controller (FLC) which has been previously described in detail [16]. Briefly, the FLC made adjustments to the R2000 kinematics, Ach tendon force, and TA tendon force in order to track the desired vGRF. The FLC had three inputs: percent stance phase, vGRF error, and the integral of the vGRF error. The outputs of the FLC were a change in Ach force, a change in TA force, and a change in the mobile force plate translational kinematics. Adjustments to the target tendon forces were performed in real time while adjustments to the R2000 kinematics were done iteratively, similarly to a previously developed iterative learning vGRF controller [17]. clamps were used for the other tendons. The motion analysis system was used to measure the pose of the tibia wrt the R2000 base frame. An optimization algorithm was used to determine the optimum tibial pose which would minimize the required R2000 motor velocity during the simulation [16]. The optimization allowed the simulation to occur in the desired 2.782 s, or 4 times slower than in vivo gait. Several initial simulations were performed at a reduced vGRF to verify proper system operation. The vGRF was then manually increased iteratively by increasing the tendon force gain G in (2) and by adjusting a translational superiorinferior offset parameter in the trajectory until the vGRF was within approximately ± 10% of the target vGRF. Manual control of the vGRF was then halted and the FLC was enabled for subsequent simulations in order to track the target vGRF with high fidelity. Each cadaveric specimen was tested at both 50% BW and 75% BW. At each BW three quartets of simulations were performed. Each quartet consisted of four iterative simulations, where the first three simulations of the quartet allowed the FLC to iteratively improve the vGRF tracking. During the fourth and final simulation of the quartet the motion of the retro-reflective markers were recorded at 200 Hz and saved for post analysis. E. Statistical Analysis Linear mixed effects regression was used to test for differences in ROM by BW (75% vs. 50%) for twelve important bone-to-bone relationships. ROM was the dependent variable, BW was the independent fixed effect and cadaveric foot and cadaveric foot x BW interaction were random effects. To assess the effect of BW on ROM for all angles (17 bone-to-bone relationships in three planes each or 51 angles) together, linear mixed effects models were carried out combining all 51 angles into one model, as above, with D. Cadaveric Gait Simulation Each cadaveric specimen was mounted into the RGS via the tibia mounting device. A freeze clamp [18] was used to attach the Ach tendon to its actuator while non-freezing 655 TABLE I. MEAN RANGE OF MOTION (ROM) AND THE STANDARD ERROR (SE) OF THE MEAN FOR 12 BONE-TO-BONE RELATIONSHIPS. STATISTICALLY SIGNIFICANT DIFFERENCES IN ROM (P < 0.05) ARE SHOWN IN BOLD. 50% BW 75% BW difference ROM ROM bone ½–¾ mean mean with respect to (-) [SE] [SE] bone p-value [SE] the addition of joint/plane as fixed effects covariates, and random effects foot, joint/plane within foot, and joint/plane x BW interaction. Analyses were carried out using R 2.11.1 [19]. III. RESULTS Sagittal plane The RGS was able to recreate the physiological characteristics of gait. The mean tibia wrt ground angles in the sagittal, frontal, and transverse planes were entirely within ± 1 SD of the target in vivo tibia angles for both the 50% BW and 75% BW simulations. The in vitro vGRF also closely match that of the living subjects. For the 50% BW simulations the average RMS error between the target in vivo and actual in vitro vertical, medial/lateral and anterior/posterior GRF was 5.1% BW, 1.8% BW and 3.7 % BW, respectively. The 75% BW simulations had similar GRF tracking results with RMS tracking errors of 5.9% BW, 3.6% BW, and 4.0% BW for the vertical, medial/lateral and anterior/posterior GRF, respectively. The average RMS tracking error for all tendons except for the fuzzy logic controlled TA and Ach was 3.6 N and 3.9 N for the 50% BW and 75% BW simulations, respectively. The mean and the standard error (SE) of the mean ROM for 12 bone-to-bone relationships was calculated for both the 50% BW and 75% BW simulations (Table I, Fig. 3 - 4). The difference (75% BW - 50% BW) in the mean ROM ranged from 0.7° for the TAL wrt the TIB in the sagittal plane to a maximum of 6.7° for the HAL wrt the MET1 in the sagittal plane. The linear mixed effects regression found statistically significant differences in ROM by BW for six of the 12 angles investigated (Table I). In the sagittal plane statistically significant differences were found for the MET1 wrt the TAL (3.7° ROM difference; p=.0002) and for the HAL wrt the MET1 (6.7° ROM difference; p=.0061). In the frontal plane statistically significant differences were found for the CALC wrt the TAL (1.4° ROM difference; p=.016) and NAV wrt the TAL (2.9° ROM difference; p=.0056). In the transverse plane, statistically significant differences in ROM were found for the MET1 wrt TAL (3.1° ROM difference; p=.0059) and for the NAV wrt the TAL (2.7° ROM difference; p=.014). The model combining ROM measures for all 51 bone-tobone relationships (1707 individuals ROM measurements) found that on average the ROM for the 75% BW simulations was systematically higher than that for the 50% BW simulations (p < .0001), although the magnitude of the difference was small (1.2˚) (Table I). CALC - TIB 22.0 [3.0] 23.6 [2.9] 1.6 [0.8] .057 TAL - TIB 22.5 [2.0] 23.2 [1.9] 0.7 [0.7] .3 NAV - TAL 8.4 [1.8] 9.6 [1.9] 1.2 [0.7] .094 CUN - NAV 11.0 [1.2] 12.2 [0.9] 1.2 [0.6] .062 MET1 - TAL 18.9 [2.6] 22.6 [2.7] 3.7 [0.6] .0002 HAL - MET1 55.2 [3.0] 61.9 [2.8] 6.7 [1.9] .0061 CALC - TIB 8.2 [0.9] 9.2 [1.3] 1.0 [0.6] .11 CALC – TAL 7.1 [0.7] 8.6 [1.1] 1.4 [0.5] .016 NAV –TAL 15.9 [1.9] 18.8 [2.1] 2.9 [0.8] .0056 Frontal plane Transverse plane CALC - TAL 5.4 [0.7] 6.2 [0.9] 0.8 [0.4] .086 NAV – TAL 12.2 [1.7] 14.9 [2.4] 2.7 [0.9] .014 MET1 – TAL 16.3 [1.3] 19.4 [1.6] 3.1 [0.9] .0059 1.2 [0.2] <.0001 All angles combined In general the temporal joint motions patterns were similar between the 50% BW and 75% BW conditions. For example, motion of the talotibial joint (TAL wrt the TIB) in the sagittal plane plantar flexed at heel strike then dorsiflexed during midstance and finally plantar flexed again during push off for both the 50% BW and 75% BW tests (Fig. 5, top plot). CALC wrt the TAL in the frontal plane and MET1 wrt the TAL in the transverse plane are also representative, with minimal changes in the kinematics between the 50% BW and the 75% BW simulations (Fig. 5, middle and bottom plot). Fig. 3. Mean ± 1 SE sagittal plane range of motion (ROM) for the 50% body weight (BW) (empty squares) and 75% BW (black circles) simulations. 656 associated with walking and the fragility of cadaveric specimens has resulted in routinely testing specimens at reduced BWs, the effects of which are unknown. For this study, we sought to determine if foot bone kinematics during the stance phase of gait differ between a 50% BW and a 75% BW simulation. Our study results suggest that differences in foot bone kinematics between the BW simulations are small and often less than a couple of degrees. This implies that reduced BW simulations of the stance phase of gait are able to approximately model in vivo foot kinematics. The inability to test the cadaveric feet at 100% BW is one limitation of this study. Ideally we would have been able to test the cadaveric feet at 100%, 75% and 50% BW. While the RGS is able to deliver the force required to test at 100% BW, we instead tested at lower forces because one of the earlier tested specimens failed at 100% BW. Our results, however, still provide new insight into how scaling the vGRF affects foot kinematics. The differences between 75% and 100% BW are likely similar to the minimal differences discovered between 50% and 75%. Furthermore, our results facilitate other research groups trying to weigh the advantages and disadvantages of testing at large or small BWs which until now have been unknown. Another limitation of this study is the accuracy and precision to which the joint angles were measured. The 40marker foot model employed in this study pushes the boundary of what is currently possible for in vitro foot models. Many of the bone measured are in close proximity to one another, have small feature sizes, and have minimal angular movement. Camera settings (position, alignment focal length, aperture and infrared strobe intensity), bone pin rigidity, retro-reflective marker size, and anatomical coordinate system construction all affect the accuracy and precision of the recorded kinematics. Some of the variability in the results is likely due to these limitations. The ROM of HAL wrt MET1 in the sagittal plane for both the 50% BW and 75% BW simulations was greater than the 42° ROM previously reported by Nawoczenski et al. [20]. Interestingly, HAL wrt the MET1 also had the largest difference in ROM between 50% BW and 75% BW. Two reasons may explain these findings. First, the TIB wrt GND kinematics were held constant and equal to the in vivo TIB kinematics for all cadaveric specimens even though interspecimen foot size differences were present, as were size differences between the cadaveric feet and the living subject’s feet. Thus, a smaller than average cadaveric foot would have had greater ankle plantar flexion to maintain contact with the ground during late stance which would have led to greater HAL dorsiflexion. Secondly, and perhaps more importantly, the intrinsic musculature of the foot was not actuated in this study. The flexor hallucis brevis, for example, is a plantar flexor of HAL, and if actuated it would have likely stabilized and limited the sagittal plane ROM of the great toe. An important implication of this finding is that joints that are not actively articulated by intrinsic muscles, Fig. 4. Mean ± 1 SE frontal and transverse plane range of motion (ROM) for the 50% body weight (BW) (empty squares) and 75% BW (black circles) simulations. Fig. 5. Joint motion from one cadaveric foot for the three 50% BW (black lines) and three 75% BW (gray lines) simulations. The plots shown are the talotibial joint (TAL wrt TIB) in the sagittal plane (top), the subtalar joint (CALC wrt TAL) in the frontal plane (middle), and the first metatarsal with respect to the talus (MET1 wrt TAL) in the transverse plane (bottom). These representative figures demonstrate the similarity of the joint’s motion between different BW simulations indicating that the kinematics of the joint are well modeled at reduced BW. IV. DISCUSSION Cadaveric robotic gait simulators are useful to investigate the biomechanics of the foot and ankle. The large forces 657 [5] such as the naviculo-cuneiform joint, are better modeled by, and less sensitive to, the limitations associated with dynamic cadaveric gait simulators as compared to other segments articulated by intrinsic musculature such as the metatarsophalangeal joints. The results of this study can be used to facilitate the design and development of future robotic cadaveric simulators. Designing a high force system is often more complex and expensive than a comparable low force system. These results can aid future investigators in performing a cost benefit analysis for their designs. The utility of robotic technologies was also demonstrated. Specifically, the robotic methodology we used allowed for precise and accurate kinematic control, complex force control, and good experimental repeatability. The implications of this study should be use cautiously. While joint kinematics have been shown to have low sensitivity to the applied vGRF, that is not to say that scaling the vGRF is in general not a limitation of dynamic cadaveric robotic gait simulation studies. Many investigators have used cadaveric robotic gait simulators to investigate a variety of parameters ranging from bone strain [21] to midfoot joint pressure [4] to plantar fascia strain [22]. It is important to keep in mind that other biomechanical properties may be more sensitive to vGRF than foot bone kinematics. [6] [7] [8] [9] [10] [11] [12] [13] V. CONCLUSION [14] Differences in foot bone kinematics during the stance phase of gait at 50% BW and 75% BW were quantified using a robotic cadaveric gait simulator. While some statistically significant differences in ROM were found, in general the differences were small and are likely comparable to the accuracy of many kinematic foot models. When designing their experimental protocols, investigators can use these results to evaluate the advantages and disadvantages of testing at reduced BW. [15] [16] [17] [18] ACKNOWLEDGMENT The authors would like to thank Jane Shofer for her generous help with the statistical analysis of the ROM data. [19] REFERENCES [20] [1] [2] [3] [4] A. Leardini, M.G. Benedetti, L. Berti, D. Bettinelli, R. Nativo, and S. Giannini, “Rear-foot, mid-foot and fore-foot motion during the stance phase of gait,” Gait & Posture, vol. 25, Mar. 2007, pp. 453462. N. Okita, S.A. Meyers, J.H. Challis, and N.A. Sharkey, “An objective evaluation of a segmented foot model,” Gait & Posture, vol. 30, Jul. 2009, pp. 27-34. P. Lundgren, C. Nester, A. Liu, A. Arndt, R. Jones, A. Stacoff, P. Wolf, and A. Lundberg, “Invasive in vivo measurement of rear-, mid- and forefoot motion during walking,” Gait & Posture, vol. 28, Jul. 2008, pp. 93-100. D.G. Lee and B.L. Davis, “Assessment of the effects of diabetes on midfoot joint pressures using a robotic gait simulator,” Foot & Ankle International / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society, vol. 30, Aug. 2009, pp. 767772. [21] [22] 658 C. Hurschler, J. Emmerich, and N. Wülker, “In vitro simulation of stance phase gait part I: Model verification,” Foot & Ankle International / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society, vol. 24, Aug. 2003, pp. 614-622. K. Kim, H. Kitaoka, Z. Luo, S. Ozeki, L. Berglund, K. Kaufman, and K. An, “In Vitro Simulation of the Stance Phase in Human Gait,” Journal of Musculoskeletal Research, vol. 5, Jun. 2001, pp. 113-122. C.J. Nester, A.M. Liu, E. Ward, D. Howard, J. Cocheba, T. Derrick, and P. Patterson, “In vitro study of foot kinematics using a dynamic walking cadaver model,” Journal of Biomechanics, vol. 40, 2007, pp. 1927-1937. E. Whittaker, P. Aubin, and W. Ledoux, “Foot Bone Kinematics as Measured in a Cadaveric Robotic Gait Simulator,” Gait & Posture, vol. in press, 2011. N. Wülker, C. Hurschler, and J. Emmerich, “In vitro simulation of stance phase gait part II: Simulated anterior tibial tendon dysfunction and potential compensation,” Foot & Ankle International / American Orthopaedic Foot and Ankle Society [and] Swiss Foot and Ankle Society, vol. 24, Aug. 2003, pp. 623-629. G. Wu, S. Siegler, P. Allard, C. Kirtley, A. Leardini, D. Rosenbaum, M. Whittle, D.D. D'Lima, L. Cristofolini, H. Witte, O. Schmid, and I. Stokes, “ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion--part I: ankle, hip, and spine. International Society of Biomechanics,” Journal of Biomechanics, vol. 35, Apr. 2002, pp. 543-548. R.A. Brand, D.R. Pedersen, and J.A. Friederich, “The sensitivity of muscle force predictions to changes in physiologic cross-sectional area,” Journal of Biomechanics, vol. 19, 1986, pp. 589-596. T. Fukunaga, R.R. Roy, F.G. Shellock, J.A. Hodgson, and V.R. Edgerton, “Specific tension of human plantar flexors and dorsiflexors,” Journal of Applied Physiology (Bethesda, Md.: 1985), vol. 80, Jan. 1996, pp. 158-165. M. Pierrynowski, “A Physiological Model For The Solution Of Individual Muscle Forces During Normal Human Walking,” Fraser University, 1982. T.L. Wickiewicz, R.R. Roy, P.L. Powell, and V.R. Edgerton, “Muscle architecture of the human lower limb,” Clinical Orthopaedics and Related Research, Oct. 1983, pp. 275-283. D.G. Lloyd and T.F. Besier, “An EMG-driven musculoskeletal model to estimate muscle forces and knee joint moments in vivo,” Journal of Biomechanics, vol. 36, Jun. 2003, pp. 765-776. P. Aubin, “The Robotic Gait Simulator: A Dynamic Cadaveric Foot and Ankle Model for Biomechanics Research,” University of Washington, 2011. P. Aubin, M. Cowley, and W. Ledoux, “Gait Simulation via a 6DOF Parallel Robot With Iterative Learning Control,” Biomedical Engineering, IEEE Transactions on, vol. 55, 2008, pp. 1237-1240. N.A. Sharkey, T.S. Smith, and D.C. Lundmark, “Freeze clamping musculo-tendinous junctions for in vitro simulation of joint mechanics,” Journal of Biomechanics, vol. 28, May. 1995, pp. 631635. Development Core Team, R: A language and environment for statistical computing, Vienna, Austria: R Foundation for Statistical Computing, 2010. D.A. Nawoczenski, J.F. Baumhauer, and B.R. Umberger, “Relationship between clinical measurements and motion of the first metatarsophalangeal joint during gait,” The Journal of Bone and Joint Surgery. American Volume, vol. 81, Mar. 1999, pp. 370-376. S.W. Donahue, N.A. Sharkey, K.A. Modanlou, L.N. Sequeira, and R.B. Martin, “Bone strain and microcracks at stress fracture sites in human metatarsals,” Bone, vol. 27, Dec. 2000, pp. 827-833. E.D. Ward, K.M. Smith, J.R. Cocheba, P.E. Patterson, and R.D. Phillips, “2003 William J. Stickel Gold Award. In vivo forces in the plantar fascia during the stance phase of gait: sequential release of the plantar fascia,” Journal of the American Podiatric Medical Association, vol. 93, Dec. 2003, pp. 429-442.