Cardiovascular Pathophysiology Assignment: Atherosclerosis & Hypertension
advertisement

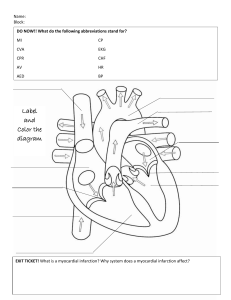
BMS310 Pathophysiology Module 6: Cardiovascular System Full credit is earned by providing as much detail to adequately address the objective. Write all responses using full-sentence structure format. Please write responses using your own words. Access all available resources to include as much information as possible for each item. Not mandatory, but be encouraged to insert images, diagrams, tables, and additional information from the textbook, video lectures, and supplementary medical literature into your document. Less than full credit for the assignment will be issued for work that is hand-written and, also, for work containing incomplete, abbreviated responses, one-word answers, fragmented phrases, bullet lists, and blank responses. Each blank response results in a point deduction. Video Lecture Unit 3 Cardiovascular 1 Atherosclerosis and Hypertension Write all responses using full-sentence structure format. 6.1 Describe the normal forward flow of blood through the heart beginning from where blood enters through the superior vena cava and inferior vena cava. In your discussion, identify all valves and all chambers until blood leaves the heart through the aorta. (refer to information in recorded lecture, fig. 32.3, and pp. 1019-1021 in McCance, 8th ed) 6.1 answer: When blood enters the superior and inferior vena cava from the body, it starts in the right atrium and enters the right ventricle through the right atrioventricular valve (tricuspid). Blood then enters the pulmonary trunk through the pulmonary semi-lunar valve and exits into the lungs. From the lungs, blood enters through the pulmonary arteries into the left atrium. It flows down to the left ventricle through the left atrioventricular valve (bicuspid) and then through the aortic valve to the aortic body and to the rest of the body. 6.2 Describe what the term “tissue perfusion” specifically refers to. (refer to information in recorded lecture and p. 1044 in McCance, 8th ed) 6.2 answer: Tissue perfusion refers to amount of blood that reaches the organs from the heart. For questions 6.3a – 6.3e, refer to the Scientific American article, “Atherosclerosis: The New View”, to describe the five various stages that link that evolution of an atherosclerotic plaque to myocardial infarction (a heart attack): 6.3a step 1- The first stage of the evolution of an atherosclerotic plaque to myocardial infarction is a damaged endothelium. Excess LDL accumulates in the arteries and undergoes chemical alterations. The LDLs stimulate endothelial cells to display adhesion molecules that latch to monocytes and T-cells. The endothelial cells secrete Chemokines that lure shared cells into the intima. 6.3b step 2- The second stage the formation of a yellow, fatty streak. In the intima, the monocytes mature into active macrophages. The macrophages and T cells produce many inflammatory 1 mediators, including cytokines and factors that promote cell division. The macrophages also display so-called scavenger receptors, which help them ingest modified LDLs. There are growth factors produced stimulating smooth muscle growth, lipid laden macrophages bind to endothelium, LDLs become oxidized, and vascular lesions may be reversible with diet modification. 6.3c step 3- Step three includes fibrous plaques where smooth muscle cells proliferate in lesions and deposit collagen in creating a more firm, rigid mass. The macrophages feast on the LDLs, which becomes filled with fatty droplets. These macrophages and T- cells constitute the fatty streaks, the earliest form of the plaques. 6.3d step 4- Step four includes complicated lesions and the progression of lesions. Inflammatory molecules can promote further growth of the plaque and formation of a fibrous cap over the lipid core. The cap develops when the molecules induce smooth muscle cells of the media to migrate to the top of the intima, multiply and produce a tough, fibrous matrix that glues the cells together. The cap adds to the size of the plaque but also walls it off safely from the blood. 6.3e step 5- Step five includes the rupture of plaques. Later, inflammatory substances secreted by foam cells can dangerously weaken the cap by digesting matrix molecules and damaging smooth muscle cells, which then fail to repair the cap. If the weakened plaque ruptures, tissue factor will interact with clot-promoting elements in the blood, causing a thrombus, or clot, to form. If the clot is big enough, it will halt the flow of blood to the heart, producing a heart attack—the death of cardiac tissue. 6.4 Describe how atherosclerosis affects the normal anatomy and physiology of a coronary artery to eventually cause an increased workload on the heart. (refer to information in recorded lecture, p. 1035, and pp. 1072-1074 in McCance, 8th ed) 6.4 answer: In atherosclerosis, there is deposition of fat and fibrin in the wall of the arteries which tend to harden over time. There is occlusion of the arterial lumens and there is a decrease in compliance (stretchability). The reduction of blood flow to tissue causing ischemia where there is cerebral ischemia in the brain, myocardial ischemia in the heart, and peripheral artery disease in the legs. Because of the increase in peripheral resistance to the blood flow, there is, in turn, in increase of workload on the heart. 6.5 Differentiate between (a) non-modifiable risk factors and (b) modifiable risk factors for the development of atherosclerosis. (refer to information in recorded lecture and pp. 1072-1074 in McCance, 8th ed) 6.5a answer: Non-modifiable risk factors are age, sex, family history, and race. 6.5b answer: Modifiable risk factors include low density lipoproteins (bad cholesterol), high density lipoproteins (good cholesterol), hypertension, cigarette spoken, and C reactive protein (CRP) 2 6.6 Describe how the levels of the biomarkers C-reactive protein and cholesterol serve as serve as an index for the relative risk of a future heart attack. In your discussion, clearly indicate the significance of low levels and high levels of both biomarkers. (refer to information in recorded lecture, p. 98 in lecture note-pack, and pp. 1072-1078 in McCance, 8th ed) 6.6 answer: Studies showed that people who had low levels of Cholesterol are at lower risk of having a heart attack that high levels of cholesterol. Low levels of CRP also had low risk of having a heart attack which high levels of CRP had a high chance of having a heart attack. Having high levels of cholesterol and CRP had the highest chance of having a heart attack. In atherosclerosis, there are constant high levels of CRP. 6.7 Describe four endocrine disorders that could be the causative factor of a diagnosis of secondary hypertension. (refer to information in recorded lecture and p 1061-1065 in McCance, 8th ed) 6.7a answer: The first endocrine disorder is hyperthyroidism. 6.7b answer: The second endocrine disorder is hypercortisolism. 6.7c answer: The third endocrine disorder is hyperaldosteronism. 6.7d answer: The fourth endocrine disorder is pheochromocytoma. 6.8 According to the latest JNC report, describe blood pressure values to qualify for (a) normal blood pressure, (b) elevated blood pressure, (c) stage 1 hypertension, and (d) stage 2 hypertension. (refer to information in recorded lecture, p. 99 in lecture note-pack, and table 33.1 on p. 1061 in McCance, 8th ed) 6.8a answer: The normal blood pressure value is 120/80. 6.8b answer: The elevated blood pressure value is 120-129/80 6.8c answer: The stage one hypertension is 130-139/ 80-89. 6.8d answer: The stage two hypertension is above 140/ above 90. For questions 6.9a-6.9b, describe the general physiological mechanisms by which diuretics, beta blockers, vasodilators (including calcium channel blockers and ACE inhibitors) act to decrease the workload of the heart. (refer to information in recorded lecture, p. 99 in lecture note-pack, and pp. 1067-1068 in McCance, 8th ed) 6.9a diuretics- Reduce blood volume which in turns, causes water loss (increase in urine output), and a decrease in blood pressure. 6.9b beta-blockers- Decreases heart rate and myocardial contractility. 6.9c calcium channel blockers- Decrease tension in arterial smooth muscle cells. Because it decreases the amount of calcium in the blood, vasodilation occurs. 3 6.9d angiotensin converting enzyme (A.C.E.) inhibitors- ACE inhibitors stop the conversion of angiotensin I to angiotensin II. Angiotensin II causes vasoconstriction, so when ACE is inhibited, vasodilation occurs. 6.10 Near the beginning of the video showing the Rheos Implantable Pulse Generator, describe the three consequences of chronic, unmanaged high blood pressure on the human body. 6.10a answer: Consequences of the chronic, unmanaged high blood pressure of the human body includes a higher risk of heart failure. 6.10b answer: It reduces the quality of life. 6.10c answer: It shortens life expectancy. 6.11 At the end of the video showing the Rheos Implantable Pulse Generator, describe the four health benefits of reducing high blood pressure. 6.11a answer: There is a reduction in heart disease. 6.11b answer: There is a reduction in kidney failure 6.11c answer: There is a reduction in stroke. 6.11d answer: There is a reduction in heart disease and death in general. Video Lecture Unit 3 Cardiovascular 2 Myocardial Ischemia Write all responses using full-sentence structure format. 6.12 Discuss the pathophysiological consequences the myocardium may suffer with chronic, untreated hypertension. (Refer to lecture and table 33.2, and pages 1061-1068 in McCance 8th ed.) 6.12 answer: There is a decreased contractibility of myocardium which can produce an abnormal wall motion over ischemic area with each contraction. 6.13 List several risk factors associated with the development of coronary artery disease. (refer to information in recorded lecture and pp. 1072-1074 in McCance, 8th ed) 6.13 answer: The several risk factors associated with the development of coronary artery disease includes hyperlipidemia, hypertension, cigarette smoking, diabetes mellitus, genetic predisposition, obesity, sedentary life style, loss of estrogen, alcohol, gender, and personality. 4 6.14 Describe the major difference between myocardial ischemia and myocardial infarction by indicating (a) which condition creates transient/reversible myocardial tissue damage and (b) which condition creates permanent tissue damage. (refer to information in recorded lecture, p. 100 and p. 102 in lecture note-pack, and pp. 1074-1087 in McCance, 8th ed) 6.14a answer: Myocardial infarction creates reversible myocardial tissue damage. 6.14b answer: Myocardial infarction causes permanent damage to the tissue. 6.15 Describe the pathophysiology associated with myocardial ischemia focusing on changes in (a) myocardial cellular function, (b) changes in ventricular function, (c) changes in stroke volume, and (d) changes in end diastolic volume. (refer to information in recorded lecture, fig. 33.15, and pp. 1079-1081 in McCance, 8th ed) 6.15a answer: Myocardial cellular function is transient reversible lack of oxygen to the myocardium. There is an increase anaerobic metabolism and increased production of lactic acid. 6.15b answer: There is impaired left ventricular function due to hypoxia and lactic acid accumulation. 6.15c answer: There is a decrease in stroke volume. 6.15d answer: There is an increase end diastolic volume and pressure 6.16 (a) Describe the average normal values of stroke volume, (b) end diastolic volume, and (c) describe how to calculate ejection fraction. (d) Describe if ejection fraction increases or decreases during myocardial ischemia. Justify your answer to (d) based on changes in stroke volume and end diastolic volume. (refer to information in recorded lecture, p. 1032, table 32.3 on p. 1034, and pp. 1079-1083 in McCance, 8th ed) 6.16a answer: Normal values of stroke volume is 70mL. SV is the volume of blood ejected out of a ventricle with each cardiac cycle. 6.16b answer: End diastolic volume is the volume of blood in each ventricle at the end of diastole. The average is 120mL. 6.16c answer: Ejection infarction is calculated by the stroke volume divided by the end diastolic. 6.16d answer: If ejection fraction increases, so does stroke volume. However, end diastolic volume decreases when ejection fraction increases. If ejection fraction decreases, stroke volume decreases and the end diastolic volume increases. 6.17 (a) Provide a definition of the term angina pectoris and (b) describe several symptoms of angina pectoris. (refer to information in recorded lecture and pp. 1079-1080 in McCance, 8th ed) 6.17a answer: Angina pectoris is sudden onset chest pain caused by myocardial ischemia. 5 6.17b answer: Symptoms of angina pectoris are a pressing, squeezing, or crushing pain in the chest, left arm pain, pain in shoulders, jaw, neck, or back, shortness of breath, weakness, and fatigue. 6.18 Provide a definition of the terms (a) “pre-load” and (b) “after-load”. (c) Provide a detailed description explaining how nitroglycerine relieves pain associated with angina pectoris. (*The terms “pre-load” and “after-load” are described in more detail in McCance and Huether’s textbook 8th edition on pages 1032-1035 in chapter 32.) 6.18a answer: The pre-load refers to the amount of tension the muscle has to generate during the resting phase. 6.18b answer: The afterload refers to the amount of tension of the muscle has to generate during the contraction phase. 6.18c answer: Nitroglycerin affectively reduces pre-load and after-load very quickly. Pain can be relieved by nitroglycerin which will decrease the workload on the heart. It gets introduced into the circulatory system and converted into nyclooxide causing smooth muscle cells in the arteriole and veins to relax which promotes vasodilation. This decreases the amount of blood for venous return which equals less cardiac input which means less blood going into the heart which means less pressure. 6.19 Provide a description of (a) subendocardial ischemia and (b) transmural ischemia. Include characteristic EKG changes associated with each type of ischemia. (refer to information in recorded lecture, fig. 33.17, and text on p. 1081 in McCance, 8th ed) 6.19a answer: Subendocardial ischemia has a ST segment depression and T wave inversion. It occurs in the deep layer of the left ventricular muscle. 6.19b answer: Transmural ischemia has elevation of the ST segment. It happens when the entire wall thickness from endocardium to epicardium is affected in the area supplied by an occluded artery. 6.20 Discuss the theory of coronary artery bypass graft surgery for treatment of coronary artery disease and myocardial ischemia. (refer to information in recorded lecture and pp. 1081-1082 in McCance, 8th ed) 6.20 answer: Coronary artery bypass graft surgery occurs on the saphenous vein, left internal thoracic artery, and the radial artery. 6.21 Discuss the theory for using balloon angioplasty in the treatment of coronary artery disease and myocardial ischemia. (refer to information in recorded lecture and pp. 1081-1082 in McCance, 8th ed) 6.21 answer: Balloon angioplasty is when a small balloon is inserted into the lumen of the vessel and is then inflated to Unblock the artery. 6 6.22 Discuss the theory using stents for treatment of coronary artery disease and myocardial ischemia. (refer to information in recorded lecture and pp. 1081-1082 in McCance, 8th ed) 6.22 answer: Stents are inserted into the lumen of the vessel with the balloon to stabilize the open lumen that the balloon just unblocked. Video Lecture Unit 3 Cardiovascular 3 Myocardial Infarction Write all responses using full-sentence structure format. 6.23 Describe defining characteristics of a myocardial infarction including changes in cardiac function. (refer to information in recorded lecture and pp. 1083-1087 in McCance, 8th ed) 6.23 answer: Myocardial infarction is commonly known as a heart attack. It is the end point of coronary artery disease and prolonged ischemia and causes irreversible hypoxic injury to cells and, inevitably cell death and tissue necrosis. It can lead to decreased cardiac contractability, altered left ventricular compliance, decreased stroke volume, decreased ejection infarction, increased left ventricular end diastolic pressure, and sino-arterial node malfunction. 6.24 Describe the pathophysiology and characteristic ECG changes associated with (a) transmural myocardial infarction and (b) subendocardial myocardial infarction. (refer to information in recorded lecture, fig. 32.23, and pp. 1083-1087 in McCance, 8th ed) 6.24a answer: Transmural myocardial infarction is when the discolored dead tissue extends to the entire width of the wall of the myocardium. 6.24b answer: The subendocardial myocardial infarction is when the discolored dead tissue does not extend to the entire width and there is still live tissue on the width of the myocardium. 6.25 Discuss responses in the myocardium following a myocardial infarction after (a) 24 hours, (b) 2 weeks, and (c) 6 weeks. (refer to information in recorded lecture and p. 1085 in McCance, 8th ed) 6.25a answer: In the myocardium after 24 hours, leukocyte infiltration into inflamed and necrotic area. Proteolytic enzymes degrade necrotic tissue, and catecholamines are released from damaged cells which increases blood sugar. 6.25b answer: After 2 weeks, there is an increase in insulin release and a weak collagen matrix is formed which is mushy and vulnerable. 6.25c answer: After 6 weeks, strong scar tissue develops, and this tissue does not contract/relax or conduct (non-functional). 7 6.26 Describe symptoms associated with a myocardial infarction and explain the physiology producing these effects. (refer to information in recorded lecture and pp. 1085-1087 in McCance, 8th ed) 6.26 answer: Signs and symptoms associated with myocardial infarction include sudden/severe chest pain, pain not relieved by nitrated, initial drop in blood pressure caused by sympathetic activation causing profuse sweating, cool and clammy skin from peripheral vasoconstriction, reflexive increase in heart rate and blood pressure, and detection of cardiac proteins called Isoenzyme that are contractile proteins, abnormal heart sounds, and act as biomarkers of myocardial infarction. 6.27 Describe the theory why cardiac iso-enzymes (and other myocardial-specific proteins) present in plasma serve as biomarkers of myocardial infarction. In your discussion, identify specific proteins that serve as biomarkers for a myocardial infarction including relative timing of their appearance in blood. (refer to information in recorded lecture, box 33. 2, and pp. 1086-1087 in McCance, 8th ed) 6.27 answer: Cardiac iso-enzymes and myocardial-specific proteins serve as biomarkers because they aid in diagnosing myocardial infarction. Specific proteins include creatine kinase, lactate dehydrogenase, myoglobin, troponin T, and myeloperoxidase. 6.28 In reference to a myocardial perfusion scan using thallium-201 (or other compounds), describe the significance of the presence of a “cold spot”. (refer to information in recorded lecture and pp. 1051-1052 in McCance, 8th ed) 6.28 answer: The presence of a cold spot tells where the actual location of the myocardial infarction is and the extent of the injury. 6.29 Referring to a person that has (or is having) severe chest pain along with elevated cardiac proteins in their blood, describe the significance of an elevated ST segment and/or a very large Q wave appearing on their electrocardiogram. (refer to information in recorded lecture, fig. 32.23, and pp. 1083-1087 in McCance, 8th ed) 6.29 answer: The significance of an elevated ST segment refers to dead tissues correlated with a rise of cardiac protein in the bloodstream. This injury occurs under the endocardium. The very large Q wave refers to a transmural infarction that shows permanent injury. This extends through the entire width of the myocardium from the endocardium to the pericardium. 6.30 Describe the purpose and rationale for administering “blood thinners” such as aspirin or heparin to a person following a myocardial infarction. (refer to information in recorded lecture and pp. 10861087 in McCance, 8th ed) 6.30 answer: Blood thinners helps the blood from clotting. 8 6.31 Describe the purpose and rationale for administering a “clot-busting drug” such as tissue plasminogen activator (tPA) to a person following a myocardial infarction. (refer to information in recorded lecture and pp. 1086-1087 in McCance, 8th ed) 6.31 answer: tPA circulates in the persons vasculature and works quickly to dissolve proteiins that are active in a blood clot. 6.32 Describe several physiological complications associated with myocardial infarctions. (refer to information in recorded lecture and p. 1087 in McCance, 8th ed) 6.32 answer: Complications include dysrhythmias, left ventricular failure, rupture of heart structures, rupture of the wall of infarcted ventricle, systemic thromboembolism, and sudden death. Video Lecture Unit 3 Cardiovascular 4 Disorders of the Heart Wall Write all responses using full-sentence structure format. 6.33 Define cardiac tamponade and describe differences between gradual and rapid accumulation of fluid in the pericardial sac. (refer to information in recorded lecture and pp. 1088-1089 in McCance, 8th ed) 6.33 answer: Cardiac tamponade is rapid accumulation of about 50-100 cc of blood where there is a lot of cardiac compression, leading to mechanical impedance of the heart with a normal electrical current still conducting as normal. Gradual accumulation can accommodate up to 1000 cc of fluid in the pericardial space. 6.34 Describe two procedures that can rapidly eliminate accumulated fluid in the pericardial space. In your discussion, identify the goal of these treatments. (refer to information in recorded lecture and pp. 1088-1089 in McCance, 8th ed) 6.34a answer: One procedure is a thoracotomy where these is a cutting of the myocadiac sac to release the pressure of fluid. 6.34b answer: Another procedure is called a pericardial cyntethis where a needle is inserted to withdraw the fluid. 6.35 (a) Describe the pathophysiology associated with dilated cardiomyopathy. (b) Describe potential treatment options available to a person suffering from symptoms associated with dilated cardiomyopathy. (refer to information in recorded lecture and pp. 1089-1090 in McCance, 8th ed) 9 6.35a answer: Dilated cardiomyopathy is when the heart is enlarged causing it to dilate which creates a weaker heart that results from degeneration from myocardial muscle fibers. The ventricular myocardium becomes weaker and it ultimately leads to heart failure. There is a decrease in cardiac contractability, decreased systolic performance, increased EDV, and a decrease in stroke volume. 6.35b answer: Potential treatment options are ACE inhibitors where it widens the blood vessels to lower the blood pressure, improve blood flow, and decrease the heart’s workload. 6.36 (a) Describe the pathophysiology associated with hypertrophic cardiomyopathy. (b) Describe potential treatment options available to a person suffering from symptoms associated with hypertrophic cardiomyopathy. (refer to information in recorded lecture and pp. 10890-1091 in McCance, 8th ed) 6.36a answer: Hypertrophic cardiomyopathy is hypertrophy (cells get larger) of the interventricular septum and the myocardium becomes non-compliant. There is a decrease in volume of the chambers which leads to a decrease in stroke volume and cardiac output. 6.36b answer: Beta-blockers and calcium channel blockers increase the performance of the cardiac tissue and there is a surgical reception like open-heart surgery. 6.37 (a) Identify at least three diseases associated with causing restrictive cardiomyopathy and describe the pathophysiology associated with restrictive cardiomyopathy. (b) Describe at least one potential treatment option available to a person suffering from symptoms associated with restrictive cardiomyopathy. (refer to information in recorded lecture and p. 1091 in McCance, 8th ed) 6.37a answer: Three diseases associated with causing restrictive cardiomyopathy are amyloid, hemochromatosis, and glycogen storage disease. It is when excess material gets deposited into the tissue which can lead to inflammation. The outcome is a deposition of collagen fibers which has no compliance and causes the heart to be stiff and rigid. 6.37b answer: One treatment is getting a heart transplant. Video Lecture Unit 3 Cardiovascular 5 Valve Disorders Write all responses using full-sentence structure format. 6.38 Describe the general differences between (a) valvular stenosis and (b) valvular insufficiency. (refer to information in recorded lecture, fig. 33.29, and p. 1091 in McCance, 8th ed) 6.38a answer: Valvular stenosis is when the valves of the heart ate stiff and rigid and cannot open. Valve orifice is constricted and narrowed, chambers behind the valves have increased workload, 10 myocardial wall becomes larger, aortic semilunar valves and bicuspid valve are most affected. Causes include rheumatic heart disease, congenital malformations, and calcification. 6.38b answer: Vascular insufficiency is when the valve is flimsy and does not open properly. 6.39 Describe all the pathophysiology associated with aortic valvular stenosis as presented in the recorded lectures. Be sure to include an explanation of how fluid accumulates in alveoli causing difficult breathing. (refer to information in recorded lecture, lecture note-pack, table 33.6, and pp. 10911092 in McCance, 8th ed) 6.39 answer: Aortic semilunar valve stenosis is hypertrophy of the left ventricle. There is a decrease in stroke volume and cardiac output which results in a decrease in tissue perfusion. Fluid accumulates in the alveoli because there is an increase workload on the ventricles which causes the cell dies sooner, leading to heart failure. When the blood does not continue to go through the heart, it accumulates and enlarges the ventricle and pulmonary veins and capillaries. This leads to an increase in pulmonary hydrostatic pressure and water enters the alveoli leading to breathing problems. 6.40 (a) Provide a mathematical definition of “pulse-pressure”. In aortic valvular stenosis, describe (b) why systolic pressure decreases and, (c) why diastolic pressure increases accounting for a “narrowing” of the pulse pressure. (refer to information in recorded lecture, lecture note-pack, and p. 1092 in McCance, 8th ed) 6.40a answer: Pulse pressure is systolic minus diastolic. 6.40b answer: Systolic pressure decreases because there is less blood being ejected. 6.40c answer: When there is a decrease in volume and pressure, baroreceptors tell the brain that it needs to increase sympathetic stimulation causing the arterioles constrict. This leads to increased diastolic pressure. 6.41 Describe the pathophysiology associated with mitral valve (left AV valve) stenosis as presented in the recorded lectures. (refer to information in recorded lecture, lecture note-pack, table 33.6, and pp. 1092-1093 in McCance, 8th ed) 6.41 answer: Mitral valve stenosis is left atrial hypertrophy that causes a decrease in cardiac output and an increased blood volume and pressure backs up into pulmonary circulation. 6.42 Referring to mitral valve stenosis, (a) define the clinical concept of pulmonary “wedge pressure” and (b) include an explanation of how fluid accumulates in alveoli causing and increased wedgepressure and difficult breathing. (refer to information in recorded lecture, lecture note-pack, table 33.6, and p. 1092-1093 in McCance, 8th ed) 11 6.42a answer: Pulmonary wedge pressure measures pulmonary capillary pressure by putting a catheter in the heart until it hits the end of the capillary. 6.42b answer: Fluid accumulates in alveoli due to an increase in pulmonary capillary hydrostatic pressure. 6.43 Describe the pathophysiology associated with aortic valvular insufficiency (regurgitation) as presented in the recorded lectures. Be sure to include an explanation of how fluid accumulates in alveoli causing difficult breathing. (refer to information in recorded lecture, lecture note-pack, table 33.6, and p. 1093 in McCance, 8th ed) 6.43 answer: Aortic valvular insufficiency involves a retrograde flow into the left ventricle. It causes an increase in end diastolic volume, increased stroke volume, and a widened pulse pressure. The results are left sided heart failure. 6.44 In aortic valvular insufficiency, (a) describe why systolic pressure increases and, (b) why diastolic pressure decreases accounting for a “widening” of the pulse pressure. (refer to information in recorded lecture, lecture note-pack, table 33.6, and p. 1093 in McCance, 8th ed) 6.44a answer: Systolic pressure increases because the blood abnormally comes back from the aorta. 6.44b answer: Diastolic pressure decreases because of the stretched myocardial cells. This effect causes an increase in the force of contraction to help push the blood out. 6.45 Describe the pathophysiology associated with mitral valvular insufficiency (regurgitation) as presented in the recorded lectures. Be sure to include an explanation of how fluid accumulates in alveoli causing difficult breathing. (refer to information in recorded lecture, lecture note-pack, table 33.6, and pp. 1093 in McCance, 8th ed) 6.45 answer: Mitral valvular regurgitation is when there is retrograde flow of blood into the left ventricle. EDV increases and so does stroke volume because there is an increase in the force of contraction (this widens the pulse pressure). 6.46 Describe the connection between rheumatic fever and rheumatic heart disease. (refer to information in recorded lecture, lecture note-pack, fig. 33.33, and pp. 1094-1095 in McCance, 8th ed) 6.46 answer: Rheumatic fever happens from a pharyngeal infection which happens to be about three percent of the population. The delayed reactions cause a fever. About 10 percent of the population develop rheumatic heart disease resulting from the untreated condition and will affect the people for the rest of their lives. 12 6.47 (a) Describe the pathophysiology associated with rheumatic heart disease. (b) Also, refer to text on page 1094 in McCance (8th ed) to explain why there has been a decline in the incidence of rheumatic heart disease since the 1950’s. (refer to information in recorded lecture, lecture note-pack, fig. 33.33, and pp. 1094-1095 in McCance, 8th ed) 6.47a answer: Rheumatic heart disease is associated with heart disease stemming from a group A betahemolytic streptococcus infection. Bacterial antigens bind to receptors on the heart, brain, and synovial joints. Autoimmune response and inflammatory response producing arthritis and inflammation of endocardium and myocardium. All three layers of the heart become inflamed. 6.47b answer: There has been a decline because of the medical socioeconomic improvements as well as changes in the virulence of group A streptococci. Video Lecture Unit 3 Cardiovascular 6 Heart Failure Write all responses using full-sentence structure format. 6.48 Define the terms (a) bradycardia and (b) tachycardia. Provide an example of a heart rate exemplifying each condition. (refer to information in recorded lecture, lecture note-pack, *table 33.9, and pp. 1098-1108 in McCance, 8th ed) 6.48a answer: Bradycardia is low heart rate that is less than 60bpm and maintains normal rhythm. 6.48b answer: Tachycardia is high heart rate that is greater than 100bpm and maintains a normal rhythm. 6.49 (a) Explain why ventricular fibrillation can be rapidly fatal and (b) describe a treatment discussed during lecture to rapidly correct ventricular fibrillation. (refer to information discussed in class, in the recorded lecture, lecture note-pack, *table 33.9, and pp. 1098-1108 in McCance, 8th ed) 6.49a answer: ventricular fibrillation can be rapidly fatal because the heart rate can become greater than 300bpm which is not compatible with life. 6.49b answer: A treatment may be a defibrillator to shock the cells to stop depolarization and allow AS node to reset the pace. 6.50 (a) Describe diagnostic criteria and (b) pathophysiology (if any) associated with a first-degree heart block. (refer to information in recorded lecture, lecture note-pack, *table 33.10, and pp. 1098-1108 in McCance, 8th ed) 6.50a answer: ECG changes that include a PR interval of greater than 0.20 without disruption of atrial to ventricular conduction 13 6.50b answer: First degree heart block is benign partial blockage where the EKG looks normal the P-R intervals are prolonged longer than 200ms. 6.51 (a) Describe diagnostic criteria and (b) pathophysiology associated with a second-degree heart block (Mobitz II). (refer to information in recorded lecture, lecture note-pack, *table 33.10, and pp. 10981108 in McCance, 8th ed) 6.51a answer: ECG changes include an increase of P waves than R waves. 6.51b answer: Second degree block is a disturbance, delay, or interruption of atrial impulse conduction to the ventricles through the AV nodes and bundles. It is a partial block. 6.52 (a) Describe the pathophysiology and (b) treatment associated with a third-degree heart block. (refer to information in recorded lecture, lecture note-pack, *table 33.10, and pp. 1098-1108 in McCance, 8th ed) 6.52a answer: Pathophysiology of their- degree heart block is when the AV node does not conduct action potentials into ventricles. The impulse never travels to the fibers, causing a decrease in heart rate. The atria and ventricles beat independently. 6.52b answer: Treatments include an artificial pacemaker to remedy situation. 6.53 How does the McCance textbook define the term “heart failure”. (refer to text on page 1098 in McCance 8th ed) 6.53 answer: Heart failure is defined as the pathophysiologic condition in which the heart is unable to generate an adequate cardiac output such as inadequate perfusion of tissues or increased diastolic filling pressure of the left ventricle, or both, occurs. Consequently, pulmonary capillary pressure are increased. 6.54 Provide an explanation for all the symptoms associated with right-sided heart failure as presented in the recorded lecture. (refer to information in recorded lecture, lecture note-pack, and p. 1102 in McCance, 8th ed) 6.54 answer: Right sides heart failure shows a descendant of a person’s neck due to jugular veins. There is accumulation of blood leading to leakage of block showing swelling and enlarged organs. An increase pulmonary vascular resistance causes an increase central venous pressure (jugular veins) which causes an increased systemic capillary hydrostatic pressure, leading to edema. 6.55 Provide an explanation for all the symptoms associated with left-sided heart failure (congestive heart failure) as presented in the recorded lecture. (refer to information in recorded lecture, lecture note-pack, and p. 1098 in McCance, 8th ed) 14 6.55 answer: Left side symptoms are trouble breathing due to dyspnea because they are suffocating. 6.56 Describe several diseases/disorders that may lead to heart failure. (refer to information in recorded lecture, lecture note-pack, and p. 1098 in McCance, 8th ed) 6.56 answer: Diseases include aortic vascular regurgitation, damage to the heart, heart attacks, myocardial ischemia, aortic valvular stenosis, and systemic hypertension. 6.57 (a) Describe normal source and function of the hormone, b-type natriuretic peptide (BNP). (b) Describe the clinical utility of measuring BNP levels in a person with congestive heart failure. (refer to information in recorded lecture, lecture note-pack, and p. 1046, 1063, and 1099, in McCance, 8th ed) 6.57a answer: The normal source is myocardial cells and serves as a biomarker to distinguish between cardiac and respiratory problems. When BNP is made, the kidneys do not retain sodium. Instead, they get rid of it and water follows. This allows fluid to clear out of the lungs. 6.57b answer: Measuring BNP levels in a person with congestive heart failure will be important because if the BNP levels drop, that means that treatment is working. 6.58 (a) Define the term “circulatory shock” and (b) describe several causes of shock. (refer to information in recorded lecture, lecture note-pack, and p. 1543 in McCance, 8th ed) 6.58a answer: Circulatory shock is a condition in which the cardiovascular system fails to perfuse tissues adequately, resulting in a widespread impairment of cellular metabolism. 6.58b answer: It can be caused by a decrease in cardiac output. 6.59 Describe molecular mechanisms of adrenergic receptor activation with norepinephrine promoting arterial vasoconstriction and increasing blood pressure in a person in circulatory shock. (hint – Does adrenergic receptor activation promote calcium channels on vascular smooth muscle cells to open or close and what effect does this promote on tension in the muscle cell?) (refer to information in recorded lecture and the figure on p. 40 in the article in Scientific American, “Insights into Shock”) 6.59 answer: Adrenergic receptors promotes arterial vasoconstriction and increased blood pressure because someone might not be able to respond to adrenalin. 6.60 Describe molecular mechanisms of vasopressin receptor activation promoting arterial vasoconstriction and increasing blood pressure in a person in circulatory shock. (hint – Does vasopressin receptor activation promote potassium channels to open or close? Does vasopressin receptor activation promote calcium channels on vascular smooth muscle cells to open or close and what 15 effect does this promote on tension in the muscle cell?) (refer to information in recorded lecture and the figure on p. 40 in the article in Scientific American, “Insights into Shock”) 6.60 answer: Vasopressin receptor activation opens calcium channels and calcium influxes inward which increases tension in the cell. Questions 6.61-6.67 are derived from the medical journal article published in JAMA-Cardiology, “Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19)”. Please read this article which can be accessed for free at: https://jamanetwork.com/journals/jamacardiology/fullarticle/2763845 (PDF and link also located on Blackboard in “Coronavirus 2020 Related Links” folder found in “web-links”) Write all responses using full-sentence structure format. 6.61 What is the stated objective of this investigation? (page E1) 6.61 answer: The objective is to evaluate the association of underlying cardiovascular disease and myocardial injury with fatal outcomes in patients with Covid-19. 6.62 Describe the design, setting, and participants in this study. (page E1) 6.62 answer: It is a single center case series analyzed patients with Covid-19 at the Seventh Hospital of Wuhan City, China, from Jan. 23, 2020, to Feb. 23, 2020. Analysis began Feb. 25, 2020. 6.63 Describe the main outcomes and measures in this study. (page E1) 6.63 answer: Main outcomes and measures are demographic data, laboratory findings, comorbidities, and treatments were collected and analyzed in patients with and without elevation of troponin T levels. 6.64 Referring to Table 2 “Laboratory Results Among Different Groups”, identify “inflammatory biomarkers” used in this study. For any biomarker commonly referred to using an abbreviation, include both the abbreviation and full name of the molecule. (page E4) 6.64 answer: Inflammatory biomarkers are hsCRP (high sensitivity C reactive protein), procalcitonin, and globulins. 16 6.65 Referring to Table 2 “Laboratory Results Among Different Groups”, identify “other cardiac biomarkers” used in this study. For any biomarker commonly referred to using an abbreviation, include both the abbreviation and full name of the molecule. (page E4) 6.65 answer: Other cardiac biomarkers include creatine kinase MB fraction, myoglobin, and natriuretic peptide tests (NT-proBNP) 6.66 On page E6 in Figure 2, “Mortality of Patients With Coronavirus Disease 2019 (COVID-19) With/Without Cardiovascular Disease (CVD) and With/Without Elevated Troponin T (TnT) Levels”, what is the mortality (percentage) for the following groups: 6.66 answer: patients with CVD+elevated TnT = 69.44% patients without CVD+elevated TnT = 37.50% patients with CVD+normal TnT = 13.33% patients without CVD+normal TnT = 7.62% 6.67 What are the conclusions of this study? (p. E7) 6.67 answer: Conclusions made were that myocardial injury is significantly associated with the fata outcome of covid-19, while the prognosis of patients with underlying CVD but without myocardial injury is relatively favorable. Myocardial injury is associated with cardiac dysfunction and arrhythmias. Inflammation may be a potential mechanism for myocardial injury. Aggressive treatment may be considered for patients at high risk of myocardial injury. *Before submitting your assignment, please double-check to make sure all questions have been addressed and, also, responses are written using full-sentence structure. 17