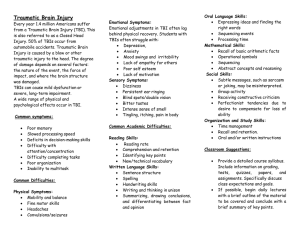
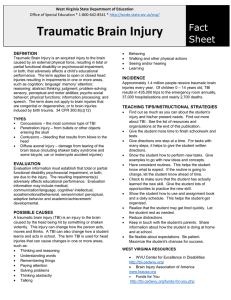
COGNITIVE-COMMUNICATION THERAPY IN TBI POPULATION: FUNCTIONAL BASED INTERVENTION AND GOAL PLANNING 2018 KSHA CONFERENCE – WICHITA, KS OCTOBER 5, 2018 LESLEY TILLEY, M.S., CCC-SLP FINANCIAL DISCLOSURE • Full Time Position year round NONFINANCIAL DISCLOSURE • No financial or nonfinancial relationships exist with the research or resources cited in this presentation. https://vimeo.com/mindsmatter/joshsjourney JOSH’S JOURNEY OBJECTIVES • The learner will be able to describe the community-based model of intervention for persons with TBI. • The learner will be able to list benefits and outcomes of this approach to the TBI population. • The learner will be able to demonstrate the process involved in functional goal planning. TRAUMATIC BRAIN INJURY DEFINITION • Traumatic brain injury (TBI) is defined as sudden trauma, such a blow or jolt to the head that disrupts the normal function of the brain. The severity of a TBI may range from “mild” to “severe”. (www.cdc.gov) TRAUMATIC BRAIN INJURY DEFINITION • A closed brain injury is trauma to the brain as a result of the brain being violently shaken within the skull. (ex. Concussion) • Penetrating head injury is trauma to the brain as a result of an object being projected through the skull into the brain. (ex. Gunshot wound) • Post-Concussion Syndrome is defined as a complex disorder in which various symptoms — such as headaches and dizziness — last for weeks and sometimes months after the injury that caused the concussion. FACTS ABOUT TRAUMATIC BRAIN INJURY Brain injury is known as the silent epidemic Approximately 5.3 million Americans are living with a TBI-related permanent disability Every 23 seconds one person in the U.S. will sustain a TBI Males sustain more TBIs than females (more than 1.5 times more) Falls are the #1 cause of TBI (The Essential Brain Injury Guides 2009) SPECTRUMS OF BRAIN INJURY (MILD, MODERATE, SEVERE) Mild Brain Injury A mild brain injury, also known as “concussion” is one in which there is only a brief or momentary loss of consciousness if any without any major complications. This is often followed by “postconcussion syndrome” that can include temporary headaches, dizziness, mild mental slowing and fatigue. Mild Brain Injury The most important element in the management of mild brain injury is recognizing that the symptoms are real and can be treated. Symptoms of mild brain injury almost always improve over 1-3 months. Mild Brain Injury Mild TBI may also result in word-finding difficulties, decreased motivation, anxiety, depression, and irritability (Levin, Eisenberg, & Benton, 1989; Sohlberg & Mateer, 1989a). Symptoms following mild TBI are quite variable and may include difficulty concentrating under distracting conditions or problems managing tasks involving multiple demands. Moderate Brain Injury Results in a loss of consciousness usually lasting only minutes or a few hours followed by a few days or weeks of confusion. It may be accompanied by brain contusions or hematomas. Moderate Brain Injury Persons sustaining a moderate brain injury will usually have cognitive and psychosocial impairments that can last for many months. With treatment these individuals are generally able to make a nearly complete recovery. Severe Brain Injury Severe brain injury almost always results in prolonged unconsciousness or coma lasting days, weeks or even longer. Such persons often have brain contusions, hematomas or damage to the nerve fibers or axons, and some may have suffered from anoxia. Severe Brain Injury Persons who sustain a severe TBI can make significant improvements in the first year after injury and can continue to improve at a slower pace for many years, and will often be left with some permanent physical, behavioral and/or cognitive impairments. Severe Brain Injury The consequences of severe TBI can affect all aspects of an individual’s life (socially, physically, psychologically). (J Head Trauma Rehabil 1999) This can include relationships with family and friends, as well as their ability to work or be employed, do household tasks, drive, and/or participate in other activities of daily living. SEVERITY QUOTE “Many professionals and family members feel that the severity of the actual injury and the severity of the problems or consequences do not necessarily match the strict definitions of mild, moderate and severe.” (The Essential Brain Injury Guide 2009) https://askabiologist.asu.edu/brain-regions AREAS OF BRAIN FUNCTIONS AREAS OF FOCUS FOR TBI INTERVENTION https://brainandcommunication.ca/who-benefits-from-speech-language-pathology/ COGNITIVE-COMMUNICATION DEFINITION Impairments of communication related to linguistic and nonlinguistic cognitive functions LINGUISTIC: NONLINGUISTIC: SYNTAX SEMANTICS WRITTEN READING NONVERBAL MESSAGES ATTENTION PROBLEM SOLVING REASONING MEMORY EXECUTIVE FUNCTIONING ASHA 1996 80-100 PERCENT OF PEOPLE WHO HAVE A TBI ALSO HAVE A COMMUNICATION DISORDER https://simonefriedmansls.com/traumatic-brain-injury/4165463044/ COGNITIVE-COMMUNICATION The goal of intervention in traumatic brain injury (TBI) is to achieve the highest level of independent function for participation in daily living. Cognitive-communication treatment approaches in TBI focus either on restoration of skills or compensation for difficulties. Treatments can also be specific to retraining discrete cognitive processing components. Asha.org SLP’S ROLE IN INTERVENTION WITH TBI POPULATION • Identify current communication barriers and if and how they may affect job performance and provides or trains rehabilitation strategies to minimize the impact of those barriers in functional settings (Bonelli, Ritter, & Kinsler, 2007). • Establish treatment programs to decrease the effects of impairments in all aspects of communication. SLP’S ROLE IN INTERVENTION WITH TBI POPULATION • Identify effective and functional supports to enable individuals to be as independent and successful as possible. • Facilitates carryover of treatment objectives within context of environment. COMMUNITY INCLUSION AFTER BRAIN INJURY • The best rehabilitation happens in a setting where the individual is most likely to reach his or her immediate goals. • The optimal setting should be suited to the individual’s stage in the recovery process. (JANET WILLIAMS : COMMUNITY INCLUSION AFTER BRAIN INJURY(2015)) COMMUNITY INCLUSION AFTER BRAIN INJURY • By participating in regular routines with the support of rehabilitation professionals, individuals can make progress in a real world environment. • By supporting people at home by providing services needed for self-sufficiency and community membership, there’s a significant long-term savings. (JANET WILLIAMS : COMMUNITY INCLUSION AFTER BRAIN INJURY(2015)) LITERATURE REVIEWS – EFFECTIVENESS OF COMMUNITY BASED INTERVENTION • Published 2010: Effectiveness of Community-Based Rehabilitation After TBI for 489 Program Completers Compared With Those Precipitously Discharged • Study Objective: Evaluate outcomes of home and community based postacute brain injury rehab • Conclusion to Study: Showed significant positive changes from admission to discharge for those completed course of rehab compared to those discharged suddenly, gains were maintained 3 and 12 months after discharge LITERATURE REVIEWS – EFFECTIVENESS OF COMMUNITY BASED INTERVENTION • Published 2004: Community Integration and Satisfaction With Functioning After Intensive Cognitive Rehabilitation for TBI • Study Objective: Evaluate the effectiveness of an intensive cognitive rehab program (ICRP) compared to standard neurorehab (SRP) for persons with TBI • Conclusion to Study: Intensive, holistic, cognitive rehab is an effective form of rehab for TBI. ICRP participants over twice as likely to show clinically significant improvement in community integration as those receiving SRP. Improvement in overall neuropsychologic functioning LITERATURE REVIEWS – EFFECTIVENESS OF COMMUNITY BASED INTERVENTION • Published 2017: TBI Case Study: Effectiveness of Home and Community-Based Rehabilitation Services Using Consumer-Driven Goal Planning • Study Objective: Identify level of functioning post injury and at discharge following high intensity collaborative rehabilitation between therapists and the consumer. Use of International Classification of Functioning (ICF) model for analysis. • Conclusion to Study: This model of TBI rehabilitation proved effective for the individual as he made substantial gains across expressive and receptive communication skills, physical function, ADLs and IADLs, including management of finances and health maintenance needs. Allowed individual to attain functional outcomes of their choosing resulting in an overall increase in participation in society and improved quality of life. Additionally, this individual achieved independent living in the community and maintained steady employment for multiple years. MODELS TO THERAPY APPROACH MEDICAL MODEL • Professional determining goals • Uses objective, standardized measures for methods of treatment • Condition is labeled • Options for control held by expert or other representative • Treated in separate facilities INDEPENDENT LIVING MODEL • Consumer driven goals • Know themselves the best • Right to make own decisions and problem solve when mistakes occur • Less emphasis on label of disability, more on person’s strengths and needs • Nothing for me without me approach (The Essential Brain Injury Guide 2009) BENEFITS AND OUTCOMES OF APPROACH • Person centered • Focus on strengths, not difficulties • Goals set by the person, not the professional. • Related to functional skill in their natural environment • Life changing transition • Measurable • Achievable http://careerfitone.com/for-students/abilities-and-the-whole-person/ EXAMPLE OF FUNCTIONAL BASED INTERVENTION AND INDEPENDENT LIVING MODEL Josh, 37 yrs old Experienced a severe TBI in 2013 due to a MVA. Received rehab services in a rehab facility in the TBI unit for 4 months. Josh received speech therapy services on the HCBS waiver from March 2014 to July 2018 JOSH’S GOALS Long-term Goals: • In 8 weeks, I want identify a counselor that has experience with TBI and decrease mood swings/anger. • In 8 weeks, I want to find a job. • In 16 weeks, I want to live on my own. • In 16 weeks, I want to be able to get out of the house more and do more socializing. • In 24 weeks, I want help communicating with my words for times when I get stuck so I am able to interact with others in my community and at work • In 24 weeks, I want to have less frustration when I speak. I want to communicate better when speaking with others. Short-term Goals: • In 24 weeks, I want to utilize targeted functional communication phrases with familiar or unfamiliar communication partners with minimal cueing (I.e., question forms: "Can I use this?", social phrases, "slow down", "show me", "I don't understand", "say it again"). • In 24 weeks, I want to identify social communication targets and develop strategies to utilize them in the community setting with less than 2 visual prompts provided by the therapist. • In 16 weeks, I want to describe objects by providing information such as color, shape, size, function, etc. with 70% accuracy. • In 16 weeks, I want to repeat up to 4 words in functional phrases/sentences after a verbal model. FUNCTIONAL GOAL PLANNING • Related to function and impact on life • Person-centered=positive outcomes • Specific skill teaching to increase independence • Written for individual to understand • Measurable • Achievable • Time specific • Relevant=more motivation by person CASE STUDIES: FUNCTIONAL INTERVENTION AND GOAL PLANNING • Case studies with cognitive-communication barriers affecting real life situations • Create 2 long term functional goals and 2 short term goals for speech therapy • Identify 2 functional activities/tasks you’d incorporate in therapy that addresses these goals FUNCTIONAL GOALS LONG-TERM • In 24 weeks, I want to manage my own SHORT-TERM • In 8 weeks, I will be able to follow a visual support to recall medication management information (amt, times, pharmacy, etc.) with 80% accuracy. • In 8 weeks, I will be able to follow a written sequence to search for apartments online with minimal assistance provided. • In 8 weeks, I will be able to recall speech intelligibility strategies without reminders. • In 8 weeks, when given a short paragraph, I will answer comprehension questions given multiple choice options with 80% accuracy. medications. • In 24 weeks, I want to move to my own apartment. • In 16 weeks, I want to be understood by my friends, family and others. • In 16 weeks, I want to understand what I am reading in a book. CASE STUDY #1: 46 year old female Consumer has history of a brain tumor. Following surgery, consumer fell during a seizure and sustained a TBI. Additional falls and a car accident resulted in multiple concussions. – moderate TBI Actively searching for employment. Enjoys arts and craft activities, baking and spends a great deal of time with her friends and at her church. Not able to provide her own transportation and has very limited transportation options. Filling out paperwork is harder due to word recall and written abilities. Referred for speech therapy due to difficulty in the following areas: topic maintenance, decision making and emotional control. As well as verbal and written language and organizational skills. CASE STUDY #2 42 year old male Sustained his most recent brain injury in 2014 by falling while getting out of bed. – moderate TBI Medical History: Exhibits left side neglect, Spasticity in left arm and leg, causing pain and tightness, which can impact participation in various activities. Social: Has a close group of friends that he engages in activities with, such as visiting sporting events, museums and camping. Regularly goes to the gym two days a week for physical therapy activities. Currently unemployed and requires others to transport him into the community. Wants to live on his own in the near future. Referred to speech therapy due to concerns in the areas of memory, cognition, expressive and receptive language. CASE STUDY #3 43 year old female Involved in a car accident head on by a drunk driver – severe TBI Medical History: Cannot see out of her right eye. Diagnosed with severe sleep apnea and becomes tired quickly. Not currently working, Volunteers at an elementary school in a 2nd grade classroom. Social: Came home to live with parents and has two daughters who she speaks to frequently. Consumer uses her computer to communicate with family and friends through e-mail. Recently has started working on using her new iphone to increase contact with friends and family independently. Consumer likes to play games, read, talk with others, attend horseback riding lessons and attend her daughter’s sporting events. Requires assistance with transportation. Difficulty in the areas of: memory and cognition, attention, social pragmatics (repeating messages, body language), and visual neglect. CASE STUDY #4 24 year old female Fell from balcony at a party – severe TBI Medical History: Consumer just received communication device, depression and chronic pain, uses wheelchair Not currently working, would like to start volunteering at her community library. Social: Came home to live with parents and siblings. Consumer likes to play games, make jewelry, go shopping and watch movies. Requires assistance with transportation. Needs assistance with scheduling public transportation Difficulty in the areas of: memory and cognition, problem solving, attention, expressive aphasia, reading comprehension, medication management CASE STUDY #5 22 year old male Biking accident - mild TBI Medical history: fatigue, chronic pain in legs Social: wants to socialize more and begin dating, returned back to school taking one online course, wants to return to college full time, likes to go out to eat Relies on others to transport, would like to obtain driver’s license or ride his bike again Difficulty in areas of: processing language, attention, short-term memory, written language CASE STUDY #6 38 year old female History of abuse - mild TBI Working part time Single parent with two children in elementary school Social: involved in church and has two close friends, minimal family support Driving on own Difficulty in the areas of: managing schedules due to memory/organization, social pragmatics: low voice volume, expressive language, budgeting CASE STUDY #7 58 year old female Multiple car accidents - mild TBI Not currently employed, would like to begin volunteering Lives at home alone Social: involved in church, has grandkids she sees on a weekly basis, likes to cook Drives on own; however, car currently broke down Difficulty in the areas of: social communication (controlling volume level, interrupting), problem solving daily tasks, budgeting, executive functioning CASE STUDY #8 16 year old male Sports injury accident in 2017- mild TBI Attends high school and would like to go to community college Lives at home with parents and younger siblings Social: likes to hang out with friends, play video games, art Relies on parents and friends to transport; however, wants to drive on own someday Difficulty in the areas of: attention, short-term memory, social pragmatics: making inappropriate comments, following a schedule, organization CASE STUDY #9 25 year old male Gunshot wound – severe TBI Medical History: Uses a cane, history of seizures and migraines Not currently working, wants to pursue employment Social: Living in apartment, would like to start dating. Consumer likes to play games, listen to live music Requires assistance with transportation. Difficulty in the areas of: cognition (problem solving), short-term memory, expressive and receptive aphasia, pragmatics (interruptions, initiating, voice volume). CASE STUDY #10 60 year old male Fell from ladder working on his house - severe TBI Medical History: uses power wheelchair, severe depression, chronic pain Not currently working Social: Lives with wife at home. Likes to listen to audiobooks, watch/listen to the news, social isolation Requires wife and others to transport in the community, primarily to doctor’s appointments. Difficulty in the areas of: social pragmatics (maintaining conversations, low voice volume), expressive and receptive language, immediate memory, problem solving. SHARE CASE STUDIES/GOALS/ACTIVITIES CONCLUSION • Involve individual as much as possible in their therapy journey • Incorporate real life tasks in therapy goals related to functional daily living skills • Always be thinking of how to approach therapy goals to increase independence and/or independent living REFERENCES Brain Injury Association of America, 2009. The Essential Brain Injury Guide Edition 4.0. Rainbow Rehabilitation Centers, Inc., Livonia, MI. Burleigh, S.A., Farber, R. S., Gillard, M. Community Integration and Life Satisfaction After Traumatic Brain Injury: Long-Term Findings (1997). The American Journal of Occupational Therapy, 45-52. Coelho, C.A., DeRuyter, F., Stein, M. Treatment Efficacy: Cognitive-Communicative Disorders Resulting From Traumatic Brain Injury in Adults (1996). Journal of Speech and Hearing Research Vol 39, S5-S17. REFERENCES Irwin M. Altman, PhD, MBA, Shannon Swick, MA, Devan Parrot, BS, James F. Malec, PhD, ABPP-Cn, Rp. Effectiveness of Community-Based Rehabilitation After Traumatic Brain Injury for 489 Program Completers Compared With Those Precipitously Discharged (2010). Arch Phys Med Rehabil Vol 91, 1697-1704. Keith D. Cicerone, PhD, Tasha Mott, PhD, Joanne Azulay, PhD, John C. Friel, PsyD. Community Integration and Satisfaction With Functioning After Intensive Cognitive Rehabilitation for Traumatic Brain Injury (2004). Arch Phys Med Rehabil Vol 85, 943-950. REFERENCES Williams, J. Community Inclusion after Brain Injury: busting myths, revealing reality (2015). http://communityworksinc.com/janets-blog/ Williams, J., Bates, E., Boswell, L. (2018). TBI Case Study: Effectiveness of Home and Community-Based Rehabilitation Services Using Consumer-Driven Goal Planning. Poster presented at Brain Injury Across the Age Spectrum: Improving Outcomes for Children and Adults, NABIS, Houston, TX. THANK YOU FOR PARTICIPATING IN THIS SESSION TODAY! Lesley Tilley, MS, CCC-SLP lesleyt@mindsmatterllc.com