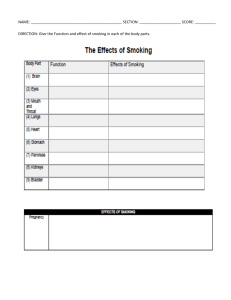
REVIEW ARTICLE Cigarette Smoking and Infection Lidia Arcavi, MD; Neal L. Benowitz, MD Background: Infectious diseases may rival cancer, heart disease, and chronic lung disease as sources of morbidity and mortality from smoking. We reviewed mechanisms by which smoking increases the risk of infection and the epidemiology of smoking-related infection, and delineated implications of this increased risk of infection among cigarette smokers. Methods: The MEDLINE database was searched for articles on the mechanisms and epidemiology of smokingrelated infectious diseases. English-language articles and selected cross-references were included. Results: Mechanisms by which smoking increases the risk of infections include structural changes in the respiratory tract and a decrease in immune response. Cigarette smoking is a substantial risk factor for important bacterial and viral infections. For example, smokers incur a 2- to 4-fold increased risk of invasive pneumococcal disease. Influenza risk is severalfold higher and is much C Author Affiliations: Clinical Pharmacology Unit, Kaplan Medical Center, Rehovot, Israel (affiliated with Hadassah and the Hebrew University School of Medicine, Jerusalem, Israel) (Dr Arcavi); Division of Clinical Pharmacology and Experimental Therapeutics, Medical Service, San Francisco General Hospital Medical Center, San Francisco, Calif (Dr Benowitz); and Department of Medicine, Psychiatry, and Biopharmaceutical Sciences, University of California, San Francisco (Dr Benowitz). Financial Disclosure: None. more severe in smokers than nonsmokers. Perhaps the greatest public health impact of smoking on infection is the increased risk of tuberculosis, a particular problem in underdeveloped countries where smoking rates are increasing rapidly. Conclusions: The clinical implications of our findings include emphasizing the importance of smoking cessation as part of the therapeutic plan for people with serious infectious diseases or periodontitis, and individuals who have positive results of tuberculin skin tests. Controlling exposure to secondhand cigarette smoke in children is important to reduce the risks of meningococcal disease and otitis media, and in adults to reduce the risk of influenza and meningococcal disease. Other recommendations include pneumococcal and influenza vaccine in all smokers and acyclovir treatment for varicella in smokers. Arch Intern Med. 2004;164:2206-2216 METHODS IGARETTE SMOKING IS A well-known major risk factor for premature mortality due to cancer, cardiovascular disease, and chronic obstructive pulmonary disease. Cigarette smoking also appears to be a major risk factor for respiratory tract and other systemic infections. Both active and passive cigarette smoke exposure increase the risk of infections. The morbidity and mortality of infectious diseases due to smoking are not widely appreciated by physicians. The mechanism of increased susceptibility to infections in smokers is multifactorial and includes alteration of the structural and immunologic host defenses. The aims of this article are to review the mechanisms by which smoking increases the risk of infection, to review the epidemiology of smoking-related infections, and to discuss implications of the increased risk of infection among cigarette smokers. (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2206 The MEDLINE database was searched for articles on the mechanisms and epidemiology of smoking-related infectious diseases. All relevant English-language articles published between 1978 and 2003 in the MEDLINE database were searched, by using the terms cigarette smoking and immune system, cellular immunity, humoral immunity, white blood cell, cytokine, and chemotaxis, as well as cigarette smoking with various specific infectious diseases. Selected references contained in these articles were also reviewed. Studies were included if they appeared to be scientifically valid; however, no formal quality rating system was used to screen articles for inclusion. MECHANISMS BY WHICH SMOKING MAY PREDISPOSE TO INFECTION The specific mechanisms by which cigarette smoking increases the risk of systemic infections are incompletely understood. They are multifactorial and probably interactive in their effects. They include structural and immunologic mechanisms. WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 Mechanical and Structural Changes Caused by Smoking Cigarette smoke and many of its components produce structural changes in the respiratory tract. These changes include peribronchiolar inflammation and fibrosis, increased mucosal permeability, impairment of the mucociliary clearance, changes in pathogen adherence, and disruption of the respiratory epithelium.1 These changes are thought to predispose to the development of upper and lower respiratory tract infections, which may amplify the cigarette smoke– induced lung inflammation. A number of components of cigarette smoke, including acrolein, acetaldehyde, formaldehyde, free radicals produced from chemical reactions within the cigarette smoke, and nitric oxide, may contribute to the observed structural alterations in the airway epithelial cells.2,3 Immunologic Mechanisms Cigarette smoking affects both cellmediated and humoral-mediated immune responses in humans and animals.4-6 Cell-Mediated Immune Responses. Cell Counts and Distribution in Peripheral Blood. Smokers on average exhibit an elevated peripheral white blood cell count, about 30% higher than that of nonsmokers. All major cell types are increased.6-10 Taylor et al11 found a significant relationship between the total white blood cell count in smokers and the plasma concentration of nicotine. Friedman et al9 suggested that nicotineinduced catecholamine release might be the mechanism for this effect. Other studies support the hypothesis that cigarette smoking causes bone marrow stimulation. Van Eeden and Hogg12 found that polymorphonuclear leukocytes (PMNs) from long-term smokers have phenotypic changes indicating bone marrow stimulation, such as increase in band cell counts, higher levels of L-selectin, and increased myeloperoxidase content. The authors suggested that proinflammatory factors released from alveolar macrophages, such as tumor necrosis factor ␣, interleukin (IL) 1, IL-8, and granulocyte-macrophage colony-stimulating factor, are probably responsible for the stimulation of bone marrow by cigarette smoking. Vanuxem et al13 found that white blood cell count in smokers was related to the carboxyhemoglobin concentration reflecting exposure to cigarette smoke. Tell et al14 showed the same relationship between cigarette smoking and increased leukocyte count in adolescents, indicating that there appears to be a rapid effect of cigarette smoking on white blood cell count that is unlikely to be due to smokinginduced chronic disease conditions as seen in adult smokers. Reports of the effects of smoking on the different subsets of lymphocyte T cells are conflicting. The influence of cigarette smoking on lymphocyte T-cell subpopulations in the peripheral blood has been investigated by means of monoclonal antibodies. Light to moderate smokers (history of less than 50 packyears) were reported to have a significant increase in CD3+ and CD4+ counts and a trend toward increased CD8+ lymphocyte count. The observed increase in the ratio of CD4+ to CD8+ lymphocytes in light smokers was due to the increase of CD4+ cells.6,10,15-17 Two to 4 years after smoking cessation, the increase in CD4+ cells disappeared.15,18 By contrast, studies of heavy smokers (ⱖ50 pack-years) reported a decrease in CD4+ and a significant increase in CD8+ cell counts. Thus, the decrease observed in the ratio of CD4+ to CD8+ lymphocytes in heavy smokers was due predominantly to an increase of CD8+ cells.16 These effects appeared to be reversible as soon as 6 weeks after smoking cessation,17 although in one study6 it took 2 to 4 years for these effects to disappear. Other studies have reported no difference in the CD4+ and CD8+ lymphocyte counts among moderate smokers.19 Since CD4+ cells facilitate B-cell proliferation and differentiation and immunoglobulin synthesis, the decrease in this subset observed in heavy smokers might contribute to the increased susceptibility to infections in this population. An increase in CD8+ cells, such as that observed in heavy smokers, has been (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2207 associated with both neoplasia and infection.20 Studies on Lung Fluids. The results of studies of bronchoalveolar fluid from smokers differ from findings in the peripheral blood. Bronchoalveolar lavage studies19,21,22 have demonstrated a marked decrease in the percentage and absolute number of CD4+ cells, and an increase in CD8+ cells with a lower CD4+/CD8+ cell ratio in moderate smokers (average, 14 pack-years) vs nonsmokers. No significant changes in these variables in the peripheral blood were found in this population of moderate smokers, in contrast with the findings in heavy smokers discussed previously. Thus, changes in lymphocyte population in the bronchoalveolar lavage in smokers may disclose pathologic changes earlier than in blood. Moreover, these findings suggest that smokers have a deficit in cell-mediated immunity in the lung alveolus, a site critical in the first-line defense against infection. Smoking is also associated with significant increases in the percentage of macrophages22 in bronchoalveolar lavage fluid. Effects on PMN Function. Several studies have shown that cigarette smoking affects the function of white blood cells.23,24 Polymorphonuclear leukocytes from the peripheral blood of smokers exhibit depressed migration and chemotaxis compared with PMNs from nonsmokers.24,25 The motility and chemotaxis of PMNs are depressed in the oral cavity of smokers compared with nonsmokers.24,26 Which constituents of smoke are responsible for these effects remains unclear. Bridges et al27 demonstrated that whole cigarette smoke, its gas phase, and the water-soluble fraction were potent inhibitors of PMN chemotaxis. Of the water-soluble fraction of cigarette smoking, the unsaturated aldehydes (acrolein and crotonaldehyde) were the major contributors to the inhibitor properties. Bridges and Hsieh28 showed that the nonvolatile components of cigarette smoking also inhibit chemotaxis by a mechanism that differs from that of the unsaturated aldehydes present in the vapor phase of smoke. The nonvolatile component did not inhibit migration. A relationship was observed between WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 the polarity of a fraction and its inhibitory potency; thus, the inhibition of PMN chemotaxis could not be attributed to either nicotine or the polycyclic hydrocarbons. Sasagawa et al29 found that nicotine had no effect on PMN migration and chemotaxis. Macrophages from the lungs of smokers have a greater inhibitory effect on lymphocyte proliferation than macrophages from the lungs of nonsmokers. Thus, the immunosuppressive effects of the macrophages on cell-mediated immune response are increased in smokers.30 The release of cytokines from macrophages may also be altered in smokers.31 Twigg and coworkers32 showed that cigarette smoking decreases the secretion of the proinflammatory cytokines such as IL-1 and IL-6. Wewers et al22 showed decreased production of tumor necrosis factor ␣. Ouyang et al33 and Hagiwara et al34 reported that cigarette smoking also suppresses IL-2 and interferon ␥ production. Hydroquinone, the phenolic compound in cigarette tar, had the most potent inhibitory effect of these cytokines, whereas nicotine had little effect. On the other hand, IL-10 production by human mononuclear cells was inhibited by treatment with nicotine patches in patients with inflammatory bowel disease.35 Recently, Matsunaga et al36 reported that nicotinic acetylcholine receptors are involved in the cytokine responses of alveolar macrophages to Legionella pneumophila infection. The cytokines IL-1 and IL-6 are important in the host defense against infection.37,38 Animal studies have shown that depletion of these cytokines increases susceptibility to bacterial pneumonia. Since PMNs play a significant role in host defense against acute bacterial infections, an impairment of PMN functions by smoke may contribute to the increased susceptibility of smokers to systemic infections, including bacterial pneumonia. Effects on Lymphocyte Functions. Natural killer (NK) cell activity in peripheral blood has been reported to be reduced in smokers compared with nonsmokers.6,15,39-41 Using a cytotoxicity assay, Ginns et al16 found that smokers had 47% of the NK activity of nonsmokers. These al- terations appear to be reversible, since NK activity in ex-smokers was similar to that of a never-smoking group compared with smokers.18,42 The recovery period was relatively short, as little as 6 weeks.15,17 Since NK cells are important in the early surveillance response against viral infections and resistance against microbial infections,43,44 impairment of NK cell activity by cigarette smoking is a potential mechanism for the increased incidence of infections among smokers. The molecular mechanisms by which cigarette smoking alters lymphocyte function, as described previously, are still poorly defined. Animal studies have shown that nicotine inhibits the antibody-forming cell response through impairment of antigen-mediated signaling in T cells and suppression of intracellular calcium response.5,45,46 Kalra et al47 exposed rats to mainstream cigarette smoke or to nicotine via constantrelease osmotic pumps for up to 30 months and concluded that nicotine was the major immunosuppressive component in cigarette smoking. One suggested mechanism was through activation of protein tyrosine kinases and the depletion of inositol-1,4,5-trisphosphate–sensitive calcium stores in T cells.47 Humoral Immune System. Peripheral Blood. The effects of cigarette smoking on humoral immunity have been studied extensively.4,5 Several studies have found that smokers had serum immunoglobulin levels (IgA, IgG, and IgM) 10% to 20% lower than those of nonsmokers.39,48-51 Mili et al10 found that IgA, IgG, and IgM levels were higher among former smokers than current smokers and increased with duration of smoking cessation. This suggests that the effect was reversible, with a return toward the immunoglobulin levels of nonsmokers. Hersey et al18 found that 3 months after subjects stopped smoking, IgG and IgM but not IgA levels had increased compared with levels during smoking. Lung Fluids. The IgG content of bronchial fluids was found to be twice as high in smokers than nonsmokers.18,52 A selective increase in immunoglobulin levels could be ex- (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2208 plained either by stimulation of local immunoglobulin production or by exudation of plasma immunoglobulin into alveolar spaces in response to inhaled cigarette smoke.53 The availability of opsonic antimicrobial antibodies is essential for optimal function of phagocytes to take up and contain bacteria.54 The antibody response to a variety of antigens, such as influenza virus infection and vaccination55 and Aspergillus fumigatus,56 is depressed in cigarette smokers. Summary of Immunologic Effects of Cigarette Smoking. In summary, cigarette smoking is associated with a variety of alterations in cellular and humoral immune system function. These alterations include a decreased level of circulating immunoglobulins, a depression of antibody responses to certain antigens, a decrease in CD4+ lymphocyte counts, an increase in CD8+ lymphocyte counts, depressed phagocyte activity, and decreased release of proinflammatory cytokines. The pathogenesis of smoking effects on the immune system is not well understood. Some investigatorshavedemonstratedanantigenic role of substances in cigarette smoking, resulting in the development of antigen-antibody complexes. These complexes are capable of causing pulmonary and peripheral changes in responses of the humoral and cellmediated system. Hersey et al18 and Costabel et al19 suggested that the antigen-antibody complexes may induce localized alterations of the immune status of the saliva and the bronchoalveolar fluid and predispose to respiratory tract infections. Smoking, via the effects of nicotine, can stimulate catecholamine and corticosteroid release. These mediators might increase CD8+ lymphocytes in the cellular-mediated system17 and suppress the host defense against infections. It is important to recognize that many of the immunologic abnormalities in smokers resolve within 6 weeks after smoking cessation, supporting the idea that smokingcessationiseffectiveinarelatively short time in the prevention of infections. The results of several studies suggest that nicotine is an important im- WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 6 Nuorti et al, 2000 58 Almirall et al, 199959 Smoking Status Odds Ratio* (95% CI) Attributable Risk, % Current smoker ⬎25 Cigarettes/d 30 Pack-years Passive smoker Never smoked Current smoker ⬎20 Cigarettes/d ⬎38 Pack-years Never smoked 4.1 (2.4-7.3) 5.5 (2.5-12.9) 3.2 (1.6-6.9) 2.5 (1.2-5.1) 1.0 1.88 (1.11-3.19) 2.97 (1.52-5.81) 3.15 (1.52-6.51) 1.00 51 17 SMOKING AND CLINICAL INFECTIOUS DISEASES General Considerations With Respect to Epidemiologic Studies In evaluating epidemiologic studies reportinganassociationbetweencigarette smoking and infectious diseases, one must consider the possibility of confounding. Compared with nonsmokers, cigarette smoking is associated with lower socioeconomic status, different diet, greater alcohol and drug use, lower levels of physical activity, and more risk-taking behaviors, including risky sexual behaviors. Most studies have controlled for factors such as age, sex, race/ethnicity, alcohol consumption, sexual habits, etc, although not every study has controlled for every possible confounder. Because of space limitations, we are unable to describe which factors were controlled for every study, but we have selectively commented on controls for particular studies where it seemed relevant. Bacterial Infections Pneumococcal Pneumonia. Cigarette smoking is a substantial risk factor for pneumococcal pneumonia, especially in patients with chronic obstructive pulmonary disease. However, even without chronic obstructive pulmonary disease, smoking is a major risk factor. In a populationbased surveillance study conducted in Dallas County, Texas, in 1995,57 smoking was strongly associated with 1-14 >24 Figure 1. Cigarette consumption and the risk of pneumococcal disease (data from Nuorti et al58). 4 3 2 1 0 <5 5-9 ≥10 No. of Years Since Quitting Smoking Figure 2. Decline in the risk of pneumococcal disease (data from Nuorti et al58). In vitro adherence of Streptococcus pneumoniae to buccal epithelial cells has been shown to be increased in cigarette smokers.60 This increased adherence may persist for up to 3 years after smoking cessation. Since increasedadherenceofbacteriatosurface cells is an established pathogenic step for bacterial colonization and infection in both lung and other organs, this may contribute to the increased risk of respiratory infection that exists in cigarette smokers. Legionnaires Disease. Legionnaires disease is a life-threatening bronchopneumonia responsible for 1% to 3% of community-acquired pneumonia. Diverse environmental factors have been identified, and cigarette smoking appears to be an independent risk factor.61 Straus et al62 reported that the risk of legionnaires disease was increased 121% per cigarette pack consumed daily, with an OR of 3.48 (95% CI, 2.09-5.79) for smoking. For persons without an underlying disease, the OR for smokers compared with nonsmokers was 7.49 (95% CI, 3.27-17.17). WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 15-24 No. of Cigarettes Smoked Daily invasive pneumococcal disease in otherwise healthy young and middleaged adults (30 to 64 years of age), for whom pneumococcal vaccination is not currently recommended. Among such individuals with invasive pneumococcal disease, 47% were current smokers. The odds ratio (OR) for invasive pneumococcal disease was 2.6 (95% confidence interval [CI], 1.9-3.5) for smokers in the 24to 64-year age group and 2.2 (95% CI, 1.4-3.4) for smokers 65 years or older. The attributable risk from smoking was 31% and 13% in these 2 groups, respectively. A recent populationbased case-control study58 showed that smoking was the strongest independent risk factor for invasive pneumococcal disease among immunocompetent adults. The OR was 4.1 (95% CI, 2.4-7.3) for active smoking and 2.5 (95% CI, 1.2-5.1) for passive smoke exposure in nonsmokers compared with nonexposed nonsmokers (Table 1). The attributable risk in this population was 51% for cigarette smoking and 17% for passive smoking. This effect showed a strong dose-response relationship (Figure 1). The risk of pneumococcal disease declined to nonsmoker levels 10 years after cessation (Figure 2). In another case-control study, Almirall et al59 found that current smoking was associated with a nearly 2-fold risk of community-acquired pneumonia (OR,1.88; 95% CI, 1.113.19), where 32% of the risk was attributable to cigarette smoking. In this study, there was a trend toward a dose-response relationship. A 50% reductionintheORwasreported5years after cessation of smoking. Table 1 summarizes these results. (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2209 2 0 Abbreviation: CI, confidence interval. *Adjusted for multiple variables (age, sex, race, chronic illness, level of education, and residence). munosuppressive component of cigarette smoke, but other components also appear to have a role. 4 32 Odds Ratio Source Odds Ratio Table 1. Cigarette Smoking and Risk of Pneumococcal Infections Meningococcal Disease Active Smokers. In a case-control study by Fischer et al,63 36% of patients with meningococcal disease were current smokers, while 14% were nonsmokers (OR, 2.4; 95% CI, 0.9-6.6). During an outbreak of serogroup C meningococcal disease among college students, 4 of 6 cases were in cigarette smokers, a prevalence much higher than that of exposed controls (OR, 7.8; 95% CI, 1.3-64.4).64 Cigarette smoking is associated with meningococcal colonization of the nasopharynx. Stuart et al65 found that 55% of active smokers were carriers compared with 36% of nonsmokers and 76% of those exposed to secondhand tobacco smoke. The risk of carriage associated with active smoking increased with the daily number of cigarettes smoked. The OR for all smokers was 2.3 (95% CI, 1.2-4.6), with a greater risk for smokers of more than 20 cigarettes per day. Caugant et al66 performed a survey among a Norwegian population and found that active smoking was independently associated with meningococcal carriage (OR, 2.79; 95% CI, 1.67-4.64). There was no association between the number of cigarettes smoked daily and carriage. A similar pattern was found in a study conducted among recruits in Greece.67 Exposure to Secondhand Tobacco Smoke. Secondhand tobacco smoke exposure has also been associated with an increased risk of meningococcal disease. In a case-control study, Fischer et al63 established a strong epidemiologic link between smoking and meningococcal disease in children. For children younger than 18 years, having a mother who smoked was the strongest independent risk factor for invasive meningococcal infection compared with other risk factors such as maternal education, no primary physician, or humidifier use (OR, 3.8; 95% CI, 1.6-8.9). Thirty-seven percent of the infections could be attributed to maternal smoking. The number of smokers living in the home and the number of packs smoked per day had a significant linear relationship with the risk of meningococcal disease. No such association was ob- served for paternal smoking in this study. Among adult patients with meningococcal disease, 50% were passive smokers compared with 29% controls (OR, 2.5; 95% CI, 0.9-6.9). In the Norwegian population survey, Caugant et al66 found a doubling of carriage rate for passive smokers (OR, 2.30; 95% CI, 1.21-4.37). In a prospective study, Haneberg et al68 found that passive smoking in children younger than 12 years was significantly more frequent in meningococcal patients (62%) than the population controls (32%) (P⬍.001). There are several potential mechanisms by which tobacco might increase the risk of meningococcal disease. One is that tobacco smoke is a risk factor for meningococcal nasopharyngeal carriage, so that persons living with smokers have a greater chance to be exposed to meningococci. A second possible mechanism is that a preceding viral infection, which is more frequent in smokers, can act as a cofactor for meningococcal disease. During an outbreak of meningococcal disease in Los Angeles County, California, patients with meningococcal disease were more likely than matched neighborhood controls to have had an upper respiratory tract infection (OR, 3.2; 95% CI, 1.4-7.1) or to be exposed to a household visitor with an upper respiratory tract infection (OR, 2.6; 95% CI, 1.02-6.6).69 Third, ineffective humoral immunity against the Neisseria meningitidis polysaccharide capsule is a wellrecognized risk factor for invasive meningococcal disease. Otitis Media and Exposure to Secondhand Tobacco Smoke. Longterm tobacco smoke exposure is a risk factor for otitis media and bronchitis in children.3 In a prospective study, 175 children with recurrent otitis media were compared with an age-matched group of 175 children to determine the role of passive cigarette smoking on the incidence of this disease. The case group more commonly had exposure to secondhand smoke, with an OR of 1.88 (95% CI, 1.02-3.49) (P=.04). Prospective follow-up of the case group showed no significant difference in the clinical course of the children who were exposed to secondhand (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2210 smoke and those who were not.70 Ilicali et al71 examined the development of otitis media with effusion and recurrent otitis media in 166 children 3 to 7 years old, compared with an age-matched control group of 166 children. Passive smoking was a significant risk factor for otitis media with effusion and recurrent otitis media. The case group was exposed to smoke from a mean of 19.6 cigarettes per day vs 14.4 cigarettes per day for the control group (P⬍.004). Only maternal smoking was a significant factor (P⬍.001). Moreover, in utero exposure to cigarette smoke was associated with an increased risk of otitis media. In a study carried out by Stathis et al,72 acute ear infections were associated with the mother’s consumption of 1 to 9 cigarettes (OR, 1.6; 95% CI, 1.1-2.5), 10 to 19 cigarettes (OR, 2.6, 95% CI, 1.6-4.2), and 20 or more cigarettes (OR, 3.3; 95% CI, 1.95.9) per day during pregnancy. For subacute ear infections, an association was present with the mother’s consumption of 10 to 19 cigarettes (OR, 2.6; 95% CI, 1.4-5.0) and 20 or more cigarettes (OR, 2.8; 95% CI, 1.3-6.0). In utero exposure to 20 or more cigarettes per day was also associated with an increased risk of ear surgery by 5 years after delivery (OR, 2.9; 95% CI, 1.3-6.6). Periodontal Disease. Tobacco use is a substantial risk factor for periodontal disease.73,74 Smokers are 2.5 to 6 times more likely to develop periodontal disease than nonsmokers, and there is a direct relationship between the number of cigarettes smoked and the risk of developing periodontal disease. Among current smokers, the odds of periodontitis range from 2.79 (95% CI, 1.90-4.10) for 9 or fewer cigarettes per day to 5.88 (95% CI, 4.038.58) for 31 or more cigarettes per day. Among former smokers, the odds of periodontitis declined with the number of years since quitting, from 3.22 (95% CI, 2.18-4.76) for 0 to 2 years to 1.15 (95% CI, 0.831.60) for 11 or more years since quitting.75 The severity of periodontal disease is also increased in smokers and the postoperative results are poorer WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 than those achieved in nonsmokers.76 There is a direct relationship between tobacco use and increased attachment loss, pocket depth, and reduced bone crest height.77,78 Smokers have a greater extent of subgingival bacterial colonization than never-smokers.79,80 Helicobacter pylori Infection. The pathogenesis of peptic ulcer disease is multifactorial. Helicobacter pylori infection and smoking are wellestablished risk factors. More than 95% of duodenal ulcers are associated with H pylori infection, and treatment of H pylori markedly reduces ulcer recurrence rates. Smokers are more likely to develop ulcers.81 Ulcers in smokers take longer to heal82 and relapse more often in smokers compared with nonsmokers.83-85 Moshkowitz et al86 found that gastric and duodenal ulcers were more prevalent in smokers than nonsmokers (gastric, 4.1% vs 1.8%; duodenal, 50% vs 39.8%, respectively; P⬍.05). Bateson,87 in a prospective study, reported that 51.8% of patients with duodenal ulcers and 48.8% of those with gastric ulcers were smokers, compared with 31.8% of the controls. This study reported an association between current smoking and H pylori infection in patients with normal results of endoscopy. Current cigarette smokers had a higher rate (49.6%) of H pylori infection than nonsmokers and ex-smokers (35.5%) (P⬍.01). In another study, 73% of H pylori– positive smokers had a duodenal or gastric ulcer, whereas only 27% of seropositive nonsmokers had ulcers.88 Recently, Nakamura et al89 reported an increased risk of severe atrophic gastritis and intestinal metaplasia associated with smoking (OR, 9.31; 95% CI, 3.85-22.50; and OR, 4.91; 95% CI, 1.90-12.68) within H pylori–positive subjects. Nicotine potentiates the vacuolating toxin activity of H pylori. This toxin may be an important determinant of the virulence of H pylori. In an in vitro model, Cover et al 90 showed that treatment of cells with nicotine after exposure to H pylori toxin induces formation of vacuoles within eukaryotic cells and incites mucosal damage. While ciga- rette smoking is a strong predictor of recurrent ulcer in the presence of H pylori treatment, cigarette smoking appears to have little effect on ulcer healing after eradication of H pylori.91 Borody et al92 showed that, in 197 patients with eradicated H pylori and cured duodenal ulcer by endoscopy examination, there was no recurrence of ulcer, regardless of smoking status during a follow-up period of 6 years. These observations support the idea that a major mechanism by which smoking increases ulcer disease is by increasing the rate of infection and/or the virulence of H pylori. Viral Infections Common Cold. Large epidemiologic studies support the association between smoking and the prevalence of colds and lower respiratory tract symptoms. In a prospective cohort study, Blake et al93 examined a large group of US Army recruits (1230 soldiers) and found that 22.7% of smokers had upper respiratory infection compared with 16% of nonsmokers; a relative risk of 1.5 (95% CI, 1.1-1.8). Cohen et al94 showed that smoking status was predictive of the development of clinical colds when they exposed 400 healthy volunteers intranasally to a low dose of 1 of 5 respiratory viruses. Viral suspensions were installed into the nares and infections were diagnosed on the basis of viral isolation, virus-specific antibody, and clinical findings. Smokers had a significantly higher incidence of acute infection (clinical cold) than nonsmokers, with an OR of 2.23 (95% CI, 1.03-4.82). Among virologically confirmed infected individuals, smoking was associated with a higher likelihood of symptoms leading to a clinical diagnosis (OR, 1.83; 95% CI, 1.00-3.36). This risk for smokers was independent of alcohol consumption, as well as of demographic, environmental, immunologic, and psychological variables. Cohen et al94 suggested that the relationship between smoking and increased symptoms from viral respiratory infections could be explained by impairment of immune processes that limit viral replication or (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2211 enhancement of inflammatory processes involved in the production of symptoms. When Vitalis et al95 exposed guinea pigs with latent adenoviral infection to a single dose of cigarette smoke, they developed a more aggressive inflammatory response. An important feature of adenovirus infection is that portions of its viral DNA persist in host cells after viral replication has stopped. This may be important in the pathogenesis of permanent airway obstruction, bronchiectasis, chronic obstructive pulmonary disease, and emphysema. The probable mechanism is through a protein expressed by the latent viral DNA. This protein amplifies the expression of genes that are activated in cigarette smoke–induced airway inflammation.96 Influenza. Several studies have confirmed the relationship between cigarette smoking and the risk of influenza infections.97 Influenza infections are more severe, with more cough, acute and chronic phlegm production, breathlessness, and wheezing in smokers. Female smokers in the Israeli Army had a 60% risk of influenza compared with 41.6% in nonsmokers (OR, 1.44; 95% CI, 1.03-2.01). They also had a 44% increase in complications (visited the clinic more frequently) during an epidemic influenza illness caused by the A(H1N1) subtype.98 In another study of 336 healthy young male recruits in the Israeli military unit conducted by Kark et al, 99 the incidence of influenza was 68.5% among smokers and 47.2% among nonsmokers (P⬍.001). The OR was 2.42 (95% CI, 1.53-3.83). Influenza was more severe among smokers, with a dose-related increase in rate: 30% in nonsmokers, 43% in light smokers, and 54% in heavy smokers (P ⬍.001). Work loss occurred in 50.6% of smokers and 30.1% of nonsmokers. Overall, 31.2% (95% CI, 16.5-43.1) of influenza cases were attributed to cigarette smoking. Enhanced bacterial adherence has been documented for respiratory cells infected, with influenza A virus being responsible for viral-bacterial combination pneumonia.100 Studies have suggested that inflammatory activation of platelet-activating factor is an WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 important factor in the attachment and invasion of cells by pneumococcal strains. Cigarette smoking alters platelet-activating factor metabolism and may contribute to the increased incidence of bacterial superinfection in people who develop influenza.101,102 Although influenza was more severe in smokers, smokers’ antibody levels to A(H1N1) antigen were not significantly higher than those of nonsmokers. Only 50% of those with severe disease achieved titers greater than 20. Moreover, influenza antibodies wane more rapidly in smokers than in nonsmokers.55 This finding suggests that smokers are not only at a high risk of influenza, but have an increased susceptibility to new attacks afterward.99 Influenza rates are similar in vaccinated smokers and nonsmokers. However, influenza vaccination can be considered to be moreefficacious in smokers than nonsmokers because the infection rates arehigherinunvaccinatedsmokers.103 Varicella. In adults, varicella infection is associated with a substantial incidence of complications. One of these complications is varicella pneumonitis, for which smokers appear to be at greater risk. Ellis et al104 showed that among 29 adults with varicella infection, 7 of the 19 smokers were hospitalized with pneumonitis, but none of the 10 nonsmokers developed pneumonia. Later, Grayson and Newton-John105 reported a 15-fold risk of varicella pneumonitis in smokers compared with nonsmokers and varicella (P⬍.001). Human Papillomavirus Infections. Human papillomavirus (HPV) infection of the lower genital tract is one of the most common sexually transmitted diseases and is the cause of cervical intraepithelial neoplasia. Although the human papillomavirus is the infectious agent, the clinical manifestations of HPV are a function of the interaction of the virus and other factors such as the patient’s cell-mediated and humoral immune system, as well as patient characteristics such as smoking.106 The incidence of HPV infection is difficult to establish, since most of the infections are transient and, un- til the advent of polymerase chain reaction–based diagnostic techniques, the serologic measurements did not have good sensitivity or specificity. Between 7% and 50% of teenage patients are infected with HPV,107,108 depending on their sexual behavior. The association of cigarette smoking, both active and passive, with HPV expression and cervical intraepithelial neoplasia is strong. A relative risk of 2.7 (95% CI, 1.7-4.3) for smoking has been reported.109 Nicotine and other constituents of smoke have been found in the cervical mucus of active and passive smokers.110 These constituents have been associated with decreased numbers of Langerhans cells in the cervix in a cytologic examination.106 The Langerhans cells are part of the antigen–T-lymphocyte cell-mediated immune response system and are responsible for recruiting CD4+ lymphocytes, which are necessary for the local immune response. Patients who did not respond to interferon treatment for HPV had low levels of CD4+ lymphocytes and a low CD4+/CD8+ ratio. This ratio was nearly normal in patients who responded to interferon treatment.111 The at-risk profile of low CD4+/CD8+ ratio is similar to that due to smoking described earlier in this article. In addition, some studies have shown that vitamin A and beta carotene protect against cervical intraepithelial neoplasia.112 Cigarette smokers have decreased serum beta carotene levels. Most likely, cigarette smoke acts as a cofactor facilitating HPV infection and as an immune suppressant. However, the virus and smoking are independent and additive in their effects on the immune system. Human Immunodeficiency Virus Infection. A few studies have investigated cigarette smoking as a cofactor for AIDS in individuals infected with human immunodeficiency virus (HIV). The first association between smoking and AIDS was observed by Newell et al. 113 Later, Royce and Winkelstein114 reported an elevated risk of AIDS and a more rapid progression in seropositive smokers compared with nonsmokers. In 1990, Boulos et al 115 reported an association between smok- (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2212 ing and HIV infection in pregnant Haitian women. Women who smoked 4 or more cigarettes per day had a 25% HIV-1 seropositive rate, compared with 9.6% for women who smoked fewer than 4 cigarettes per day. The association between HIV infection and smoking was confounded by an association between cigarette smoking and high-risk sexual behavior, but cigarette smoking was found to be an independent risk factor after controlling for both high-risk sexual behavior and HIV infection in this population. The OR for smoking and HIV infection was significant (OR, 3.4; 95% CI, 1.6-7.5). On the other hand, Burns et al116 observed a higher HIV seroconversion rate in persons who were homosexual who smoked than in nonsmokers, but found no effect of smoking on clinical outcome in their cohort. Similar results were also reported by Craib et al,117 who failed to find a significant association between cigarette smoking and the development of Pneumocystis carinii pneumonia. Although the association between smoking and HIV infection could be due to a confounding factor such as participation in highrisk behaviors, a biological effect of cigarette smoking must be considered. Nicotine and cotinine are concentrated in the cervical secretions of women who smoke 118,119 and could alter local immune factors and increase susceptibility to viral infections of the genital tract. In patients infected with HIV, smoking is also associated with an increased incidence of bacterial pneumonia. In a multicenter study done by the Pulmonary Complications of HIV Infection Study Group, this smoking effect was strongest in the most lymphopenic subgroup of patients.120 As discussed previously, cigarette smoking is associated with an increase in the percentage of CD4+ in blood in seronegative populations. Several studies112,114,116,117,121,122 have shown that these effects are attenuated in the HIV-infected smoking population during the first 2 years of infection. Analysis of the data suggested that an effect of smoking is present within the first few years of HIV infection but then disappears, and these patients ex- WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 perience a marked decrease in CD4+ counts. In other words, when smokers become infected with HIV, it takes up to 2 years for viral-related depletion of CD4 cells to overwhelm the smoking effect. In contrast, a significant decrease in CD4 and CD8 cells is seen in their bronchoalveolar lavage fluid, suggesting that cigarette smoking has a significant impact on lung defenses in HIV-infected individuals.22 In HIV-infected patients, cigarette smoking increases the risk of oral candidiasis (relative risk, 1.32; 95% CI, 1.02-1.70), hairy leukoplakia (associated with Epstein-Barr virus infection; relative risk, 1.51; 95% CI, 1.15-1.99), and communityacquired pneumonia (relative risk, 2.62; 95% CI, 1.30-5.27).116,122 Tuberculosis Persons at special risk for tuberculosis include immune-suppressed individuals and persons of low socioeconomic status. Several studies have shown that smoking is a risk factor for tuberculin skin test reactivity, skin test conversion, and the development of active tuberculosis. Yu et al123 reported that the relative risk of development of tuberculosis for heavy smokers compared with nonsmokers was 2.17 (95% CI, 1.29-3.63). Buskin et al124 found that, after adjusting for age and heavy drinking, smokers of 20 years’ or greater duration had 2.6 times (95% CI, 1.1-5.9) the risk of nonsmokers for tuberculosis. Alcaide et al125 also found a strong association between active smoking and the risk of pulmonary tuberculosis. Both studies showed a dose-response relationship with the number of cigarettes consumed daily. McCurdy et al126 reported an incidence of 16.6% in tuberculin reactivity (⬎10 mm in duration at 48 to 72 hours) among Hispanic migrant farm worker residents in California. This prevalence was higher for former smokers than for neversmokers (OR, 3.11 [95% CI, 1.28.09] vs 1.00). Current smokers had a nearly 2-fold increased risk compared with never-smokers (OR, 1.87; 95% CI, 0.73-4.80). In a case-control study among incarcerated adults, Anderson et al127 reportedan81%rateoftuberculinskin Table 2. Cigarette Smoking and Risk of Tuberculosis OR (95% CI) Smoking Status Observed Tuberculin Reactivity* Skin Test Conversion† Smoking history Never Former Current 1.00 3.11 (1.20-8.09) 1.87 (0.73-4.80) 1.00 1.00 1.78 (0.98-3.21) Current or former Duration of smoking ⬍15 y ⱖ15 y Cigarettes/d ⬍20 ⱖ20 ⬍10 ⱖ10 Cigarettes/y ⱕ199 200-399 ⱖ400 1.00 1.4 (0.8-2.3)‡ 1.3 (0.8-2.1)‡ 2.17 (1.29-3.63)§ 3.8 (1.5-9.8)储 2.4 (1.9-3.0)¶ 1.60 (0.81-3.16) 2.12 (1.03-4.36) 3.0 (1.3-7.9)储 13.0 (2.3-73.8)储 1.7 (1.4-2.2)¶ 2.6 (2.2-3.1)¶ 0.96 (0.59-1.55)§ 1.16 (0.66-2.04)§ 2.17 (1.29-3.63)§ Abbreviations: CI, confidence interval; OR, odds ratio; TB, tuberculosis. *From McCurdy et al.126 †From Anderson et al.127 ‡From Buskin et al.124 §From Yu et al.123 储From Alcaide et al.125 ¶From Gajalakshmi et al.128 test conversion in smokers compared with 10.3% in nonsmokers. An interesting finding of this study was that the duration of smoking was more important than the number of cigarettes smoked daily. Table 2 summarizes the results of these studies. A large case-control study in India examined smoking and tuberculosis in men between 35 and 69 years of age.128 The tuberculosis prevalence risk ratio was 2.9 (95% CI, 2.63.3) for ever-smokers compared with never-smokers, and the prevalence was higher with a higher level of cigarette consumption (Table 2). The mortality from tuberculosis among men 25 to 69 years of age, based on 4072 tuberculosis deaths, showed a risk ratio of 4.5 (95% CI, 4.0-5.0) and 4.2 (95% CI, 3.7-4.8) for urban and rural residents, respectively. The authors found that the smokingattributable fraction of deaths from tuberculosis was 61%, greater than the fractionofsmoking-attributabledeaths from vascular disease or cancer. In a study among children living with a patient with active pulmonary tuberculosis, passive smoking was a strong risk factor for the (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2213 development of active tuberculosis (OR, 5.39; 95% CI, 2.44-11.91). Passive smoke exposure was confirmed by measurement of urinary cotinine levels, which were higher in children who developed the disease.129 The biological basis by which tobacco smoking increases tuberculosis risk may be through a decrease in immune response, mechanical disruption of cilia function, defects in macrophage immune responses, and/or CD4+ lymphopenia, increasing the susceptibility to pulmonary tuberculosis.130,131 Of historical interest is the relationship between tuberculosis and the rise of cigarette smoking in the early 20th century. Before that time, chewing tobacco was the preferred type of tobacco. Public fears that users of chewing tobacco who spit in public places might be spreading tuberculosis is one of the factors that led to the increase in cigarette sales in the United States. This is nicely described by Kluger132 as follows: “Chewing tobacco was no longer merely messy but socially disagreeable in more crowded urban America, and its inevitable by-product, spit- WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 Risk of TB ting, was now identified as a spreader of tuberculosis and other contagions and, thus, an official health menace. The leisurely pipe all at once seemed a remnant of a slower-temp age, and cigar fumes were newly offensive amid thronged city life. The cigarette, by contrast, could be quickly consumed and easily snuffed out on the job as well as to and from work.” SUMMARY AND IMPLICATIONS Cigarette smoking remains an enormous health problem and is the principal cause of several preventable diseases and much premature death. Generally, physicians think of cancer, atherosclerotic cardiovascular disease, and chronic obstructive pulmonary disease as the major health problems caused by smoking. Our review summarizes research on another significant adverse health effect due to active and passive smoking: the development of infections. Infectious diseases may rival cancer, heart disease, and chronic lung disease as sources of morbidity and mortality from smoking. We have reviewed the strength of the association between smoking and infections as measured by relative risk and the presence of a doseresponse effect. The possible mechanisms by which smoking increases the risk of infections include structural changes in the respiratory tract and a decrease in immune response, both systemically and locally within the lungs. Cigarette smoking is a substantial risk factor for important bacterial and viral infections. To highlight some of the more common and serious links between smoking and infection, smokers incur a 2- to 4-fold increased risk of invasive pneumococcal disease, a disease associated with high mortality. Influenza risk is severalfold higher and much more severe in smokers compared with nonsmokers. Perhaps the greatest public health impact of smoking on infection is the increased risk of tuberculosis. The highest rates of tuberculosis and associated mortality are among the poor and people in underdeveloped countries. The prevalence of smoking is high among the poor in developed countries and is increasing rapidly in underdeveloped countries. Thus, it is likely that smoking contributes substantially to the worldwide disease burden of tuberculosis. The findings of our review further emphasize the potential health benefits of smoking cessation and have specific clinical implications: 1. Smoking cessation should be part of the therapeutic plan for people with any serious infectious disease, periodontitis, or positive results of tuberculin skin tests. 2. Secondhand smoke exposure should be controlled in children to reduce the risks of meningococcal disease and otitis media and in adults to reduce the risks of influenza and meningococcal disease. 3. We have 3 recommendations for prevention of specific diseases: • Pneumococcal and influenza vaccine in all smokers • Acyclovir treatment for varicella in smokers • Yearly Papanicolaou smears in women who smoke. Accepted for Publication: November 28, 2003. Correspondence: Neal L. Benowitz, MD, Division of Clinical Pharmacology and Experimental Therapeutics, University of California, San Francisco, Box 1220, San Francisco, CA 94143-1220 (nbeno@itsa .ucsf.edu). Funding/Support: This study was supported in part by Public Health Service grants DA02277 and DA12393 from the National Institutes of Health, Bethesda, Md, and the Flight Attendants’ Medical Research Institute, Miami, Fla. Acknowledgment: We thank Joel Ernst, MD, for his critical review of the manuscript and Kaye Welch for editorial assistance. REFERENCES 1. Dye JA, Adler KB. Effects of cigarette smoke on epithelial cells of the respiratory tract. Thorax. 1994;49:825-834. 2. Marcy TW, Merrill WW. Cigarette smoking and respiratory tract infection. Clin Chest Med. 1987; 8:381-391. 3. Richardson MA. Upper airway complications of cigarette smoking. J Allergy Clin Immunol. 1988; 81:1032-1035. (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2214 4. Sopori ML, Goud NS, Kaplan AM. Effect of tobacco smoke on the immune system. In: Dean JH, Luster AE, Kimer M, eds. Immunotoxicology and Immunopharmacology. New York, NY: Raven Press; 1994:413-432. 5. Sopori ML, Kozak W, Savage SM, et al. Effect of nicotine on the immune system: possible regulation of immune responses by central and peripheral mechanisms. Psychoneuroendocrinology. 1998;23:189-204. 6. Tollerud DJ, Clark JW, Brown LM, et al. The effects of cigarette smoking on T cell subsets: a population-based survey of healthy caucasians. Am Rev Respir Dis. 1989;139:1446-1451. 7. Yeung MC, Buncio AD. Leukocyte count, smoking, and lung function. Am J Med. 1984;76: 31-37. 8. Corre F, Lellouch J, Schwartz D. Smoking and leucocyte-counts: results of an epidemiological survey. Lancet. 1971;2:632-634. 9. Friedman GD, Siegelaub AB, Seltzer CC, Feldman R, Collen MF. Smoking habits and the leukocyte count. Arch Environ Health. 1973; 26:137-143. 10. Mili F, Flanders WD, Boring JR, Annest JL, Destefano F. The associations of race, cigarette smoking, and smoking cessation to measures of the immune system in middle-aged men. Clin Immunol Immunopathol. 1991;59:187-200. 11. Taylor RG, Woodman G, Clarke SW. Plasma nicotine concentration and the white blood cell count in smokers. Thorax. 1986;41:407-408. 12. van Eeden SF, Hogg JC. The response of human bone marrow to chronic cigarette smoking. Eur Respir J. 2000;15:915-921. 13. Vanuxem D, Sampol J, Weiller PJ. M’Barki M, Grimaud C. Influence of chronic smoking on leukocytes [in French]. Respiration. 1984;46: 258-264. 14. Tell GS, Grimm RH Jr, Vellar OD, Theodorsen L. The relationship of white cell count, platelet count, and hematocrit to cigarette smoking in adolescents: the Oslo Youth Study. Circulation. 1985; 72:971-974. 15. Hughes DA, Haslam PL, Townsend PJ, TurnerWarwick M. Numerical and functional alterations in circulatory lymphocytes in cigarette smokers. Clin Exp Immunol. 1985;61:459-466. 16. Ginns LC, Goldenheim PD, Miller LG, et al. Tlymphocyte subsets in smoking and lung cancer: analysis of monoclonal antibodies and flow cytometry. Am Rev Respir Dis. 1982;126: 265-269. 17. Miller LG, Goldstein G, Murphy M, Ginns LC. Reversible alterations in immunoregulatory T cells in smoking: analysis by monoclonal antibodies and flow cytometry. Chest. 1982;82:526529. 18. Hersey P, Prendergast D, Edwards A. Effects of cigarette smoking on the immune system: follow-up studies in normal subjects after cessation of smoking. Med J Aust. 1983;2:425-429. 19. Costabel U, Bross KJ, Reuter C, Ruhle KH, Matthys H. Alterations in immunoregulatory Tcell subsets in cigarette smokers: a phenotypic analysis of bronchoalveolar and blood lymphocytes. Chest. 1986;90:39-44. 20. Reinherz EL, Rubinstein A, Geha RS, Strelkauskas AJ, Rosen FS, Schlossman SF. Abnormalities of immunoregulatory T cells in disorders of immune function. N Engl J Med. 1979;301:1018-1022. 21. Leatherman JW, Michael AF, Schwartz BA, Hoidal JR. Lung T cells in hypersensitivity pneumonitis. Ann Intern Med. 1984;100:390392. WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 22. Wewers MD, Diaz PT, Wewers ME, Lowe MP, Nagaraja HN, Clanton TL. Cigarette smoking in HIV infection induces a suppressive inflammatory environment in the lung. Am J Respir Crit Care Med. 1998;158:1543-1549. 23. Fisher GL, McNeill KL, Finch GL, Wilson FD, Golde DW. Functional evaluation of lung macrophages from cigarette smokers and nonsmokers. J Reticuloendothel Soc. 1982;32:311-321. 24. Noble RC, Penny BB. Comparison of leukocyte count and function in smoking and nonsmoking young men. Infect Immun. 1975;12:550-555. 25. Corberand J, Nguyen F, Do AH, et al. Effect of tobacco smoking on the functions of polymorphonuclear leukocytes. Infect Immun. 1979; 23:577-581. 26. Eichel B, Shahrik HA. Tobacco smoke toxicity: loss of human oral leukocyte function and fluidcell metabolism. Science. 1969;166:14241428. 27. Bridges RB, Kraal JH, Huang LJ, Chancellor BM. Effects of tobacco smoke on chemotaxis and glucose metabolism of polymorphonuclear leukocytes. Infect Immun. 1977;15:115-123. 28. Bridges RB, Hsieh L. Effects of cigarette smoke fractions on the chemotaxis of polymorphonuclear leukocytes. J Leukoc Biol. 1986;40:73-85. 29. Sasagawa S, Suzuki K, Sakatani T, Fujikura T. Effects of nicotine on the functions of human polymorphonuclear leukocytes in vitro. J Leukoc Biol. 1985;37:493-502. 30. Holt PG. Immune and inflammatory function in cigarette smokers. Thorax. 1987;42:241-249. 31. McCrea KA, Ensor JE, Nall K, Bleecker ER, Hasday JD. Altered cytokine regulation in the lungs of cigarette smokers. Am J Respir Crit Care Med. 1994;150:696-703. 32. Twigg HL III, Soliman DM, Spain BA. Impaired alveolar macrophage accessory cell function and reduced incidence of lymphocytic alveolitis in HIV-infected patients who smoke. AIDS. 1994; 8:611-618. 33. Ouyang Y, Virasch N, Hao P, et al. Suppression of human IL-1, IL-2, IFN-␥, and TNF-alpha production by cigarette smoke extracts. J Allergy Clin Immunol. 2000;106:280-287. 34. Hagiwara E, Takahashi KI, Okubo T, et al. Cigarette smoking depletes cells spontaneously secreting Th(1) cytokines in the human airway. Cytokine. 2001;14:121-126. 35. Madretsma S, Wolters LM, van Dijk JP, et al. Invivo effect of nicotine on cytokine production by human non-adherent mononuclear cells. Eur J Gastroenterol Hepatol. 1996;8:1017-1020. 36. Matsunaga K, Klein TW, Friedman H, Yamamoto Y. Involvement of nicotinic acetylcholine receptors in suppression of antimicrobial activity and cytokine responses of alveolar macrophages to Legionella pneumophila infection by nicotine. J Immunol. 2001;167: 6518-6524. 37. Smith KA. Interleukin-2: inception, impact, and implications. Science. 1988;240:1169-1176. 38. Luster MI, Simeonova PP, Gallucci R, Matheson J. Tumor necrosis factor ␣ and toxicology. Crit Rev Toxicol. 1999;29:491-511. 39. Ferson M, Edwards A, Lind A, Milton GW, Hersey P. Low natural killer–cell activity and immunoglobulin levels associated with smoking in human subjects. Int J Cancer. 1979;23:603609. 40. Nair MP, Kronfol ZA, Schwartz SA. Effects of alcohol and nicotine on cytotoxic functions of human lymphocytes. Clin Immunol Immunopathol. 1990;54:395-409. 41. Tollerud DJ, Clark JW, Brown LM, et al. Association of cigarette smoking with decreased numbers of circulating natural killer cells. Am Rev Respir Dis. 1989;139:194-198. 42. Silverman NA, Potvin C, Alexander JC Jr, Chretien PB. In vitro lymphocyte reactivity and Tcell levels in chronic cigarette smokers. Clin Exp Immunol. 1975;22:285-292. 43. Herberman RB, Holden HT. Natural cell– mediated immunity. Adv Cancer Res. 1978; 27:305-377. 44. Herberman RB. Natural Cell–Mediated Immunity Against Tumors. New York, NY: Academic Press; 1980. 45. Geng Y, Savage SM, Johnson LJ, Seagrave J, Sopori ML. Effects of nicotine on the immune response, I: chronic exposure to nicotine impairs antigen receptor–mediated signal transduction in lymphocytes. Toxicol Appl Pharmacol. 1995;135:268-278. 46. Geng Y, Savage SM, Razani-Boroujerdi S, Sopori ML. Effects of nicotine on the immune response, II: chronic nicotine treatment induces T cell anergy. J Immunol. 1996;156:2384-2390. 47. Kalra R, Singh SP, Savage SM, Finch GL, Sopori ML. Effects of cigarette smoke on immune response: chronic exposure to cigarette smoke impairs antigen-mediated signaling in T cells and depletes IP3-sensitive Ca(2+) stores. J Pharmacol Exp Ther. 2000;293:166-171. 48. Dales LG, Friedman GD, Siegelaub AB, Selzer CC. Cigarette smoking and serum chemistry tests. J Chronic Dis. 1974;27:293-307. 49. Gulsvik A, Fagerhoi MK. Smoking and immunoglobulin levels [letter]. Lancet. 1979;1:449. 50. Gerrard JW, Heiner DC, Ko CG, Mink J, Meyers A, Dosman JA. Immunoglobulin levels in smokers and non-smokers. Ann Allergy. 1980; 44:261-262. 51. Andersen P, Pedersen OF, Bach B, Bonde GJ. Serum antibodies and immunoglobulins in smokers and nonsmokers. Clin Exp Immunol. 1982; 47:467-473. 52. Onari K, Seyama A, Inamizu T, et al. Immunological study on cigarette smokers, part I: serum protein pattern in smokers. Hiroshima J Med Sci. 1978;27:113-118. 53. Warr GA, Martin RR, Sharp PM, Rossen RD. Normal human bronchial immunoglobulins and proteins: effects of cigarette smoking. Am Rev Respir Dis. 1977;116:25-30. 54. Reynolds HY. Immunoglobulin G and its function in the human respiratory tract. Mayo Clin Proc. 1988;63:161-174. 55. Finklea JF, Hasselblad V, Riggan WB, Nelson WC, Hammer DI, Newill VA. Cigarette smoking and hemagglutination inhibition response to influenza after natural disease and immunization. Am Rev Respir Dis. 1971;104:368-376. 56. Gruchow HW, Hoffmann RG, Marx JJ Jr, Emanuel DA, Rimm AA. Precipitating antibodies to farmer’s lung antigens in a Wisconsin farming population. Am Rev Respir Dis. 1981;124:411-415. 57. Pastor P, Medley F, Murphy TV. Invasive pneumococcal disease in Dallas County, Texas: results from population-based surveillance in 1995. Clin Infect Dis. 1998;26:590-595. 58. Nuorti JP, Butler JC, Farley MM, et al; Active Bacterial Core Surveillance Team. Cigarette smoking and invasive pneumococcal disease. N Engl J Med. 2000;342:681-689. 59. Almirall J, Gonzalez CA, Balanzo X, Bolibar I. Proportion of community-acquired pneumonia cases attributable to tobacco smoking. Chest. 1999; 116:375-379. (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2215 60. Raman AS, Swinburne AJ, Fedullo AJ. Pneumococcal adherence to the buccal epithelial cells of cigarette smokers. Chest. 1983;83:23-27. 61. Doebbeling BN, Wenzel RP. The epidemiology of Legionella pneumophila infections. Semin Respir Infect. 1987;2:206-221. 62. Straus WL, Plouffe JF, File TM Jr, et al; Ohio Legionnaires Disease Group. Risk factors for domestic acquisition of legionnaires disease. Arch Intern Med. 1996;156:1685-1692. 63. Fischer M, Hedberg K, Cardosi P, et al. Tobacco smoke as a risk factor for meningococcal disease. Pediatr Infect Dis J. 1997;16:979-983. 64. Imrey PB, Jackson LA, Ludwinski PH, et al. Outbreak of serogroup C meningococcal disease associated with campus bar patronage. Am J Epidemiol. 1996;143:624-630. 65. Stuart JM, Cartwright KA, Robinson PM, Noah ND. Effect of smoking on meningococcal carriage. Lancet. 1989;2:723-725. 66. Caugant DA, Hoiby EA, Magnus P, et al. Asymptomatic carriage of Neisseria meningitidis in a randomly sampled population. J Clin Microbiol. 1994;32:323-330. 67. Blackwell CC, Tzanakaki G, Kremastinou J, et al. Factors affecting carriage of Neisseria meningitidis among Greek military recruits. Epidemiol Infect. 1992;108:441-448. 68. Haneberg B, Tonjum T, Rodahl K, Gedde-Dahl TW. Factors preceding the onset of meningococcal disease, with special emphasis on passive smoking, symptoms of ill health. NIPH Ann. 1983;6:169-173. 69. Tappero JW, Reporter R, Wenger JD, et al. Meningococcal disease in Los Angeles County, California, and among men in the county jails. N Engl J Med. 1996;335:833-840. 70. Kitchens GG. Relationship of environmental tobacco smoke to otitis media in young children. Laryngoscope. 1995;105:1-13. 71. Ilicali OC, Keles N, Deger K, Savas I. Relationship of passive cigarette smoking to otitis media. Arch Otolaryngol Head Neck Surg. 1999;125: 758-762. 72. Stathis SL, O’Callaghan DM, Williams GM, Najman JM, Andersen MJ, Bor W. Maternal cigarette smoking during pregnancy is an independent predictor for symptoms of middle ear disease at five years’ postdelivery [serial online]. Pediatrics. 1999;104:e16. 73. Barbour SE, Nakashima K, Zhang JB, et al. Tobacco and smoking: environmental factors that modify the host response (immune system) and have an impact on periodontal health. Crit Rev Oral Biol Med. 1997;8:437-460. 74. Arbes SJ Jr, Agustsdottir H, Slade GD. Environmental tobacco smoke and periodontal disease in the United States. Am J Public Health. 2001; 91:253-257. 75. Tomar SL, Asma S. Smoking-attributable periodontitis in the United States: findings from NHANES III: National Health and Nutrition Examination Survey. J Periodontol. 2000;71: 743-751. 76. Muller HP. Smoking and periodontal health [in German]. Gesundheitswesen. 2000;62:400408. 77. Genco RJ. Current view of risk factors for periodontal diseases. J Periodontol. 1996;67: 1041-1049. 78. van der Weijden GA, de Slegte C, Timmerman MF, van der Velden U. Periodontitis in smokers andnon-smokers:intra-oraldistributionofpockets. J Clin Periodontol. 2001;28:955-960. 79. Haffajee AD, Socransky SS. Relationship of ciga- WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022 80. 81. 82. 83. 84. 85. 86. 87. 88. 89. 90. 91. 92. 93. 94. 95. 96. 97. rette smoking to the subgingival microbiota. J Clin Periodontol. 2001;28:377-388. Shiloah J, Patters MR, Waring MB. The prevalence of pathogenic periodontal microflora in healthy young adult smokers. J Periodontol. 2000;71:562-567. Anda RF, Williamson DF, Escobedo LG, Remington PL. Smoking and the risk of peptic ulcer disease among women in the United States. Arch Intern Med. 1990;150:1437-1441. Kato I, Nomura AM, Stemmermann GN, Chyou PH. A prospective study of gastric and duodenal ulcer and its relation to smoking, alcohol, and diet. Am J Epidemiol. 1992;135:521-530. Sontag S, Graham DY, Belsito A, et al. Cimetidine, cigarette smoking, and recurrence of duodenal ulcer. N Engl J Med. 1984;311:689-693. Korman MG, Hansky J, Eaves ER, Schmidt GT. Influence of cigarette smoking on healing and relapse in duodenal ulcer disease. Gastroenterology. 1983; 85:871-874. Endoh K, Leung FW. Effects of smoking and nicotine on the gastric mucosa: a review of clinical and experimental evidence. Gastroenterology. 1994;107:864-878. Moshkowitz M, Brill S, Konikoff FM, Averbuch M, Arber N, Halpern Z. Additive deleterious effect of smoking on gastroduodenal pathology and clinical course in Helicobacter pylori–positive dyspeptic patients. Isr Med Assoc J. 2000;2: 892-895. Bateson MC. Cigarette smoking and Helicobacter pylori infection. Postgrad Med J. 1993; 69:41-44. Martin DF, Montgomery E, Dobek AS, Patrissi GA, Peura DA. Campylobacter pylori, NSAIDS, and smoking: risk factors for peptic ulcer disease. Am J Gastroenterol. 1989;84:1268-1272. Nakamura M, Haruma K, Kamada T, et al. Cigarette smoking promotes atrophic gastritis in Helicobacter pylori–positive subjects. Dig Dis Sci. 2002;47:675-681. Cover TL, Vaughn SG, Cao P, Blaser MJ. Potentiation of Helicobacter pylori vacuolating toxin activity by nicotine and other weak bases. J Infect Dis. 1992;166:1073-1078. O’Connor HJ, Kanduru C, Bhutta AS, Meehan JM, Feeley KM, Cunnane K. Effect of Helicobacter pylori eradication on peptic ulcer healing. Postgrad Med J. 1995;71:90-93. Borody TJ, George LL, Brandl S, Andrews P, Jankiewicz E, Ostapowicz N. Smoking does not contribute to duodenal ulcer relapse after Helicobacter pylori eradication. Am J Gastroenterol. 1992;87:1390-1393. Blake GH, Abell TD, Stanley WG. Cigarette smoking and upper respiratory infection among recruits in basic combat training. Ann Intern Med. 1988;109:198-202. Cohen S, Tyrrell DA, Russell MA, Jarvis MJ, Smith AP. Smoking, alcohol consumption, and susceptibility to the common cold. Am J Public Health. 1993;83:1277-1283. Vitalis TZ, Keicho N, Itabashi S, Hayashi S, Hogg JC. A model of latent adenovirus 5 infection in the guinea pig (Cavia porcellus). Am J Respir Cell Mol Biol. 1996;14:225-231. Hogg JC. Latent adenoviral infection in the pathogenesis of emphysema: the Parker B. Francis Lectureship. Chest. 2000;117(5, suppl 1): 282S285S. Finklea JF, Sandifer SH, Smith DD. Cigarette smoking and epidemic influenza. Am J Epidemiol. 1969;90:390-399. 98. Kark JD, Lebiush M. Smoking and epidemic influenza-like illness in female military recruits: a brief survey. Am J Public Health. 1981;71: 530-532. 99. Kark JD, Lebiush M, Rannon L. Cigarette smoking as a risk factor for epidemic A(H1N1) influenza in young men. N Engl J Med. 1982;307: 1042-1046. 100. Hament JM, Kimpen JL, Fleer A, Wolfs TF. Respiratory viral infection predisposing for bacterial disease: a concise review. FEMS Immunol Med Microbiol. 1999;26:189-195. 101. Miyaura S, Eguchi H, Johnston JM. Effect of a cigarette smoke extract on the metabolism of the proinflammatory autacoid, platelet-activating factor. Circ Res. 1992;70:341-347. 102. Ichimaru T, Tai HH. Alteration of platelet activating factor (PAF) metabolism in rat pulmonary alveolar macrophages and plasma by cigarette smoking. Prostaglandins Leukot Essent Fatty Acids. 1992;47:123-128. 103. Cruijff M, Thijs C, Govaert T, Aretz K, Dinant GJ, Knottnerus A. The effect of smoking on influenza, influenza vaccination efficacy and on the antibody response to influenza vaccination. Vaccine. 1999;17:426-432. 104. Ellis ME, Neal KR, Webb AK. Is smoking a risk factor for pneumonia in adults with chickenpox? BMJ (Clin Res Ed). 1987;294:1002. 105. Grayson ML, Newton-John H. Smoking and varicella pneumonia [letter]. J Infect. 1988;16: 312. 106. Sedlacek TV. Advances in the diagnosis and treatment of human papillomavirus infections. Clin Obstet Gynecol. 1999;42:206-220. 107. Schneider A, Kirchhoff T, Meinhardt G, Gissmann L. Repeated evaluation of human papillomavirus 16 status in cervical swabs of young women with a history of normal Papanicolaou smears. Obstet Gynecol. 1992;79:683-688. 108. Moscicki AB, Shiboski S, Broering J, et al. The natural history of human papillomavirus infection as measured by repeated DNA testing in adolescent and young women. J Pediatr. 1998; 132:277-284. 109. Kataja V, Syrjanen S, Yliskoski M, et al. Risk factors associated with cervical human papillomavirus infections: a case-control study. Am J Epidemiol. 1993;138:735-745. 110. Hellberg D, Nilsson S, Haley NJ, Hoffman D, Wynder E. Smoking and cervical intraepithelial neoplasia: nicotine and cotinine in serum and cervical mucus in smokers and nonsmokers. Am J Obstet Gynecol. 1988;158:910-913. 111. Arany I, Tyring SK. Status of local cellular immunity in interferon-responsive and -nonresponsive human papillomavirus-associated lesions. Sex Transm Dis. 1996;23:475-480. 112. Winkelstein W Jr. Smoking and cervical cancer— current status: a review. Am J Epidemiol. 1990; 131:945-960. 113. Newell GR, Mansell PW, Wilson MB, Lynch HK, Spitz MR, Hersh EM. Risk factor analysis among men referred for possible acquired immune deficiency syndrome. Prev Med. 1985;14:8191. 114. Royce RA, Winkelstein W Jr. HIV infection, cigarette smoking and CD4+ T-lymphocyte counts: preliminary results from the San Francisco Men’s Health Study. AIDS. 1990;4:327-333. 115. Boulos R, Halsey NA, Holt E, et al; Cite Soleil/ JHU AIDS Project Team. HIV-1 in Haitian women 1982-1988. J Acquir Immune Defic Syndr. 1990; 3:721-728. (REPRINTED) ARCH INTERN MED/ VOL 164, NOV 8, 2004 2216 116. Burns DN, Kramer A, Yellin F, et al. Cigarette smoking: a modifier of human immunodeficiency virus type 1 infection? J Acquir Immune Defic Syndr. 1991;4:76-83. 117. Craib KJ, Schechter MT, Montaner JS, et al. The effect of cigarette smoking on lymphocyte subsets and progression to AIDS in a cohort of homosexual men. Clin Invest Med. 1992;15: 301-308. 118. Sasson IM, Haley NJ, Hoffmann D, Wynder EL, Hellberg D, Nilsson S. Cigarette smoking and neoplasia of the uterine cervix: smoke constituents in cervical mucus. N Engl J Med. 1985;312: 315-316. 119. Winkelstein W Jr. Smoking and cervical cancer: current status. Am J Epidemiol. 1990; 131:945-957. 120. Hirschtick RE, Glassroth J, Jordan MC, et al; Pulmonary Complications of HIV Infection Study Group. Bacterial pneumonia in persons infected with the human immunodeficiency virus. N Engl J Med. 1995;333:845-851. 121. Park LP, Margolick JB, Giorgi JV, et al. Influence of HIV-1 infection and cigarette smoking on leukocyte profiles in homosexual men: the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 1992;5:1124-1130. 122. Conley LJ, Bush TJ, Buchbinder SP, Penley KA, Judson FN, Holmberg SD. The association between cigarette smoking and selected HIVrelated medical conditions. AIDS. 1996;10: 1121-1126. 123. Yu GP, Hsieh CC, Peng J. Risk factors associated with the prevalence of pulmonary tuberculosis among sanitary workers in Shanghai. Tubercle. 1988;69:105-112. 124. Buskin SE, Gale JL, Weiss NS, Nolan CM. Tuberculosis risk factors in adults in King County, Washington, 1988 through 1990. Am J Public Health. 1994;84:1750-1756. 125. Alcaide J, Altet MN, Plans P, et al. Cigarette smoking as a risk factor for tuberculosis in young adults: a case-control study. Tuber Lung Dis. 1996;77:112-116. 126. McCurdy SA, Arretz DS, Bates RO. Tuberculin reactivity among California Hispanic migrant farm workers. Am J Ind Med. 1997;32:600-605. 127. Anderson RH, Sy FS, Thompson S, Addy C. Cigarette smoking and tuberculin skin test conversion among incarcerated adults. Am J Prev Med. 1997;13:175-181. 128. Gajalakshmi V, Peto R, Kanaka TS, Jha P. Smoking and mortality from tuberculosis and other diseases in India: retrospective study of 43 000 adult male deaths and 35 000 controls. Lancet. 2003; 362:507-515. 129. Altet MN, Alcaide J, Plans P, et al. Passive smoking and risk of pulmonary tuberculosis in children immediately following infection: a case-control study. Tuber Lung Dis. 1996; 77:537-544. 130. Rich EA, Ellner JJ. Pathogenesis of tuberculosis. In: Friedman LN, ed. Tuberculosis: Current Concepts and Treatment. Boca Raton, Fla: CRC Press; 1994:27-31. 131. Onwubbalili JK, Edwards AJ, Palmer L. T4 lymphopenia in human tuberculosis. Tubercle. 1987; 68:195-200. 132. Kluger R. Ashes to Ashes: America’s HundredYear Cigarette War, the Public Health, and the Unabashed Triumph of Philip Morris. New York, NY: Alfred A Knopf; 1996:19. WWW.ARCHINTERNMED.COM ©2004 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 03/10/2022