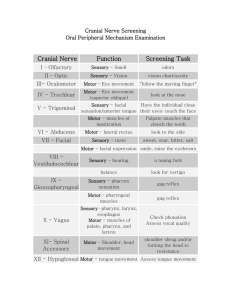
Huntington's Disease – A. Cause: Hereditary (too much dopamine) B. Prognosis: Progressive, fatal (Usually w/in 15 years of onset of symptoms) C. Signs: Large amts. of huntingtin protein builds up in the basal nuclei & eventually the cerebral cortex, causing tissue degeneration & death D. Symptoms: Chorea - Continual, involuntary movement. Hyperkinesis Eventually marked mental deterioration E. Treatment: No cure 1. Medications that block the effect of dopamine in the basal nuclei 2. +/- stem cell research to provide fetal tissue implantation of basal nuclei II. Parkinson's Disease – A. Cause: Unknown (too little dopamine) B. Signs: Degeneration of dopamine-releasing neurons in the substantia nigra, causing over-activity of the basal nuclei C. Symptoms: Persistent tremor, awkward posture, shuffling gait, slow initiation of movement, stiff facial expression D. Treatment: No cure 1. L-dopa can alleviate symptoms but has bad SEs, & eventually becomes ineffective 2. Deprenyl is safer with fewer SEs 3. +/- stem cell research to explore intra-brain transplants of dopamine-producing cells III. Alzheimer's Disease – A. Cause: Unknown (Genetics plays a role) B. Prognosis: Progressive, eventually fatal C. Signs: ACh shortage, & structural changes in brain areas involved with memory & cognition 1. Neuronal degeneration. Plaques of beta amyloid peptide & tangles of tau 2. Increased Ca++ influx into neurons D. Symptoms: Memory loss, decreased attention span, language loss, personality changes, hallucinations, mental deterioration E. Treatment: No cure 1. Medications inhibiting ACh breakdown help alleviate symptoms I. I. Peripheral nervous system: Provide brain with link to environment A. Sensory receptors (Afferents) B. Peripheral nerves - Cranial & spinal nerves (& associated ganglia) C. Efferent motor endings D. Cranial nerves: (emanate from ventral surface of brain & extend out foramen magnum) 12 pair – a. 1st 2 - Optic (II) & Olfactory (I) originate from forebrain b. All others extend from brain stem c. Vagus (X) extends into abdomen d. All others innervate only the head & neck. 1. Olfactory (I) – a. Sensory (smell) b. From nasal mucosa to olfactory bulbs c. Olfactory bulbs & tracts are really brain structures d. Terminates in frontal lobe of cortex 2. Optic (II) – a. Sensory (vision) b. Actually part of the optic tract (brain structure) to optic chiasma to.... c. terminate in occipital lobe of cortex 1 3. Oculomotor (III) – a. Motor (mostly) b. Extrinsic eyeball muscles, lens accommodation, pupil constriction c. Has some parasympathetic fibers Motor PS to iris constrictors & lens shapers from midbrain d. From midbrain to eyeball muscles 4. Trochlear (IV) – a. Motor (mostly) b. Extrinsic eyeball muscles c. From midbrain to eyeball muscles 5. Trigeminal (V) – a. Sensory & motor b. Largest c. Three branches: Sensory to face (Touch, pain, temp.) From face to pons Motor to muscles of mastication To muscles of mastication from pons 6. Abducens (VI) – a. Motor (mostly) b. Abduction (Lateral movement) of eyeball c. From Pons to orbital muscles 7. Facial (VII) – a. Sensory & motor b. Motor to facial muscles (facial expression) From pons to facial skeletal muscles c. Sensory to tongue (taste) From taste buds to pons d. Has some parasympathetic fibers Motor PS impulses to tear & salivary glands 8. Vestibulocochlear (auditory or acoustic) (VIII) – a. Sensory b. Hearing & balance c. From Inner ear to brain stem 9. Glossopharyngeal (IX) – a. Sensory & motor b. Sensory to tongue (taste) Sensory fibers from pharyngeal muscles & posterior tongue to medulla From Chemoreceptors in carotid sinus (to monitor CO2 & O2 levels) to medulla c. Motor to pharynx From medulla to pharyngeal muscles d. Swallowing, gag reflex, salivary glands e. Has some parasympathetic fibers Motor PS fibers to parotid salivary gland from medulla 10. Vagus (X) – a. Sensory & motor b. Extends to thorax & abdomen c. Sensory (taste) 2 From posterior tongue & pharynx to medulla. d. Motor (swallowing) To skeletal muscles of pharynx & larynx from medulla. e. Autonomic NS functions (has parasympathetic fibers) Motor PS fibers from medulla to heart, lungs, abdominal viscera Sensory PS from abdominal & thoracic viscera to medulla Sensory PS from pressoreceptors in carotid sinus (blood pressure regulation) & chemoreceptors in carotid & aortic bodies (respiratory regulation) f. Innervates visceral muscles (see above) 11. Accessory (spinal accessory) (XI) – a. Motor (mostly) b. Joins with a spinal nerve, which innervates large neck muscles from medulla c. Motor (swallowing) Joins with Vagal branches to larynx, pharynx, & soft palate from medulla 12. Hypoglossal (XII) – a. Motor (mostly) b. Muscles of tongue (speech & swallowing) From medulla to tongue muscles E. Spinal Nerves - From SC to supply all body parts except head & neck 1. 31 pair 2. All are mixed nerves (sensory & motor) 3. Named according to where they originate in the SC a. Cervical-Spinal - (C1-C8) - 8 pair b. Thoracic - (T1-T12) - 12 pair c. Lumbar - (L1-L5) - 5 pair d. Sacral - (S1-S5) - 5 pair e. Coccygeal - (C0) - 1 pair 4. Connect to the SC by a ventral root (motor) & dorsal root (sensory) a. Ventral root fibers - (also contain some ANS efferent fibers) From anterior horn neurons Innervate skeletal muscles b. Dorsal root fibers – From sensory neurons in dorsal root ganglia Conduct impulses from peripheral sensory receptors to SC c. Both roots join prior to emerging from the vertebral column 5. Divide into (small) dorsal ramus, (large) ventral ramus, & tiny meningeal branch a. Each ramus is mixed (sensory/motor) b. Dorsal rami supply voluntary muscles & skin of the back c. Ventral rami supply rest of trunk & limbs Most ventral rami join into complex nerve plexuses in the cervical, brachial, lumbar, & sacral regions & serve the limbs Advantage - When one segment is damaged, an entire limb is not paralyzed Ventral rami of T1-T12 form the intercostal nerves Give off cutaneous branches to the skin 6. Cervical Plexus - (1st 4 cervical nerves) – a. Most cutaneous sensory (superficial) to neck, ear, back of head, & shoulder b. Some motor (deep) to anterior aspect of neck Phrenic nerve - Motor & sensory to diaphragm 3 7. Brachial Plexus – Very large, complex. Formed by the 5 ventral rami of C5-T1 Upper, middle, & lower trunks (small nerve fibers branch off continually Anterior & posterior divisions of each along the way to supply muscles/skin of shoulder & thorax) Lateral, medial, posterior cords Ends in the axilla to give rise to the main 5 limb nerves a. Axillary - Shoulder muscles (deltoid, teres minor), joint capsule, skin b. Musculocutaneous – Biceps, brachialis, & cutaneous to lateral forearm c. Median – Flexors, skilled wrist/finger movements, & cutaneous to anterior forearm d. Ulnar – Medial hand/wrist muscles & skin e. Radial – Upper limb extensors, among others 8. Lumbar plexus – (lumbosacral plexus) – Overlapping fibers of spinal nerves L1-L4 & L4-S4 a. Parts of abdominal wall b. Anterior & medial thigh – Femoral nerve - Thigh flexors & knee extensors Opturator nerve – Adductor muscles 9. Sacral plexus – (L4-S4 immediately caudal to the lumbar plexus) a. Pelvic structures & perineum Gluteal nerves (superior & inferior) – Pelvic area Pudendal nerve – Perineum b. Buttocks & lower limb Sciatic nerve (Tibial & Common Fibular – Diverge just proximal to the knee) – Thigh extensors, knee flexors, & adductor Tibial nerve – Posterior lower leg Common Fibular nerve – (Superficial & deep) – Knee joint & anteriolateral leg 4 10. Dermatome – The area of skin innervated by a single spinal nerve a. Every spinal nerve but C1 innervates a dermatome b. Uniform, almost horizontal, in-line w/spinal nerve Ventral rami of C5-T1-2 – Skin of upper limbs Lumbar nerves – Anterior thighs & legs Sacral nerves – Posterior surfaces of lower limbs 11. Joint Innervation – a. Hilton’s law – Any nerve serving a muscle causing movement at a joint also innervates that joint & the skin covering it b. Peripheral Motor Endings - (neurotransmitters) - Descending efferent circuits c. Neuromuscular junction - The area of innervation of somatic skeletal muscle (effectors) d. Axon terminals - Contain synaptic vesicles with ACh (Acetylcholine) Remember transmission of nerve impulses via neurotramsmitters! e. Autonomic nerve junctions - Between ANS (motor endings) & visceral effectors Visceral effectors = Smooth & cardiac muscle + visceral glands Varicosities - Knob-like swellings w/ synaptic vesicles & mitochondria Contain ACh or norepinephrine Synaptic cleft is wider, so visceral motor responses usually slower 12. Motor integration – a. Cerebral cortex - Conscious motor pathways b. Cerebellum + basal nuclei = Ultimate planner & coordinator of complex motor activity Fixed action patterns - Stereotyped, sequential motor actions triggered internally, or by appropriate environmental $ c. Segmental - Lowest circuit Spinal cord circuits - Anterior horn neurons within a single SC segment, which $ a specific group of muscle fibers Central Pattern Generators (CPGs) - Circuits controlling locomotion & frequently repeated motor activities d. Projection - Upper motor neurons of the motor cortex which initiate the direct (pyramidal) system + brain stem motor areas over-seeing the indirect (multi-neuronal) system Project to the SC & help control reflex & fixed-action motor activity + discrete, voluntary skeletal muscle movement Send information about what's happening to the higher command centers e. Pre-command - Highest level (Cerebellum & basal nuclei) - Control outputs of the cortex & brain stem motor centers. Cortex says " I wanna move my toe", then pre-command areas take over to lay the groundwork for the movement (Provide proper timing/pattern) Then, the cortex decides whether to go through with it. (carry out the command) Precisely start/stop movements Coordinate movement w/ posture Block unwanted movement Monitor muscle tone Cerebellum is the key center for sensorimotor integration & control Basal nuclei - Involved in more complex actions Inputs from all cortical areas, sending output to premotor & prefrontal areas 5