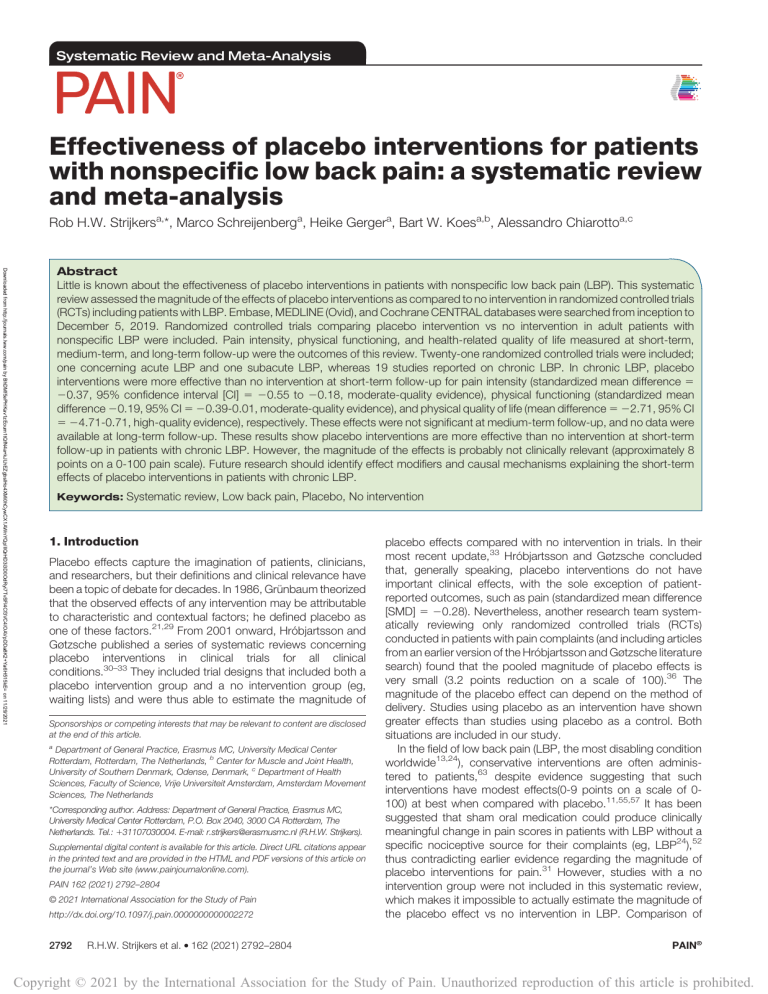
Systematic Review and Meta-Analysis Effectiveness of placebo interventions for patients with nonspecific low back pain: a systematic review and meta-analysis Rob H.W. Strijkersa,*, Marco Schreijenberga, Heike Gergera, Bart W. Koesa,b, Alessandro Chiarottoa,c Downloaded from http://journals.lww.com/pain by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8K2+Ya6H515kE= on 11/29/2021 Abstract Little is known about the effectiveness of placebo interventions in patients with nonspecific low back pain (LBP). This systematic review assessed the magnitude of the effects of placebo interventions as compared to no intervention in randomized controlled trials (RCTs) including patients with LBP. Embase, MEDLINE (Ovid), and Cochrane CENTRAL databases were searched from inception to December 5, 2019. Randomized controlled trials comparing placebo intervention vs no intervention in adult patients with nonspecific LBP were included. Pain intensity, physical functioning, and health-related quality of life measured at short-term, medium-term, and long-term follow-up were the outcomes of this review. Twenty-one randomized controlled trials were included; one concerning acute LBP and one subacute LBP, whereas 19 studies reported on chronic LBP. In chronic LBP, placebo interventions were more effective than no intervention at short-term follow-up for pain intensity (standardized mean difference 5 20.37, 95% confidence interval [CI] 5 20.55 to 20.18, moderate-quality evidence), physical functioning (standardized mean difference 20.19, 95% CI 5 20.39-0.01, moderate-quality evidence), and physical quality of life (mean difference 5 22.71, 95% CI 5 24.71-0.71, high-quality evidence), respectively. These effects were not significant at medium-term follow-up, and no data were available at long-term follow-up. These results show placebo interventions are more effective than no intervention at short-term follow-up in patients with chronic LBP. However, the magnitude of the effects is probably not clinically relevant (approximately 8 points on a 0-100 pain scale). Future research should identify effect modifiers and causal mechanisms explaining the short-term effects of placebo interventions in patients with chronic LBP. Keywords: Systematic review, Low back pain, Placebo, No intervention 1. Introduction Placebo effects capture the imagination of patients, clinicians, and researchers, but their definitions and clinical relevance have been a topic of debate for decades. In 1986, Grünbaum theorized that the observed effects of any intervention may be attributable to characteristic and contextual factors; he defined placebo as one of these factors.21,29 From 2001 onward, Hróbjartsson and Gøtzsche published a series of systematic reviews concerning placebo interventions in clinical trials for all clinical conditions.30–33 They included trial designs that included both a placebo intervention group and a no intervention group (eg, waiting lists) and were thus able to estimate the magnitude of Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article. a Department of General Practice, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, b Center for Muscle and Joint Health, University of Southern Denmark, Odense, Denmark, c Department of Health Sciences, Faculty of Science, Vrije Universiteit Amsterdam, Amsterdam Movement Sciences, The Netherlands *Corresponding author. Address: Department of General Practice, Erasmus MC, University Medical Center Rotterdam, P.O. Box 2040, 3000 CA Rotterdam, The Netherlands. Tel.: 131107030004. E-mail: r.strijkers@erasmusmc.nl (R.H.W. Strijkers). Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.painjournalonline.com). PAIN 162 (2021) 2792–2804 © 2021 International Association for the Study of Pain http://dx.doi.org/10.1097/j.pain.0000000000002272 2792 · R.H.W. Strijkers et al. 162 (2021) 2792–2804 placebo effects compared with no intervention in trials. In their most recent update,33 Hróbjartsson and Gøtzsche concluded that, generally speaking, placebo interventions do not have important clinical effects, with the sole exception of patientreported outcomes, such as pain (standardized mean difference [SMD] 5 20.28). Nevertheless, another research team systematically reviewing only randomized controlled trials (RCTs) conducted in patients with pain complaints (and including articles from an earlier version of the Hróbjartsson and Gøtzsche literature search) found that the pooled magnitude of placebo effects is very small (3.2 points reduction on a scale of 100).36 The magnitude of the placebo effect can depend on the method of delivery. Studies using placebo as an intervention have shown greater effects than studies using placebo as a control. Both situations are included in our study. In the field of low back pain (LBP, the most disabling condition worldwide13,24), conservative interventions are often administered to patients,63 despite evidence suggesting that such interventions have modest effects(0-9 points on a scale of 0100) at best when compared with placebo.11,55,57 It has been suggested that sham oral medication could produce clinically meaningful change in pain scores in patients with LBP without a specific nociceptive source for their complaints (eg, LBP24),52 thus contradicting earlier evidence regarding the magnitude of placebo interventions for pain.31 However, studies with a no intervention group were not included in this systematic review, which makes it impossible to actually estimate the magnitude of the placebo effect vs no intervention in LBP. Comparison of PAIN® Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. December 2021 · Volume 162 · Number 12 placebo intervention vs no intervention is important to correct for phenomena such as regression to the mean and natural history of the disease, which do not represent true placebo effects. Thus, the current knowledge about actual magnitude of placebo effects in LBP is still limited. As the literature search of Hróbjartsson and Gøtzsche is now over 10 years old and because uncertainty remains about the effectiveness of placebo interventions for LBP, it is time to gain further insight into the magnitude of placebo effects in the LBP field. The main objective of this systematic review is to assess the magnitude of effects of placebo interventions in comparison with no intervention for patients with LBP. www.painjournalonline.com 2793 2.3. Outcomes of interest Pain intensity, physical functioning, and health-related quality of life (HRQoL; ie, core outcome domains for LBP8) measured at short-term (up to 3 months), medium-term (4-12 months), and long-term (1 or 2 years) follow-up were the primary outcomes of this review. If an RCT did not include at least one of these outcomes, the article was excluded. In case of multiple shortterm outcomes, the outcome closest to 1-month follow-up was used for the primary analysis. 2.4. Selection of studies The study protocol for this systematic review was written a priori and was registered on February 4, 2019 (PROSPERO Registration number CRD42019127465). The guidance of the Cochrane Back and Neck Review Group was followed for the methods.19 The PRISMA statement was adopted for the reporting of this systematic review.44 Two reviewers (M.S. and A.C.) independently screened titles and abstracts of the articles found in the literature search to decide which articles to retrieve in full text. The same 2 reviewers read the full-text articles to include all relevant studies according to the selection criteria, as mentioned above. A consensus meeting was held to discuss studies about which there was disagreement between the reviewers. In case of disagreement, a third independent reviewer (B.W.K.) made the final decision whether or not to include the study. 2.1. Databases and search strategy 2.5. Data extraction Embase, MEDLINE (Ovid), and Cochrane CENTRAL databases were searched from inception up to December 5, 2019. The search strategies for this systematic review were based on the strategy used in Hróbjartsson and Gøtzsche’s 2010 Cochrane review,33 with “low back pain” as an additional search key term. The new search strategy was developed in collaboration with an experienced information specialist. Elements of the search were “back pain,” “placebo,” and “randomized controlled trial” and corresponding synonyms (Appendix A, supplemental digital content available at http://links.lww.com/PAIN/B345). No language restrictions were adopted for the search. Furthermore, the references of all included studies of the most recent update of the Cochrane review by Hróbjartsson and Gøtzsche were searched manually for additional studies.33 Data extraction on outcomes was performed in duplicate by 2 reviewers (R.H.W.S. and H.G.), whereas data extraction on characteristics of included studies and their patients was performed by one reviewer (R.H.W.S.) and double checked by a second one (M.S.). Standardized extraction forms were used (Appendix B, supplemental digital content available at http://links.lww.com/PAIN/ B345). These characteristics included study design, sample size, baseline patients’ characteristics (eg, age, sex, pain duration, pain intensity, physical functioning, chronicity [acute: ,6 weeks, subacute: 6 , 12 weeks, and chronic .12 weeks]), interventions’ characteristics, follow-up time, primary outcomes, results for outcomes at all follow-ups (mean, SD, and sample size), and funding source. We performed the meta-analysis in RevMan (Review Manager v5.3, The Nordic Cochrane Centre, Copenhagen, DK). Whenever possible means and SDs were extracted directly from the article or derived from available values (medians, IQR, 95% confidence interval [CI], ranges, etc) using appropriate estimation formulas.61 We used GetData Graph Digitizer version 2.26.0.20 to retrieve data from article figures and graphs in case no written data were available. If articles reported change from baseline, the endpoint mean was calculated and SD of the baseline was used as suggested by the Cochrane Handbook v6, chapter 6.5.2.8. In case of multiple placebo groups (eg,enhanced and nonenhanced placebo interventions), the results of the placebo groups were combined by taking the weighted mean and SDs of the 2 groups.12 2. Methods 2.2. Eligibility criteria Inclusion criteria were as follows: (1) randomized controlled trials with a three-group design (active intervention group, placebo group, and no intervention groups) or at least a comparison of a placebo intervention vs no intervention (in a 2-group design); (2) studies recruiting adult patients (.18 years old) with nonspecific LBP; in trials with a mixed population (eg, LBP and neck pain patients), at least 75% of participants had LBP for the trial to be eligible; (3) the study has evaluated the effectiveness of a placebo intervention; and (4) the study is available as a full-text article. The authors have chosen to only include RCTs as they provide the least biased estimates on the effectiveness of interventions for clinical practice.64 Following Hróbjartsson and Gøtzsche,33 we defined a placebo intervention as any intervention labelled in the trial report as being a placebo or an analogous term, such as sham, fake, dummy, or nonspecific or unspecific treatment. Randomized controlled trials in which the placebo group and no treatment group received the same underlying treatment (eg, “usual care”) were included. Studies focusing on nocebo treatments or effects were excluded. 2.6. Risk of bias assessment Two reviewers (R.H.W.S. and M.S.) independently scored the risk of bias (RoB) of included studies using the revised Cochrane riskof-bias tool for randomized trials, version of August 22, 2019.28 This RoB tool consists of 23 items in 5 subdomains that can be answered with “yes,” “probably yes,” “probably no,” “no,” or “no information.” This results in a trial overall RoB judgement that may be “low,” “high,” or “some concerns.” A consensus meeting was held to discuss studies about which there was disagreement between the reviewers. In case a consensus was not reached, a third independent reviewer (A.C.) made the final decision concerning the risk of bias assessment. Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. 2794 · PAIN® R.H.W. Strijkers et al. 162 (2021) 2792–2804 2.7. Meta-analysis and interpretation of results Between-group MDs were calculated for continuous or ordinal outcomes measured with the same instruments; SMDs were estimated if different instruments were used to assess the same outcome (eg, Roland–Morris Disability Questionnaire and Oswestry Disability Index to measure physical functioning). Statistical pooling was performed if there was clinical (sufficiently homogeneous study population) and methodological homogeneity (comparison, outcome, and assessment time points) across trials. Random-effects models rather than a fixed-effects model was used on the assumption that the included studies differed to some extent with respect to clinical and other factors. To assess the presence of between-study heterogeneity of effect sizes, t2 was calculated to get an estimate of the variance between the effect sizes from individual studies.26 For the primary outcome a value of t2 5 0.04 was considered as low heterogeneity, 0.09 as moderate, and 0.16 as high heterogeneity.3 In addition, the I2 statistic was used which can be interpreted as the percentage of heterogeneity attributable to between-study variation rather than a random error.27 Meta-analyses were performed in Review Manager (RevMan) 5.3. If at least 10 studies were included in a meta-analysis, a funnel plot was created to explore whether there was asymmetry among the trial results (which may indicate publication bias). Separate analyses were conducted for patients with (sub)acute or chronic LBP, consistently with the method guideline for systematic reviews of the Cochrane Back and Neck Group.19 Subgroup analyses were also considered for different placebo interventions (eg, open-label placebo, placebo acupuncture, and placebo tape). A sensitivity analysis was conducted, excluding studies rated as having a high RoB. For all analyses, a 2-sided P , 0.05 was used to indicate statistical significance, ie, whether placebo interventions were more effective than no intervention. Based on recent studies estimating the smallest worthwhile effect for conservative interventions vs no intervention in patients with LBP,9,17 a 20% between-group difference was a priori established as a clinically relevant effect. 2.8. Evidence synthesis The Grading of Recommendations Assessment, Development, and Evaluation22 approach was subsequently used to rate the quality of evidence of pooled estimates into “high,” “moderate,” “low,” or “very low” as suggested by the Cochrane Back and Neck Group.19 For each specific outcome, evidence was downgraded one or more levels for each of the 5 Grading of Recommendations Assessment, Development, and Evaluation components that was met across all studies measuring that particular outcome: limitations, inconsistency, indirectness, imprecision, and publication bias. 19,22 The following rules were used for downgrading quality of evidence: (1) Limitations: one level if 50% to 75% of included trials scored “low or some concerns” on RoB and 2 levels if less than 50% of included trials scored “low or some concerns” on RoB. (2) Inconsistency: one level if the value for the I2 statistic was between 40% and 75%. (3) Indirectness: one level if a study did not specifically mention the target population (adult patients with nonspecific LBP) or if it was unclear whether the intervention could be indeed considered a placebo and whether the control was indeed a no intervention with respect to the placebo. (4) Imprecision: one level if the total sample for a specific outcome was ,100 patients and 2 levels if the total sample for a specific outcome was ,50 patients. (5) Publication bias: one level if the funnel plot indicates publication bias may be present. 3. Results 3.1. Characteristics and included studies The literature search revealed 7803 potentially relevant articles, and 21 RCTs were included in the review (Fig. 1). Of the 21 studies, one reported on subjects with acute LBP,58 one reported on subacute LBP,16 and the remaining 19 studies reported on patients with chronic LBP.2,4–7,14,35,37–43,45,46,50,54,62 Study characteristics of all 21 included RCTs are shown in Table 1. 3.2. Risk of bias analysis Three studies were identified as having an overall high risk of bias.14,41,54 All of the studies had a high risk of bias on measurement of the outcome, which is inherent to the study setup. The risk of bias analysis for each individual study is presented in Figure 2. 3.3. Primary endpoints 3.3.1. Chronic low back pain 3.3.1.1. Pain intensity There was moderate-quality evidence (19 RCTs, N 5 1443) that placebo interventions reduced back pain intensity compared with no intervention at short-term follow-up (SMD 20.37, 95% CI 20.55 to 20.18, P , 0.0001, t2 5 0.11) (refer to Figure 3). This between-group difference translates to approximately 8 points on a 0 to 100 pain scale, corresponding to approximately 14% major improvement in the placebo group, which did not reach the predefined 20% improvement for clinical relevance. Sensitivity analyses excluding RCTs with a high risk of bias showed a smaller but still statistically significant effect in favor of placebo interventions (SMD 20.27, 95% CI 20.47 to 20.06, P 5 0.0003). There was low-quality evidence (3 RCTs, N 5 154) that placebo interventions are not significantly better than no intervention for back pain reduction at medium-term follow-up (SMD 20.26, 95% CI 20.59-0.06, P 5 0.11 t2 5 0.00) (refer to Figure 3). Sensitivity analyses excluding high risk of bias studies confirmed this finding (SMD 20.19 95% CI 20.56 to 0.18, P 5 0.31). No long-term follow-up data were available. 3.3.1.2. Physical functioning There was moderate-quality evidence (11 RCTs, N 5 775) that placebo interventions improved physical functioning compared with no intervention at short-term follow-up (SMD 20.19, 95% CI 20.39 to 20.01, P 5 0.07 t2 5 0.06) (refer to Figure 4). This difference corresponds to approximately 1.3 points between-group difference on the 0 to 24 Roland–Morris Disability Questionnaire, which is not considered to be a clinically relevant effect. Sensitivity analysis excluding high risk of bias studies confirmed this finding (SMD 20.17 95% CI 20.32 to 20.02, P 5 0.03). Only one study reported on medium-term outcomes for physical functioning, showing no statistical difference between placebo intervention and no intervention (MD 22.60 95% CI 29.09 to 3.89 P 5 0.43 [scale 0-24]). No study reported on long-term outcomes. Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. December 2021 · Volume 162 · Number 12 www.painjournalonline.com 2795 Figure 1. PRISMA 2009 flow diagram. LBP, lower back pain. 3.3.1.3. Health-related quality of life There was high-quality evidence (3 RCTs, N 5 267) that placebo interventions improved quality of life on the physical component summary score of the SF-36 compared with no intervention on short-term follow-up (MD 2.71, 95% CI 0.71-4.71, P 5 0.008, t2 5 0.34 [scale 0-100]) (refer to Figure 5). There was high-quality evidence (3 RCTs, N 5 267) that placebo intervention does not improve quality of life on the mental component summary score of the SF-36 compared with no intervention on short-term follow-up (MD 20.49, 95% CI 23.49 to 2.51, P 5 0.75, t2 5 2.85 [scale 0100]) (refer to Figure 5). No study data were available for mediumterm or long-term follow-up. 3.3.2. (sub)Acute low back pain No meta-analysis for acute LBP was performed because of lack of studies on any of the primary endpoints. One study reported on physical functioning.58 There was no statistical difference between placebo intervention and no treatment (MD 7.0; 95% CI 20.13 to 14.13, P 5 0.05 [scale 0-24]). Another study reported on pain intensity in short-term follow-up.16 Short-term pain intensity was not different between placebo intervention and no treatment (MD 7.0; 95% CI 26.02 to 20.02; P 5 0.29 [scale 0-100]). 3.4. Subgroup analysis Subgroup analysis of open-label placebo RCTs as compared to placebo control intervention RCTs showed a similar effect on shortterm pain intensity (SMD 20.33 vs SMD 20.37, appendix C, supplemental digital content available at http://links.lww.com/PAIN/ B345, Fig. 1). There was high-quality evidence (3 RCTs, N 5 335) that placebo acupuncture intervention improved back pain intensity compared with no intervention at short-term follow-up (SMD 20.37, 95% CI 20.64 to 20.10, P 5 0.007). There was very low-quality evidence (2 RCTs, N 5 80) that placebo taping does not improve back pain compared with no intervention at short-term follow-up (SMD 0.09, 95% CI 20.52 to 0.70, P 5 0.77). There was high-quality evidence (2 RCTs, N 5 345) that placebo injection intervention does not improve back pain compared with no intervention at short-term follow-up (SMD 0.03, 95% CI 20.18 to 0.24, P 5 0.77). There was Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. 2796 First author, journal, Population total Percentage year of publication sample participants female (N) mean age in y (SD) participants Duration of complaints Placebo acute (<6 wk), intervention subacute (6-12 wk), or group chronic (>12 wk) Comparison control group No. of treatments. Total duration of treatment. Pain outcome Physical functioning Quality of life measures outcome measures outcome measures Follow-up available Placebo N 5 27 Age placebo: 33.22 (13.29) Control N 5 27 Age control: 29.85 (12.09) Placebo 63% Control 68% Chronic Placebo spinal manipulative therapy No intervention N56 2 wk NRS ODI NA 2 wk Borges et al.,4 2014 Placebo N 5 15 Age: 39.6 (9.6)* Control N 5 14 Age: 39.6 (9.6)* Placebo 73.3% Control 64.3% Chronic Sham laser therapy No intervention N 5 12 6 wk NRS NA NA 6 wk Brinkhaus et al.,5 2006 Placebo N 5 70 Age placebo: 58.2 (9.4) Control N 5 74 Age control: 58.9 (9.5) Placebo 75.3% Control 68.4% Chronic Sham acupuncture Waiting list N 5 12 8 wk VAS pain FFbH-R SF-36, MCS, and PCS 8 wk Carvalho et al.,6 2016 Placebo N 5 41 Placebo 70.7% Age placebo: 44.4 (13.2) Control 71.4% Control N 5 42 Age control: 44.1 (13.7) Chronic Open-label placebo pills Treatment as usual N 5 2dd2 3 wk NRS RMDQ NA 3 wk Celenay et al.,7 2019 Placebo N 5 21 Placebo 81% Median (range) Control 71% Age placebo: 48 (39-63) Control N 5 21 Median(Range) Age control: 55 (24-65) Chronic Sham massage therapy Standard treatment N 5 15 3 wk VAS pain ODI SF-36, MCS, and PCS 3 wk Eardley et al.,14 2013 Placebo N 5 21 Placebo 67% Age placebo: 48.1 (10.6) Control 64.7% Control N 5 17 Age control: 44.6 (10.3) Chronic Sham physiotherapy Waiting list N55 5 wk VAS pain RMDQ SF-36, MCS, and PCS 5 wk Farasyn et al.,16 2006 Placebo N 5 20 Age placebo: 43 (12) Control N 5 20 Age control: 40 (12) Sub-acute Sham endermology treatment Waiting list N51 30 min VAS pain ODI NA 1 wk Imamura et al.,35 2016 Placebo N 5 125 Placebo 70.4% Age placebo: 47.91 Control 63.78% (8.52) Control N 5 127 Age control: 48.01 (9.48 Chronic Sham infusion therapy Standard treatment N 5 3 3 wk VAS pain RMDQ NA 3 mo · Bialosky et al.,2 2014 R.H.W. Strijkers et al. 162 (2021) 2792–2804 Placebo 55% Control 56% (continued on next page) PAIN® Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. Table 1 Table 1Characteristics of eligible studies (n 5 21). Chronic Open-label placebo pills No. of treatments. Total duration of treatment. Pain outcome Physical functioning Quality of life measures outcome measures outcome measures Follow-up available Treatment as usual N 5 21 21 d NRS ODI NA 3 wk VAS pain ODI NA 4 wk Brief Pain Inventory subscore 1 NA NA 3 wk Kleine-Borgmann et al.,37 2019 Placebo N 5 67 Age placebo: 60.2 (15.15) Control N 5 60 Age control: 58.37 (13.97) Köroglu et al.,38 2017 Placebo N 5 20 Placebo 60% Age placebo: 50.3 (11.5) Control 40% Control N 5 20 Age control: 47.9 (15.2) Chronic Placebo taping Treatment as usual N 5 10 2 wk Placebo 58% Leichtfried et al.,39 Placebo N 5 36 2014 Median (range) Control 57% Age placebo: 47 (39-54) Control N 5 33 Median (range) Age control: 52.5 (49-58) Chronic Light intervention Prestudy therapy Placebo 55.6% Control 69.5% · NA Mixed, mostly Chronic Sham straincounterstrain exercise Laying in a sleeping N 5 1 position for 6 min 6 min VAS pain NA NA 1-3 d Licciardone et al.,41 2003 Placebo N 5 23 Age placebo: 52 (12) Control N 5 17 Age control: 49 (12) Placebo 57% Control 65% Chronic Sham manipulation therapy Received no intervention N57 5 mo VAS pain NA NA 1, 3 and 6 mo Luz Jr et al.,42 2015 Placebo N 5 20 Placebo 65% Age placebo: 50.1 (17.5) Control 85% Control N 5 20 Age control: 48.1 (13.4) Chronic Sham taping No intervention N51 48 h NRS RMDQ NA 1 wk Marchand et al.,43 1993 Placebo N 5 12 Placebo 50% Age placebo: 35.08 Control 50% (7.38) Control N 5 16 Age control: 37.25 (8.18) Chronic Sham tense therapy Waiting list N 5 20 10 wk VAS pain NA NA 3, 6 mo Chronic Sham acupuncture Standard therapy N 5 12 4 wk VAS pain NA NA 3 mo Placebo 45.90% Control 53.33% www.painjournalonline.com Placebo N 5 28 Age: 39.2 (11.1)* Control N 5 28 Age: 39.2 (11.1)* Number 12 N59 3 wk Lewis et al.,40 2010 Molsberger et al.,45 Placebo N 5 61 2002 Age placebo: 50 (6) Control N 5 60 Age control: 49 (7) Volume 162 Comparison control group · Duration of complaints Placebo acute (<6 wk), intervention subacute (6-12 wk), or group chronic (>12 wk) December 2021 (continued on next page) 2797 Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. Table 1 (continued) First author, journal, Population total Percentage year of publication sample participants female (N) mean age in y (SD) participants Placebo 75% Control 81% No. of treatments. Total duration of treatment. Pain outcome Physical functioning Quality of life measures outcome measures outcome measures Follow-up available Chronic Sham acupuncture No orientation, no intervention. N55 5 wk Brief Pain Inventory NA NA 2 wk Chronic Sham injection No treatment N 5 12 8 wk VAS pain FFbH-R SF-36, MCS, and PCS 2, 6 mo N52 8d NRS FFbH-R NA 8d · Placebo N 5 36 Age placebo: 51.03 (14.9) Control N 5 37 Age control: 46.19 (15.73) Comparison control group R.H.W. Strijkers et al. 162 (2021) 2792–2804 Moura et al.,46 2019 Duration of complaints Placebo intervention acute (<6 wk), subacute (6-12 wk), or group chronic (>12 wk) 2798 Placebo 56.3% Pach et al.,50 2011 Placebo N 5 43 Age placebo: 54.8 (11.3) Control 56.9% Control N 5 50 Age control: 56.7 (10.7) Schmitz et al.,54 2019 Placebo N 5 21 Placebo 76.19% Age placebo: 55.48 Control 57.14% (10.72) Control N 5 14 Age control: 48.07(8.49) Chronic Sham transdermal No treatment infusion Vas et al.,58 2012 Placebo N 5 69 Placebo 49.3% Age placebo: 43.6 (12.2) Control 64.3% Control N 5 70 Age control: 41.2 (12) Acute Sham acupuncture Treatment as usual N 5 5 2 wk VAS pain RMDQ NA 3 wk Wepner et al.,62 2008 Placebo N 5 18 Age: 47.06 (9.33)* Control N 5 18 Age: 47.06 (9.33)* Chronic Sham singing bowls therapy Treatment as usual N 5 6 4 wk VAS pain RMDQ SF-36, MCS, and PCS 5 wk NA * Not separately available. FFbH-r, Hannover Functional Ability Questionnaire; MCS, mental component summary; NRS, numerical rating scale; NA, not available; ODI, Oswestry Disability Index; PCS, physical component summary; RMDQ, Roland–Morris Disability Questionnaire; VAS, visual analog scale; SF-36, Short-Form 36. PAIN® Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. Table 1 (continued) First author, journal, Population total Percentage year of publication sample participants female (N) mean age in y (SD) participants December 2021 · Volume 162 · Number 12 www.painjournalonline.com 2799 Figure 2. Cochrane risk of bias analysis summary of included studies. very low-quality evidence (2 RCTs, N 5 89) that placebo spinal manipulation does not improve back pain compared with no intervention at short-term follow-up (SMD 20.28, 95% CI 21.15 to 0.59, P 5 0.53). There was low-quality evidence (2 RCTs, N 5 80) that placebo taping therapy does not improve physical functioning compared with no intervention at short-term followup (SMD 0.15, 95% CI 20.29 to 0.59, P 5 0.51). We found highquality evidence (2 RCTs, N 5 205) that open-label placebo pill treatment improves short-term pain intensity compared with no intervention (SMD 20.33 95% CI 20.61 to 20.05, P 5 0.02) and also improves physical functioning (SMD 20.34 95% CI 20.62 to 20.07, P 5 0.01). None of these between-group differences was clinically relevant. We found no difference in short-term pain intensity outcomes with exclusion of open-label placebo trials (SMD 20.437, 95% CI 20.5559 to 20.216, P 5 0.20007) (appendix C, supplemental digital content available at http://links.lww.com/PAIN/B345). acute LBP was too small for conducting meta-analyses and to draw conclusions for this subgroup of patients. In patients with chronic LBP, 19 studies were identified. Meta-analyses showed that placebo interventions are more effective than no intervention for pain intensity at short-term follow-up (SMD 20.37; moderate-quality evidence), but this effect, which corresponds to about 8 point on a 0 to 100 scale, may not be considered as clinically relevant. No significant effect was found on pain intensity at medium-term follow-up (SMD 20.26; lowquality evidence). A statistically significant positive effect on physical functioning at short-term follow-up (SMD 20.19; moderate-quality evidence) was found for placebo interventions as compared with no intervention control, but also this effect may not be clinically relevant. Placebo interventions were more effective than no intervention on short-term HRQoL physical health (MD 2.71 on a 0-100 scale; highquality evidence) but not more effective for short-term HRQoL mental health (MD 20.49 on a 0-100 scale; high-quality evidence). No longterm follow-up data were available on any outcome. 4. Discussion 4.1. Results in perspective of the available literature This systematic review shows the magnitude of the placebo effect in patients with LBP. The number of studies (n 5 2) focusing on (sub) Multiple nonpharmacological interventions for chronic LBP have previously been studied and recommended, among these individual Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. 2800 · R.H.W. Strijkers et al. 162 (2021) 2792–2804 PAIN® Figure 3. Forest plots for pain intensity at short-term and medium-term follow-up. Risk of bias assessment: The red circle corresponds with a high risk of bias. The yellow circle corresponds with an unclear risk of bias. The green circle corresponds with a low risk of bias. education, exercise therapy, and multidisciplinary rehabilitation.49 Hayden et al. recently published an individual patient data metaanalysis on exercise therapy for chronic LBP showing a 10.7-point improvement in pain intensity scores at short-term follow-up in comparison with no intervention or usual care, which met our predefined 20% between-group difference for clinical relevance. Regarding physical functioning, a short-term clinically relevant improvement was also reported for exercise therapy.25 Only shortterm effects on pain were found in our analysis. This can in part be explained by the inability to blind the no intervention group. Literature demonstrates there is an effect of expectations on treatment outcome in patients with LBP, and this effect is not expected to last in the medium-term to long-term follow-up.23 Another recent systematic review showed that spinal manipulative therapy (SMT) did not improve pain intensity at short-term follow-up (1 month) compared with sham SMT in patients with chronic LBP, but disability improved only slightly at one month compared with sham SMT.53 Nonsteroidal anti-inflammatory drugs (NSAIDs) are currently the most recommended medications for patients with chronic LBP.49 Interestingly, in a Cochrane review on NSAIDs, authors found an 8point improvement on a pain scale of 0 to 100 compared with placebo.15 Therefore, the magnitude of improvement on pain and functioning of NSAIDs vs placebo intervention is similar to the magnitude of effect for placebo interventions vs no interventions found in this review, both being not clinically relevant effects. However, this is not a direct comparison because the comparator groups are different. It would be more meaningful to compare the placebo effect found in this review with the effect of NSAIDs as compared to no intervention; this indirect comparison would be possible using network meta-analysis but it was outside the scope of this review. This systematic review further contributes to the literature discussion on the magnitude of placebo effects. In 2010, the latest version of the Cochrane review of Hrobjartsson et al. concluded, on basis of 156 trials, that there is no powerful placebo effect, only a potential small effect on subjective outcomes (eg, pain). Contrary to the review of Hrobjartsson, a recent narrative review on the placebo and nocebo effects of Colloca et al. concluded that placebo effects are “powerful and pervasive,” based on the results of laboratory studies.10 Such powerful effects were not found in our meta-analyses that focused on placebo effects on subjective outcomes in RCTs in the field of nonspecific LBP. We argue that laboratory studies, although representing a good platform to modulate placebo effects, may not have a sufficiently controlled setting to determine the magnitude of these effects, which was the focus of this systematic review. In fact, Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. December 2021 · Volume 162 · Number 12 www.painjournalonline.com 2801 Figure 4. Forest plot for physical functioning at short-term follow-up. Risk of bias assessment: The red circle corresponds with a high risk of bias. The yellow circle corresponds with an unclear risk of bias. The green circle corresponds with a low risk of bias. laboratory research is not usually used to assess the effectiveness of health interventions.1 In this review, a larger effect size was found for open-label placebo RCTs as compared to 3-arm RCTs not including an open-label placebo treatment. A possible explanation for the discrepancy in effect size might be that the researchers in the open-label studies are focused on purposively delivering an enhanced placebo intervention, increasing its effectiveness. Given all these observations, we conclude there is a short-term placebo effect on pain intensity in patients with chronic LBP. Although previous research suggested that the magnitude of effect may depend on how exactly the placebo is delivered,59,60 our subgroup analysis separating open-label placebo from placebo controls did not confirm this assertion, at least for patients with chronic LBP. However, it should also be acknowledged that the small number of included studies (n 5 2) prevents definite conclusions at the moment. Most recently, another small open-label placebo trial in patients with chronic LBP was published, showing again a small effect in favor of the placebo intervention as compared to no intervention.34 Another large and adequately powered clinical trial is probably needed to draw firm conclusions on the clinical relevance of the effect of open-label placebos in patients with chronic LBP. Figure 5. Forest plots of health-related quality of life at short-term follow-up. Risk of bias assessment: The red circle corresponds with a high risk of bias. The yellow circle corresponds with an unclear risk of bias. The green circle corresponds with a low risk of bias. Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. 2802 · PAIN® R.H.W. Strijkers et al. 162 (2021) 2792–2804 A previous systematic review in patients with osteoarthritis concluded that contextual effects of interventions are very large and that the more invasive is an intervention, the larger is the placebo effect.65 This conclusion was not confirmed by the subgroup analyses undertaken in this review (supplement E, supplemental digital content available at http://links.lww.com/ PAIN/B345). In fact, an arguably more intensive intervention such as placebo injections did not show a significant reduction in pain intensity compared with no intervention and did not show a larger effect than placebo taping and placebo spinal manipulation (SMD 0.03, SMD 0.09, and SMD 20.28, respectively; see supplement C, supplemental digital content available at http://links.lww.com/ PAIN/B345). Only placebo acupuncture and open-label placebo pills exhibited a significant result in reduction of pain intensity compared with no intervention (SMD 20.37, 95% CI 20.64 to 20.10; N 5 2; P 5 0.007, and SMD 20.33, 95% CI 20.61 to 20.05, P 5 0.02, respectively), but this effect may not be clinically relevant. Hence, in contrast with Zou et al. we could not identify a specific intervention that elicits more profound effects on shortterm pain intensity. This difference could be due to the fact that Zou et al.65 did not rule out the effect of no intervention interventions in their review and the difference in patient population (ie, LBP vs osteoarthritis). Therefore, for patients with chronic LBP, the effect of placebo intervention may not be dependent on the type of intervention but more on other factors such as interaction with researchers or physicians. It is also important to note, however, that the number of studies was very small in these subgroup analyses, and certainly the power to detect significant differential findings was limited. 4.2. Strengths and limitations The use of no intervention control groups corrected for factors such as regression to the mean and natural course of disease thus allows for a valid estimate of symptom improvement that may be attributed to the administration of placebo interventions. Nevertheless, even including a waiting list or no intervention group in a trial gives rise to potential bias.18 For instance, patients in the no intervention group may seek more alternative interventions than patients in the placebo group. Our RoB analyses did not control for the potential impact of co-medication or other co-intervention, and this may have slightly underestimated the magnitude of placebo effects. Conversely, considering that it is not possible to blind personnel and patients in a trial with a no intervention group, there may have also been some overestimation of the effectiveness of placebo interventions, although there is conflicting evidence on the difference in intervention effects between study with or without blinding.47,48 Furthermore, the heterogeneity of placebo interventions summarized in our meta-analyses might be considered a limitation. However, in all analyses the t2 estimate of between study heterogeneity indicated only low variation between effect sizes from individual studies, which allows for meta-analytic summary across the pool of studies despite the obvious diversity in placebo interventions approaches. Another limitation of our study is that by choosing to conduct meta-analyses on aggregate data only we were not able to investigate differential placebo effects with respect to certain patient characteristics. It is known from laboratory research that some individuals experience larger effects of placebo intervention than others depending on personality traits,20 and this aspect could be further explored within individual patient data meta-analyses of the trials included in this review. 4.3. Future research Future research should focus on the factors that moderate and cause the effect in the placebo groups of RCTs. Most of the RCTs included in this systematic review reported pain intensity, but fewer studies reported on physical functioning or disability outcomes, and an even smaller number of studies reported HRQoL as an intervention outcome. We stress the need for uniformity in reporting outcomes, as previously suggested.8 All studies on LBP should at least report on these 3 outcomes. Other outcome measures such as pain interference and pain selfefficacy can also be of use. Furthermore, we observed considerable variation regarding the follow-up period. We advise to use the standard follow-up moments as suggested by the Cochrane Back and Neck review group.19 Only few data were available for medium-term follow-up, and only one study reported on longterm follow-up. However, from a clinical perspective it would be most relevant to see whether the effects caused by placebo interventions sustain over time in patients with LBP. More research is needed in (sub)acute LBP. With the overview on the current evidence based on the effects of placebo interventions from our meta-analysis and other literature, we suggest that future intervention trials in LBP should consider using a 3-arm design, which includes an intervention group, a placebo group (which closely resembles the intervention group), and a waiting list or no intervention group. We recognize recruitment of patients might prove difficult with such a design.56 A potential solution to this problem could consist of an adaptive clinical trial design,51 in which the no intervention group could be dropped if there is an apparent great difference in effectiveness. Alternatively, a trial with multiple baseline assessments might be considered if the use of a no intervention group is unfeasible or considered unethical. 5. Conclusion Placebo interventions in any form seem to be mildly effective in reducing pain intensity in patients with chronic nonspecific LBP at short-term follow-up compared with no intervention. The reduction in pain intensity of 8 points on a 0 to 100 pain scale was statistically significant but may be of limited clinical relevance. Results are independent of the actual type of placebo intervention. A small difference was seen in physical functioning outcome between placebo and no intervention, but this difference may also not be clinically relevant. Placebo intervention improved the physical summary component score of the ShortForm 36 compared with no intervention. Conflict of interest statement The authors have no conflicts of interest to declare. Acknowledgements The authors would like to thank Wichor M. Bramer for his help in developing the database search syntaxes for this systematic review. M. Schreijenberg, A. Chiarotto, and B.W. Koes made substantial intellectual contributions to the development of the original study protocol of this systematic review. R.H.W. Strijkers and M. Schreijenberg performed the data selection, data extraction, and risk of bias assessment. R.H.W. Strijkers conducted the analyses under supervision of H. Gerger and A. Chiarotto. R.H.W. Strijkers, A. Chiarotto, and H. Gerger interpreted the Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. December 2021 · Volume 162 · Number 12 results. R.H.W. Strijkers and M. Schreijenberg drafted the manuscript, which was revised by A. Chiarotto, B.W. Koes, and H. Gerger. All authors have read and approved the final manuscript. www.painjournalonline.com [18] [19] Appendix A. Supplemental digital content Supplemental digital content associated with this article can be found online at http://links.lww.com/PAIN/B345. Article history: Received 23 August 2020 Received in revised form 4 March 2021 Accepted 5 March 2021 Available online 24 March 2021 [20] [21] [22] [23] References [1] Benedetti F. Placebo Effects. 2nd ed. Oxford, United Kingdom:Oxford University Press, 2014. [2] Bialosky JE, George SZ, Horn ME, Price DD, Staud R, Robinson ME. Spinal manipulative therapy-specific changes in pain sensitivity in individuals with low back pain (NCT01168999). J Pain 2014;15:136–48. [3] Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010;1:97–111. [4] Borges TP, Kurebayashi LF, Silva MJ. [Occupational low back pain in nursing workers: massage versus pain] Lombalgia ocupacional em trabalhadores de enfermagem: massagem versus dor. Rev Esc Enferm USP 2014;48:669–75. [5] Brinkhaus B, Witt CM, Jena S, Linde K, Streng A, Wagenpfeil S, Irnich D, Walther HU, Melchart D, Willich SN. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med 2006;166: 450–7. [6] Carvalho C, Caetano JM, Cunha L, Rebouta P, Kaptchuk TJ, Kirsch I. Open-label placebo treatment in chronic low back pain: a randomized controlled trial. PAIN 2016;157:2766–72. [7] Celenay ST, Kaya DO, Ucurum SG. Adding connective tissue manipulation to physiotherapy for chronic low back pain improves pain, mobility, and well-being: a randomized controlled trial. J Exerc Rehabil 2019;15:308–15. [8] Chiarotto A, Deyo RA, Terwee CB, Boers M, Buchbinder R, Corbin TP, Costa LO, Foster NE, Grotle M, Koes BW, Kovacs FM, Lin CW, Maher CG, Pearson AM, Peul WC, Schoene ML, Turk DC, van Tulder MW, Ostelo RW. Core outcome domains for clinical trials in non-specific low back pain. Eur Spine J 2015;24:1127–42. [9] Christiansen DH, de Vos Andersen NB, Poulsen PH, Ostelo RW. The smallest worthwhile effect of primary care physiotherapy did not differ across musculoskeletal pain sites. J Clin Epidemiol 2018;101:44–52. [10] Colloca L, Barsky AJ. Placebo and nocebo effects. N Engl J Med 2020; 382:554–61. [11] Costa LO, Maher CG, Latimer J, Hodges PW, Herbert RD, Refshauge KM, McAuley JH, Jennings MD. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Phys Ther 2009;89: 1275–86. [12] Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, Thomas J. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 2019;ED000142. [13] Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392: 1789–858. [14] Eardley S, Brien S, Little P, Prescott P, Lewith G. Professional kinesiology practice for chronic low back pain: single-blind, randomised controlled pilot study. Forsch Komplementmed 2013;20:180–8. [15] Enthoven WT, Roelofs PD, Deyo RA, van Tulder MW, Koes BW. Nonsteroidal anti-inflammatory drugs for chronic low back pain. Cochrane Database Syst Rev 2016;CD012087. [16] Farasyn A, Meeusen R, Nijs J. A pilot randomized placebo-controlled trial of roptrotherapy in patients with subacute non-specific low back pain. J Back Musculoskelet Rehabil 2006;11:7. [17] Ferreira ML, Herbert RD, Ferreira PH, Latimer J, Ostelo RW, Grotle M, Barrett B. The smallest worthwhile effect of nonsteroidal anti- [24] [25] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36] [37] [38] 2803 inflammatory drugs and physiotherapy for chronic low back pain: a benefit-harm trade-off study. J Clin Epidemiol 2013;66:1397–404. Franke RH, Kaul JD. The hawthorne experiments: first statistical interpretation. Am Sociological Rev 1978;43:623–43. Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, van Tulder MW. Editorial board of the Cochrane back NG. 2015 updated method guideline for systematic reviews in the Cochrane back and neck group. Spine 2015;40:1660–73. Geers AL, Helfer SG, Kosbab K, Weiland PE, Landry SJ. Reconsidering the role of personality in placebo effects: dispositional optimism, situational expectations, and the placebo response. J Psychosom Res 2005;58:121–7. Grunbaum A. The placebo concept in medicine and psychiatry. Psychol Med 1986;16:19–38. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schunemann HJ, Group GW. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008;336: 924–6. Haanstra TM, Kamper SJ, Williams CM, Spriensma AS, Lin C-WC, Maher CG, de Vet HCW, Ostelo RWJG. Does adherence to treatment mediate the relationship between patients’ treatment outcome expectancies and the outcomes of pain intensity and recovery from acute low back pain? PAIN 2015;156:1530–6. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, Smeets RJ, Underwood M. Lancet Low Back Pain Series Working G. What low back pain is and why we need to pay attention. Lancet 2018;391:2356–67. Hayden JA, Wilson MN, Stewart S, Cartwright JL, Smith AO, Riley RD, van Tulder M, Bendix T, Cecchi F, Costa LOP, Dufour N, Ferreira ML, Foster NE, Gudavalli MR, Hartvigsen J, Helmhout P, Kool J, Koumantakis GA, Kovacs FM, Kuukkanen T, Long A, Macedo LG, Machado LAC, Maher CG, Mehling W, Morone G, Peterson T, Rasmussen-Barr E, Ryan CG, Sjogren T, Smeets R, Staal JB, Unsgaard-Tondel M, Wajswelner H, Yeung EW. Chronic Low Back Pain IPDM-AG. Exercise treatment effect modifiers in persistent low back pain: an individual participant data metaanalysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med 2020;54:1277–78. Higgins JP. Commentary: heterogeneity in meta-analysis should be expected and appropriately quantified. Int J Epidemiol 2008;37:1158–60. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. Higgins JPT, Sterne JAC, Savović J, Page MJ, Hróbjartsson A, Boutron I, Reeves B. A revised tool for assessing risk of bias in randomized trials. In: Chandler J, McKenzie J, Boutron I, Welch V, eds. Cochrane Methods Cochrane Database of Systematic Reviews. Chichester, United Kingdom: Wiley-Blackwell, 10, 2016. Hrobjartsson A. What are the main methodological problems in the estimation of placebo effects? J Clin Epidemiol 2002;55:430–5. Hrobjartsson A, Gotzsche PC. Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med 2001; 344:1594–602. Hrobjartsson A, Gotzsche PC. Is the placebo powerless? Update of a systematic review with 52 new randomized trials comparing placebo with no treatment. J Intern Med 2004;256:91–100. Hrobjartsson A, Gotzsche PC. Placebo interventions for all clinical conditions. Cochrane Database Syst Rev 2004:CD003974. Hrobjartsson A, Gotzsche PC. Placebo interventions for all clinical conditions. Cochrane Database Syst Rev 2010:CD003974. Ikemoto T, Ueno T, Arai YC, Wakao N, Hirasawa A, Hayashi K, Deie M. Open-label placebo trial among Japanese patients with chronic low back pain. Pain Res Manage 2020;2020:6636979. Imamura M, Imamura ST, Targino RA, Morales-Quezada L, Onoda Tomikawa LC, Onoda Tomikawa LG, Alfieri FM, Filippo TR, da Rocha ID, Neto RB, Fregni F, Battistella LR. Paraspinous lidocaine injection for chronic nonspecific low back pain: a randomized controlled clinical trial. J Pain 2016;17:569–76. Kamper SJ, Machado LA, Herbert RD, Maher CG, McAuley JH. Trial methodology and patient characteristics did not influence the size of placebo effects on pain. J Clin Epidemiol 2008;61:256–60. Kleine-Borgmann J, Schmidt K, Hellmann A, Bingel U. Effects of openlabel placebo on pain, functional disability, and spine mobility in patients with chronic back pain: a randomized controlled trial. PAIN 2019;160: 2891–7. Koroglu F, Colak TK, Polat MG. The effect of Kinesio(R) taping on pain, functionality, mobility and endurance in the treatment of chronic low back pain: a randomized controlled study. J Back Musculoskelet Rehabil 2017; 30:1087–93. Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited. 2804 · R.H.W. Strijkers et al. 162 (2021) 2792–2804 [39] Leichtfried V, Matteucci Gothe R, Kantner-Rumplmair W, Mair-Raggautz M, Bartenbach C, Guggenbichler H, Gehmacher D, Jonas L, Aigner M, Winkler D, Schobersberger W. Short-term effects of bright light therapy in adults with chronic nonspecific back pain: a randomized controlled trial. Pain Med 2014;15:2003–12. [40] Lewis C, Khan A, Souvlis T, Sterling M. A randomised controlled study examining the short-term effects of Strain-Counterstrain treatment on quantitative sensory measures at digitally tender points in the low back. Man Ther 2010;15:536–41. [41] Licciardone JC, Stoll ST, Fulda KG, Russo DP, Siu J, Winn W, Swift J Jr. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine 2003;28:1355–62. [42] Luz Junior MA, Sousa MV, Neves LA, Cezar AA, Costa LO. Kinesio Taping(R) is not better than placebo in reducing pain and disability in patients with chronic non-specific low back pain: a randomized controlled trial. Braz J Phys Ther 2015;19:482–90. [43] Marchand S, Charest J, Li J, Chenard JR, Lavignolle B, Laurencelle L. Is TENS purely a placebo effect? A controlled study on chronic low back pain. PAIN 1993;54:99–106. [44] Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9, W264. [45] Molsberger AF, Mau J, Pawelec DB, Winkler J. Does acupuncture improve the orthopedic management of chronic low back pain–a randomized, blinded, controlled trial with 3 months follow up. PAIN 2002;99:579–87. [46] Moura CC, Chaves ECL, Chianca TCM, Ruginsk SG, Nogueira DA, Iunes DH. Effects of auricular acupuncture on chronic pain in people with back musculoskeletal disorders: a randomized clinical trial. Rev Esc Enferm USP 2019;53:e03418. [47] Moustgaard H, Clayton GL, Jones HE, Boutron I, Jorgensen L, Laursen DLT, Olsen MF, Paludan-Muller A, Ravaud P, Savovic J, Sterne JAC, Higgins JPT, Hrobjartsson A. Impact of blinding on estimated treatment effects in randomised clinical trials: meta-epidemiological study. BMJ 2020;368:l6802. [48] Nuesch E, Reichenbach S, Trelle S, Rutjes AW, Liewald K, Sterchi R, Altman DG, Juni P. The importance of allocation concealment and patient blinding in osteoarthritis trials: a meta-epidemiologic study. Arthritis Rheum 2009;61:1633–41. [49] Oliveira CB, Maher CG, Pinto RZ, Traeger AC, Lin CC, Chenot JF, van Tulder M, Koes BW. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 2018;27:2791–803. [50] Pach D, Brinkhaus B, Roll S, Wegscheider K, Icke K, Willich SN, Witt CM. Efficacy of injections with Disci/Rhus toxicodendron compositum for chronic low back pain–a randomized placebo-controlled trial. PLoS One 2011;6:e26166. [51] Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, Holmes J, Mander AP, Odondi L, Sydes MR, Villar SS, Wason JMS, Weir CJ, Wheeler GM, Yap C, Jaki T. Adaptive designs in clinical trials: why use them, and how to run and report them. BMC Med 2018;16:29. [52] Puhl AA, Reinhart CJ, Rok ER, Injeyan HS. An examination of the observed placebo effect associated with the treatment of low back pain a systematic review. Pain Res Manage 2011;16:45–52. PAIN® [53] Rubinstein SM, de Zoete A, van Middelkoop M, Assendelft WJJ, de Boer MR, van Tulder MW. Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: systematic review and meta-analysis of randomised controlled trials. BMJ 2019;364:l689. [54] Schmitz J, Muller M, Stork J, Eichler I, Zollner C, Flor H, Klinger R. Positive treatment expectancies reduce clinical pain and perceived limitations in movement ability despite increased experimental pain: a randomized controlled trial on sham opioid infusion in patients with chronic back pain. Psychother Psychosom 2019;88:203–14. [55] Schreijenberg M, Chiarotto A, Mauff KAL, Lin CC, Maher CG, Koes BW. Inferential reproduction analysis demonstrated that “paracetamol for acute low back pain” trial conclusions were reproducible. J Clin Epidemiol 2020;121:45–54. [56] Schreijenberg M, Luijsterburg PAJ, Van Trier YDM, Rizopoulos D, Koopmanschap MA, Voogt L, Maher CG, Koes BW. Discontinuation of the PACE Plus trial: problems in patient recruitment in general practice. BMC Musculoskelet Disord 2018;19:146. [57] Traeger AC, Lee H, Hubscher M, Skinner IW, Moseley GL, Nicholas MK, Henschke N, Refshauge KM, Blyth FM, Main CJ, Hush JM, Lo S, McAuley JH. Effect of intensive patient education vs placebo patient education on outcomes in patients with acute low back pain: a randomized clinical trial. JAMA Neurol 2019;76:161–9. [58] Vas J, Aranda JM, Modesto M, Benitez-Parejo N, Herrera A, MartinezBarquin DM, Aguilar I, Sanchez-Araujo M, Rivas-Ruiz F. Acupuncture in patients with acute low back pain: a multicentre randomised controlled clinical trial. PAIN 2012;153:1883–9. [59] Vase L, Riley JL III, Price DD. A comparison of placebo effects in clinical analgesic trials versus studies of placebo analgesia. PAIN 2002;99: 443–52. [60] Vase L, Wartolowska K. Pain, placebo, and test of treatment efficacy: a narrative review. Br J Anaesth 2019;123:e254–62. [61] Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. [62] Wepner F, Hahne J, Teichmann A, Berka-Schmid G, Hordinger A, Friedrich M. [Treatment with crystal singing bowls for chronic spinal pain and chronobiologic activities—a randomized controlled trial] Quarzklangschalentherapie bei Wirbelsaulenbeschwerdenund chronobiologische Vorgange—eine randomisiertekontrollierte Studie. Forsch Komplementmed 2008;15:130–7. [63] Williams CM, Maher CG, Hancock MJ, McAuley JH, McLachlan AJ, Britt H, Fahridin S, Harrison C, Latimer J. Low back pain and best practice care: a survey of general practice physicians. Arch Intern Med 2010;170: 271–7. [64] Wood L, Egger M, Gluud LL, Schulz KF, Juni P, Altman DG, Gluud C, Martin RM, Wood AJ, Sterne JA. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ 2008;336:601–5. [65] Zou K, Wong J, Abdullah N, Chen X, Smith T, Doherty M, Zhang W. Examination of overall treatment effect and the proportion attributable to contextual effect in osteoarthritis: meta-analysis of randomised controlled trials. Ann Rheum Dis 2016;75:1964–70. Copyright © 2021 by the International Association for the Study of Pain. Unauthorized reproduction of this article is prohibited.