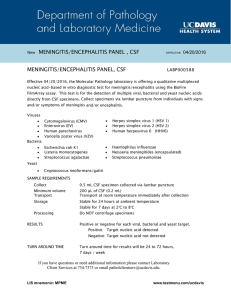
Bacterial & Viral Meningitis (1324-1326) Inflammation caused by: • Bacteria • Viruses • Fungi • Chemicals (contrast media, blood in subarachnoid space) CNS infections may occur via: • The bloodstream • By extension from a primary site • Along cranial and spinal nerves Rates – higher in older immunocompromised pts • Some who recover have long-term neuro deficits (hearing loss) Meningitis • Acute inflammation of meningeal tissues surround the brain and spinal cord • Usually occurs in fall, winter or early spring o Related to viral respiratory disease o Older adults and debilitated – affected more • College students living in dorms and people living in institutions (prisoners) have higher risk Bacterial meningitis • Etiology & pathophysiology o Streptococcus pneumoniae and Neisseria meningitidis = leading cause N. M. has 13 subtypes with 5 of them causing most cases (A, B, C, Y, W) H. influenzae used to be the most common cause before flu vaccine o Organisms gain entry to CNS through – URT or bloodstream May enter by direct extension from penetrating wounds of skull or through fractured sinuses in basilar skull fractures o Inflammatory response increases CSF production (w/ mod increase ICP) Purulent secretions quickly spread to other areas of brain through the CSF & cover CN and other intracranial structures If this process extends into the brain parenchyma or if concurrent encephalitis is present, cerebral edema and increased ICP become bigger problem • Clinical manifestations: o Key signs: Fever Severe HA (becomes progressively worse; + vomiting & irritability) Nausea Vomiting Nuchal rigidity (neck stiffness) o Photophobia, decreased LOC and signs of increased ICP may be present o Coma (5-10% pts) = poor prognosis o Seizures (1/3 of cases) o Rash – if meningococcus is infecting organism o Petechia – trunk, LE, mucous membranes Tumbler test – pressing base of drinking glass against the rash The rash does not blanch or fade under pressure • Complications o Most common = increased ICP o Residual neuro dysfunction (involving many cranial nerves) Optic nerve (2) – papilledema and blindness 3,4, 6 – ocular movements affected (pstosis, unequal pupils, diploplia) 5- sensory losses and loss of corneal reflex 7 – facial paresis 8 – tinnitus, vertigo, deafness (usually disappears but hearing loss may be permanent) o Hemiparesis, dysphasia, and hemianopsia o Acute cerebral edema may cause seizures, CN III palsy, bradycardia, hypertensive coma, and death o noncommunicating hydrocephalus – if exudate causes adhesions that prevent normal flow of CSF from ventricles o Waterhouse-Friderichsen syndrome petechiae, disseminated intravascular coagulation (DIC), adrenal hemorrhage, and circulatory collapse • Diagnostic studies: o Suspected = Blood culture & CT o To confirm diagnosis = LP w/ analysis of CSF LP done after CT scan has r/o obstruction in foramen magnum to prevent fluid shift resulting in herniation o Before starting abx – Culture CSF, sputum, and nasopharyngeal secretions Gram stain don’t to detect bacteria Abx started even before dx confirmed Predominant WBC in CSF w/ bacterial meningitis = neutrophils o X-rays of skull may show infected sinuses o CT and MRI may be normal in uncomplicated meningitis Other cases: CT may show increased ICP and hydrocephalus Signs/Symptoms. Brudzinski & Kernig’s sign • Kernig's is performed by having the supine patient, with hips and knees flexed, extend the leg passively. o The test is positive if the leg extension causes pain. o Helps in the diagnosis of meningitis • Brudzinski's sign is positive when passive forward flexion of the neck causes the patient to involuntarily raise his knees or hips in flexion. o Helps in the diagnosis of meningitis • Interprofessional Care Table 56-17 Diagnostic Assessment • History and physical examination • Analysis of CSF (for protein, WBC, and glucose), Gram stain, and culture • CBC, coagulation profile, electrolyte levels, glucose, platelet count • Blood culture • CT scan, MRI, PET scan • Skull x-ray studies Management • Rest • IV fluid • Hypothermia Drug Therapy • IV antibiotics • ampicillin, penicillin • cephalosporin (e.g., cefotaxime, ceftriaxone) • codeine for headache • dexamethasone • acetaminophen or aspirin for temperature >100.4° F (38° C) • phenytoin IV • mannitol (Osmitrol) IV for diuresis Transmission & Isolation • Respiratory isolation until cultures are negative o Meningococcal meningitis - Highly contagious Prevention & Nursing Care Prevention • Pneumonia and flu vaccines – to prevent respiratory tract infections • Meningococcal vaccines – protect against the serogroups that are most often seen in US but do not prevent all cases o 2 types: Meningococcal conjugate vaccines (MCV4) (Menactra, Menveo) Serogroup B meningococcal vaccines (Bexsero, Trumenba) • Early tx of respiraotyr tract and ear infections is important • Persons who have close contact with anyone who has bacterial meningitis should receive prophylactic antibiotics. Acute care • Assess and record vital signs, neurologic status, fluid intake and output, skin, and lung fields at regular intervals based on the patient’s condition. o Bacterial meningitis = acutely ill High fever, severe head pain, possible seizures, change in mental status/LOC o Codeine – pain relief (head and neck pain) o Position of comfort – curled up with head slightly flexed o HOB slighlty elevated o Darkened room and cool cloth over eyes (photphobia) o Delirium – low lighting may decrease hallucinations o Min. environmental stimuli o Familiar person at bedside= calming effect o Antiseizure drugs – phenytoin (Dilantin) or levetiracetam (Keppra) o Fever vigorously treated (because it increases cerebral edema and risk seizures) Acetaminophen or aspirin or cooling blanket (tepid sponge baths) o Assess dehydration and adequacy of fluid intake Ambulatory care • Adequate nutrition – high protein, high calorie in small, frequent feedings • ROM exercises and warm baths – muscle rigidity may persist • Assess vision, hearing, cognitive skills, and motor and sensory abilities after recovery, with appropriate referrals as indicated. Viral Meningitis • Most common cause: o Enteroviruses Spread through direct contact with respiratory secretions o Arboviruses o HIV & HSV • Viral manifestations: o headache o fever (moderate or high) o photophobia o stiff neck • diagnosis: o Expert EV test Sample of CSF used to determine if enterovirus present Results available within hours of symptoms onset • o CSF can be clear or cloudy Typical finding: lymphocytosis o Organisms not seen on gram stain or acid-fast smears o PCR (polymerase chain reaction) – used to detect viral-specific DNA or RNA Sensitive method for dx CNS viral infections o Antibiotics should be given after the LP while awaiting the results of the CSF analysis. Antibiotics are the best defense for bacterial meningitis. We can easily discontinue them if the meningitis is found to be viral. Management: o Self – limiting disease (managed symptomatically) o Full recovery expected o Rare sequelae = persistent HA, mild mental impairment, incoordination