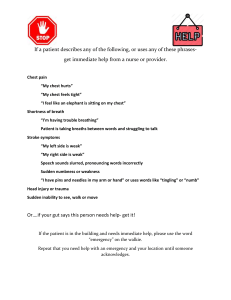
Case Study – Gastrointestinal Disorders -UGI Instructions: All questions apply to this case study. Your responses should be brief and to the point. When asked to provide several answers, list them in order of priority or significance. Do not assume information that is not provided. Scenario Your patient is a 56-year-old general contractor who is admitted to the telemetry unit directly (Direct Admission) from his internist’s office with a diagnosis of chest pain. On report, you are informed that he has an intermittent 2-month history of chest tightness with substernal burning that radiates through the mid back intermittently, in a stabbing fashion. Symptoms occur after meals, especially after dinner or a larger lunch; with heavy lifting at the construction site; and in the middle of the night when he awakens from sleep with coughing, shortness of breath, and sometimes a foul bitter taste in his mouth. Recently, he has developed nausea, without emesis, that is worse in the morning or if he skips a meal. He reports “heartburn” three or four times a day. When this happens, he takes a couple of Tums® or Rolaids® which he keeps in his home, office and truck. VS in his physician’s office were: 130/80 lying, 120/72 standing, 100, 20, 98.6F (37 C), SpO2 92% on RA. A 12-lead showed NSR with a rare PVC. Questions 1. 2. What are some common causes of chest pain? ● GERD- Most common sign is heartburn which is a burning and tightening sensation felt below the sternum that radiates upward to the throat and jaw. ● MI- Myocardial Ischemia symptoms include Angina which often feels like heartburn (chest feels tight like it’s being squeezed and there is chest pain and pressure as well). ● Hiatal hernia when not asymptomatic, the chest pain feels like heartburn especially after eating or lying down. ● Esophageal cancer can cause chest pain below the sternum that can radiate to the shoulders. ● Pneumonia- feels sharp chest pain ● Pleurisy- Pleuritic chest pain usually with feelings of SOB ● Pulmonary embolism- sharp, aching and heaviness is felt in the chest. ● Peptic ulcer disease ● Panic attacks What mnemonic can you use to help you better evaluate his pain? Use PQRST (Provokes the pain/Palliative for the pain, Quality of pain (description of pain like throbbing/stabbing), Radiation (does the pain radiate anywhere or does it stay local?), S (rate pain on a scale of 1-10), Time (how frequently is pain occurring? When did it start?) 3. What other history is important? Patient’s previous medical history. What types of food is he eating? What types of drinks? Is he on any other medication besides TUMS or Rolaids? Is he taking any NSAIDS or aspirin? Does the patient have a history of or does he currently smoke or drink? I would want to get his current weight to see if he is obese. Is the job stressful? What is his mental status like? Does he have anxiety? Depression? Case Study Progress The patient reports that the antacids usually relieve his chest pain, but this time they had no effect. A “GI cocktail” consisting of Mylanta® and viscous lidocaine given at the physician’s office helped briefly. Questions 1. What tests can be done to determine the source of his problems? ● EKG and troponin labs to rule out any cardiac problems (MI) ● ● ● ● ● ● ● ● ● Chest x-ray to rule out Respiratory issues like pneumonia and pleurisy. ABG’s - testing CO, O2, pH imbalances in the blood Endoscopy to see the lower esophagus and assess for any inflammation or abnormalities like ulcers, scarring or strictures. While there, they can obtain a biopsy of the esophageal tissue as well. Esophagogram (barium swallow)- to assess for abnormalities in your upper GI tract. This test could show if there is a gastric obstruction or a protrusion of the gastric mucosa through the opening in the diaphragm that the esophagus passes through (esophageal hiatus). This test can be given as an alternative to endoscopy. Esophageal manometric study- to measure the pressure in the esophagus and in the lower esophageal sphincter (LES). this check to see how well the esophagus relaxes and contracts. CT or MRI to detect if its esophageal cancer H. pylori can be tested by biopsy of the mucosa and tested for urease. Urea is a byproduct from the H. pylori bacteria. Other ways include a blood test, stool and breath testing which can identify active infections. CBC count Xray to detect abnormalities in the upper GI tract such as hiatal hernias Case Study Progress The patient reports that he is a cigarette smoker and has smoked about a pack a day for the last 35 years, drinks 2-3 beers on most night after work, and has noticed a 20-pound weight gain over the past 10 years. He feels “tired and old now”. He has dark circles under his eyes and reports constant daytime fatigue. His wife is even sleeping in another bedroom because he snores so loudly. He also tells you that he reinjured his back a about a month ago at work, lifting a pile of boards, so his physician prescribed ibuprofen (Motrin®) 800 mg twice or three times a day for 4 weeks and famotidine (Pepcid®) 20 mg orally at bedtime for heartburn. Questions 1. Which factors in this patient’s life are likely contributing to his chest pain and nausea? Explain how. Nausea could stem from many organ system problems but in this case it is more likely to be due to an over irritated GI tract, a GI disorder, or from a psychological factor like work stress. Smoking can contribute to GERD by relaxing the LES sphincter which is supposed to prevent gastric juices from leaving the stomach and moving upward. If the patient is obese (his weight in unknown to us but he did mention a 20lb weight gain), this can increase intrabdominal pressure. Drinking decreases pressure in LES and affects its ability for the LES to contract or close which can lead to acid regurgitation into the esophagus. Smoking and drinking both stimulate acid secretion on the body and when there is too much acid in your stomach this can lead to feelings of nausea and chest pain from heartburn. Continuous lifting of heavy weights can increase intra-abdominal pressure which can lead to the development of a hiatal hernia. 2. Why do you think famotidine did not help? Famotidine may not be working because this may not be a GERD issue with there being too much acid being present in the stomach and moving upwards into the esophagus. There is another underlying issue causing the heartburn. The time of day that the patient is taking the medication may also play a factor into the reason for why this is not working since he is complaining of a bitter taste in the morning and heartburn issues at lunch and dinner. Case Study Progress The patient’s repeat 12-lead ECG and first set of cardiac enzymes were normal. The chest x-ray showed no abnormalities. Room air SpO2 is 94% and breathing is unlabored. VS remain stable. Admission Laboratory Values WBC 6,000 /mm3 Hgb 15.0 g/dL Hct 47% Platelets 220,000/mm3 Na K BUN Creatinine 140 mEq/L 3.7 mEq/L 20 mg/dL 1.0 mg/dL Lipase Amylase 20 units/L 18 units/L PT INR 12 sec 1.0 H. pylori. 20 units/mL The patient suddenly reports nausea and vomits coffee-ground emesis with specks of bright red blood. Questions 1. 2. What concerns do you have about the coffee ground emesis? The return of emesis with bright blood specks is a sign of upper GI bleeding and could possibly be esophageal damage or worse cancer. Also, coffee is a strong stimulant of gastric acid secretions so knowing the patient is drinking coffee even though they have heartburn and GI problems is a concern. What is the significance of the H. pylori test result? This bacteria is a common cause of gastric ulcers. Results showing Less than 30 units/mL means it is negative. This patient doesn't have gastric ulcers caused by H. pylori. Case Study Progress You ask the charge nurse to contact the GI consulting doctor and update them on the patient’s condition and recent events. The physician assesses the patient and gives several orders in preparation for an esophogastrodudenoscopy (EGD). Chart View Physician’s Orders ● ● ● ● ● ● ● NPO status for emergent esophogastrodudenoscopy (EGD) STAT CBC Oxygen by nasal canula; titrate oxygen to maintain SpO2 over 92% Type and crossmatch (T&C) 2 units packed red blood cells (PRBC) and hold Start a pantoprazole (Protonix) drip at 8 mg/hour, preceded by an 80 mg bolus IV over 8 minutes. Insert a Salem Sump nasogastric (NGT) and start a gastric lavage with normal saline. Insert two large bore IVs and start normal saline (NS) at 100 mL/hour. Questions 1. 2. List the previous orders in order of priority. 1. NPO 2. STAT CBC 3. TNC 4. Insert IV 5. O2 by nasal cannula 6. Protonix 7. NGT Explain the rationale for each of the preceding orders. 1. NPO- want to prevent aspiration of food and 2. IV access to draw blood and to deliver medications and NS 3. CBC- Want HCT, HGB to assess blood loss 4. TNC- to match donor’s blood to the recipient’s to prevent donor blood rejection 5. O2- reduces oxygen carrying capacity due to active bleeding. 6. Protonix is ordered to relieve heartburn and to aid in healing acidic damage in the esophagus and stomach. 7. NGT- want to clean the stomach if the patient has been vomiting blood. This allows the technician and physician to be able to see the stomach and esophagus during the EGD procedure. Case Study Progress The gastroenterologist finds erosive esophagitis, a moderately sized hiatal hernia, diffuse erosive gastritis, and an ulcer in the antrum of the stomach that is oozing blood. The duodenal bulb yielded a normal endoscopic appearance. During the EGD, the bleeding was stopped with cautery. Biopsies were obtained of the gastric mucosa, and the biopsies are negative for H. pylori bacteria; his bleeding ulcer is attribute to the NSAIDs. He is kept NPO until the next morning to allow for good hemostasis of the cauterized site. Clear liquids are allowed at breakfast. His hematocrit dropped to 32%, but he remained asymptomatic for the mild anemia; the drop, in part, was believed to reflect that he was dehydrated upon admission, and the drop reflected the dilution from the IV fluids added. He tolerated the liquid diet without N/V and was discharged home the next day with the following instructions: ● ● ● ● ● Advance your diet slowly, as tolerated to mechanically soft. Take pantoprazole 40 mg orally every morning on an empty stomach, at least 30 minutes before eating. Make a follow-up appointment with the following physician (name, address and telephone) Stop all aspirin and over-the-counter (OTC) medications (ibuprofen, naproxen) or herbal pain relief medications and omega 3 preparations (fish oil). Stop or limit smoking and alcohol intake. Questions 1. Why does the patient need to take the pantoprazole first thing in the morning? This used to stop the production of gastric acid, and this helps with preventing further gastric mucosa injury. 2. After discussing lifestyle modifications for controlling acid reflux with the patient, which statements indicate a further need for teaching? a. “I will try to stop smoking.” b. “I will wait thirty minutes before lying down or sitting in my recliner after meals.” c. “I will avoid fatty foods, caffeine, and chocolate.” d. “I will avoid eating two to three hours before my bedtime.” B. the patient should not lie down for 2 to 3 hours after a meal.