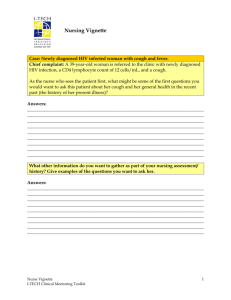
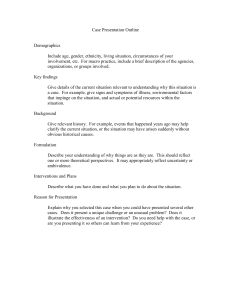
Subjective Chief Complaint: Patient reports new onset of a cough History of Present Illness: Ms. A is a 40-year-old female who presents with a cough. Ms. A stated she has a new onset of a cough that started at least 7 to 10 days ago. She also noted that along with her cough she had a fever up to 100ºF. She states the cough is intermittent, worse with exertion and occasionally becomes short of breath. Her cough is wet and reports having green sputum, except over the last 2 days it has become blood tinged. Ms. A reports her cough is worse at night and admits to smoking. Ms. A admits that she has not been sleeping well due to her cough and has become increasingly tired over the last week. Ms. A is a high school English teacher and states she has been around sick colleagues and children. She stated “it’s that time of the year again when everyone gets sick” making her believe she picked her cough up from work. Ms. A states her cough is relieved by resting and drinking water. Ms. A admits to trying over the counter Mucinex every 12 hours, however, does not have any relief. Ms. A states she has a headache that started 5 days ago. States the headache is dull and throbbing, located in the occipital region. Denies current headache. Denies pain that radiates to her neck and arms. Denies neck pain and stiffness. Admits to taking over the counter Extra Strength Tylenol, 650 mg every 6 hours as needed for headaches. States the Tylenol “seems to be helping”. She states that her headache is from coughing. She denies a runny nose, sinus congestion, nasal discharge, postnasal drip and sneezing. Ms. A states she also has left ear pain. Stated the ear pain started around the same time as the cough. She states the ear pain is associated with cough. Denies ear discharge and pain currently. Denies sore throat and difficulty swallowing. Denies recent fever (only had a slight fever in the beginning) and chills. Denies dizziness or lightheadedness. Denies night sweats, epistaxis, weight or appetite loss. Denies vision or hearing changes. Denies chest pain or tightness. Denies watery, dry, red, or painful eyes. Denies sinus pain. Denies using inhalers or supplemental oxygen. Past Medical History: Admits to seasonal allergies. Denies food, medication, latex, and animal allergies. Allergies are worse in the springtime. She denies ever having an allergy test done. Currently takes Claritin 10mg once a day for allergies. Denies vitamins or herbal medication. Admits to missing 2 days of work due to cough, ear pain, and headache. Denies asthma diagnosis. Denies tuberculosis exposure. Denies hospitalization within the last year. States her immunizations are up to date. Denies ever having a cough like this before. Age 6 patient had her tonsils removed. States she has 1 child and had no difficulties with the birthing process. Family History: Denies family history of asthma or tuberculosis. Denies family history of respiratory problems. Social History: Current smoker. Has been smoking 1 pack a day for almost 20 years. States she is currently ready to quit. Admits to trying to quit in the past, attempts were unsuccessful. Denies chewing tobacco and illicit drugs. Admits to drinking 1-2 glasses of wine every weekend. Reports living at home with her significant other and child. Denies Objective Vital Signs: All WNL. General Survey: An alert and oriented 40-year-old female. She maintains eye contact and is dressed appropriately for this interview. She does not appear to be in acute distress. Head: Head is normocephalic and atraumatic. Face is symmetrical. Scalp nontender. Sinuses nontender. No other visible abnormal findings. Eyes: Pupils are equal, round and reactive to light. +3mm. Pupils accommodate accordingly. Convergence tested, no abnormal findings. Both eyes disc margin is sharp. Retina normal. Conjunctiva is moist and pink. Sclera is white. No discharge present. Ears: Right ear auditory canal is pink, tympanic membrane is pearly gray. Cone of light is at 5:00. No discharge present. No other abnormal findings for the right ear. Left ear auditory canal is erythematous, tympanic member is pearly gray. Cone of light is at 7:00. No discharge present. Nose: Nasal cavities are pink and patent. No discharge present. Septum is symmetrical. No other visible abnormal findings. Mouth and Throat: Oral mucosa is moist and pink. No tonsils present. Throat is pink with no cobblestoning or exudate. Gums are pink. Teeth are intact, no loose teeth. No foul odor from breath noted. No postnasal drip presents. Lymph nodes: Neck is symmetrical. No palpable masses noted. Respiratory: Chest rise is symmetrical. Breath sounds are present in all areas. No adventitious lung sounds. All areas are clear. Tactile fremitus is symmetrical, equal and vibration is expected. Bronchophony negative. All areas resonant. No dullness noted. No other abnormal findings. Cardiac: Audible S1, S2, without murmurs, gallops, clicks, or rubs. Abdomen: Abdomen is symmetrical and rounded. No scarring present. Bowel sounds are present is all quadrants. Negative for abdominal bruit. No tenderness for deep or light palpation. Liver and spleen nonpalpable. Tympany and dullness noted in appropriate quadrants. Skin: Skin is warm, dry, no edema present. No tenting noticed. Extremities: Upper extremities + 5. Lower extremities +5. Pulses felt bilaterally and equally in carotids, brachial, radial, popliteal, posterior tibial, and dorsal pedis areas. Assessment Diagnosis: Pneumonia Possible Diagnosis: Bacterial/Viral pneumonia, Legionnaire pneumonia, asthma, pulmonary embolism, bronchitis, influenza, common cold, acute sinusitis, tuberculosis, rhinitis Plan Ms. A will need a chest x-ray and possibly a chest CT. A chest x-ray will help determine if there is an infection in her lungs. A chest CT will help get a closer look at a possible infection. Acid fast bacilli smear can be used to diagnose or rule out tuberculosis An allergy test can be done to determine allergies or asthma triggers Blood cultures to detect any current infection An EKG can be ordered to evaluate the patient’s heart that may be affected by respiratory distress or respiratory disorders CBC and CMP to assess for elevated white blood cell count to indicate infection, to check electrolytes, liver and kidney functions Legionnaire disease antibody can be used to rule out a specific type of pneumonia Peak expiratory flow rate can help determine if the patient has asthma A respiratory PCR to rule out or identify any current infection Throat and nose cultures to detect any bacterial or viral infection A sputum culture should be gathered to identify or rule out infection, this helpful in diagnosing pneumonia and bronchitis I would also order Robitussin 10 mL every 6 hours for her cough, Ibuprofen 800 mg for her headache and ear pain, and then melatonin to help her sleep at night. Ms. A should be educated on proper hand washing techniques to prevent the spread of infection. Ms. A should also be given smoking cessation informational pamphlets to help her quit smoking