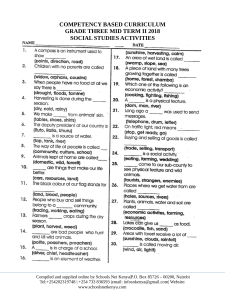
lOMoARcPSD|11334620 Medsurgultimate - Nurse Angie Medical Surgical Nursing II (ECPI University) StuDocu is not sponsored or endorsed by any college or university Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 JULY 2020 | ISSUE NO. 7 MEDICAL SURGICAL Nursing 1. NOTE TAKING TEMPLATE 2. SMART GOALS 3. CONCEPT MAPS 4. NEURO 5. RESPIRATORY 6. CARDIAC 7. ONCOLOGY 8. BILIARY 9. RENAL 10. ELECTROLYTES 11. ENDOCRINE 12. EYE 13. GI 14. LIVER "THE MEANING OF LIFE IS TO FIND YOUR GIFT. THE PURPOSE OF LIFE IS TO GIVE IT AWAY." —WILLIAM SHAKESPEARE "When I think about all the patients and their loved ones I have worked with over the years, I know most of them don't remember me, nor I them. But I do know that I gave a little piece of myself to each of them, and they to me, and those threads make up the tapestry that is my career in nursing." —Donna Wilk Cardillo 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 2 ADPIE NOTE TAKING METHOD Assessment Diagnosis PATHOPHYSIOLOGY Disease Process: Planning Interventions Evaluation 2 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 3 SMART GOALS FOR PLANNING PATIENT CARE Specific Who, what, where , when, which and why Attainable Measurable Create criteria SMART GOAL Track progress Develop attitudes, abilities, skills Plan your steps Willing and able to work towards the goal Anchor your goal to a specific date Realistic Timely Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 3 lOMoARcPSD|11334620 4 Pathophysiology Concept Maps 4 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 5 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 5 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 6 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 6 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 7 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 7 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 8 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 8 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 9 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 9 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 10 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 10 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 11 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 11 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 12 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 12 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 13 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 13 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Medical Surgical Nursing Concept Map 14 Disease & Pathophysiology Assessment Physical Findings Causes Risk Factors Interventions Medications Monitoring Prioritization 14 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 15 MEDICAL SURGICAL NURSING: NEURO 1.9.5 NURSE ANGIE 2018 Head Injury Trauma to the skull such as jarring, shaking or laceration can lead to mild or extensive brain damage. Assessment Types Concussion: A brain injury caused by a blow to the head or a violent shaking of the head and body. This is a closed type of head injury. Contusion: Bruising or bleeding on the brain due to localized trauma.This is also a closed head injury. Closed head injury: Traumatic brain injury in where the skull and dura mater remain intact. These are the leading cause of death in children under 4 years old and the most common cause of physical disability and cognitive impairment in young people. Basilar Skull Fracture: Is a fracture of the base of the skull, typically involving the temporal bone, occipital bone, sphenoid bone, and/or ethmoid bone. These are very uncommon. Can be a closed fracture. Epidural Hematoma: Bleeding occurs between the skull and the dura (the brain cover). The bleeding is from an injury to a vein or a branch of the posterior meningeal artery. The most dangerous type of hematoma Subdural hematoma: Known as a subdural hemorrhage (SDH), is a type of hematoma, usually associated with traumatic brain injury. Blood gathers between the inner layer of the dura mater and the arachnoid mater. Intracerebral Hematoma: Blood leaks into the brain as a result of head trauma or spontaneously. Subarachnoid Hemorrhage: Bleeding into the subarachnoid space. Can be caused by ruptured aneurysm or trauma ‣ Assessment finding will vary depending on the type and severity of the head injury. ‣ Increased ICP ‣ LOC changes ‣ Altered mental status ‣ Airway and breathing changes ‣ Vital signs will show increased ICP ‣ Visual changes ‣ Pupillary changes and papilledema ‣ Nuchal Rigidity ‣ CSF drainage ‣ Weakness and paralysis ‣ Posturing ‣ Decreased sensation ‣ Reflex changes ‣ Seizure activity Treatments ‣ Minor Injury: Repair CSF leak, lacerations of the scalp ‣ Penetrating wounds: Surgical repair and antibiotics ‣ Moderate to severe head injury: supportive care, prophylactic antiseizure medications, prevent and control intracranial hypotension, prevent brain damage from hypotension , prevent anemia, Increased arterial Carbon Dioxide levels. COMPLICATIONS ‣ Cerebral bleeding ‣ Hematoma ‣ Uncontrollable ICP ‣ Infections ‣ Seizures ‣ CSF leakage EDUCATION INTERVENTIONS ‣ Administer Glucocorticoids: Dexamethasone, mannitol and Educate the client and family on possible behavior changes, the long term effects of a traumatic brain injury and when to contact the HCP ‣ Monitor respiratory status and maintain patent airway, increased C02 levels cause cerebral edema. ‣ Monitor vitals & Temperature Monitor neuro status ‣ Monitor for signs of ICP ‣ Keep head elevated to reduce venous pressure ‣ Prevent neck flexion ‣ Initiate normothermia measures. ‣ Assess for pain and restlessness. ‣ Monitor for CSF drainage ‣ Mental status changes ‣ Behavioral changes ‣ Cranial nerve deficits 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) furosemide these are hypertonic solutions that will pull fluid from the brain and decrease intracranial pressure. ‣ Barbiturate therapy: Decreases cerebral metabolic weight. ‣ Morphine Sulfate: Decreases agitation and restlessness, administer with caution because it can cause respiratory depression which will also cause ICP. 15 lOMoARcPSD|11334620 16 MEDICAL SURGICAL NURSING: NEURO 1.9.1 NURSE ANGIE 2018 Hyperthermia An elevated body temperature due to failed thermoregulation that occurs when a body produces or absorbs more heat than it dissipates. Pathophysiology Assessment A fever occurs when the body sets the core temperature to a higher temperature, through the action of the pre-optic region of the anterior hypothalamus. In contrast, hyperthermia occurs when the body temperature rises without a change in the heat control centers. temp above 105* increases cerebral metabolism and increases the risk for hypoxia. Hyperthermia is different from a fever because it is characterized by an uncontrolled increase in body temperature that exceeds the body’s ability to lose heat. The setting of the hypothalamic thermoregulatory center is unchanged. In contrast to fever in infections, hyperthermia does not involve pyrogenic molecules. ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Agitation Confusion Dizziness Hypertension then hypotension Moist cool skin Thready pulse Seizures Tachypnea Arrhythmias Medications ‣ ‣ ‣ ‣ ‣ Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ Interventions Increased PaCO2 Increased CK Increased plasma lactate Decreased PaO2 acidosis Hyperkalemia (potassium leaks out of the muscle cells) Myoglobin in blood or urine (from cell death and rhabdomyolysis - precipitates in renal tubules causes urinary obstruction and RF) CAUSES ‣ Infection ‣ Salt and water deprivation in a hot environment Stages ‣ Mild: Temp over 99 degrees to 102 degrees ‣ Moderate: up to 104 degrees ‣ Severe: temperature greater than 105 degrees Severity of symptoms are based on the clients temperature. Symptoms range from mild confusion to critical neurological and cardiovascular issues including death. Dantrolene: To lower temperature and prevent seizures. Bicarbonate: To reverse acidotic state. Glucose: Due to elevations in insulin levels with higher body temperatures IV fluids: To replenish fluid loss and reverse dehydration. Chlorpromazine and diazepam: To stop excessive shivering. ‣ Heat stroke ‣ Endocrine disorders INTERVENTIONS ‣ Medications such as: diuretics, ‣ ‣ ‣ ‣ ‣ Oxygen therapy Cvp monitoring Intubation if needed Continue vital sign monitoring If you reduce the body temperature too fast you can cause vasoconstriction which increases metabolic demand and oxygen consumption from shivering ‣ Monitor neuro and cardio status anticholinergics, malignant hyperthermia can result from anesthesia or succinylcholine due to a genetic issue. ‣ Remove clothing and avoid shivering ‣ Apply hypothermic blanket ‣ Apply ice packs to the groin area ‣ Treatment continues until body temperature has decreased to 102.2 Memory Trick Some hot dude better give fluids fast! Stop triggering agents Hyperventilate & give 100% 02 Dantrolene administration Bicarbonate administration Glucose and insulin IV fluids and cooling blanket Fluid intake & output monitoring ‣ Exposure to high temps ‣ Dysfunction of thermoregulatory centers ‣ Brain injury or trauma 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 16 lOMoARcPSD|11334620 17 MEDICAL SURGICAL NURSING: NEURO 1.9.12 NURSE ANGIE 2018 Guillain barre syndrome Disorder in which a person's immune system attacks the peripheral nervous system. Pathophysiology Assessment Prior infection leads to an immune response. The immune response the cross-reacts with the peripheral nerve components, causing segmental demyelination of peripheral nerves. Preventing normal transmission of electrical RISK FACTORS impulses. Sensorimotor nerve roots are affected; autonomic nerve ‣ Recent surgery or transplant ‣ Diabetes mellitus transmission may also be affected ‣ Rabies or swine influenza vaccination ‣ Viral illness, most commonly respiratory followed by gastrointestinal infections ‣ Hodgkins. Meningococcal vaccination ‣ Zika viral infection ‣ Meningococcal vaccination ‣ Zika viral infection INTERVENTIONS ‣ Supportive measures ‣ Emotional support ‣ Maintenance of skin integrity ‣ Possible endotracheal Laboratory Findings: intubation or tracheotomy with ‣ Liver function levels: May be elevated. ‣ Creatinine phosphokinase level and erythrocyte sedimentation rate test: Results may be elevated ‣ Cerebrospinal fluid (CSF) analysis: May show a normal white blood cell count, an elevated protein count, and, in severe disease, increased CSF pressure. ‣ Electromyography: Demonstrates repeated firing of the same motor unit instead of widespread sectional stimulation. ‣ Nerve conduction studies: Show prolonged F-wave latency initially, conduction block, and marked slowing of nerve conduction velocities. CAUSES/COMPLICATIONS Education ‣ Not to receive live vaccines ‣ Can get PPD ‣ Encourage coughing and deep breathing ‣ Use TENS ‣ Home oxygen ventilator support ‣ Cardiac monitoring ‣ Fluid volume replacement ‣ Urinary catheterization for urine retention due to autonomic neuropathy ‣ Plasmapheresis ‣ Transcutaneous electrical nerve stimulation (TENS) for ‣ Can be a post infectious immunemediated disorder ‣ Campylobacter jejuni and cytomegalovirus ‣ Paralysis ‣ Permanent residual weakness ‣ Arrhythmias, Urine retention ‣ Thrombophlebitis ‣ Pressure injury ‣ Contractures ‣ Muscle wasting, Aspiration ‣ Respiratory tract infections; adult respiratory distress syndrome ‣ Life-threatening respiratory and cardiac compromise pain ‣ Occupational and speech therapy ‣ Venous thromboembolism (VTE) prophylaxis ‣ Adequate fluid and caloric intake ‣ Enteral feedings if intubated ‣ Aspiration precautions 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ MS: Weakness of the limbs, muscle weakness, Paralysis of the ocular, facial, and oropharyngeal muscles. ‣ GI/GU: Urinary retention or difficulty with bowel and bladder function, decreased bowel sounds. ‣ Neuro: Sensory loss, usually in the legs (spreads to arms), difficulty talking, chewing, and swallowing, sensory loss, usually in the legs (spreads to arms), Difficulty talking, chewing, and swallowing, facial flushing. ‣ RESP: oor inspiratory effort, Diminished breath sounds, respiratory failure, dyspnea on exertion. ‣ Cardio: Tachycardia, bradycardia, labile blood pressure. Treatments ‣ I.V. immune globulin ‣ Low-molecular-weight heparin : Enoxaparin sodium (Lovenox) for deep vein thrombosis prophylaxis ‣ Analgesics: Opioids for pain control ‣ Laxatives: Constipation or ileus due to autonomic neuropathy ‣ Tricyclic antidepressants, tramadol hydrochloride (Ultram), gabapentin(Neurontin), carbamazepine (Tegretol), or pregabalin (Lyrica) for long-term management of pain; gabapentin or carbamazepine for pain control during the acute phase ‣ Oxygen ‣ I.V. fluids for volume expansion if hypotensive 17 lOMoARcPSD|11334620 18 MEDICAL SURGICAL NURSING: NEURO 1.9.13 NURSE ANGIE 2018 Alzheimer’s Degenerative, irreversible disorder of the cerebral cortex. Pathophysiology The disease initially involves the parts of the brain that control thought, memory, and language. Neurons involved with communication, metabolism, and repair are disrupted.Brain damage is caused by a substance called amyloid. The disorder reveals three distinguishing features of brain tissue: Neurofibrillary tangles, neuritic plaques, and granulovacuolar degeneration Assessment ‣ C:Cognitive changes ‣ O: Olfactory dysfunction ( loss of smell) ‣ N: Not able to remember recent events ‣ F: Frustration, irritability ‣ U: Unable to recognize self ‣ S: Steroidogenesis is impaired ‣ I: Incontinence ‣ O: organic brain disease ‣ N: Not able to walk steadily Treatments INTERNVENTIONS Laboratory Findings: ‣ Positron emission tomography: Reveals metabolic activity of the cerebral cortex. ‣ Computed tomography scanning (brain): Shows excessive and progressive brain atrophy and rules out other neurologic problems. ‣ Magnetic resonance imaging:Rules out intracranial lesions and detects biochemical and anatomic changes, including generalized and focal atrophy. ‣ Cerebral blood flow studies: Reveal abnormalities in blood flow to the brain. ‣ Cerebrospinal fluid analysis: Shows chronic neurologic infection and possibly elevated tau protein levels and low amyloid protein levels. ‣ Electroencephalography: May show slowing of the brain waves in late stages of the disease. ‣ Preclinical Alzheimer disease: ‣ Neuropsychological tests may show Evidence of measurable impaired cognitive ability and changes in brain biomarkers reasoning. years before any signs and ‣ Diagnosis is by exclusion; tests are symptoms involving memory, performed to rule out other diseases. thinking, or behavior are noted ‣ Positive diagnosis is made on autopsy. STAGES CAUSES ‣ Abnormal processing of amyloid-beta protein ‣ Acetylcholinesterase inhibitors, such as donepezil hydrochloride (Aricept), rivastigmine (Exelon), and galantamine hydrobromide (Razadyne) ‣ Safe activities as tolerated ‣Selective serotonin reuptake inhibitors (SSRIs), such as (may need to be monitored) sertraline hydrochloride ‣ Exercise to reduce restlessness (Zoloft) and citalopram ‣ Participation in mental hydrochloride (Celexa), for depression activities (patients with normal ‣Trazodone hydrochloride or mildly impaired cognition) (Oleptro), zolpidem tartrate (Ambien), zaleplon(Sonata), or ‣ A home-based balanced ramelteon (Rozerem) for exercise program may insomnia ‣Benzodiazepines, such as decrease risk of falls. lorazepam (Ativan) and ‣ Well-balanced (may need to be buspirone monitored) hydrochloride(Aplenzin), or SSRIs for moderate anxiety ‣ Avoidance of caffeineand restlessness containing foods, such as ‣Antipsychotics, such as coffee, tea, cola, and chocolate risperidone (Risperdal) and olanzapine (Zyprexa), or ‣ Nutritional supplements in anticonvulsants, such as later stages carbamazepine (Tegretol) and valproic acid(Depakene), for ‣ Behavioral interventions severe aggressive agitation (patient-centered or caregiver ‣Memantine hydrochloride training) focused on managing (Namenda) to help preserve memory cognitive and behavioral ‣Ginkgo biloba (conflicting changes results) to improve or preserve memory ‣ Occupational therapy ‣ Music therapy (being used primarily for research purposes, not for diagnosis) ‣ Mild cognitive impairment: Noticeable mild changes in memory and thinking that can be measured using a mental status examination Changes not severe enough to affect the person's daily functioning. ‣ Dementia due to Alzheimer disease: Significant impairment in memory, thinking, and behavior. Impairments impacting the person's ability to function independently ‣ Advance directive planning 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 18 lOMoARcPSD|11334620 19 MEDICAL SURGICAL NURSING: NEURO 1.9.8 NURSE ANGIE 2018 Amyotrophic Lateral Sclerosis A degenerative disorder that is progressive in nature ALS is also known as Lou Gehrig’s disease. Pathophysiology Risk Factors Excess glutamate causes progressive muscle weakness and atrophy until flaccid tetraplegia occurs. As the disease progresses the respiratory muscles become affected causing respiratory compromise, pneumonia and eventually death. ‣ Age ‣ Family history ‣ Cigarette smoking Assessment P: Pneumonia L: Loss of coordination A: Atrophy of the muscles Y: Young or old can get it B: Bilateral weakness and tetraplegia Complications ‣ Respiratory tract infections and respiratory failure ‣ Complications of immobility ‣ Aspiration ‣ Injury ‣ Pressure injury ‣ Pulmonary emboli ‣ Nutritional deficiencies ‣ Death A: Aspiration risk L: Loss of energy , fatigue. L: Loss of respiratory function Treatments ‣ Riluzole (Rilutek) slows the progression of ALS in some patients, by reducing levels of glutamate in the brain ‣ Edaravone (Radical) — reduces the decline in daily functioning associated with ALS. It is given by intravenous infusion (typically 10-14 days Laboratory Findings: in a row, once a month), and ‣ Electromyogram: Shows fibrillation and fasciculation. Motor conduction will be slow or slightly normal. ‣ CCK: elevation in creatinine Kinase from muscle changes. ‣ Respiratory: pulmonary function testing will show decreased vital capacity. bruising, gait disturbance, side effects may include hives, swelling and shortness of breath. ‣ EDUCATION ‣ Educate the caregiver on suctioning to remove secretions and reduce the risk of aspiration. ‣ Educate the patient to tuck their chin in while eating and drinking to avoid aspiration. ‣ Patient may need thickened liquids. CAUSES INTERVENTIONS ‣ Gene mutation. ‣ Chemical imbalance. ‣ Monitor respiratory status. ‣ Prevent aspiration. ‣ Prepare to begin respiratory support. ‣ Administer spasmolytic agents as ordered. ‣ BIPAP ‣ Refer to hospice. ‣ Monitor vitals and cardiovascular status ‣ Assess gag reflex ‣ Disorganized immune response. ‣ Protein mishandling. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 19 lOMoARcPSD|11334620 20 MEDICAL SURGICAL NURSING: NEURO 1.9.4 NURSE ANGIE 2018 Brain abscess A lesion on the brain that is rare in healthy people. Pathophysiology Assessment Infectious material that has collected in the brain mostly caused by accumulation of bacteria. The most common cause of brain abscess is otitis media and rhino-sinusitis. Abscesses can also be a result of intracranial surgery, penetrating head injury, and tongue piercings. Organisms can spread from the lungs, gums, wound, heart, or tongue. ‣ S: severe headache ‣ T: total loss of consciousness ‣ I: Impaired motor function , nuchal rigidity. ‣ F: funky rash ‣ F: fever Treatments ‣ Antibiotic agents that cross the blood brain barrier. ‣ Penicillin G in combination with a cephalosporin : ceftriaxone IV within 30 minutes of hospital arrival. ‣ Dexamethasone: adjunct therapy in acute bacterial meningitis, improves the outcome of adults. Does not cause GI bleeding. Laboratory Findings: ‣ ‣ ‣ ‣ ‣ Fluid replacement: treatment for CT: Is mostly used to identify location and size of the abscess. Aspiration is also guided by CT or MRI. Culture & Sensitivity: To identify the organism and how to treat it. Chest X-Ray: Rules out prior lung infections. EEG: To Localize the lesion. dehydration and shock. With fluid volume expanders. Preventions CAUSES ‣ Otitis media ‣ Tongue piercings ‣ Oral infections ‣ Cardiac infections ‣ Lung infections ‣ Mastoiditis ‣ Rhinosinusitis ‣ Systemic infections Education INTERVENTIONS ‣ Importance of immediately reporting worsening of symptoms ‣ need for continued follow-up care, for at least 3 months to evaluate the effectiveness of treatment, identify any new lesions, and manage any complications ‣ Seek treatment immediately for infections ‣ importance of adhering to the prescribed medication regimen to ensure complete resolution of the infection ‣ Continuous neurological monitoring ‣ Monitor vital signs ‣ Administer antibiotics ‣ Monitor for signs of ICP ‣ Monitor blood glucose and Potassium when administering corticosteroids. ‣ Initiate seizure precautions ‣ Keep patient safe and free of falls ‣ Assess distress and ability to cope with altered state. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Meningitis vaccine. ‣ Treatment of those who have been exposed within 24 hours. ‣ Flu vaccine ‣ Pneumonia vaccine. FACTS Aminoglycosides, erythromycin, tetracyclines, and first-generation cephalosporins aren’t indicated for use with brain abscess. These agents don’t cross the blood-brain barrier at concentrations that are high enough to be effective. 20 lOMoARcPSD|11334620 21 MEDICAL SURGICAL NURSING: NEURO 1.9.5 NURSE ANGIE 2018 Increased intracranial pressure Pressure on the brain from increased swelling on the brain. Assessment Pathophysiology Can be caused by trauma, intracranial hemorrhage, tumors, hydrocephalus, edema, or inflammation. Increased ICP impaired cerebral circulation, decreases absorption of CSF, affects the functioning of nerve cells and can lead to brain stem herniation or death. Normal ICP ranges from 5-15 mmHg anything above 20 indicates immediate treatment. INTERVENTIONS • • • • • ! • CPP • Pressure that pushes blood to the brain. • Normal CPP 60-100 mmHg • When CPP falls too low < 50 mmHg brain death occurs due to cerebral hypoxia. • CPP= MAP-ICP INFLUENCING FACTORS • Body temperature: Fever • Oxygenation : Elevated C02 • causes vasodilation or hypoxia • Body position • Arterial or Venous pressure • Intra Abdominal or thoracic pressure: vomiting, hip flexion • P: Position, elevate HOB 30-35 degrees, midline. Avoid flexion of head or hips R: Respiratory status monitoring, prevent hypoxia and hypercapnia. Maintaining a PCO2 at 30-35 mmhg will decrease ICP by causing vasoconstriction Suction for only 15 seconds at a time. Keep peep low with mechanical ventilation. E: Elevated temp, lower body temp, prevent shivering, this can increase ICP. administer antipyretics, cool blankets, decreased room temp. S: Systems to monitor, frequent neuro checks, glasgow coma scale, S: Straining activities to avoid: Vomiting, sneezing, valsalva, keep a calm environment and avoid restraints. U: Unconscious patient care: avoid morphine to avoid hypoxia, monitor lung sounds, ROM, eye care, blood clots. R: RX: administer vasopressors,IVF, barbiturates to decrease brain metabolism, MAINTAIN SBP >90 <150, anticonvulsants, hyperosmotic drugs such as mannitol to pull fluids from the brain. E: Edema management with mannitol to dehydrate the brain. Electrolyte monitoring r/t fluid volume or depletion 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Altered LOC ( earliest presenting symptom) ‣ Headache ‣ Cheyne stokes ‣ Increased BP with ‣ widening pulse ‣ pressure ‣ Double vision ‣ Swelling of optic ‣ nerve ‣ Unequal pupils ‣ Fever ‣ Vomiting ‣ Pupil changes Late signs •Cushing's triad: increased systolic pressure, bradycardia, bradypnea. •widened pulse pressure, decreased CPP, •Hemiplegia •Posturing : Decorticate, Decerebrate ( death) •Seizures •Papilledema • Dolls eyes Treatments • Anticonvulsants: Prophylaxis against seizures which increase ICP. • Antipyretics/ Muscle relaxants: Antipyretics prevent temperature elevation & Muscle relaxants prevent shivering • Blood pressure drugs: Needed to maintain BP of 90-150 mmHg to avoid cerebral hypoxia. • Corticosteroids: Stabilize the cell and reduces leakage of fluids through the blood brain barrier which, decrease cerebral edema • IV Fluids: Hypotonic fluids are avoided due to risk of cerebral edema • Hyperosmotic Fluids: Increase intravascular pressure by drawing fluids from the brain to the vasculature and out via the kidneys. Monitor renal function. Monitor intake and output 21 lOMoARcPSD|11334620 22 MEDICAL SURGICAL NURSING: NEURO 1.9.2 NURSE ANGIE 2018 Encephalitis An acute inflammatory process that affects the brain tissue, the cerebrum, brainstem, and cerebellum. Pathophysiology Assessment Encephalitis is an inflammatory process caused by the herpes simplex virus or bites from a tick or mosquito and causes necrotizing hemorrhage of the brain that becomes generalized and is followed by edema. Encephalitis also can cause damage to nerve cell bodies. • • • • • • • • • • • • H: Herpes Virus infection E: Enterovirus infection R: Rigidity P: Populations with lots of disease E: Extreme changes in LOC S: Sores in the mouth V: Varicella infection I: Insect Bites R: Really high fever U: unilateral paralysis S: Seizures Lab studies • MRI: Inflammation in the basal ganglia • • • • • • ( St. Louis) or periventricular area ( West Nile) EEG: Abnormal brain waves. CSF: Immunoglobulin M antibodies will be present Fungal Encephalitis CSF: Elevated White cells and protein or candida Neuroimaging: Identifies CNS changes MRI: Is the study of choice, identifies hemorrhage, abscess or inflammation. Treatments Laboratory Findings: ‣ EEG: Diffuse slowing or focal changes in the temporal lobe. ‣ Lumbar Puncture: High opening pressure, normal glucose range, high protein levels. ‣ Viral cultures: Usually negative ‣ Polymerase Chain reaction: Standard test for early diagnoses and identifies the DNA of HSV-1, validity is highest on the 3rd and 10th day post symptom onset. EDUCATION ‣ Encourage fluid intake ‣ Small frequent meals ‣ Educate the client on the disease. ‣ Educate the client on the treat regimens and when to call the HCP. INTERVENTIONS ‣ Assess neurological function and for signs of ICP ‣ Assist client to Turn cough and Deep breathe ‣ Elevate HOB 30-45 degrees ‣ Comfort measures to reduce headache. ‣ Administer analgesia. ‣ Use opioids cautiously because they can mask neurological symptoms. ‣ Seizure precautions. ‣ Monitor Blood cultures. ‣ Monitor intake and output due to possible renal impairment from the antivirals. ‣ Initiate rehabilitation for motor dysfunction CAUSES ‣ Viral infection of HSV ‣ Mosquito bites ‣ Tick bites ‣ Bacteria ‣ Fungi ‣ parasites 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Acyclovir: Antiviral agent , decreased dose if the patient has a history of renal impairment. ‣ Ganciclovir: Antiviral Agent ‣ Starting antivirals early is well tolerated and the patient should continue treatment for up to 3 weeks. ‣ IV administration over 1 hour prevents crystallization of the medication in the urine. ‣ Interferon : St. Louis Encephalitis ‣ Lumbar Puncture and Shunting: Fungal encephalitis. ‣ Amphotericin B: Treats progressive fungal infection. May cause renal dysfunction ‣ Fluconazole: Treats fungal infection and may cause bone marrow depression 22 lOMoARcPSD|11334620 23 MEDICAL SURGICAL NURSING: NEURO 1.9.3 NURSE ANGIE 2018 Meningitis Inflammation of the meninges in the brain and spinal cord. Pathophysiology Assessment Bacterial meningitis occurs as an opportunistic infection and is concentrated in the nasopharynx. Transmission occurs by secretion or aerosol contamination. Once the organism is in the blood stream it moves across the blood brain barrier and infiltrates into the CSF. this causes inflammation in the sub arachnoid and pia mater causing ICP and meningeal inflammation. • S: severe headache • T: total loss of consciousness • I: Impaired motor function , nuchal rigidity. • F: funky rash • F: fever Treatments Laboratory Findings: ‣CT/MRI: Detects a shift in brain contents. ‣Lumbar Puncture: Culture is taken of the CSF to test strain and culture and sensitivity of the bacteria. CAUSES ‣ IBacterial : Streptococcus pneumoniae ‣ Viral: Neisseria meningitidis. EDUCATION INTERVENTIONS ‣ Remind the patient about the importance of keeping appointments and screening. ‣ Educate the client on the disease process and how it's transmitted. ‣ Educate the client on treatments and the importance of adhering to the recommended treatment regimens ‣ Finish all antibiotics. ‣ Educate the patient of asepsis and preventing the spread of meningitis. ‣ Institute infection control precautions for 24hrs. ‣ Assist with pain management. ‣ Provide a restful environment. ‣ Administer antipyretics. ‣ Offer a cooling blanket. ‣ Encourage hydration. ‣ Monitor neurologic status. ‣ Monitor vitals. ‣ Initiate seizure precautions ‣ Keep the patient safe. ‣ Monitor daily weights ‣ Monitor electrolytes ‣ Obtain and monitor U/A results ‣ Maintain skin integrity by providing immaculate skin care. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Antibiotic agents that cross the blood brain barrier. ‣ Penicillin G in combination with a cephalosporin : ceftriaxone IV within 30 minutes of hospital arrival. ‣ Dexamethasone: adjunct therapy in acute bacterial meningitis, improves the outcome of adults. Does not cause GI bleeding. ‣ Fluid replacement: treatment for dehydration and shock. With fluid volume expanders. Preventions ‣ Meningitis vaccine. ‣ Treatment of those who have been exposed within 24 hours. ‣ Flu vaccine ‣ Pneumonia vaccine. 23 lOMoARcPSD|11334620 24 MEDICAL SURGICAL NURSING: NEURO 1.9.10 NURSE ANGIE 2018 Multiple Sclerosis A chronic and progressive disease of the CNS that causes demyelination of the neurons. Pathophysiology Assessment Sporadic patches of demyelination occur in the central nervous system, resulting in widespread and varied neurologic dysfunction. Typically progresses slowly; may progress rapidly if diagnosed late, causing death within months. Occurrence is between 20 and 40 years of age. MS is precipitated by a viral infection , pregnancy, immune response, fatigue, stress, trauma, and infection. ‣ ‣ ‣ ‣ W: Weakness E: Electric shock sensations A: Apathy and other mood changes K: Killer pain ‣ V: Vision changes ( diplopia, nystagmus, blurry vision) ‣ I: Incontinence ‣ S: Sensory loss ‣ I: Inability to swallow ‣ O: Optic neuritis ‣ N: Neuralgias Treatments ‣ Symptomatic treatment for acute exacerbations ‣ Plasmapheresis (second-line treatment for exacerbations that won't respond to corticosteroid therapy; not indicated for chronic or secondary progressive multiple sclerosis) ‣ Venous thromboembolism (VTE) prophylaxis Laboratory Findings: Education ‣ Nonpharmacologic pain relief, such as imagery, distraction, transcutaneous electrical nerve stimulation, heat, massage ‣ Physical therapy helps maintain joint mobility and prevent contractures; ‣Magnetic resonance imaging (MRI) of the neurologic system: The most sensitive method of detecting multiple sclerosis focal lesions in the brain and spinal cord. ‣Computed tomography scanning may reveal plaques. ‣Electroencephalography : Abnormalities occur in one-third of patients with multiple sclerosis. ‣Evoked potential studies: Show slowed conduction of nerve impulses. ‣Lumbar puncture with cerebrospinal fluid analysis: Results show mononuclear cell pleocytosis, an elevation in total immunoglobulin (Ig) G levels, and the presence of oligoclonal IgG (used when MRI is inconclusive or unavailable). ‣ Stress management ‣ Ensure safety ‣ Education on treatment regimen ‣ Eye patch for diplopia ‣ Safety related to sensory loss ( no heating pads, monitor water temperature. ‣ High-fluid and high-fiber (for constipation) acute attacks or exacerbations with full recovery and no lasting disability and no worsening of the disease between attacks (approximately 85% of cases) ‣ Primary progressive: Steadily progressing or worsening with minor recovery or plateaus, possibly involving different brain and spinal cord damage from other forms occupational therapy; speech therapy Types ‣ Relapsing-remitting: Clear relapses or CAUSES ‣ Autoimmune response ‣ Viral infection ‣ Genetic factors possibly also involved ‣ Environmental factors INTERVENTIONS (approximately 10% of cases) ‣Secondary progressive: Beginning as a pattern of clear-cut relapses and recovery ‣ Monitor activity and pain but becoming steadily progressive and ‣ Monitor mobility worsening between acute attacks ‣ Monitor medication response (approximately 50% of cases of the ‣ Sensory function relapsing-remitting type change to the ‣ Muscle function secondary progressive type within 10 years ‣ Speech & Elimination ‣ Vision changes of onset) ‣Progressive-relapsing: Steadily ‣ Energy level progressing from onset but also involving clear, acute attacks (less than 5% of cases) 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 24 lOMoARcPSD|11334620 25 MEDICAL SURGICAL NURSING: NEURO 1.9.9 NURSE ANGIE 2018 Myasthenia Gravis A neuromuscular disease that manifests as severe weakness and extreme fatigue of the voluntary muscles. Pathophysiology Assessment Blood cells and the thymus gland produce antibodies that block, destroy, or weaken neuroreceptors that transmit nerve impulses, mainly acetylcholine. The number of acetylcholine receptors in the postsynaptic muscle membrane is decreased, causing failure of transmission of nerve impulses at the neuromuscular junction. CAUSES/COMPLICATIONS ‣ Idiopathic ‣ Congenital ‣ Myasthenia crisis: Acute exacerbation caused by rapid unrecognized progression of the disease, inadequate amount Laboratory Findings: Education ‣ Disease process ‣ Medications ‣ Symptoms are transient ‣ need to avoid strenuous exercise, stress, infection, and unnecessary exposure to the sun or cold weather ‣ swallowing-therapy program ‣ danger signs and symptoms, especially those of myasthenic crisis and cholinergic crisis and the need to report any to the practitioner immediately. Masklike expression Diplopia Decreased breath sounds Ptosis Weakness Trouble swallowing Treatments ‣ Anticholinesterase: pyridostigmine bromide (Mestinon) and neostigmine. ‣ Immunosuppressive drugs: azathioprine (Imuran), cyclosporine (Neoral), cyclophosphamide (Cytoxan), mycophenolate mofetil (CellCept), and tacrolimus ‣ Corticosteroids prednisone ‣ I.V. immune globulin ‣ Stop triggering agents ‣ Plasmapheresis ‣ Emergency airway management of medication, infection, fatigue, or stress. ‣ Anti-acetylcholine receptor antibody: is positive in 80% to 90% of patients ‣ Anti–muscle-specific kinase antibody: 30% to 40% of patients Anti Striated muscle antibody is present. ‣ Muscle-specific tyrosine kinase antibody: Is present in about 40% to 50% of patients with generalized myasthenia gravis and is absent in patients with ocular myasthenia gravis. Tensilon test or endorphin test: Results are positive, showing temporary improved muscle function and confirming the diagnosis. ‣ Ice pack test results: (for patients for whom the Tensilon test is contraindicated) reveal decreased ptosis after ice is applied for 60 seconds to the closed eyelid. ‣ ‣ ‣ ‣ ‣ ‣ Characterized by rapid pulse rate, increased respirations, dyspnea, anoxia, cyanosis, bowel and bladder incontinence, decreased urine output, absent cough and Risk Factors ‣ Systemic lupus erythematosus ‣ Thyrotoxicosis ‣ Autoimmune disorder associated with the thymus gland ‣ immune and thyroid disorders causing secondary symptoms swallow reflex. ‣ Interventions: increase anti INTERVENTIONS cholinesterase medications. ‣ Monitor respiratory status ‣ Monitor for respiratory failure ‣ Maintain patent airway and suctioning. ‣ Thickened liquids ‣ Encourage the client to sit up and eat. ‣ Assess musculoskeletal status. ‣ Plan short activities during periods when the patient has the most strength. ‣ Monitor for myasthenic and cholinergic crisis. IMPORTANT ‣ Cholinergic crisis: Depolarization of motor end plates. Characterized by abdominal cramps, nausea, vomiting, diarrhea, blurred vision, pallor, facial muscle Monitor the patient for signs of impending myasthenic crisis, including increased muscle weakness, respiratory distress, and difficulty talking or chewing. twitching, hypotension, pupillary miosis. ‣ Interventions: Withhold anticholinesterase medications, prepare to administer antidote if ordered 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 25 lOMoARcPSD|11334620 26 MEDICAL SURGICAL NURSING: NEURO 1.9.7 NURSE ANGIE 2018 Parkinson’s Disease A slow progressive neurological disease that results in disability and long term self care deficits. Pathophysiology Assessment S: Slow movements A degenerative disease resulting from a depletion of dopamine and an imbalance of acetylcholine which interferes in with the inhibition of excitatory impulses, thus causing the patient to shake and tremor uncontrollably. The debilitation can cause self care deficits, falls, failure of body systems. Later as the disorder progresses mental deterioration can occur. GOALS ‣ Improving functional mobility ‣ Maintaining independence ‣ Maintaining acceptable nutritional status ‣ Achieving adequate bowel elimination ‣ Achieving effective communication ‣ Develop positive coping mechanism H: Hypotension A: Akinesia K: Kinesis ( Brady) Y:Yes they walk with forward flexion M: Mask like expression A: Agitation N: Not steady, tremors when at rest Treatments ‣ PNo treatment cures the disorder. ‣ Treatment is individualized. ‣ Antiparkinsonian drugs: increase dopamine and reduce acetylcholine. ‣ Levodopa: Converted to dopamine in the basal ganglia. Laboratory Findings: ‣ PET scans INTERVENTIONS ‣ Assess neuro status ‣ Assess ability to swallow ‣ Provide high calorie, high protein, high fiber, soft diet. ‣ Increase fluid intake to 2000 mL/day ‣ Monitor for constipation ‣ Promote independence and avoid rushing the patient ‣ Promote safety ‣ Encourage the use of assistive devices. Help with ambulation. ‣ Promote physical therapy and rehabilitation. ‣ Position on a firm mattress, prone without a pillow. ‣ Avoid foods high in VIT B, they reduce the effects of antiparkinsonian drugs. ‣ Administer antiparkinsonian drugs as ordered. ‣ Use caution with MAOIs they may cause hypertensive crisis. See agency protocol. CAUSES ‣ Depletion of dopamine, ‣ Early diagnosis is rare because patients can rarely pinpoint when symptoms started. dopamine-generating cells, known as dopaminergic neurons (types of nerve Education ‣ possible adverse effects of such medications as levodopa carbidopa or bromocriptine ‣ measures to prevent pressure injury and contractures ‣ promote activity and participation in self-care; importance therapy ‣ household safety measures dietary recommendations, including the need for adequate fiber and fluid intake ‣ methods to improve communication ‣ swallowing therapy regimen (aspiration precautions) cells) in the substantia nigra part of the brain have died. Experts do not know why these cells die. Complications ‣ Injury from falls, Aspiration ‣ Urinary tract infections Skin breakdown, Pneumonia Anxiety, Depression, psychosis Dementia, Constipation Sleep problems, sensory issues ‣ Pain 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Levodopa is the post effective treatment for parkinson's. ‣Antiviral agents: Reduce rigidity, tremors, bradykinesia, and postural changes ‣Dopamine Agonists: Secondary to carbidopa/levodopa for early stages. ‣MAOI: Inhibit dopamine breakdown ‣Catechol-O-Methyltransferase inhibitor: increases action of carbidopa or levodopa, reduces motor fluctuations in advanced parkinson's. ‣Tricyclic antidepressants/SSRI : Anticholinergic and antidepressant ‣Antihistamines: may reduce tremors. 26 lOMoARcPSD|11334620 27 MEDICAL SURGICAL NURSING: NEURO 1.9. 10 NURSE ANGIE 2018 Spinal Cord Injury Trauma to the spine that results in full or partial severance, this leads to loss of mobility Emergency management Pathophysiology • Always suspect spinal injury when trauma occurs • Assess and maintain a patent Trauma to the spinal cord causes disruption of the nerve tracts and neurons. A spinal cord injury can result in edema, total or partial severance of the cord causing paralysis. Common affected vertebrae • Cervical : C5-C7 • Thoracic: T 12 • Lumbar: L 1 airway and assess respirations. • Prevent head flexion, extension or rotation. • Log-roll the client. • Never twist or turn the client. • Do not allow them to sit. • In the emergency department, place the patient immediately in skeletal traction. To reduce fracture and dislocation. ! Assessment •Cervical: injury at C2 or C3 is fatal, injury above C4 causes respiratory difficulty and paralysis in all extremities. Client may move shoulder and have decreased respiratory reserve with injury to C5-C8. •Thoracic: Loss of movement in the trunk, chest, bowel, bladder and legs. Paraplegia may occur, autonomic dysreflexia in injuries above T6. Distended bladder or impacted rectum, bradycardia, hypertension and goosebumps. • Lumbar: Loss of movement or sensation in the lower extremities, injury to S2 or S3 can cause neurogenic bladder. Injury above S2 in males enables them to still experience erection but not ejaculate due to sympathetic nerve damage. Injury at S2-S4 will result in inability to obtain an erection or ejaculate. Types INTERVENTIONS FOR AUTONOMIC DYSREFLEXIA • Raise the head of the bed • Loosen tight clothes • Administer antihypertensives • Document occurrence treatment and response. Autonomic dysreflexia: • • • • • Severe hypertension bradycardia severe headache nasal stuffiness and flushness. SYNDROMES INTERVENTIONS • Immediately stabilize the spine • Assess neuro function • Assess respiratory function every Central cord syndrome: Is a result of a lesion on the central portion of the spinal cord. Motor function loss is apparent in the upper extremities, some sensation remains intact. Anterior syndrome: Results from injury to the anterior portion of gray and white matter. Motor function, pain sensation and temperature are lost below the area of injury. Posterior Syndrome: Results from damage to the posterior portion of the gray and white matter in the spinal cord. Motor function remains intact, but the patient will experience a loss of sense of vibration , crude touch, and position sensation. Brown-Sequard syndrome: Is a result of a penetrating injury that cause injury to half the cord. Sensation, temperature and pain are affected on the opposite side of hour • Monitor secretions and breath sounds • Monitor 02 saturation • Assess cardiovascular function every hour • Monitor blood pressure • If there is a pulmonary catheter in • • • • • • • the injury. 1 monitor inform the HCP of a decrease in right atrial pressure, pulmonary artery pressure, systemic vascular resistance, or pulmonary wedge pressure as this could indicate neurogenic shock Monitor GI status Monitor intake and output Avoid uriniary retention to avoid autonomic dysreflexia Monitor for dvt Frequent skin assessments Begin rehab as soon as possible Provide emotional support Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣Transection of the cord: Complete severance of the spinal cord, results in total loss of sensation, movement, and reflexes. ‣Partial Transection : The cord is partially severed, symptoms depend on the extent of the damage, early treatment may result in avoidance of permanent damage. Complications • Respiratory failure • Death • Autonomic dysreflexia • Spinal shock • Extensive cord damage Effects • Tetraplegia: Injury between C1 and C2. paralysis involving all extremities. • Paraplegia: Injury between T1 and L4 paralysis only involving lower extremities. 27 lOMoARcPSD|11334620 28 MEDICAL SURGICAL NURSING: NEURO 1.9.6 NURSE ANGIE 2018 Stroke Sudden loss of neurological function caused by cerebrovascular disease. CAUSES Pathophysiology ‣ Thrombosis ‣ Embolism A stroke can be caused by an embolus in the peripheral vasculature that breaks off and makes its way into the cerebral vessels causing a blockage. This blockage causes cerebral ischemia which leads to the death of cerebral cells and tissues causing paralysis, weakness, impaired speech and possibly death. ‣ Hemorrhage: Intracranial or Subarachnoid •D: Drooping of the face •E: Extra high BP • A: Apraxia • D: Dysarthria RISK FACTORS ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Maintain a patent airway. Position. Monitor elimination patterns Provide skin care. Perform passive/Active ROM. Move extremities that have been affected slowly. ‣ Teach the use of supportive device ( cane, walker, commode) ‣ Address communication needs. ‣ Orient client to person, place and time. Smoking Advanced age Hypertension, Stress TIA’s Diabetes, Obesity High Cholesterol Oral contraceptives Atherosclerosis Anticoagulant therapy Assessment of cranial nerves •V: Difficulty chewing. •VII: Facial paralysis or paresis •IX: Absent gag reflex •IX & X: Dysphagia •XII: Impaired tongue movement Criteria for t-PA admin ‣18 yrs old ‣Clinical diagnoses of ischemic stroke ‣ Time of onset of stroke under 3 hours ‣BP less than 185/110 mmHg ‣Not a minor or rapid resolving stroke ‣No seizure at onset of stroke Maintain a patent airway ‣Not on warfarin Administer TpA within 6 hrs of ‣Prothrombin < 15 seconds symptom onset, and not for ‣Not on heparin within the past hemorrhagic stroke if indicated to 48 hrs. break up a thrombus. ‣Platelet count > 10,000/mm3 Administer 02 as prescribed ‣No prior aneurysm, hemorrhage, Monitor Vitals or neoplasm Maintain BP of 150/100 mmHg to ‣No major surgery in the last 14 maintain cerebral perfusion. days. Suction secretions as ordered. No ‣No stroke within 3 months longer than 10 seconds to prevent ‣No GI or GU bleeding within 3 ICP. months. Monitor for increased ICP the ‣Dosage : 0.9mg/ kg not to highest risk for ICP is within the exceed 90mg. Given IV 10% as a first 72 hours. bolus over 1 min. The remaining Position the client on the side with IV over 1 hour pump. the head of the bed elevated 15-30 degrees. Monitor LOC, PERRLA. Insert foley Administer IV fluid. PRIORITY INTERVENTIONS CT scan Electroencephalography Cerebral arteriography MRI. NURSING INTERVENTIONS POST ACUTE PHASE Assessment •B: Bothered field of vision •R: Respiratory changes •A: Agnosia •I: Instant LOC changes •N: Not able to speak clearly ‣ ‣ EDUCATION ‣ Remind the patient about the importance of keeping appointments and screening. ‣ Educate the client on the disease process and how it's transmitted. ‣ Educate the client on treatments and the importance of adhering to the recommended treatment regimens ‣ Finish all antibiotics. ‣ Educate the patient of asepsis and preventing the spread of meningitis. ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 28 lOMoARcPSD|11334620 29 MEDICAL SURGICAL NURSING: NEURO 1.9.11 NURSE ANGIE 2018 Trigeminal Neuralgia A sensory disorder that affects the 5th cranial nerve. Risk Factors Pathophysiology The trigeminal nerve has multiple branches. This nerve affects movements and sensations of the face, scalp, and teeth. Compression of the nerve root occurs from an unknown cause. Demyelination occurs in the area of the compression. An impulse triggers the area, and interaction or short-circuiting of touch and pain fibers occurs. Paroxysmal attacks causing excruciating facial pain ‣ ‣ ‣ ‣ ‣ ‣ Herpes zoster History of multiple sclerosis Age over 50 years Disorder of blood vessels Female gender Arteriovenous malformation Complications ‣ weight loss ‣ Depression Social isolation Paresthesia ‣ loss of corneal reflex Assessment ‣ ‣ ‣ ‣ P: Pain on the lips, face & gums A: Along the trigeminal nerve I : Initiated by light touch N: No impairment of sensory or motor function ‣ E: Exacerbated by extreme temperatures ‣ D: Does Not shave or chew on the affected side ‣ ‣ F: Favors the affected side, splinting the affected side ‣ A: A Draft or cold air can aggravate it ‣ C: Cold drinks and food can aggravate ‣ E: Eating, smiling, talking, and brushing teeth can exacerbate the pain. Treatments ‣ Anticonvulsants: Carbamazepine (Tegretol) or oxcarbazepine, as a first-line agent and phenytoin, gabapentin, lamotrigine, or valproic acid as a second-line agent; tizanidine hydrochloride as alternative agent ‣ Skeletal muscle relaxants: Baclofen, Laboratory Findings: as an adjunct to phenytoin or ‣ Skull radiography, computed tomography scanning (brain), and magnetic resonance imaging rule out sinus or tooth infections and tumors. carbamazepine ‣ Antidepressants: Amitriptyline hydrochloride, fluoxetine hydrochloride, or trazodone Education CAUSES ‣ Instruct the client to avoid hot or cold food. ‣ Small frequent feedings of ‣ Compression of the nerve root by: Middle fossa tumors, posterior fossa tumors, vascular lesions ‣ Afferent reflex phenomenon soft food. ‣ Instruct client to chew food hydrochloride, in conjunction with an INTERVENTIONS on unaffected side. ‣ Frequency of attacks ‣ effectiveness of medications ‣ Microvascular decompression ‣ Monitor CBC with tegratol ‣ Monitor post OP neuro compresses the trigeminal nerve. ‣ Radiofrequency waveforms: Creates function ‣ Administer anticonvulsants as ‣ Obtain informed consent for ordered. surgery ‣ Prepare for microvascular ‣ Focused pain assessments ‣ Wound assessment decompression surgery if indicated. anticonvulsant ‣ Topical capsaicin cream surgery: Relocates the artery that lesions that provide pain relief. ‣ Rhizotomy: Resection of the trigeminal nerve root. ‣ Glycerol injection: Destroys the myelinated fibers of the trigeminal nerve root. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 29 lOMoARcPSD|11334620 30 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.4 NURSE ANGIE 2018 Tuberculosis A highly contagious communicable disease caused by mycobacterium tuberculosis. Pathophysiology Assessment Multiplication of the bacillus Mycobacterium tuberculosis causes an inflammatory process where deposited. A cell-mediated immune response follows, usually containing the infection in 2 to 8 weeks. The T-cell response results in the formation of granulomas around the bacilli, making them dormant. This confers immunity to subsequent infection. Bacilli within granulomas may remain viable for many years, resulting in a positive purified protein derivative or other skin test for TB. Transmission occurs via airborne droplet nuclei when a person with active disease coughs or sneezes. Complications Massive pulmonary tissue damage Respiratory failure Bronchopleural fistulas Bronchiectasis Hemoptysis Pneumothorax Pleural effusion Pneumonia Infection of other body organs by small mycobacterial foci ‣ Liver involvement disease secondary to drug therapy ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ INTERVENTIONS ‣ Tuberculin skin test result is positive in active and inactive (latent) TB. ‣ T-SPOT TB test identifies interferon-gamma response to specific Mycobacterium tuberculosis proteins to detect infection. ‣ QuantiFERON-TB gold test or interferon gamma release assay detects latent TB infection. ‣ Stains and cultures of sputum, cerebrospinal fluid, urine, abscess drainage, or pleural fluid show heat-sensitive, nonmotile, aerobic, acid-fast bacilli. ‣ Chest radiography shows nodular lesions, patchy infiltrates, cavity formation, scar tissue, and calcium deposits; may be normal in primary infection. ‣ Exposure to M. tuberculosis ‣ Exposure to other strains of mycobacteria called mycobacteria other than tuberculosis (MOTT) N: not able to sleep I: intense chest pain G: gross sputum( bloody) H: history of influenza T: travel to TB prevalent areas ‣ S: sweats at night ‣ W: weight loss ‣E: extra effort to breathe ‣A: anorexia ‣T: tightness in chest Medical Treatment ‣ First-line drugs: Antitubercular therapy for at least 6-9 months isoniazid ( isonicotinic acid hydrazide) (Isotamine), rifampin (rifampicin) (Rifadin), and pyrazinamide,plus ethambutol hydrochloride (Myambutol) or streptomycin in some cases ‣ Second-line drugs: Laboratory Findings: CAUSES ‣ ‣ ‣ ‣ ‣ ‣ Isolate the patient in a quiet, properly ventilated room. ‣ Institute airborne precautions for pulmonary TB until the patient has at least three consecutive negative sputum cultures ‣ Properly dispose of secretions; encourage respiratory hygiene measures. ‣ Provide adequate rest periods. Cluster activities to provide for adequate rest. ‣ Provide well-balanced, high-calorie foods & foods high in iron, vitamin c and protein. ‣ Provide small, frequent meals. ‣ Perform chest physiotherapy. Encourage frequent coughing and deep-breathing exercises. ‣ Obtain specimens for laboratory testing, such as sputum cultures, as indicated. ‣ Notify the local health department if required by state regulations. EDUCATION ‣ Take all of your medications ‣ Wear proper PPE ‣ Appropriate infection control precautions. ‣ Coughing and deep breathing exercises ‣ Follow up ‣ TB medications can reduce the effectiveness of birth control ‣ High calorie, high protein diet 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ➢ Capreomycin (Capastat Sulfate) ➢ Streptomycin ➢ Ethionamide (Trecator) ➢ Aminosalicylic acid (paraaminosalicylic acid [Parasol]) ➢ Pyrazinamide ➢ Cycloserine (Seromycin) ‣ Alternative agents: levofloxacin (Levaquin), moxifloxacin hydrochloride(oral; injection) (Avelox), linezolid (Zyvox), or meropenem-clavulanate for treatment of multidrug or highly drug-resistant TB 30 lOMoARcPSD|11334620 31 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.12 NURSE ANGIE 2018 Pleural Effusion Fluid accumulation between the visceral and parietal pleura of the lung Pathophysiology Assessment Fluid and other blood components migrate through the walls of intact capillaries bordering the pleura. Classified as transudative or exudative Usually unilateral but can be bilateral (usually due to heart failure, kidney failure, liver failure, or malignant neoplasms). ‣ Shortness of breath, chest pain; referred abdominal or shoulder pain, malaise, cough, productive or nonproductive, weight loss, night sweats, fever, trachea, mediastinum, or both deviating from the affected side . Dullness and decreased tactile fremitus over the effusion, diminished or absent breath sounds, tachypnea, bronchial breathing or egophony, hemoptysis, pleural friction rub, bronchial breath sounds, peripheral edema, distended neck veins, and S3 gallop (suggesting heart failure) foul-smelling sputum (empyema) Medical Treatment ‣Thoracentesis to remove fluid CAUSES Laboratory Findings: ‣ Pleural fluid analysis findings: May show empyema, elevated WBC, elevated amylase or lipase if related to pancreatitis, elevated protein. ‣ Chest radiography may show pleural effusions; lateral decubitus films may show loculated pleural effusions or small pleural effusions not visible on standard chest radiography. ‣ Computed tomography scanning (thorax) shows pleural effusions. ‣ Transthoracic ultrasonography reveals the amount and level of fluid accumulation. ‣ Pleural biopsy may be positive for carcinoma. SURGICAL PROCEDURES ‣ Tube thoracostomy ‣ Pleuroperitoneal shunts (rare; for ‣ recurrent effusions) ‣ Pleurodesis—chemical or mechanical ‣ sclerosing agents under VATS ‣ Pleurectomy—radical total or subtotal ‣ and decortication for malignant ‣ effusions ‣ Insertion of long-term tunneled ‣ indwelling pleural catheter to allow for outpatient management with recurrent INTERVENTIONS ‣ Monitoring Vitals ‣ Coping ‣ Administer prescribed drugs and I.V. fluids, initiate I.V. access, and maintain I.V. patency. Provide I.V. site care ‣ Give supplemental oxygen based on oxygen saturation levels and arterial blood gas results. ‣ Elevate the head of the bed at least 30 degrees ‣ Assist the patient with relaxation measures to reduce oxygen demand ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Empyema Infected wound Intra-abdominal infection Lung abscess Pulmonary infection Thoracic surgery Malignancy Connective tissue diseases Transudative Pleural Effusion Cardiovascular disease Hepatic disease Hypoproteinemia Renal disease Exudative Pleural Effusion Pleural infection Pleural inflammation Pleural malignancy (most often occurring with lung or breast cancer) Pneumonia Pulmonary embolism Pancreatitis Trauma Drug use Tuberculosis Asbestos exposure 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣Possible chest tube insertion ‣Possible chemical pleurodesis ‣Intrapleural fibrinolytic agents in limited cases ‣Treatment of underlying condition ‣Antimicrobial therapy,: ampicillin sodium imipenem–cilastatin sodium clindamycin phosphate (injection)(Cleocin Phosphate), or piperacillin sodium–tazobactam sodium (Zosyn), doxycycline (Vibramycin), bleomycin sulfate, or talc for chemical pleurodesis to treat recurrent pleural effusions ‣Chemotherapy for malignancy ‣Corticosteroids and nonsteroidal anti-inflammatory drugs for effusions due to rheumatologic or inflammatory causes ‣ Diuretics, such as furosemide (Lasix), for effusions resulting from heart failure and ascites ‣Oxygen ‣I.V. fluid therapy 31 lOMoARcPSD|11334620 32 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.8 NURSE ANGIE 2018 S.A.R.S Severe form of alveolar injury or acute lung injury Assessment Pathophysiology Coronaviruses cause diseases in pigs, birds, and other animals. A theory suggests that a coronavirus may have mutated, allowing transmission to and infection of humans. Mucous membranes come in direct or indirect contact with infectious respiratory droplets or fomites. The virus attaches itself to human receptor cells, initiating a nonspecific acute lung injury. The result is diffuse severe alveolar damage. Risk Factors ‣ Close contact with aerosolized (exhaled) droplets and bodily secretions from an infected person ‣ Travel to endemic areas ‣ O:out of the country ‣ U:underdeveloped countries ‣ T: travel to endemic areas ‣ O: out of breath ‣ F: fever, fatigue ‣ B: bad muscle aches ‣ R: rhinorrhea/ respiratory distress ‣ E: excess vomiting ‣ A: A sore throat ‣ T: tachypnea ‣ H: headache Medical Treatment Complications Laboratory Findings: ‣ Respiratory difficulties ‣ Severe thrombocytopenia (low platelet count) ‣ Heart failure ‣ Liver failure ‣ Death ‣ Arterial blood gas (ABG) analysis initially shows hypoxemia and respiratory alkalosis ‣ ABG analysis later showed respiratory acidosis ‣ B-type natriuretic peptide assay result of less than 100 pg/mL suggests ARDS. ‣ Gram stain and sputum culture and sensitivity show infectious organisms. ‣ Leukopenia or leukocytosis may be present in patients with sepsis. ‣ Blood culture reveals infectious organisms. ‣ Chest radiography show early bilateral infiltrates ‣ ‣ INTERVENTIONS CAUSES ‣ Coronavirus known as SARSassociated coronavirus (SARS-CoV Education ‣ ‣ ‣ ‣ ‣ Monitor respiratory status. Administer 02 Trach care if indicated Conservative fluid management Tube feedings or parenteral nutrition as indicated ‣ Bed rest with frequent turning and position changes ‣ Elevation of the head of the bed to 45 degrees importance of frequent hand washing importance of covering the mouth and nose when coughing or sneezing avoiding close personal contact with friends and family Report condition to CDC 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Treatment of the underlying cause ‣ Correction of electrolyte and acid-base imbalances ‣ Mechanical ventilation ‣ Vasopressors if the patient is hypotensive ‣ Antimicrobials if nonviral infection is identified ‣ Inotropic agents ‣ Inhaled vasodilators ‣ Anxiolytics : lorazepam (Ativan) ‣ Anti embolic ‣ Bronchodilators ‣ Paralyzing agents ‣Sodium bicarbonate ‣Sedatives ‣Opioids ‣Neuromuscular blocking agents ‣Fluids and vasopressors if hypotensive ‣ Antimicrobials if nonviral infection is identified ‣Prone positioning to help with perfusion of the lungs 32 lOMoARcPSD|11334620 33 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.6 NURSE ANGIE 2018 COPD: Chronic Bronchitis Progressive respiratory disease characterized by airflow limitation that is progressive, not preventable, and not fully reversible. Assessment Pathophysiology Changes associated with chronic bronchitis include hypertrophy and hyperplasia of the bronchial mucous glands, increased goblet cells, ciliary damage, squamous metaplasia of the columnar epithelium, and chronic leukocytic and lymphocytic infiltration of bronchial walls. Widespread inflammation occurs, leading to airway narrowing and mucus within the airways. Producing resistance in the small airways and, consequently, a severe ventilation-perfusion imbalance. ‣ Increased respiratory rate ‣ Increased hemoglobin ‣ Decreased breath sounds, wheezes, crackles at the lung bases ‣ Increased anteroposterior diameter of the chest. Clubbing of the nails. ‣ Acidosis, Hypoxia ‣ Hypercapnia, Tripod position to assist in breathing, Full use of the accessory respiratory muscles of the neck and shoulders, Pursedlips expiration, Hoover sign (paradoxical retraction of the lower interspaces during inspiration), Cyanosis. ‣ Asterixis due to severe hypercapnia. Neck vein distention (especially during expiration). ‣ Coughing and sputum production. Medical Treatment Laboratory Findings: ‣ Arterial blood gas analysis may reveal: mild or moderate hypoxemia without hypercapnia in patients with mild COPD, and with hypercapnia when the disease progresses and the hypoxemia becomes more severe.. ‣ Hemoglobin level test shows an increased hemoglobin level late in the disease ‣ Pulmonary function tests show increased residual volume, increased total lung capacity, and decreased diffusion capacity as well as decreased vital capacity, decreased forced expiratory flow, normal static compliance, and normal diffusing capacity. CAUSES ‣ Tobacco smoking ‣ ‣ ‣ Occupational exposure to dusts and chemicals ‣ Indoor and outdoor air pollution, including the use of biomass fuel for heating and cooking ‣ Antiprotease deficiency (rare inherited disorder known as alpha-1-antitrypsin deficiency Education INTERVENTIONS ‣ ‣ ‣ ‣ Monitor airway. Provide 02 as ordered Clear secretions. Provide a high-calorie, protein-rich diet to ensure adequate nutritional status; offer small, frequent meals to minimize energy expenditure. Ensure adequate oral fluid intake to maintain hydration and help mobilize secretions. Auscultate lungs for evidence of adventitious breath sounds. Elevate the head of the bed to ease the work of breathing. Coughing and Deep breathing exercises Chest physiotherapy Energy conservation Avoid triggers Obtain vaccinations Importance of balanced high protein diet Maintain adequate nutrition and hydration Perform chest physiotherapy to help mobilize and remove secretions; 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Influenza vaccine yearly; pneumococcal vaccine at diagnosis and again in 5 years if first vaccine at < age 65 ‣ Short-acting bronchodilators: Anticholinergics (such as ipratropium bromide[Atrovent]) or beta-adrenergic agonists (such as albuterol sulfate [Ventolin HFA]). ‣ Long-acting bronchodilators: Anticholinergics (such as tiotropium bromide [Spiriva]) and long-acting beta-adrenergic agonists (such as salmeterol . ‣ Inhaled glucocorticosteroids (Flovent) for repeated exacerbations ‣ long-term oxygen therapy ‣ Theophylline (Theolair) ‣ Combination of inhaled corticosteroids, long-acting betaadrenergic agonists, and anticholinergics for severe disease ‣ Low-dose macrolides (clarithromycin [Biaxin] or erythromycin) to decrease inflammation ‣ Mucolytic agents to improve secretions but not outcomes ‣ Systemic glucocorticosteroids for 5 to 10 days 33 lOMoARcPSD|11334620 34 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.5 NURSE ANGIE 2018 Asthma Airway inflammation, intermittent airflow obstruction, and bronchial hyper-responsiveness Pathophysiology Chronic inflammation of the airways that causes varying degrees of obstruction. Marked by inflammation and hyper-responsiveness to a variety of stimuli “triggers”. Once a trigger has been met the patient may wheeze, feel breathlessness, may feel tight chested and may cough , this is associated with airway obstruction. Complications ‣ Acute, severe asthma (formerly known as status asthmaticus) ‣ Respiratory failure ‣ Pneumonia ‣ Atelectasis ‣ Air-leak syndrome (such as pneumothorax) ‣ Death Assessment ‣ C: chest tightness ‣ L: long exhalation ‣O: obstructed airway ‣S: sounds wheezy ‣E: expiratory wheezes ‣D: diminished breath sounds ‣ ‣ ‣ ‣ ‣ ‣ T: tachycardia H: has lots of sweat R: restlessness O: oh he’s blue A: altered mental status T : tachypnea Medical Treatment Laboratory Findings: ‣ Arterial blood gas analysis (ABG) provides the best indication of an attack's severity and may reveal hypoxemia during an acute attack. A normal Paco2 during an acute attack may be a sign of impending respiratory failure. ‣ Complete blood count with white blood cell count and differential shows increased eosinophil count in acute phases. ‣ Pulmonary function tests commonly show decreased peak flow rates and forced expiratory volume in 1 second, low-normal or decreased vital capacity, and increased total lung and residual capacities. However, pulmonary function tests may be normal between attacks. ‣ Skin testing may identify specific allergens. ‣ Pulse oximetry measurements may show decreased oxygen saturation. ‣ Peak flow monitoring reveals a result of less than 80% of personal best; a reading below 50% of personal best indicates a severe exacerbation. CAUSES ‣ Sensitivity to specific external allergens (leading cause) ‣ Internal, nonallergenic factors, such as genetic factors and stress EDUCATION INTERVENTIONS ‣ ‣ ‣ ‣ ‣ Educate on the need for long term management ‣ Identify triggers and have the patient avoid them. ‣ Educate on medication regimen. ‣ Educate on the correct use of a peak flow meter. Maintain patient airway Monitor pulse ox Monitor vitals Monitor peak flow 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Quick-relief bronchodilators,: albuterol sulfate ‣ Quick-relief anticholinergics: ipratropium bromid for relief of bronchospasm ‣ Corticosteroids: methylPREDNISolone, prednisoLONE, and prednisone, to prevent exacerbation during moderate or severe exacerbations ‣ Corticosteroids for persistent asthma : an inhaled corticosteroid of fluticasone furoate, beclomethasone dipropionate, budesonide, or mometasone ‣ Long-acting beta-agonist or combination drug: salmeterol xinafoate inhaler, formoterol, fluticasone furoate/ salmeterol xinafoate inhaled or budesonideformoterol fumarate dihydrate (Symbicort) ‣ Leukotriene antagonists (antileukotrienes): montelukast sodium(Singulair) ‣ Anticholinergic bronchodilators : tiotropium bromide inhaled (Spiriva) 34 lOMoARcPSD|11334620 35 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.7 NURSE ANGIE 2018 COPD: EMPHYSEMA The destruction of alveoli Assessment Pathophysiology ‣ Increased respiratory rate Changes associated with emphysema include recurrent inflammation associated with the release of proteolytic enzymes from lung cells that causes abnormal, irreversible enlargement of the air spaces distal to the terminal bronchioles.The amount of alveolar surface area available for gas exchange decreases. This enlargement leads to the destruction of alveolar walls in the distal or terminal airways, which results in a breakdown of elasticity. Elastic recoil is reduced, limiting airflow. Supporting ‣ Increased hemoglobin ‣ Decreased breath sounds, wheezes, crackles at the lung bases ‣ Increased anteroposterior diameter of the chest. Clubbing of the nails. ‣ Acidosis, hypoxia ‣ Hypercapnia, tripod position to assist in breathing, full use of the accessory respiratory muscles of the neck and shoulders, pursed-lips expiration, hoover sign, cyanosis. ‣ Asterixis due to severe hypercapnia ‣ Neck vein distention ‣ Coughing and sputum production. Medical Treatment Laboratory Findings: ‣Arterial blood gas analysis may reveal: mild or moderate hypoxemia without hypercapnia in patients with mild COPD, and with hypercapnia when the disease progresses and the hypoxemia becomes more severe.. ‣ Hemoglobin level test shows an increased hemoglobin level late in the disease ‣ Sputum culture may reveal the number of microorganisms and neutrophils.. ‣ Pulmonary function tests show increased residual volume, increased total lung capacity, and decreased diffusion capacity as well as decreased vital capacity, decreased forced expiratory flow ‣ Influenza vaccine yearly ‣ Short-acting bronchodilators: Anticholinergics ‣ Long-acting bronchodilators: Anticholinergics and long acting beta-adrenergic agonists (such as salmeterol . ‣ Inhaled glucocorticosteroids for repeated exacerbations ‣ Long-term oxygen therapy ‣ Theophylline (Theolair) ‣ Combination of inhaled INTERVENTIONS CAUSES ‣ Tobacco smoking ‣ ‣ Occupational exposure to dusts and chemicals ‣ ‣ ‣ Indoor and outdoor air pollution, including the use of biomass fuel for heating and cooking ‣ ‣ Antiprotease deficiency (rare inherited disorder known as alpha-1-antitrypsin deficiency) ‣ EDUCATION Monitor airway. Provide 02 as ordered. Clear secretions Provide a high-calorie, protein-rich diet. Ensure adequate oral fluid intake to ‣ Pursed lip breathing ‣ Use of incentive spirometer ‣ Eat frequent small meals corticosteroids, long-acting beta-adrenergic agonists, and anticholinergics for severe disease ‣ Low-dose macrolides, maintain hydration and help mobilize secretions. clarithromycin ‣ Mucolytic agents to improve Auscultate lungs for evidence of adventitious breath sounds. Elevate the head of the bed to ease secretions but not outcomes ‣ Systemic glucocorticosteroids for 5 to 10 days the work of breathing. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 35 lOMoARcPSD|11334620 36 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.1 NURSE ANGIE 2018 INFLUENZA Known as the “FLU” , a highly contagious acute viral respiratory infection. Pathophysiology Assessment Virus invades the epithelium of the respiratory tract, causing inflammation and desquamation. After attaching to the host cell, viral ribonucleic acid enters the cell and uses host components to replicate its genetic material and protein, which are then assembled into new virus particles. Newly produced viruses burst out to invade other healthy cells. Viral invasion destroys host cells, impairing respiratory defenses (especially the mucociliary transport system) and predisposing the patient to secondary bacterial infection. Usually, recent exposure (typically within 48 hours) to a person with influenza, No influenza vaccine received during the past season CNS: Headache MISC: Malaise, Fatigue, listlessness, weakness, Fever, Warm, hot skin, Red, watery eyes; clear nasal discharge, Erythema of the nose and throat without exudate MS: Myalgia, Pain with eye movement Fatigue, listlessness, weakness RESP: Sore throat, Nonproductive cough, Tachypnea, dyspnea, cyanosis Cardio: Tachycardia Medical Treatment Laboratory Findings: ‣ Immunodiagnostic techniques show viral antigens in tissue culture or in exfoliated nasopharyngeal cells obtained by washings. ‣ White blood cell (WBC) count is elevated in secondary bacterial infection. ‣ White blood cell count and differential are decreased in overwhelming viral or bacterial infection. ‣ Rapid influenza antigen tests are positive for the type of influenza (A or B). ‣ Chest radiography rules out pneumonia. CAUSES ‣ Infection by the orthomyxovirus, which is transmitted by inhaling a respiratory droplet from an infected person or by indirect contact (such as drinking from a contaminated glass) INTERVENTIONS EDUCATION Encourage rest Encourage fluid intake Monitor lung sounds Administer medications as prescribed ‣ Institute droplet precautions ‣ Hand washing ‣ Cover your mouth when you cough ‣ Influenza is a virus and isn’t cured with antibiotics. ‣ Drink fluids ‣ ‣ ‣ ‣ 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ TAntipyretics: acetaminophen (Tylenol), or nonsteroidal antiinflammatory drugs (NSAIDs) such as ibuprofen (Advil) ‣ Guaifenesin (Robitussin) or expectorant ‣ Antivirals: oseltamivir phosphate (Tamiflu) or zanamivir (Relenza Diskhaler) as precautionary medications to family members and others not vaccinated and who have been exposed by the infected even if they are not showing signs or symptoms ‣ Influenza virus vaccine (for prevention) ‣ Antibiotics for secondary bacterial infections such as bacterial pneumonia, otitis media, or sinusitis 36 lOMoARcPSD|11334620 37 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.2 NURSE ANGIE 2018 Pneumonia Infection of the pulmonary tissue including the interstitial spaces, alveoli and bronchioles. Pathophysiology Assessment The pulmonary tissue becomes infected causing edema which stiffens the lungs and decreases lung compliance and vital capacity, this also causes hypoxemia. Pneumonia can be community acquired or hospital acquired. ‣ NEURO: Chills & Fever, Loc changes ‣ RESP: Tachypnea , pleuritic pain, rhonchi, wheezes, use of accessory muscles to breathe, sputum production. CAUSES Aspiration pneumonia ‣ Caustic substance entering the airway from either vomiting or impaired swallowing Bacterial and viral pneumonia ‣ Abdominal and thoracic surgery ‣ Alcoholism ‣ Aspiration ‣ Atelectasis ‣ Bacterial or viral respiratory infections ‣ Cancer ‣ Chronic illness and debilitation ‣ Chronic respiratory disease ‣ Endotracheal intubation or mechanical ventilation ‣ Exposure to noxious gases ‣ Immunosuppressive therapy ‣ Influenza ‣ Malnutrition ‣ Sickle cell disease ‣ Tracheostomy Medical Treatment INTERVENTIONS viral pneumonia; ribavirin Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ White blood cell count and differential identifies leukocytosis. Blood culture tests are positive for the causative organism. Arterial blood gas analysis (ABG) values may show hypoxemia. Fungal or acid-fast bacilli cultures identify the etiologic agent. Assay for Legionella-soluble antigen in urine detects the presence of the antigen. Sputum culture, Gram stain, and smear reveal the infecting organism. Rapid antigen testing reveals the causative organism. ‣ Turn cough deep breath Chest radiography generally shows patchy, interstitial, or ‣ Incentive spirometer as lobar infiltrates (bilateral with ordered viral pneumonia; unilateral with bacterial pneumonia). ‣ Increase fluids Bronchoscopy or transtracheal ‣ Take medications as aspiration specimens identify the etiologic agent. prescribed ‣ EDUCATION ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Airway maintenance Monitor vitals and Spo2 Institute incentive spirometry. Monitor color, amount and consistency of sputum. Mechanical ventilation with low tidal volumes (6 mL/kg) and positive endexpiratory pressure for respiratory failure Chest physiotherapy Swallow evaluation if cause is aspiration Venous thromboembolism (VTE) prophylaxis, if hospitalized Nothing by mouth in cases of respiratory failure or of aspiration from impaired swallowing ability High-calorie, high-protein Soft, easy-to-chew foods Adequate fluids Tube feedings or total parenteral nutrition if necessary 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣Antibiotics: clarithromycin, azithromycin (Zithromax), azithromycin for Mycoplasma pneumonia ‣Piperacillin sodium-tazobactam sodium (Zosyn), imipenemcilastatin sodium (Primaxin), clindamycin phosphate (injection) (Cleocin), or metronidazole hydrochloride (Flagyl) and a respiratory fluoroquinolone and ceftriaxone sodium (Rocephin) for aspiration pneumonia ‣Antiviral agents : (Tamiflu) for (Virazole) for viral pneumonia due to adenovirus; acyclovir (Zovirax) for viral pneumonia due to herpes simplex virus ‣ Humidified oxygen ‣ Antitussives ‣ Analgesics and antipyretics: acetaminophen (Tylenol), ibuprofen (Advil) ‣ Bronchodilators: albuterol sulfate (AccuNeb), for wheezing ‣ I.V. fluids ‣ Glucocorticoids to reduce inflammatory response in certain patients in the intensive care unit. 37 lOMoARcPSD|11334620 38 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.9 NURSE ANGIE 2018 Pneumothorax Full or partial collapse of the lung Assessment Pathophysiology Pneumothorax Air enters the pleural space and accumulates and separates the visceral and parietal pleurae. Negative pressure is eliminated, affecting elastic recoil forces. The lung recoils and collapses toward the hilus, impairing lung expansion. CAUSES Spontaneous pneumothorax ‣ Rupture of bleb on lung surface ‣ Emphysematous bullae rupture Closed pneumothorax ‣ Barotrauma ‣ Blunt chest trauma ‣ Clavicle fracture ‣ Congenital bleb rupture ‣ Emphysematous bullae rupture ‣ Erosive tubercular or cancerous lesions ‣ Interstitial lung disease ‣ Rib fracture Open pneumothorax ‣ Penetrating chest injury (stabbing, gunshot) Iatrogenic pneumothorax ‣ Central venous catheter insertion ‣ Chest surgery ‣ Percutaneous lung biopsy ‣ Thoracentesis ‣ Transbronchial biopsy ‣ Tension pneumothorax ‣ Chest tube occlusion or malfunction ‣ High positive end-expiratory pressures ‣ Lung or airway puncture from positive-pressure ventilation ‣ Mechanical ventilation after chest injury ‣ Blunt or penetrating chest wound Laboratory Findings: ‣ Arterial blood gas analysis may show hypoxemia, hypercapnia, and acidosis. ‣ Chest radiography shows air in the pleural space with a white visceral pleural line defining the interface of the lung and pleural air, lack of lung markings, and, possibly, a mediastinal shift. ‣ Ultrasonography reveals absence of lung sliding (movement of visceral pleura against parietal pleura), absence of comet-tail artifact (vertical air artifacts arising from the visceral pleural line), and presence of lung point (location where lung sliding and absent lung sliding alternately appear). INTERVENTIONS ‣ Maintain patent airway ‣ Monitor respiratory status & vitals ‣ Maintain a closed chest drainage system; ‣ Monitor a chest tube unit for any kinks or bubbling ‣ Stabilize the chest tube ‣ Maintain aseptic technique ‣ Oxygen therapy and mechanical ventilation are prescribed as needed. ‣ Bed rest until lung re-expansion ‣ No air travel until chest radiography is normal EDUCATION ‣ Deep breathing exercises ‣ Incentive spirometer ‣ Causes and prevention 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Tachypnea or bradypnea, Respiratory distress, Tachycardia, Pulsus paradoxus, Asymmetrical chest wall movement Overexpansion and rigidity on the affected side, Possible cyanosis, Subcutaneous emphysema, Hyperresonance on the affected side, Diminished or absent breath sounds on the affected side Tension pneumothorax ‣ Distended jugular veins, Pallor, Anxiety, Tracheal deviation away from the affected side, Weak, rapid pulse, Hypotension, Tachypnea, Cyanosis, Absent breath sounds on the affected side, Decreased cardiac output, Chest pain, Cardiac arrest. Medical Treatment ‣ Chest tube insertion or emergent needle thoracotomy (cardiac arrest). ‣ One-way valve (such as Heimlich valve) insertion. ‣ Video-assisted thoracoscopic surgery (for recurrent primary or secondary spontaneous ‣ pneumothorax) ‣ Thoracotomy, pleurectomy (for recurrent spontaneous pneumothorax) ‣ Repair of traumatic pneumothorax ‣ Needle thoracotomy (tension pneumothorax) ‣ Pleurodesis (for repeated pneumothorax in patients who are not surgical candidates) ‣ Resection of blebs or pleura. 38 lOMoARcPSD|11334620 39 MEDICAL SURGICAL NURSING: RESPIRATORY 1.6.10 NURSE ANGIE 2018 Hemothorax Blood accumulation in the pleural cavity that may result in respiratory distress Pathophysiology Assessment Damaged intercostal, pleural, mediastinal, and sometimes lung parenchymal vessels cause blood to enter the pleural cavity. The blood acts as a space-occupying lesion, leading to respiratory difficulty. The amount of bleeding and its cause are associated with varying degrees of lung collapse and mediastinal shift. . ‣ Recent trauma, recent thoracic surgery, metastatic disease, chest pain, dyspnea, tachypnea, shallow respirations, cool, clammy, dusky colored skin, diaphoresis, hemoptysis, restlessness, anxiety, cyanosis, stupor, expansion and stiffening of the affected side, rising of the unaffected side with gasping respirations, dullness over the affected side, decreased or absent breath sounds over the affected side, symptoms associated with blunt trauma, such as bruising, tachycardia, hypotension. Medical Treatment Laboratory Findings: INTERVENTIONS ‣ Arterial blood gas (ABG) analysis may show increased partial pressure of carbon dioxide and decreased partial pressure of oxygen. ‣ Serum hemoglobin level test may be decreased, depending on blood loss. ‣ Thoracentesis may yield blood or serosanguineous fluid. ‣ Chest radiography, computed tomography scanning (thorax), or chest ultrasonography shows presence and extent of hemothorax and helps to evaluate treatment. CAUSES ‣ Blunt or penetrating chest trauma ‣ Anticoagulant therapy ‣ Central venous catheter insertion ‣ Damaged intercostal, pleural, or mediastinal vessels ‣ Damaged parenchymal vessels ‣ Dissecting thoracic aneurysm or internal ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ mammary artery aneurysm Heart or thoracic surgery Hereditary hemorrhagic telangiectasia Necrotizing infections Neoplasm Pulmonary arteriovenous fistulas Pulmonary infarction Thoracic endometriosis Tuberculosis Spontaneous pneumothorax ‣ Monitor Vital signs, Pain level and effectiveness of interventions, Intake and output, Chest tube drainage, Cardiopulmonary status, Closed drainage system function, Hemodynamic parameters, ABG results, Chest radiography results, CBC results, Signs and symptoms of infection, Skin integrity. EDUCATION ‣ Medication regimen Make follow up appointments Prevention Notify HCP if they experience s/ sx of infection ‣ Alcohol cessation if the incident was alcohol related ‣ Counseling ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Institute comfort measures and help the patient relax. Institute energy-conservation measures. Give prescribed oxygen based on oxygen saturation levels. Give prescribed I.V. fluids and blood transfusions or autotransfusion, if indicated. Change the chest tube dressing and provide chest tube care, as needed. Prepare the patient for surgery, if needed. Obtain specimens for laboratory testing, such as ABG analysis and complete blood count (CBC). 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Stabilization of the patient's clinical condition with cardiopulmonary resuscitation, if necessary ‣ Stoppage of bleeding ‣ Thoracentesis ‣ Insertion of chest tube ‣ Autotransfusion of blood loss approaches or exceeds 1L Medications ‣ Oxygen ‣ Analgesics ‣ I.V. fluid therapy, especially with hypotension ‣ Hormonal suppression for thoracic endometriosis Surgery ‣ Thoracotomy if a chest tube doesn't improve the condition and massive hemothorax or persistent bleeding are present ‣ Video-assisted thoracoscopic surgery to directly remove a clot and allow for precise placement of chest tubes 39 lOMoARcPSD|11334620 40 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.9 NURSE ANGIE 2018 Heart Failure: Left Side Due to impaired pumping ability, the heart cannot maintain adequate cardiac output. Cardiac Symptoms Pathophysiology Complications • • • • • The pumping ability of the left ventricle fails and cardiac output decreases. Blood backs up into the left atrium and lungs, causing pulmonary congestion. If untreated, left-sided heart failure will lead to right-sided heart failure. Respiratory failure Pulmonary edema Digoxin toxicity Cardiogenic shock Hypokalemia ‣ Decreased cardiac output ‣ S3 / S4 gallop, Jugular vein distention Respiratory Symptoms ‣ Dyspnea ‣ Tachypnea (30-40 /min) ‣ Orthopnea ‣ Pulmonary edema ‣ Cough ‣ Cheyenne Stokes ‣ Pleural Effusion ‣ Pink tinged sputum CNS Symptoms ‣ Fear ‣ Anxiety ‣ Cerebral Anoxia ‣ Fatigue Labs & Diagnostics ‣ BNP elevated Decreased Pa 02, increased C02 ( Acidosis) ‣ Chest X-ray may reveal cardiomegaly and alveolar edema Medical Treatment ‣ BUN and Creatinine elevated CAUSES Atherosclerosis ‣ Fluid overload ‣ MI ‣ Valvular insufficiency ‣ Hypertension ‣ Cardiomyopathy ‣ Infection ‣ Autoimmune disorders EDUCATION INTERVENTIONS ‣ Low saturated fat, trans fat, Low in sodium, and ‣ Low saturated fat & cholesterol. ‣ The client should read labels to identify heart-healthy foods. ‣ Educate client about disease ‣ Elevate HOB to SemiFowlers, Administer cardiac glycosides ‣ Monitor vital signs ‣ Record I’s & O’s ‣ Perform daily weights ‣ Oxygen therapy 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Digoxin ‣ Diuretics ‣ ACE ‣ ARB ‣ Low dose beta blockers ‣ Vasodilators: nitrates, Milrinone ‣ Morphine sulfate 40 lOMoARcPSD|11334620 41 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.9 NURSE ANGIE 2018 Heart Failure: Right Side The Hearts inability to properly pump blood to periphery to perfuse vital organs. Pathophysiology Heart failure is the inability of the heart to maintain adequate cardiac output due to impaired pumping ability. Diminished cardiac output results in inadequate tissue perfusion. Complications • Acute: Occurs suddenly. • Chronic: Develops over time, and can be accompanied by acute episodes. • • • Labs & Diagnostics Altered cardiac function Fluid overload Myocardial Infarction Death ‣ ABG my reveal Hypoxia‣ Elevated BNP/ Decreased Ejection fraction ‣ Elevated BUN & Creatinine ‣ CBC may show anemia CAUSES Atherosclerosis ‣ Fluid overload ‣ MI ‣ Valvular insufficiency ‣ Hypertension ‣ Cardiomyopathy ‣ Infection ‣ Autoimmune disorders EDUCATION INTERVENTIONS ‣ Low saturated fat, trans fat, Low in sodium, and ‣ Low saturated fat & cholesterol. ‣ The client should read labels to identify heart-healthy foods. ‣ Educate client about disease ‣ Elevate HOB to SemiFowlers, Administer cardiac glycosides ‣ Monitor vital signs ‣ Record I’s & O’s ‣ Perform daily weights ‣ Oxygen therapy 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Cardiac Symptoms ‣ Jugular vein distention ‣ Increased BP from fluid volume excess or decreased BP from pump failure ‣ Tachycardia, Dependent edema Respiratory Symptoms ‣ Chest pain ‣ Orthopnea ‣ Dyspnea CNS Symptoms ‣ Fear and anxiety GI/GU Symptoms ‣ Anorexia ‣ Weight gain ‣ Abdominal distention Treatments: ‣ ACE ‣ ARB ‣ Digoxin ‣ Diuretics ‣ Low dose beta blockers ‣ Morphine sulfate ‣ Vasodilators: nitrates, milrinone ‣ Human B natriuretic peptide: acute episodes Medical Treatment ‣ Assess clients BP and HR right before administration. ‣ Evaluate clients BP 30 mins post admin. ‣ Monitor for dizziness and hypotension. ‣ Monitor labs, especially potassium. ‣ Note interactions between NSAIDS and antihypertensive, medications. ‣ Monitor labs and look for signs of digoxin toxicity. 41 lOMoARcPSD|11334620 42 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.6 OCTOBER 10, 2018 Angina Transient ischemia of the heart muscle upon exertion. Pathophysiology Cardiac Symptoms Ischemia of the heart results in chest pain from decreased blood and oxygen supply. Angina is caused by an imbalance of oxygen supply and demand. Types of Angina ‣ Stable: occurs with activity or over exertion or stress. Disappears with Nitro ‣ Unstable: occurs with an Unpredictable amount of exertion. Happens more frequently and more severely overtime. ‣ Variant: Prinzmetal’s Angina, results from coronary artery ‣ ‣ ‣ ‣ ‣ ‣ Tachycardia Palpitations Dizziness Syncope Sweating Pallor Respiratory Symptoms ‣ Chest pain ‣ Dyspnea GI ‣ Digestive disturbances spasm. Can happen at rest Medical Treatment ‣ Nitrates: dilation of the coronary arteries and decrease preload and afterload. ‣ Calcium channel blockers: dilation of the coronary arteries and reduction of vasospasm. ‣ Beta Blockers: reduction of BP for clients who are hypertensive. ‣ Cholesterol lowering meds : HMG-COA reductase inhibitors, reduce the development of plaques. Laboratory Findings: ‣ ‣ ‣ ‣ Cardiac Enzymes are negative EKG is normal until episode occurs, the ST Depression or T-wave inversion Stress test will show changes in vital signs during episodes Cardiac Catheterization provides definitive diagnoses CAUSES ‣ Coronary artery blockage ‣ Coronary artery spasm ‣ Conditions increasing myocardial oxygen consumption INTERVENTIONS ‣ ‣ ‣ ‣ ‣ ‣ ‣ EDUCATION ‣ Balance rest and activity ‣ Follow prescribed exercise regimen ‣ Hot/Cold Temperature extremes may induce angina ‣ Encourage use of emotional support resources ‣ Avoid medications and OTC medications that increase HR ‣ Stop smoking ‣ Diet: decreased saturated fat, increased fiber, and (if indicated) decreased calorie intake Assess pain Administer oxygen Assess vitals Provide cardiac monitoring Administer Nitroglycerine Elevate HOB ‣ Can Lead to MI 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 42 lOMoARcPSD|11334620 43 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.2 OCTOBER 10, 2018 Aortic Aneurysm Pathophysiology Cardiac Symptoms Chronic inflammation which weakens the artery wall causing degenerative dilation, subsequent plaque deposits, and weakness of aorta. Risks ‣ ‣ ‣ ‣ ‣ ‣ ‣ Smoking Hypertension Advanced age Male Gender COPD Genetic Disorders Obesity ‣ Pulsation in the abdomen & systolic bruit ( If AAA) ‣ Abrupt loss of femoral and radial pulses ‣ Flatness heart over the heart Respiratory Symptoms ‣ ‣ ‣ Cyanosis Dyspnea Wheezing CNS Symptoms ‣ ‣ ‣ Limb weakness Transient paralysis Neuro Deficits Complications ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Aortic valve insufficiency Stent fractures Cardiac temperance Rupture Dissection Hemorrhage Heart failure Impaired Kidney function Stroke ‣ Atherosclerosis ‣ Bacterial infections ‣ atherosclerotic plaque ‣ Blunt chest trauma ‣ ‣ ‣ ‣ Coarctation of the aorta Marfan syndrome Rheumatic vasculitis Syphilis infection ‣ Congenital heart defects Pallor Perfuse sweating If ruptured ‣ ‣ ‣ Hypotension Tachycardia Shock ‣ If rupture or dissection occurs: Fluid replacement ‣ Airway management ‣ Cardiac Monitoring ‣ Smoking cessation ‣ Strict BP management Decreased Hemoglobin Levels X-Ray: Widening of the Aorta MRI: Confirms location EKG: Rule out MI CAUSES ‣ ‣ Treatments: Laboratory Findings: ‣ ‣ ‣ ‣ ‣ Skin Symptoms Medical Treatment EDUCATION INTERVENTIONS ‣ Low in sodium, and ‣ Low saturated fat, trans fat and cholesterol. ‣ Strict blood pressure monitoring ‣ Signs and symptoms of rupture or dissection: Sharp pain in the back or neck. ‣ Medication Compliance ‣ Smoking cessation ‣ Weight loss ‣ Making all follow visits ‣ Administer antihypertensives: Beta Blockers, ACE, ARBS. ‣ Monitor vitals and Cardiac status ‣ Monitor heart and lung sounds ‣ Assess peripheral pulses ‣ Assess for pain 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Beta Blockers: Metoprolol ‣ Negative Inotropes ‣ Morphine ‣ IV fluids or Blood Transfusion ‣ Surgery 43 lOMoARcPSD|11334620 44 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.2 MAY 13, 19, 2:50 PM CARDIAC TAMPONADE a large amount of fluid inside the pericardial sac around the heart Cardiac Symptoms Pathophysiology Cardiac tamponade is a clinical syndrome caused by the accumulation of fluid in the pericardial space, resulting in reduced ventricular filling and subsequent hemodynamic compromise. The condition is a medical emergency, the complications of which include pulmonary edema, shock, and death. Increased jugular venous pressure, hypotension, and distant heart sounds, narrow pulse pressure r/t decrease in stroke volume Rapid weak pulses Cardiac arrest Complications Jugular vein distention ‣ Pulmonary edema ‣ Cardiogenic shock ‣ Pericardial constriction Pulsus Paradoxus Respiratory Symptoms Chest pain ‣ Death Dyspnea CNS Symptoms Confusion Coolclammyextremities Paleness Swelling Laboratory Findings: Treatments: Hemodynamic support ‣ Creatinine kinase and isoform tests are elevated with myocardial infarction and cardiac trauma. ‣ ‣ ‣ ‣ ‣ Fluid therapy Pulmonary artery catheterization Chest CT or MRI of chest Chest x-ray Coronary angiography ECG (non-diagnostic, used to rule-out other conditions) Right heart catheterization Venous thromboembolism (VTE) prophylaxis Cardiopulmonary resuscitation Medical Treatment Pericardial window Pericardiocentesis CAUSES ‣ Cardiac catheterization ‣ Acute myocardial infarction ‣ Cardiac surgery, Drug reaction ‣ Effusion in cancer, bacterial infections, tuberculosis and, rarely, acute rheumatic fever ‣ Hemorrhage from non-traumatic cause. May be idiopathic ‣ Trauma, including blunt chest trauma Percutaneous balloon EDUCATION INTERVENTIONS ‣ Educate on treatment ‣ Hemodynamic monitoring ‣ Administer fluids IV ‣ Chest x-ray / echocardiogram ‣ Prepare the client for pericardiocentesis ‣ Monitor for tamponade ‣ Educate on medication regimen pericardiotomy Complete pericardectomy Pericardio-peritoneal shunt for malignant recurrent pericardial effusions Sclerosing of the pericardium for ‣ Educate on follow-up care recurrent effusion or tamponade Video-assisted thoracoscopic procedure to drain pericardial ‣ Renal failure 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 44 lOMoARcPSD|11334620 45 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.10 NURSE ANGIE 2018 Endocarditis Infection of the endocardium, heart valves, or cardiac prosthesis caused by bacteria, viruses, fungi, rickettsia, and parasites Pathophysiology Assessment: Fibrin and platelets cluster on valve tissue and engulf circulating bacteria or fungi. This produces vegetation, which in turn may cover the valve surfaces, causing deformities and destruction of valvular tissue and may extend to the chordae tendineae, causing them to rupture, leading to valvular insufficiency. Vegetative growth on the heart valves, endocardial lining of a heart chamber, or the endothelium of a blood vessel may embolize to the spleen, kidneys, central nervous system, and lungs. INTERVENTIONS ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Complete blood count WBC count, and differential Electrolytes ‣ Creatinine ‣ Blood urea nitrogen (BUN), glucose ‣ Coagulation panel Monitor for signs of emboli, splenic emboli will be evidenced by abdominal pain radiating to the left shoulder and rebound abdominal tenderness. Monitor mental status. Assess for petechiae on skin oral mucosa and conjunctiva. Assess for Osler's nodes and Janeway lesions. Assess for clubbing. Evaluate blood culture. Administer antibiotics as ordered. Prepare to dc client with IV line. ‣ Educate the client to maintain aseptic technique. ‣ Instruct the client on how to administer IV antibiotics ‣ Have the client record. temp daily for six weeks. ‣ Encourage oral hygiene for six weeks with a soft bristle toothbrush 2x daily. ‣ Have the client clean any skin lacerations and apply antibiotic ointment. ‣ Client should inform all HCP’s of hx of endocarditis ‣ Client should use prophylactic antibiotics for oral procedures. ‣ Tech the client the signs and symptoms of emboli and HF. CAUSES ‣ IV drug abuse ‣ Monitor cardiovascular status. Monitor of signs of HF. EDUCATION Laboratory Findings: ‣ Provide adequate rest and balanced activity, this prevents thrombus formation. Anti Embolism stocking. ‣ Rheumatic fever ‣ Infection ‣ Valve replacement ‣ Oral surgery ( 3-6 mos) ‣ Surgery ‣ IV line placement 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Murmurs Heart Failure Fatigue Anorexia Splinter hemorrhage in nail beds Clubbing from hypoxia Osler's nodes Janeway lesions Blood clots Petechiae Fever Splenomegaly Treatments: ‣ ‣ ‣ ‣ ‣ INSAIDS Corticosteroids Analgesia Diuretics Digoxin Medical Treatment ‣ Penicillin G at 12-18 million U/d IV by continuous pump or in six equally divided doses for four weeks. ‣ Ceftriaxone at 2 g/d IV for four weeks. ‣ Penicillin G and gentamicin at 1 mg/kg (based on ideal body weight) every 8 hours for 2 weeks ‣ Patients who are allergic to penicillin, use vancomycin at 30 mg/kg/d IV in two equally divided doses for four weeks. 45 lOMoARcPSD|11334620 46 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.9 NURSE ANGIE 2018 Cardiogenic Shock Inadequate blood flow due to the dysfunction of the ventricles of the heart. Risks Pathophysiology * * A drop in blood pressure resulting from dysfunction of the ventricles of the heart. The blood pools in the left ventricle, which then causes a backup of blood into the lungs causing pulmonary edema. This causes an increased demand for oxygen. * * Age over 65 History of heart failure or previous MI Coronary artery disease Hispanic or black ethnicity Cardiac Symptoms • • • • • Diminished peripheral pulses, rapid irregular pulses Tachycardia Hypotension Cool, clammy, pale, skin JVD Respiratory Symptoms Complications * Cardiovascular • • • • Rapid, shallow breathing Tachypnea Cyanosis Pulmonary crackles accident * Acute respiratory distress syndrome * Acute kidney injury * Cardiac arrest * Arrhythmias * Multiple organ dysfunction syndrome * Labs & Diagnostics • • Death • Troponin level test is elevated. Arterial blood gas analysis respiratory and metabolic acidosis and hypoxemia. BUN & Creatinine level (serum) test results may be elevated, indicating reduced renal perfusion. Neuro Symptoms • • • GI/GU Symptoms Urine output less than 20 mL/hr Medical Treatment * * CAUSES INTERVENTIONS EDUCATION * * • • • • • • Acute mitral or aortic insufficiency Cardiac tamponade cardiomyopathy MI (most common) Ventricular aneurysm Ventricular septal defect, ventricular tachyarrhythmia • • • • • • Oxygen Monitor urine output Iv fluid resuscitation Electrolyte replacement Elevate HOB to promote lung expansion Daily weights administer diuretics • • • Medications Disorder Possibility of death * * * 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Fatigue Anxiety Decreased level of consciousness Norepinephrine or dopamine: Gives Vasopressor support Milrinone: induces peripheral vasodilation Nitroglycerin: Decreased preload and afterload Aspirin: For patients with MI Amiodarone: for sustained tachyarrhythmias Morphine: Decrease oxygen demands Diuretics: Decrease fluid overload 46 lOMoARcPSD|11334620 47 MEDICAL SURGICAL NURSING: CRITICAL CARE NURSING 3.1.1 NURSE ANGIE 2018 Septic Shock Dysregulated response to infection resulting in acute organ dysfunction or tissue hypoperfusion Pathophysiology Risks ‣ Chronic diseases (acquired immunodeficiency syndrome, chronic obstructive pulmonary disease, diabetes, cancer) ‣ Communityacquired pneumonia Intensive care unit admission Immunosuppressive therapy Previous hospitalization, especially with Clostridium difficile infection Infection triggers pro-inflammatory and anti-inflammatory mechanisms. An imbalance leads to tissue damage and increased susceptibility to secondary infections. Organ dysfunction occurs, partly due to impaired tissue oxygenation.Vascular endothelium is damaged, leading to cell death.Altered coagulation leads to impaired tissue oxygenation, micro thrombi, and endothelial dysfunction and may lead to disseminated intravascular coagulation.Systemic vasodilation and hypotension lead to tissue hypoperfusion.Organ dysfunction and tissue hypoperfusion lead to multi-organ failure. Complications ‣ ‣ Labs & Diagnostics ‣ ‣ ‣ White blood cell count > 12,000 or < 4,000 or > 10% immature bands indicates infection and helps confirm the diagnosis. ‣ Arterial blood gas analysis may identify acidosis, hypoxemia, or hypercapnia. ‣ Elevated lactate levels indicate organ dysfunction. ‣ Urinalysis may identify urinary tract infection. ‣ ‣ ‣ ‣ Hospital-acquired infections, especially catheter-related blood stream infections, pneumonia, or abdominal infections Respiratory failure Disseminated intravascular coagulation Acute renal failure Impaired hepatic function Multi-organ failure Death ‣ Blood culture results are positive for bacterial organisms. Assessment ‣ Temperature > 100.4° F (38° C) or < 96.8° F (36° C) ‣ Tachycardia ‣ Tachypnea ‣ Symptoms specific to the infectious source ‣ Altered mental status ‣ Decreased capillary refill time or mottling ‣ Pain and purulent drainage in a surgical wound ‣ Acute oliguria (urine output < 0.5 mL/kg/ hour for 2 hours despite adequate fluid resuscitation) Medications ‣ crystalloid IV fluids or lactated Ringer solution as a 30 mL/kg bolus within 3 hours of symptom identification ‣ Albumin ‣ IV antibiotics ‣ Vasopressors ‣ Dobutamine ‣ Tylenol ‣ Blood transfusion ‣ Corticosteroids Monitoring CAUSES ‣ Community-acquired and health care-associated infections ‣ Gram-positive and gramnegative bacteria; fungal infections ‣ Pneumonia (most common cause) ‣ Urinary tract and abdominal infections INTERVENTIONS EDUCATION ‣ Oxygen ‣ Medication regimen ‣ Intubation ‣ Communication ‣ Ventilation ‣ Energy conservation ‣ Hemodialysis ‣ Disease process ‣ Fluids ‣ symptoms of infection ‣Vital signs ‣ Peripheral perfusion ‣ ‣ When to call the HCP 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Lactate level Goals of resuscitation: MAP > 65 mm Hg Lactate ≤ 2 mmol/L Urine output > 0.5 mL/ kg/hour Central venous pressure = 8 to 12 mm Hg CV oxygen saturation ≥ 70% 47 lOMoARcPSD|11334620 48 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.5 NURSE ANGIE 2018 Coronary Artery Disease Atheroscleros is caused by the narrowing or obstruction of one or more coronary Pathophysiology Cardiac Symptoms Narrowing of the coronary arteries limits blood supply to the heart muscle causing angina (chest pain due to the heart muscle ischemia).Atherosclerotic buildup will cause decreased perfusion to the myocardial tissue leading to inadequate myocardial oxygenation thus causing hypertension, angina, dysrhythmias, MI, HF or death. ‣ Chest pain ‣ palpitations ‣ Decreased peripheral pulses ‣ Pedal edema ‣ Hypertension Laboratory Findings: ‣ Elevated triglycerides. Elevated HDL and Decreased LDL ‣ C-Reactive protein may be elevated ‣ BNP may be elevated Respiratory Symptoms ‣ Dyspnea ‣ Cough ‣ Tachypnea ‣ Pulmonary congestion Risks ‣ ‣ ‣ ‣ ‣ ‣ ‣ ! Complications ‣ ‣ ‣ ‣ Cardiac arrhythmias Myocardial infarction (MI) Heart failure Angina Medical Treatment ‣ Cardiomyopathy ‣ Sudden cardiac death EDUCATION INTERVENTIONS CAUSES ‣ Atherosclerosis ‣ Dissecting aneurysm ‣ Coronary artery spasm ‣ ‣ ‣ ‣ ‣ ‣ HDL < 40 LDL >130 Smoking Hypertension Diabetes Contraception Sedentary lifestyle ‣ Low in sodium, and ‣ Low saturated fat, trans fat and cholesterol. ‣ The client should read labels to identify heart-healthy foods ‣ Educate client to reduce stress ‣ Educate on the importance of weight reduction ‣ Educate on the importance of compliance with treatments Monitor vital signs Respiratory status Edema of lower extremities Monitor fluid status Intake and output Daily weights ‣ Congenital defects 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Nitrates: dilation of the coronary arteries and decrease preload and afterload. ‣ Calcium channel blockers: dilation of the coronary arteries and reduction of vasospasm. ‣ Beta Blockers: reduction of BP for clients who are hypertensive. ‣ Cholesterol lowering meds : HMG-COA reductase inhibitors, reduce the development of plaques. 48 lOMoARcPSD|11334620 49 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.2 OCTOBER 10, 2018 Hypertension Blood pressure reading above the normal range of 120/80. Pathophysiology Cardiac Symptoms A common condition in which the force of the blood against your artery walls is high enough that it may eventually cause health problems, such as heart failure and organ damage. ‣ Tachycardia ‣ Flushing ‣ Epistaxis Respiratory Symptoms ‣ Chest pain ‣ Dyspnea CNS Symptoms ‣ Visual changes ‣ Dizziness ‣ Tinnitus ‣ Headache Treatments: ‣ Initially lifestyle changes ‣ Beta blockers Alpha Blockers ‣ Alpha 2 agonist ‣ Diuretics ‣ Vasodilators ‣ Calcium channel blockers ‣ ACE inhibitors ARBS ! ‣ Renal angiography : Test for renal disease. ‣ BUN and Creatinine Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ Urinalysis :Will detect protein, RBC, pus, and casts. Blood count/ESR Serum potassium, chloride and C02. Urinary catecholamine metabolites: To dx pheochromocytoma. Urine ketones IV pyelogram, urine cultures, radioisotope. CAUSES/COMPLICATIONS ‣ Primary: Caused by genetic, race, or unknown cause. ‣ Secondary: Result of an underlying condition such as Diabetes. ‣ Risk factors: Stress, smoking, diabetes, African American race, high cholesterol, genetics Medical Treatment ‣ Take clients BP and HR right before medication administration ‣ Assess clients BP ~30 mins post admin. ‣ Monitor for dizziness and hypotension. ‣ Monitor labs, especially INTERVENTIONS EDUCATION ‣ Document BP in the standing and lying positions. ‣ Encourage weight loss if the client is obese. ‣ Provide moderate salt restricted ‣ Low in sodium, and ‣ Low saturated fat, trans fat and cholesterol. ‣ The client should read labels to identify heart-healthy foods. diet. ‣ Plan exercise regularly ‣ Encourage stress reduction measures. ‣ Monitor s/sx of hypertensive crisis. ‣ potassium levels. ‣ Note interactions between NSAIDS and antihypertensive medication. Educate on new medication regimen ‣ Hypertensive Crisis 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 49 lOMoARcPSD|11334620 50 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.1 NURSE ANGIE 2018 Pericarditis Normal amount of fluid in the pericardium is 30 mL Pathophysiology Causes Infections MI Radiation Immune disorders Thyroid disorders Acute or chronic inflammation of the pericardium. Thickening of the pericardium causes constriction and compression of the heart. Can result in loss of pericardial elasticity, cardiac tamponade, and heart Failure. Cardiac Symptoms ‣ Precordial chest pain that radiates to the left side, neck and shoulder. ‣ Pericardial friction rub Respiratory Symptoms ‣ Grating pain with Risks ‣ ‣ ‣ ‣ ‣ ‣ ‣ Chest trauma Phenotoyin Rheumatic fever Autoimmune disease Myxedema MI TB breathing, coughing, or swallowing ‣ Exacerbation of pain in the supine position ‣ Tachypnea, dyspnea Complications ‣ ‣ ‣ ‣ ‣ ‣ Laboratory Findings: Pericardial effusion Cardiac tamponade Recurrent Constrictive pericarditis Dressler syndrome Hemodynamic instability ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Arteriosclerosis Raynauds Buerger’s Smoking Diabetes Hyperlipidemia Hypertension Obesity Sedentary lifestyle Age ‣ ‣ ‣ ‣ Fever Chills Malaise Fluid retention ‣ Possible elevated troponin ‣ Positive TB test is possible ‣ Elevated WBC count ‣ Elevated Erythrocyte sedimentation rate CAUSES Other Symptoms Medical Treatment INTERVENTIONS EDUCATION ‣ Check extremities for paleness, coolness or necrosis ‣ Do not cross legs ‣ Regular exercise ‣ No smoking ‣ Weight loss ‣ Educate on the importance of care ‣ Educate on the medication regimen 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Pericardiocentesis to identify the causative agent. ‣ Manage the underlying cause. ‣ NSAIDS: Ibuprofen ‣ Colchicine ‣ Indomethacin if allergic to NSAIDS ‣ Corticosteroids: prednisone ‣ Antibiotics or Anti-fungal therapy ‣ Proton Pump Inhibitors 50 lOMoARcPSD|11334620 51 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.8 NURSE ANGIE 2018 Peripheral Vascular Disease: Venous Pathophysiology A narrowing of vessels that carry blood to the legs, arms, stomach or kidneys. Refers to diseases of blood vessels outside the heart and brain. Risks ‣ ‣ ‣ ‣ ‣ Diabetes Obesity High cholesterol High blood pressure Sedentary lifestyle Complications ‣ PE: embolism in the lungs, tachycardia, SOB, feeling of impending doom. ‣ Embolism : stagnant collection of blood in the venous system. ‣ DVT: pain redness and decreased pulse in lower limb. Look for Homan’s sign. ‣ Cardiac enzyme levels: findings are normal in angina Labs & Diagnostics ‣ ECG: ST-depression or T-wave inversion during pain ‣ Cardiac catheterization: provides a definite dx by monitoring patency of coronary arteries. ‣ Stress Test: Changes in EKG or vitals could indicate ischemia CAUSES ‣ Advanced age causes a decreased competence of the valves ‣ Advanced age causes a greater incidence of varicose veins and slower wound healing ‣ Thrombophlebitis ‣ Venous Stasis ‣ Hyper coagulability ‣ Injury to the venous wall INTERVENTIONS EDUCATION ‣ Avoid standing or sitting ‣ Educate on medication regimen ‣ Avoid hot compresses, only apply intermittent warm moist packs ‣ Educate the client to follow prescribed anticoagulant therapy ‣ Elevate legs above heart ‣ Cardiac Symptoms ‣ Normal or decreased pulses Respiratory Symptoms ‣ Dyspnea Neuro Symptoms ‣ Numbness of the legs or feet ‣ Weakness of calf muscle ‣ Feeling coldness in the feet or legs Medications ‣ Anti-platelet medications Integumentary ‣ Cool brown skin, edema, ulcers, pain redness and induration along the vein, limb may be warmer. Musculoskeletal ‣ Deep muscle tenderness ‣ Avoid Monitor peripheral pulses 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 51 Cardiovascular Disorders Overview lOMoARcPSD|11334620 • • • • • • • 52 • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • More than 75 conditions and may cause it, including pregnancy, alcohol intake, viral infection, chemo medications • • • • • … • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • 52 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 53 • D – Drug abuser R – Replacing cardiac valves U – Untreated bacteremia; G – Gram negative and positive bacteria S – STDs • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • 53 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 54 ONCOLOGY Blood. Body. Adult. Pediatric CONTENTS Types of cancer PATHOPHYSIOLOGY Nurse Angie | 2020 Oncological Emergencies Pain Management Grading, Staging, & Diagnostics Chemotherapy Radiation therapy Oncology is the study of complex disease processes that span across many body systems as the result of mutations, malfunction, proliferation, or destruction of genes and cells. There are over one hundred types of cancer, and each has its pathophysiology, nursing Implications, and treatments. The main groups of tumors we study often include carcinoma, sarcoma, leukemia, or lymphoma. Carcinomas develop from epithelial cells that proliferate into the body tissues. Sarcomas are cancers that form that in the bones, soft tissue, and connective tissues. Lymphomas and leukemias are cancers that affect the blood and are common among children. One of the main priorities when caring for the patient with cancer is emotional support and pain management Treatments of cancer vary depending on the type, aggressiveness, stage, and receptiveness of the patient and family. Conventional treatments include 54 chemotherapy, radiation therapy, and bone marrow transplants. Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Oncology: Carcinomas 55 Patho Carcinomas are cancers that affect the epithelial tissues of various organs such as the skin, Intestines, and blood vessels. After the initial invasion of the healthy organ, carcinomas may spread to other nearby structures; this is known as metastases. Labs & Diagnostics Computerized tomography (CT) scan Bone scan Magnetic resonance imaging (MRI) Positron emission tomography (PET) scan Ultrasound and X-ray Biopsy by collecting a sample of cells for testing Treatments Chemotherapy targeted for the specific type of carcinoma Lymphnode dissection Immunotherapy Surgery Radiation therapy Types Basal cell carcinoma Squamous cell carcinoma Renal cell carcinoma Ductal carcinoma in situ (DCIS) Invasive ductal carcinoma.Adenocarcinoma Risks Aging Tobacco use Sun exposure Exposure to radiation Exposure to chemicals Viruses and bacteria Hormones such as estrogen Family history of cancer Alcohol abuse Poor diet Being overweight Interventions Maintain nutrition Prevent infection Administer chemotherapy Control pain Provide emotional support Monitor for infection & signs of decompensation Education The importance of infection control Side effects of chemotherapy & radiation treatment The importance of a healthy diet and lifestyle Community resources for mental health and support groups 55 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Oncology: Sarcoma Patho Treatments Sarcoma's are rare cancers that manifest In the bones, fat, nerves, arms, legs, and other types of connective tissues. Sarcoma's are often treated and cured by surgery, however, a small portion of them can have lasting effects and are more difficult to eradicate. Surgery Radiation therapy Brachytherapy Chemotherapy Targeted therapy Immunotherapy Labs & Diagnostics Types Tissue Biopsy Computerized tomography (CT) scan Bone scanMagnetic resonance imaging (MRI) Positron emission tomography (PET) scan Ultrasound and X-ray Risks 56 Previous radiation therapy Lymphedema Being Immunocompromised Chemicals such as agent orange or dioxin Genetic predisposition Angiosarcoma: Effects the blood vessels Osteosarcoma: Effects the bones Chondrosarcoma: Effects the cartilage Desmoid-type fibromatosis: Effects fibroblasts Ewing's sarcoma: Effects the bones of children and teens Rhabdomyosarcoma: Effects skeletal muscle Fibroblastic sarcoma: Effects fiborous tissues Kaposi's sarcoma: Occurs as the result of AIDS infection and effects the skin and mouth Interventions Maintain nutrition Prevent infection Administer chemotherapy Control pain Provide emotional support Monitor for infection & signs of decompensation Education The importance of infection control Side effects of chemotherapy & radiation treatment The importance of a healthy diet and lifestyle Community resources for mental health and support groups 56 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Oncology: Leukemia 57 Patho Leukemia's are cancers that form in the bone marrow and cause alterations in over production of faulty white blood cells. They can be myleoid or lymphoid cells. Treatments Chemotherapy Blood transfusions Stem cell transplant Radiation therapy Labs CBC: Decreased erythrocytes & platelets Leukocyte count: Normal, high or low. You may see a lot of baby WBC’S “ blast cells” and low adult WBC’s. Electrolytes : Potassium & Phosphate are elevated Uric acid: Elevated Risks Types Acute lymphoblastic leukemia Acute myeloid leukemia Chronic lymphocytic leukemia Interventions High doses of radiation Smoking Benzene Chemotherapy Down syndrome Human T-cell Virus Decrease the risk of infection Place patient on neutropenic precautions Monitor the oral mucosa for mucositis Improve nutritional intake Mouth care, small frequent meals, daily weights, low microbial diet such as, no fresh fruit Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Education Maintain nutrition Prevent infection by not eating fresh fruit , planting soil, and avoiding unhealthy environments Side effects of treatments Signs of infection 57 lOMoARcPSD|11334620 Emergencies:Spinal Cord Compression 58 Patho A oncological emergency that manifests by impeded blood flow to the spinal cord. This occurs in 5-30% of cancer patients and is caused by growth of a tumor or metastases. Can cause paralysis If left untreated for a prolonged period of time. Labs X-ray MRI Myelography with CT Causes Neoplasms Spinal tuberculosis Trauma Lesions Presentation Loss of sensation Incontinence Sexual Impotence Paralysis Muscle Atrophy Back pain Treatments Dexamethasone Surgery Radiography Chemotherapy Analgesics Disease Progression Compression of blood supply to cord Ischemia Edema Tissue death Loss of function: Motor & Sensory Interventions Deep breathing Incentive spirometry Log rolling Pain Control Mobility Safety & skin complications Provide encouragement & support to patient & family Goals Palliation of symptoms Pain control Prevention of permanent disability Avoid complications Maximize function 58 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Emergencies: D.I.C Patho 59 Assessment The coagulation cascade is activated when blood is exposed to tissue factor. In association with the coagulation system, the fibrinolytic pathway is also activated. DIC usually begins rapidly and causes bleeding and microvascular occlusion, leading to organ failure. DIC is not a disease process in itself. DIC occurs as a complication of another disorder or condition. Because of excess thrombin and fibrin, blood coagulates within the entire vascular compartment of the body, thus causing decreased amounts of platelets, ultimately depleting them. The depletion of platelets causes and increased risk of hemorrhage. Microthrombi are formed throughout the body as a result of the coagulation sequence being activated. The microthrombi are made up of coagulation proteins and platelets. Labs PT: Prolonged normal is 11-14 seconds PTT: Normal or prolonged normal is 25 to 35 seconds Platelet count: Decreased Fibrin degradation products: Elevated D-dimer: Possible elevation Risks B: Bleeding from puncture sites & wounds L: Loses unexpectedly large amounts of blood O: Oh so many mini clots O: oozing blood from your gums or nose D: Decreased platelets and RBCS Y: You may see blood in the stool or urine M: Mucosal bleeding E: Epistaxis S: Symptoms of anemia S: Shock, sepsis, cancer, OB issues may be present Interventions OB complications Neoplastic disease Infection Injury to RBC/platelets Post trauma Shock Cancer Sepsis Treatments Cefepime Continuous infusion NS 100 cc administer furosemide 40 mg IV after first unit . Vasopressors/ Heparin Blood transfusion: Packed RBC to replace loss from bleeding. Fresh frozen plasma replaces deficits in coagulation factor. Platelets replace needed cells Cryoprecipitate replaces fibrinogen Anticoagulant therapy to decrease coagulation: Heparin to interrupt the coagulation cascade and to decrease the risk of venous thromboembolism Complications Monitor for bleeding Avoid cleaning clots from exposed areas Educate the patient not to shave or to use an electric razor Use a soft bristle toothbrush Do not floss. Renal failure Cardiac tamponade Hemothorax Intracerebral hematoma Stroke Ischemic bowel Multiple organ dysfunction syndrome Death 59 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Emergencies: Tumor Lysis Syndrome 60 Patho Treatments An oncological emergency where cancer cells become destroyed and causing excess potassium and uric acid to to be released into the serum leaving the renal and cardiovascular systems vulnerable to system failure. Labs Complete metabolic panel LDH Serum uric acid Urinalysis EKG Complications IV fluids Allopurinol 300 mg BID Daily labs Rasburicase Inpatient monitoring Cardiac monitoring Treatment of hyperkalemia Dialysis may be required to remove potassium and phosphate burden calcium gluconate (decreases phos level byincreasing calcium level) Renvela (phosphate binder to decrease phosphate level) Kayexalate (binds to K+ and excretes through stool) Insulin and glucose to push potassium back Into the cells Acute renal failure Cardiac arryhthmias Seizures Death (multi-organ failure) Flank pain (nephrolithiasis) Muscle weakness/tetany Nausea & Vomiting Lethargy Risks Interventions High tumor burden Elevated baseline SCr (including dehydration) Elevated baseline uric acid Increase LDH Anticipate at risk patients Vigorous hydration Urinary alkalization with sodium bicarballopurinol Nursing Monitor labs Treatment of electrolyte imbalance Monitor I & O, weights, vital signs Complete nursing assessment 60 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Oncology: Pain Management 61 Treatments Patho Pain is a subjective feeling that can be nociceptive, somatic, or visceral as a result of mixed mediums such as inflammation and cancer mediated responses. Pain is different in every patient and is what the patient says it is. Clinicians should take special consideration when caring for patients with pain associated with cancer because it is chronic and cause Comorbidities such as anxiety and depression. Cancer Pain & Mental Health A patient's response to pain can be just as unique and Individualized as the treatment provided for it. Some patients will deny pain, but vital signs and expressions verify that pain present. Some patients will endorse pain but rate it lower than what they feel while other patients will be stoic or seem inappropriate with their pain response. No matter how the patient is expressing their pain, It Is vital to understand that whether acute or chronic, pain can have devastating effects on one's mental, spiritual, and emotional wellbeing, which is why it is critical to provide holistic care to address all of the patient's needs. Treatments for cancer pain will vary depending on the type, stage, and areas the cancer is affecting. Treating cancer pain can involve oral, IM, transdermal, and IV pain medication administration. It is critical that the clinician administering the medication know the potential side effects and complications of analgesic administration. For example, the nurse should follow institution guidelines concerning administering more than one opioid at a time. Pharmacological Treatment Common pain medications given to cancer patients includes NSAID's or Tylenol mildmoderate pain. For severe pain opioids are given such a codeine or morphine sulfate. Neuropathic pain can be treated with anticonvulsants such as Tegratol and antidepressants Cymbalta. Gabapentin may also be prescribed for this purpose also. Alternative Therapies While pharmacological treatments are the gold standard for treating pain associated with cancer it is vital the nurse understands that alternative therapies such as healing touch, reiki, meditation, and herbal suppliments have proven to have a profound impact on the cancer patients preception of pain and should be Included In the plan of care if the patient requests and the provider agrees that no harm will be caused. Causes Interventions Bone pain Organ obstruction Necrosis Fear & Anxiety Inflammation Infiltration of tissue Nerve compression Tissue distention Monitor vital signs Perform pre & post pain assessments Monitor respirations Provide relaxation Provide guided imagery Provide hot/cold therapy Provide emotional support Education Educate on medications Educate on the use opioids Educate on meditation, relaxation, and other ways to reduce pain Provide materials on support groups Educate when to call the provider 61 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 62 Oncology: Diagnostics, Grading, & Staging Diagnostics Staging Because there are so many forms of cancer there is no one size fits all approach. However, there are protocols and standards of care testing that are placed once informed consent is obtained. Common diagnostic tests and procedures include Biopsy of tissue Bone marrow Chest CT CBC & Liver function tests MRI Tumor markers Radioisotope scanning Stage 0: tumor In situ Stage I: localized tumor cell growth limited to one tissue area of origin Stage II: spread locally but limited Stage III: spread throughout the local and regional areas Stage IV: Metastasis in organs and tissues distant from the origional area of growth Surgery Grading Grade I : cells are well differentiated but look mildly abnormal Grade II : cells are more abnormal and slightly differentiated GradeIII: cells appear extremely abnormal and are poorly differentiated Grade IV: cells are not differentiated and immature Surgery is performed to stage, treat, and diagnose cancer. Surgery can be prophylactic, curative, palliative, or completed to control the growth of the tumor. Early Detection Warning signs Common Areas Skin checks Testicular exam Breast exam Mammogram Rectal exams Colonoscopy Pap smear Wounds that do not heal Sore throat that does not go away Changes in bowel and bladder habits Heartburn Hoarseness & cough Unusual bleeding Lumps In breasts or testicles Wart & mole changes Bladder cancer Brain tumor Breast cancer Colorectal cancer Lung cancer Prostate cancer Testicular cancer 62 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 Oncology: Chemotherapy 63 Types Definition Chemotherapies are cytotoxic drugs that target tumor cells systemically and are treatment modalities prescribed by oncologists to cure, palliate, maintain remission, or as a prophylatic measure. Mode of Action Chemotherapy kills normals cells while inhibiting the replication of abnormal cells causing system effects such as alterations in other areas of the body. Chemotherapy is often prescribed as series and In combination with other biotherapies to potentiate the therapeutic response efficacy. Routes of Administration Topical Oral IV push (slow admin) Infusion (most common) IM/SQ Intrathecal (spinal theca, lumbar puncture) Intraventricular (brain) What Alters Effects Tumor cell burden Tumor growth rate Vascular supply Pattern of cell division Concentration of chemotherapy available for malignant cells Adjuvant Neoadjuvant High dose/ intensiveCombination therapy Regimen changes Alkylating Agents: Non-cell specific and used for treatment in the resting cell phase. Examples Include mustard gas derivatives, Ethylenimines, Alkylsulfonates, Hydrazines, Nitrosureas, and Metal salts Plant Alkaloids: Derived from plants they treat various stages of cell growth and are cell- specific. Examples include Podophyllotoxins, Vinca alkaloids, Camptothecan analogs, and Taxanes Anti-tumor Antibiotics: Made from fungus are considered cell-specific. Some examples include Anthracyclines and Chromomycins Antimetabolites: Component are similar to the cell. Once infiltrated Into the cell they Inhibit the cancer cell from dividing and are cell cycle specific. Some examples include Folic acid antagonists, Pyrimidine antagonists, Purine antagonists, and Adenosine deaminase inhibitors Topoisomerase Inhibitors: Control the enzymes that alter the DNA during cellular replication. Some examples include Topoisomerase I inhibitors & Topoisomerase II inhibitors: Interventions Administer allopurinol prior to chemo administration to avoid tumor lysis Monitor IV access and PICC line sites Monitor for nephrotoxicity by assessing BUN and creatinine Practice safe handling and disposal Double flush the toilet Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Side Effects Anorexia Loss of taste Aversion to food Erythema Painful ulcerations Alopecia Bone marrow depression 63 lOMoARcPSD|11334620 Oncology: Radiation Therapy Patho Radiation therapy is given because it only targets cancer cells within its path and causes minimal damage to good cells. Once the cells have received the radiation they die and are no longer able to divide. Nursing Management of Dislodged Radiation Implants Types Teleatherapy: Known also as external beam therapy is administered externally to the patient which does not emit radiation thus decreasing the risk of exposure to others. Brachytherapy: Radiation is administered directly to the tumor tissue for a prescribed time and can be sealed or unsealed. Because the radiation is within the patient, the patient can pose a safety risk to those around them. Sealed vs. Unsealed Unsealed: When administering an unsealed radiation source it is important to understand that the radiation is not confined to one body area and can be excreted via sweat, urine, or feces and can be hazardous to others. Unsealed radiation can be administered via IV, oral, or through body cavities. Sealed: A sealed radiation source is typically implanted into specific tumor tissues. The patient does emit radioactivity when the implant is placed but does not excrete radiation through bodily fluids. Dose Parameters Dose Fractionation Volume Time Chemotherapy Adverse effects 64 Ensure the patients safety and have them lay still Use long forceps to gain access to the source Place the implant in a lead container Contact the radiation oncologist Document the incident and interventions Nursing Actions The patient must have a private room There should be a sign placed on the patients door Limit visitors, no pregnant women or children they should remain 6 ft away from the radiation source Cluster nursing tasks to minimize radiation exposure Rotate the patient assignment Wear a radiation measurement device and lead shield The nurse should only be assigned to one patient undergoing radiation at a time Side effects Localized skin changes Alopecia Fatigue Changes in taste or smell Education Wash irradiated area every day with warm water and mild soap Do not remove the markings Pat dry Do not use ointment or powders on the area Avoid sun and heat Wear soft loose clothing 64 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 65 MEDICAL SURGICAL NURSING: BILIARY 1.5.1 NURSE ANGIE 2018 BILIARY STRUCTURE AND FUNCTION Biliary Pathway Biliary Tree & Bile Pathway ‣ A pear shaped hollow sac-like organ under the inferior surface of the liver that holds and stores 30-50 mL of bile. Bile is mostly water that gets absorbed by the gallbladder, electrolytes, fatty acids, bilirubin, and bile salts. ‣ ‣ ‣ ‣ ‣ ‣ Biliary is made from the liver and it travels through the common hepatic duct. Then through the cystic duct and stored in the gallbladder. Cholecystokinin is released when you et fats to tell the gallbladder to contract. Bile then travels through the cystic duct to the common bile duct and into the GI tract through duodenum. In the duodenum bile mixes with fat and emulsifies with bile salts and travels to the ileum. In the ileum bile salts and fats get absorbed. The remainder of the bile salts travel back to the liver for storage until the next cheeseburger via enterohepatic circulation or get excreted in feces. Exocrine Functions The secretions of the exocrine portion of the pancreas are collected in the pancreatic duct which joins the common bile duct and enters the duodenum at the Ampulla of Vater. PANCREAS Located in the upper abdomen and functions as an endocrine and exocrine gland. ENDOCRINE FUNCTIONS OF THE PANCREAS ENZYMES SECRETED BY THE PANCREAS ‣ Sphincter of Oddi: A muscular valve that controls the flow of digestive juices (bile and pancreatic juice) through ducts from the liver and pancreas into the first part of the small intestine (duodenum.) ‣ Ampulla of Vater: Hepatopancreatic Ampulla or the hepatopancreatic duct, is formed by the union of the pancreatic duct and the common bile duct. ‣ Beta cells: Secrete insulin Cholecystokinin stimulates the release of the pancreatic/ digestive enzymes. to put glucose back into the cells. ‣ Alpha cells: Secretes glucagon to raise blood glucose levels. ‣ Delta cells: Secrete somatostatin to lower blood glucose levels. ‣ Secretin: Stimulates the release of bicarb which neutralizes he acidic gastric juices that enters the duodenum. ‣ Amylase: Breaks down carbohydrates ‣ Trypsin: Breaks down protein ‣ Lipase: Breaks down fats/lipids 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 65 lOMoARcPSD|11334620 66 MEDICAL SURGICAL NURSING: BILIARY 1.5.2 NURSE ANGIE 2018 Gallstones A small, hard crystalline mass formed abnormally in the gallbladder or bile ducts from bile pigments, cholesterol, and calcium salts. Gallstones can cause severe pain and blockage of the bile duct. Pathophysiology Assessment Gallstones are the cause of acute cholecystitis. The process is caused by a physical obstruction of the gallbladder by a gallstone, at the neck or in the cystic duct. There are two types of gallstones. Pigment stones make up 10-25% of gallstone seen in the US. Pigment stones form when unconjugated pigment is in the bile. Pigment stones must be removed surgically. Cholesterol stones make up 75% of gallstones seen in the US. Cholesterol stones are insoluble in the water and are caused by bile supersaturation with cholesterol which causes inflammatory changes in the gallbladder. Usually found by secondary detection. ‣ GI: Mild GI symptoms, epigastric distress, abdominal distention, vague right upper quadrant pain. Pain follows after eating a meal high in fat or fried foods. Pain and biliary colic. Deep breathing increases pain. ‣ GU: Very dark urine, clay colored stools. ‣ Endocrine: Deficits in vitamin absorption KADE. ‣ DERM: Jaundice, pruritus. Medical Treatment ‣ Open cholecystectomy: Removal of gallbladder. ‣ Laparoscopic cholecystectomy: Preferred removal method of the gallbladder. Short recovery. There is a risk of nicking the bile duct. Get them upright and walking. Control pain with heat or cold 15-20 minutes at a time. Laboratory Findings: ‣ Percutaneous transhepatic cholangiography: A needle ‣ ‣ ‣ ‣ ‣ ‣ Cholecystogram: Visualizes gallbladder and bile duct Cholangiogram: Visualizes gallbladder and bile duct Laparoscopy: Visualizes the liver and gallbladder Ultrasound: Visualizes abdominal organs and masses CT/MRI: Visualizes neoplasms, cysts, and hematoma, ERCP: Visualizes biliary structures and pancreas VIA endoscopy. Requires multiple position changes, starts in the left lateral position. ‣ Serum alkaline phosphatase: Measures biliary tract obstruction ‣ GCT/GGTP/LDL: Markers for biliary stasis. Elevated in alcohol abuse situations. ‣ Cholesterol levels: Elevated in biliary obstruction. Decreased in liver dysfunction. CAUSES/RISKS ‣ ‣ ‣ Ileal resection, High estrogen intake/ birth control ‣ ‣ ‣ Peritonitis, edema, gangrene, blood flow backup. ‣ ‣ Infection in the biliary tract ‣ Hemolysis, cirrhosis vile and decompress the biliary EDUCATION ‣ ‣ ‣ ‣ ‣ tract. Usually done for patients allergic to anesthesia. ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ INTERVENTIONS ‣ Obesity, Diabetes mellitus, Cystic fibrosis, Women over 40, Multipara and Native American women ‣ Frequent or rapid weight loss and changes inserted into the liver to aspirate Position changes give a temp fix NG tube and NPO status until novel sounds return. Report peritonitis. Monitor drains, monitor for bleeding, assess pain, relieve pain. Monitor intake and output, monitor incision site. Pillow or binder over incision. Turn, cough, deep breathe. Monitor respiratory status and implement incentive spirometry. Early ambulation. Maintain skin integrity. Monitor GI symptoms, fever and infection, nutrition status. ‣ ‣ ‣ ‣ ‣ Ambulation. No bathing for 48hrs. Do not drive for 4 days. Avoid lifting heavy objects for 1 week. Resume sex when ready. Check wound site daily. Wash with mild soap and water. Allow adhesive to fall off do not pull. Normal diet, gradually add fatty foods back as tolerated. Sit upright in bed or chair. Take pain medication as prescribed, report pain if unrelieved by analgesia. Follow up 7-10 days. Call if you have fever of 100 or more x 2 days, nausea vomiting or abdominal pain. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Bed rest, IV fluids, NG suction ‣ Anticholinergics: Do not give to elderly. Give toradol instead. ‣ Analgesics: Morphine, dilaudid, and fentanyl. ‣ Antibiotics ‣ Dietary altercation: low fat ‣ Ursodeoxycholic acid: Dissolves stones does not allow new ones to form, takes 6-12 month to achieve ‣ Chenodeoxycholic: dissolves stones ‣ Lithotripsy: Shockwaves to dissolve gallstones 66 lOMoARcPSD|11334620 67 MEDICAL SURGICAL NURSING: BILIARY 1.5.3 NURSE ANGIE 2018 PANCREATITIS Release of pancreatic enzymes in the pancreatic duct causing corrosion in the tissue. Pathophysiology Assessment: Pancreas begins to eat itself by using trypsin. Most patients have a history of biliary tract ideas or long term alcohol abuse issues. Gallstones enter the common bile duct and get stuck at the Ampulla of Vater thus causing an obstruction of the flow of pancreatic juices or bile reflux. Activation of the pancreatic enzymes cause vasodilation, vascular permeability and necrosis and possible hemorrhage. ‣ Lipase 0-160: Elevation can indicate and diagnose acute pancreatitis. Elevates in 24 hours and remains up to 2 weeks. ‣ H&H: Hematocrit will be elevated in hypovolemia, hemoglobin will decrease with internal bleeding. ‣ WBC: Show elevation ‣ Serum glucose: Hyperglycemia ‣ Chest & Abdominal X-Ray: to diagnose pancreatitis. ‣ CT with contrast: Show structure and increase in size of the pancreas. ‣ Peritoneal fluid samples: Show increased pancreatic enzymes. ‣ Pancreatic enzymes: Decreased ‣ Bicarb: Decreased. ‣ Albumin: Decreased. Laboratory Findings: ‣ Electrolytes: A low calcium level can indicate pancreatitis. The lower the calcium the worse the pancreatitis. Ca binds the albumin. ‣ Serum amylase 23-85 U/L: Elevation within 24 hours of start of symptoms and returns to normal within 24-72 hours. Causes ‣ Mumps virus ‣ Spasm and edema of ampulla of Vater ‣ Trauma ‣ Duodenitis ‣ Peptic ulcer ‣ Ischemic vascular disease ‣ Hyperlipidemia ‣ Hypercacemia ‣ Bacterial or viral infection INTERVENTIONS Education ‣ Respiratory care ‣ Biliary drainage ‣ Antacids, low fat low protein diet. ‣ Monitor weight, TPN and blood glucose. ‣ Skin assessments ‣ Monitor fluids and electrolytes ‣ Small frequent meals ‣ Discontinue meds that cause acute episodes. ‣ Caffeine and alcohol cessation. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ ‣ ‣ ‣ ‣ GI: Severe abdominal pain, left upper quadrant pain that radiates to the back and gets worse after a fatty meal or ingestion of alcohol and is unrelieved by antacids, abdominal distention. Worse in supine position. Poorly defined palpable abdominal mass. decreased hypoactive bowels. Vomiting that does not relieve the pain or nausea. Steatorrhea. Abdominal guarding. Fat malabsorption, starvation edema. Cardiac: Hypotension, tachycardia, cyanosis. CNS: Confusion RESP: Hypoxia, respiratory distress, dyspnea, tachypnea DERM: Jaundice Treatments: ‣ Enteral feedings/NPO status ‣ Pancreatic enzyme administration: Take enzyme before or with meals and fluids. ‣ DO not give with Benadryl. Do not chew. Do not give powder with a protein. ‣ Give Tagamet and Zantac to reduce pancreatic activity. ‣ Pain management: No opioids due to irritation of sphincter of Oddi. (morphine can be given if needed.) ‣ Pancreatic Jejunostomy (Rouxen-Y) ‣ Whipple ‣ Endoscopic & laparoscopic surgery ‣ If cysts are present, drain them. 67 lOMoARcPSD|11334620 68 MEDICAL SURGICAL NURSING: URINARY 1.7.3 NURSE ANGIE 2018 Chronic Kidney Disease Irreversible progressive loss of kidney function with a GFR of less than 60mL/ Pathophysiology Assessment Chronic Kidney Disease is characterized as an irreversible progressive loss of kidney function with a GFR of less than 60mL/ min. Chronic kidney disease occurs in stages and causes uremia and eventually end stage kidney failure. The kidneys cannot filter wastes from the blood or concentrate urine, not maintain acid base balance or regulate blood pressure. The waste and extra fluids build up in the body causing uremia and electrolyte imbalances. ‣ 24 HR urine creatinine F: 85-125 ml/min M: 95-35 ml/min.: < 95% decrease means acute damage has limited the ability to clear creatinine. ‣ Glomerular Filtration rate 125 mL/min: The amount of filtrate formed by the kidneys. GFR determines the stage of kidney failure your patient is in. ‣ CBC: If blood counts are low, kidney function is reduced. Stages of CKD Laboratory Findings: ‣ Acute Kidney Injury ‣ Oliguric phase: Give lasix, restrict fluid intake if hypertension is persistent. ‣ Diuretic phase: Administer IV fluids and Electrolytes as prescribed to replace excess fluid loss. ‣ Recovery phase: Monitor intake and output.. ‣ Diabetes ‣ Metabolic disorders ‣ Hypertension ‣ Recurrent infections ‣ ACE/ARBs : Treat hypertension and helps protect the kidneys. ‣ Diuretics: Controls fluid 1. At risk > 90 mL/min 2. Mild 60-89 mL/min Phosphorus binders, 3. Moderate 30-59 mL/min sodium bicarb, 4. Severe 15-29 mL/min kayexalate. Help control electrolyte imbalances. ‣ Erythropoietin: Increases RBC production ‣ Corticosteroids: Decrease inflammation and pain. ‣ Antihyperlipidemics: To INTERVENTIONS CAUSES Medications overload ‣ Supplements: Vit D, Ca, 5. ESKD < 15mL/min ‣ BUN 8-25 mg/dL: Indicates the renal clearance of waste products. If the BUN is elevated this indicates that the kidneys aren't clearing waste as they should. ‣ Serum Creatinine 0.7-1.4mg/dL: Creatinine is a breakdown of protein and muscle metabolism. An elevated creatinine indicates renal disease and > 50% of kidney function has been lost. H: Hypertension, hyperelectrolytes Y: Your calcium is low P: Pulmonary edema/ effusion E: Edema in the periphery R: Really confused K: Kussmaul respirations I: Itching, irritable, imbalanced gait D: Diluted urine, decreased output N: Not able to excrete waste (Uremia) E: Excess fluid volume Y: Yellow gray skin (ESKD) EDUCATION ‣ ‣ ‣ ‣ ‣ Medication routine Dialysis Fluid restrictions Dietary restrictions: Low phosphate, low potassium, moderate protein and high carbs. ‣ Avoid salmon and green leafy veggies ‣ Reduce intake of milk, chicken, beans and carbonated beverages. ‣ Renal Artery occlusion ‣ Autoimmune disorders. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) decrease cholesterol and lower BP. Treatments ‣ Hemodialysis ‣ Kidney transplant ‣ Peritoneal Dialysis ‣ Diet restrictions 68 lOMoARcPSD|11334620 69 MEDICAL SURGICAL NURSING: URINARY 1.7.3 NURSE ANGIE 2018 Cystitis -UTI UTI that usually manifests when E.coli has been misplaced into the urinary tract. Pathophysiology Assessment Inflammation of the bladder caused by obstruction, bacteria, or other irritants. The most common bacteria found in cases cystitis include; E.coli, pseudomonas, and Enterobacter. Cystitis is more common in women because they have a shorter urethra that is also positioned closer to the rectum. Sexually active women and pregnant women are at an increased risk for cystitis. C: Continual urge to pee, cloudy urine R: Really smelly pee A: Lot of restroom trips ( frequency) N: Not a lot of pee each void K: Killer pain when urinating Y: Yes I wipe the wrong way B: Bladder spasms L: Lots of blood cells in my pee A: Always unable to go ( inability to pee) D: Dark urine D: Dude I have a fever E: E Coli in my pee R: Really cold, really malaise Medical Treatment Laboratory Findings: ‣ Urinalysis :WBC’s will be present and elevated specific gravity will be noted. Bacteria may be found indicating a need for a culture and sensitivity to properly prescribe treatment. CAUSES ‣ Irritants such as soap, sprays and bubble bath. ‣ Bladder distention. Calculus ‣ Hormonal & vaginal flora changes ‣ Indwelling urinary catheters ‣ Microorganisms. Spermicides ‣ Ill-fitting vaginal diaphragms ‣ Synthetic underwear and pantyhose ‣ Bathing suits that are wet and worn for long periods of time. INTERVENTIONS ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ EDUCATION Obtain a culture & sensitivity prior to administering antibiotic treatment. Have the client increase fluids up to 3L /d especially with sulfonamides Monitor urine PH. Provide intermittent heat to the abdomen. Provide a sitz bath. Perform meticulous peri care. Perform catheter care as indicated by facility. Change the client's brief frequently. Discourage use of caffeine. ‣ Wipe front to back ‣ Avoid tub baths and bubbles baths ‣ Void every 2-3 hours ‣ Wear cotton underwear, avoid tight clothes and pantyhose ‣ Avoid sitting in a wet bathing suit ‣ Use water soluble lubricants for intercourse ‣ Void, shower, and drink water after intercourse. ‣ Avoid alcohol ‣ Take complete course of antibiotics ‣ Repeat urine culture Encourage good hygiene and handwashing. ‣ ‣ Antibiotic therapy: note that if the patients is on an aminoglycoside, sulfonamide or nitrofurantoin the actions of these drugs are decreased with increased acidity of urine. ‣ Antispasmodics ‣ Analgesia ‣ Antimicrobials ‣ 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 69 lOMoARcPSD|11334620 70 MEDICAL SURGICAL NURSING: URINARY 1.7.5 NURSE ANGIE 2018 Glomerulonephritis A group of kidney disorders caused by an inflammation in the glomerulus. Pathophysiology Assessment Most cases of glomerulonephritis are due to an immunologic response to any variety of etiologies. The response then activates a biological process that in turn results in glomerular inflammation and/or injury. ‣ ANA presence ‣ Electrolyte studies: Hyperkalemia, hyperphosphatemia, hypocalcemia Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Urinalysis (shows protein and RBCs) GFR decreased If indicated: blood, urine, or throat cultures 24 hr urine collection: For protein assay (increased in acute glomerulonephritis, decreased in chronic glomerulonephritis) Serum BUN and Creatinine increased Antistreptolysin-O titers increased after GBS infection C3 complement levels decreased Cryoglobulins present CAUSES ‣ Immunological diseases ‣ Previous hx of strep infection ‣ Autoimmune diseases ‣ GBS infection of the pharynx or skin ‣ H/o pharyngitis or tonsillitis 2-3 weeks before symptoms. s INTERVENTIONS EDUCATION ‣ Coordinate nursing cares to conserve energy. ‣ Be aware of potential fluid restrictions ordered by provider. ‣ Monitor BP, fluid and electrolytes, and respiratory status. ‣ Advise pt to complete full course of antibiotics. ‣ Daily weights; report increases to provider. ‣ Education regarding dietary and fluid restrictions. ‣ Infection control practices, ie. Hand washing 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) D: Dark colored urine, Jugular vein distention. A: Anorexia R: Really high BP K: Kind of short of breath P: Proteinuria, pulmonary HTN E: Epigastric tenderness E: Edema GI/GU: Hematuria, Oliguria or anuria, Smoky or coffee-colored urine, Sudden onset of proteinuria, Nephrotic syndrome, Sudden onset of red blood cells (RBCs) and casts in urine RESP: Dyspnea, MISC: Edema (periorbital and facial initially, then lower extremities), Fatigue, weakness (chronic), Anorexia, weight loss (chronic), Flank pain, Headache CARDIO: Increased blood pressure, hypertension, jugular vein distention, pulmonary edema, and epigastric tenderness. Medication Treatments ‣ Medications: Antibiotics, Antihypertensives (to control HTN associated with disease process). 70 lOMoARcPSD|11334620 71 MEDICAL SURGICAL NURSING: URINARY 1.7.6 NURSE ANGIE 2018 Nephrotic syndrome A kidney disorder characterized by massive proteinuria, hypoalbuminemia, hypoproteinemia, and edema. Pathophysiology Assessment Renal glomerular damage leads to massive proteinuria, leading to hypoproteinemia. The low protein in the blood leads to increased hepatic synthesis of proteins and lipids (leading to hyperlipidemia) as well as decreased oncotic pressure. The decreased oncotic pressure leads to edema, and then hypovolemia, which leads to decreased renal blood flow→ renin release→ vasoconstriction, or increased ADH/aldosterone→ Na+ and H20 reabsorption-> increased hydrostatic pressure-> edema. P: Periorbital edema U: Urine has lots of protein F: fatigue/ lethargy F: Frothy, dark urine Y: Yes the edema is in the AM F: Facial, scrotal, edema A: Ascites C: Cankles ( edema on the ankles) E: Electrolyte imbalances Laboratory Findings: Medications ‣ Urine: specific gravity, proteinuria ‣ BUN, Creatinine: Elevated Albumin ‣ Electrolytes: Monitor sodium and potassium. CAUSES ‣ Diabetes mellitus ‣ Focal segmental glomerulosclerosis ‣ Membranous nephropathy ‣ Systemic Lupus Erythematosus ‣ Amyloidosis Child gains weight Periorbital/facial edema more noticeable in morning Leg, ankle, labial, scrotal edema UOP decreases Urine dark, frothy Ascites BP normal or slightly low Lethargy Anorexia Pallor Massive proteinuria Hypoproteinemia Elevated lipids ‣ Corticosteroids: EDUCATION INTERVENTIONS ‣ Instruct parents about testing urine for protein. ‣ Importance of completion of medication therapy. ‣ Monitor VS, I/O, daily weights. ‣ Monitor urine (specific gravity, protein). ‣ Monitor for edema. ‣ NAS diet ‣ Monitor for hyperglycemia r/t use of corticosteroid use. Decreases inflammation. ‣ Immunosuppressants ‣ Diuretics: Decrease fluid build up ‣ Plasma expanders: Increase volume ‣ Blood clot in a kidney vein ‣ Heart failure 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 71 lOMoARcPSD|11334620 72 MEDICAL SURGICAL NURSING: URINARY 1.7.9 NURSE ANGIE 2018 Renal Calculi Calculi (stones) are found anywhere in the urinary tract Pathophysiology Assessment Calculi form when substances normally dissolved in the urine, such as calcium oxalate, malate, and calcium phosphate, precipitate.Renal calculi can consist of calcium stones from calcium oxalate and calcium phosphate or precipitate Large, rough calculi may occlude the opening to the ureteropelvic junction.Dilation, stretching, and spasm from acute obstruction can lead to a coliclike pain. The frequency and force of peristaltic contractions increase pain, as do local inflammation, irritation, and edema. ‣ White blood cell count may be slightly increased. ‣ Kidney-ureter-bladder (KUB) radiography or noncontrast computed tomography scanning (kidneys) reveals most renal calculi. ‣ Excretory urography helps confirm the diagnosis and determines calculi size and location. ‣ IV pyelography, computed tomography scanning (abdomen and pelvis), or magnetic resonance imaging may reveal stones or obstruction of the ureter. ‣ Ultrasonography, kidney and perirenal structures can detect obstructive changes and radiolucent calculi not seen on KUB radiography creatinine. ‣ Glomerular Filtration rate 125 mL/min: The amount of filtrate formed by the kidneys. GFR determines the stage of kidney failure your patient is in. ‣ CBC: If blood counts are low, kidney function is reduced. Laboratory Findings: ‣ A 24-hour urine collection shows calcium oxalate, phosphorus, and uric acid excretion levels. ‣ Urinalysis shows increased urine specific gravity, gross or microscopic hematuria, crystals, casts, and pyuria. ‣ Urine pH of less than 5.5 suggests uric acid stones; pH greater than 7.0 suggests struvite stones. CAUSES ‣ Family history of stone formation. ‣ Diet high in calcium and Vit D, oxalate, purines, alkali. ‣ Obstruction and urinary stasis. ‣ Diuretics ‣ UTI ‣ Prolonged urinary catheterization. ‣ Immobilization. ‣ Hypercalcemia ‣ Hyperparathyroidism ‣ Elevated uric acid level INTERVENTIONS ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ S: Sharp pain T: Temperature elevation O: onset of pain is sudden N: Noted urinary frequency E: Elevated RBC, WBC, and bacteria in the urine D: Dull aching kidney pain Types ‣ Cystine stones caused by an autosomal recessive inherited disorder involving an excess of the amino acid cystine ‣ Struvite stones, which form when ammonium magnesium phosphate is precipitated in women with urinary tract infections ‣ Uric acid stones, which form when purines are broken down in conditions such as gout or during chemotherapy. EDUCATION Monitor vitals and for temperature elevation.Administer analgesia Monitor intake & output Assess for Fever, chills & infection. Encourage fluid intake of 3L/day. Administer IV fluids if indicated. Provide warm baths and avoid massage. Encourage ambulation. Educate on proper diet for renal calculi. Prepare client for lithotripsy. Prepare to administer antibiotics and analgesia. ‣ ‣ ‣ ‣ ‣ Medication routine Dialysis Fluid restrictions Dietary restrictions: Low phosphate, low potassium, moderate protein and high carbs. ‣ Avoid salmon and green leafy veggies ‣ Reduce intake of milk, chicken, beans and carbonated beverages. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 72 lOMoARcPSD|11334620 73 MEDICAL SURGICAL NURSING: URINARY 1.7.11 NURSE ANGIE 2018 Urethritis Inflammation of the urethra, often d/t STI/STD, and may be concurrent with cystitis. Pathophysiology Assessment Inflammation of the urethra occurs d/t gonorrhea or chlamydia in men; in women, inflammation occurs d/t feminine hygiene sprays, perfumed feminine products, UTI, spermicidal jelly, UTI, or changes in vaginal mucosal lining. ‣ Dysuria ‣ Urinary frequency, urgency ‣ Nocturia ‣ Males: clear to mucopurulent penile discharge ‣ Female: lower abd pain Treatments ‣ Antibiotics ‣ Urethral dilation Laboratory Findings: ‣ UA/UC, STI/STD testing INTERVENTIONS CAUSES ‣ Inflammation results from STI/STD in men or in women: UTI, scented feminine products, changes in vaginal mucosal lining ‣ ‣ ‣ ‣ ‣ ‣ EDUCATION Encourage fluid intake Prepare for STI testing. Instruct pt in how to take a sitz/tub bath Istruct females to avoid perfumed feminine products. Instruct pt to avoid intercourse until UTI tx is complete. If STI is the cause, instruct pt on future prevention (condom use, potential for sterility with repeated infections). ‣ Similar to interventionsinstruct pt to complete abx course, safe sex practices. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 73 lOMoARcPSD|11334620 74 MEDICAL SURGICAL NURSING: URINARY 1.7.10 NURSE ANGIE 2018 Urosepsis A gram-negative bacteremia originating in the urinary tract. Pathophysiology Assessment Most commonly caused by E-coli, and in the immunocompromised patient, from an indwelling urinary catheter or untreated UTI. The greatest problem is the bacteria developing abx resistance. Fever is the most common and earliest manifestation. Treatments ‣ IV, then oral abx once discharged Laboratory Findings: ‣ UA/UC prior to abx. CAUSES INTERVENTIONS ‣ Infection from indwelling urinary catheter or untreated UTI ‣ Obtain UA/UC before abx tx is started, administer IV abx as prescribed and provide teaching regarding importance of oral abx once pt is home. EDUCATION ‣ Finish antibiotics course of treatment ‣ Increase fluid intake. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 74 lOMoARcPSD|11334620 75 MEDICAL SURGICAL NURSING: URINARY 1.7.2 NURSE ANGIE 2018 Acute Kidney Injury A rapid loss of kidney function resulting from renal cell damage. Pathophysiology Assessment Due to renal cell damage the kidney suddenly loses function from hypoperfusion and cell death. Normal kidney function may resume gradually depending on the cause and condition of the patient. disease. ‣ BUN and Creatinine ‣ Oliguric phase: less than 400 mL/ d urine output, signs of fluid volume excess, signs of uremia, metabolic acidosis, kussmaul respirations, tingling, drowsiness, disorientation, coma, pericarditis. ‣ Diuretic phase: Urine output rises slowly, followed by diuresis 4-5 L/d. This indicates damage to the nephrons is healing and recovering their ability to excrete waste. ‣ Recovery phase: Slow process and can take up to 2 years. Urine volume returns to normal, memory improves, strength increases. ‣ The signs and symptoms of Acute Kidney injury are primarily caused by the retention of nitrogenous waste. Nephrotoxic Meds Laboratory Findings: ‣ ‣ ‣ ‣ ‣ Urinalysis :Will detect protein, RBC, pus, and casts. Blood count/ESR Serum potassium, chloride and C02. Urinary catecholamine metabolites: To dx pheochromocytoma. Urine ketones ‣IV pyelogram, urine cultures, radioisotope. ‣Renal angiography : Test for renal CASE CAUSES ‣ Pre renal: Intravascular volume depletion, dehydration, decreased cardiac output, decreased peripheral vascular resistance, decreased blood flow to the kidneys, infection outside of the kidneys or obstruction. ‣ Intrarenal: Tubular necrosis, prolonged renal ischemia, intrarenal infection, obstruction, nephrotoxicity. ‣ Post renal : Bladder neck obstruction, bladder cancer, calculi, post renal infection (cystitis) . INTERVENTIONS ‣ Oliguric phase: Give lasix, restrict fluid intake if hypertension is persistent. ‣ Diuretic phase: Administer IV fluids and Electrolytes as prescribed to replace excess fluid loss. ‣ Recovery phase: Monitor intake and output. EDUCATION ‣ Decrease intake of sodium, protein, fluid, potassium, and phosphorus. ‣ Take medication as prescribed. ‣ Go to follow-up appointments. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Antibiotics: ‣ Ampocerin B ,Methicillin, Polymyxin B, Rifampin, Sulfonamides, Tetracycline chloride, Vancomycin Aminoglycosides ‣ Antineoplastics: ‣ Cisplatin, Cyclophosphamide, Methotrexate Nsaids: ‣ Celecoxib, flurbiprofen, indomethacin, ketorolac, meclofenamate, meloxicam, nabumetone, naproxen, oxaprozin, rofecoxib, tolmetin Other Medications: ‣ Acetaminophen, captopril, cyclosporine, fluorinated anesthetics, penicillamine, quinine Non-Pharmacological: ‣ Chemical agents, Radiographic contrast, pesticides, fungicides, Ethylene glycol. Heavy metals: ‣ Arsenic, Bismuth, Copper sulfate, Gold salts, Lead, Mercuric Chloride ‣ 75 lOMoARcPSD|11334620 76 MEDICAL SURGICAL NURSING: URINARY 1.7.1 NURSE ANGIE 2018 Incontinence Accidental or involuntary loss of urine from the bladder Pathophysiology Assessment Incontinence occurs when the process of micturition, physiology, functional toileting ability, has been disrupted. The underlying pathology varies among the different types of incontinence (ie, stress, urge, mixed, reflex, overflow, and functional incontinence. Types D - Delirium I - Infection, urinary A - Atrophic urethritis or vaginitis P - Pharmacologic agents P - Psychiatric illness E - Endocrine disorders R - Reduced mobility or dexterity S - Stool impaction Medical Treatment Laboratory Findings: ‣ Stress: Urine leakage associated with increased abdominal pressure from laughing, sneezing, coughing, climbing stairs, or other physical stressors on the abdominal cavity and, thus, the bladder. ‣ Urge: Involuntary leakage accompanied by or immediately preceded by urgency. ‣ Mixed: A combination of stress and urge incontinence, marked by involuntary leakage associated with urgency and also with exertion, effort, sneezing, or coughing. ‣ Overflow: The bladder becomes too full and “ leaks” ‣ Functional: The inability to hold urine due to reasons other than neuro-urologic and lower urinary tract dysfunction (eg, delirium, psychiatric disorders, urinary infection, impaired mobility). ‣ Bladder training: urinating only every 2.5 to 3.5 hours. ‣ Double voiding: Double voiding means urinating, then waiting a few minutes and trying again. ‣ Fluid and diet management ‣ Pelvic floor muscle exercises ‣ Anticholinergics: Oxybutynin. Used to treat urge incontinence, this medication relaxes the bladder muscle and can increase the amount of urine your bladder can hold. ‣ Alpha blockers. In men with urge or overflow incontinence, these relax the bladder neck muscles and muscle fibers in the prostate and make it easier ‣ Urinalysis :Will detect UTI to empty the bladder. Examples: Tamsulosin (Flomax), CAUSES ‣ Urinary tract infection. Constipation. Pregnancy. Childbirth. Changes with age. ‣ Menopause. ‣ Hysterectomy. ‣ Enlarged prostate. ‣ Prostate cancer. Obstruction. INTERVENTIONS ‣ Keep skin dry. ‣ Clean peri area well and frequently ‣ Take medications as prescribed ‣ Implement a bladder training routine. ‣ Assess for depression. ‣ Assess for signs of UTI. EDUCATION ‣ Stay hydrated ‣ Encourage family members to change the patients pad every 2 hours to prevent bacteria ‣ Frequent perineal care doxazosin (Cardura) and terazosin. ‣ Topical estrogen. For women, applying low-dose, topical estrogen in the form of a vaginal cream. ‣ Surgeries: Sling procedure, bladder neck suspension, prolapse surgery, artificial urinary sphincter. ‣ Neurological disorders. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 76 lOMoARcPSD|11334620 77 MEDICAL SURGICAL NURSING: URINARY 1.7.13 NURSE ANGIE 2018 Uremic syndrome An accumulation of nitrogenous waste products in the blood caused by the kidneys inability to filter out waste products. Pathophysiology Assessment Kidneys become damaged from disease process or injury causing inability to filter out nitrogenous waste products. This causes a buildup of waste in the blood stream, electrolyte imbalances, altered mental status and scanty output. ‣ Stool culture: Evaluate especially for E coli and Shigella bacteria. W: Waves of nausea and vomiting. A: Altered Level of conscious, anemia S: Some blood in the urine T: Terrible BP E: Extra waste in the urine and blood D: Dysrhythmias Treatments ‣ Hemodialysis, Peritoneal dialysis, Hemofiltration, and Renal replacement therapy. ‣ Calcitriol, calcium reducers, erythropoietin. ‣ Kidney transplant. ‣ Laboratory Findings: ‣ Urinalysis: Mild proteinuria may be present; red blood cells (RBCs) and RBC casts may be present. ‣ (BUN), serum creatinine, and serum electrolyte levels: Elevated. ‣ Hematologic determination: Severe anemia may be present. ‣ Hemolytic workup: Results may show anemia. Bilirubin levels may be elevated. Lactate dehydrogenase (LDH) levels may be elevated. Haptoglobin levels may be decreased. CAUSES ‣ CKD ‣ AKI ‣ Diabetes ‣ Kidney trauma INTERVENTIONS ‣ ‣ ‣ ‣ ‣ EDUCATION ‣ Educate the patient on dialysis procedures. ‣ Educate the patient on prescribed treatment regimen. ‣ Educate the patient on proper diet to reduce the risk of recurrence. Monitor VS for tachycardia, hyper/hypotension and dysrhythmias. Monitor serum electrolyte levels. Monitor intake & Output Provide a high protein diet. Provide a limited sodium, nitrogen, phosphate and potassium diet. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 77 lOMoARcPSD|11334620 78 MEDICAL SURGICAL NURSING: URINARY 1.7.12 NURSE ANGIE 2018 Ureteritis Inflammation of the ureter often associated with bacterial or viral infections and pyelonephritis Pathophysiology Assessment Pathophys will be dependent upon causative disease process ‣ Dysuria ‣ Urinary frequency ‣ Clear to mucopurulent penile discharge Treatments ‣ Metronidazole (Flagyl) or clotrimazole (Mycelex) for Trichomonas infection. ‣ Nystatin and Diflucan for yeast infections. ‣ Doxycycline or Zithromax for chlamydial infections. Laboratory Findings: ‣ Dependent upon causative organism (bacterial/viral infections, pyelonephritis). CAUSES ‣ Bacterial or viral infection ‣ Pyelonephritis INTERVENTIONS EDUCATION ‣ Identifying and treating the underlying cause, providing symptomatic relief. ‣ Encourage pt to finish abx treatment, safe sex practices. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 78 lOMoARcPSD|11334620 79 Electrolytes Introduction Keeping The Balance Electrolyte Regulation in the Body Electrolytes are minerals that come from dietary sources such as fruit, vegetables, and salt. Proper electrolyte balance is vital to maintain homeostasis and cellular regulation in the body.Each electrolytes has a specific function. For example, some electrolytes aid in nerve conduction, muscular function, acid- Potassium Magnesium Sodium Calcium Phosphate Chloride base balance, and water balance. Electrolyte imbalances can have devastating effects on the body. Symptoms of electrolyte imbalances range from mild with dizziness, weakness, or nausea. Severe symptoms can include cardiovascular irregularities, tetany, and death. Electrolyte regulation begins with the ingestion of sodium, potassium, phosphate, chloride, calcium, or potassium. The kidneys filter electrolytes and water by keeping what the body needs and excreting excess electrolytes and water out of the body. Electrolyte imbalances occur when the body is unable to excrete or hold on to the appropriate amount of water and electrolytes due to kidney disease, cardiac disease, or endocrine disorders. Excess amounts of electrolytes are classified as HYPER while deficits of electrolytes are classified as HYPO. A way to remember these is to learn how the body will present in presence of one of these imbalances. Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 79 lOMoARcPSD|11334620 80 ELECTROLYTE IMBALANCES Potassium Excess : Hyperkalemia Expected Laboratory Findings Pathophysiology Excessive amounts of potassium build up outside of the cell. This can happen because of trauma, metabolic dysfunctions such as acidosis,kidney failure, blood transfusions, and more. When the serum potassium level rises and the body is unable to excrete the excess potassium the patient may present with cardiac arrhythmia, muscular dysfunction, and eventually death if left untreated for long periods. Potassium level (serum) is greater than 5.5 mEq/L Arterial blood gas analysis shows decreased pH Complete blood count (CBC) with differential may show a decreased hemoglobin Creatinine Kinase Levels may be elevated Assessment & Physical Findings Cardiac: Tachycardia and later bradycardia T wave elevation,Cardiac arrest (with levels >7 mEq/L), Ventricular arrythmia's Musculoskeletal: Muscle weakness, flaccid paralysis GI: Nausea, diarrhea, abdominal GU: Oliguria, anuria Neuro: Hyperreflexia progressing to weakness, numbness,tingling, flaccid paralysis, Metabolic acidosis Causes Interventions Kidney dysfunction or failure Adrenal gland insufficiency Burns/crush injuries Decreased urinary excretion of potassium Mass blood transfusion Severe infection Potassium Sparring medications Serum potassium levels Cardiac status, including cardiac rate and rhythm Intake and output Signs and symptoms of hyperkalemia and hypokalemia Education Decrease dietary intake of potassium, no avocados or green veggies or oranges. 80 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 81 ELECTROLYTE IMBALANCES Potassium Deficit: Hypokalemia Expected Laboratory Findings Patho Slight deviations in serum levels can produce profound clinical consequences. Deviations result from deficient intake of potassium, increased excretion of potassium, or a shift of potassium from extracellular to intracellular space. Potassium imbalance can lead to muscle weakness and flaccid paralysis because of an ionic imbalance in neuromuscular tissue excitability. Treatments Potassium chloride, potassium phosphate, potassium bicarbonate, potassium citrate or IV infusion of potassium Magnesium sulfate Potassium-sparing diuretics Drugs That Cause Hypokalemia Adrenergic drugs, such as albuterol sulfate (Proventil-HFA) and epinephrine Digoxin potentiates hypokalemia but causes hyperkalemia Antibiotics, such as amphotericin B deoxycholate, carbenicillin, and gentamicin sulfate cisplatin corticosteroids Diuretics, such as furosemide and thiazide diuretics Insulin Laxatives Causes Acid-base imbalances Cushing syndrome Excessive GI or urinary losses, such as from vomiting, gastric suction, diarrhea, dehydration, anorexia, or chronic laxative abuse Low-potassium diet Hyperaldosteronism Severe serum magnesium deficiency Potassium level (serum) is less than 3.5 mEq/L. Arterial blood gas analysis shows elevated bicarbonate and pH levels. Serum glucose level is slightly elevated. Magnesium level may be decreased Assessment & Physical Findings Cardiac: Dizziness, Hypotension, Arrhythmias, flattened T waves, elevated U waves, decreased ST segments, cardiac arrest with levels < 2.5 mEq/L Musculoskeletal: Muscle weakness and fatigue, leg cramps GI: Nausea, vomiting, anorexia, diarrhea, abdominal distention, paralytic ileus or decreased peristalsis GU: Polyuria Neuro: Malaise, irritability, confusion, mental depression, speech changes, decreased reflexes, respiratory paralysis, Metabolic alkalosis Interventions Monitor serum potassium levels Assess cardiac rate and rhythm Monitor Intake and output, i Monitor vital signs Maintain I.V access site Monitor hypokalemia Education Increase dietary intake of potassium Educate on symptoms of hypokalemia Educate diabetics on risks of hypokalemia when taking insulin 81 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 82 ELECTROLYTE IMBALANMCES Calcium Excess: Hypercalcemia Expected Laboratory Findings Patho Hypercalcemia occurs when the amount of calcium in the blood stream becomes greater than the amount of calcium that is normally excreted by the kidneys. This can happen from a number of factors however, hyperparathyroidism is the most common cause. Treatments I.V. fluid therapy with normal saline solution Loop diuretics Furosemide Bisphosphonates Alendronate sodium Calcitonin Cinacalcet hydrochloride: lowers PTH levels PredniSONE : treats diseases related to increased absorption of dietary calcium Serum calcium level is greater than 10.2 mg/dL. PTH level elevated. Assessment & Physical Findings Cardiac: Heart block, cardiac arrest, hypertension Musculoskeletal: Weakness, flaccidity, hyporeflexia, bone pain GI: Anorexia, nausea, vomiting, constipation, dehydration, polydipsia GU: Polyuria, pain in the kidneys, azotemia Neuro: Drowsiness, lethargy, headaches, depression, apathy, irritability, confusion Drugs That Cause Hypercalcemia Thiazide diuretics Calcium-containing antacids Calcium preparations Lithium Vitamin A Vitamin D Theophylline Anti-estrogens Chlorthalidone Causes Hyperparathyroidism Multiple myeloma or bone tumors Excess vitamin D or A intake Addisonian crisis Multiple fractures Rhabdomyolysis Acute kidney injury Interventions Vital signs Pain level and effectiveness of interventions Cardiopulmonary status Cardiac rhythm Neurologic status Seizures Calcium levels Hydration and fluid balance Education Reduction of calcium and vitamin D Adequate hydration-at least 6 to 8 glasses of water per day Avoid calcium containing antacids 82 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 83 ELECTROLYTE IMBALANCES Calcium Deficit: Hypocalcemia Expected Laboratory Findings Patho Calcium and phosphate together aid in the bone making process. Calcium also affects the blood's ability to clot and affects cardiac and smooth contraction. When serum calcium is low it can have detrimental effects on the heart and CNS as well as the muscular system. Calcium level (serum) is less than 8.5 mg/dL. Phosphate level (serum) may be elevated or decreased, depending on the underlying cause. Serum magnesium level test may be low. PTH levels may be low to normal Treatments Oral calcium (calcium carbonate, calcium citrate, or calcitriol) and vitamin D supplements Calcium chloride or. calcium gluconate IV (if severe) Magnesium sulfate (IV) if serum magnesium level is less than 1 mg/dL Ergocalciferol or cholecalciferol if vitamin D deficiency is present Drugs That Cause Hypocalcemia Cinacalcet hydrochloride Chemotherapy Bisphosphonates Anticonvulsants, and foscarnet sodium Causes Hypomagnesemia Hypoparathyroidism Hyperphosphatemia Inadequate dietary intake of calcium and vitamin D Malabsorption or loss of calcium from the GI tract Overcorrection of acidosis Pancreatic insufficiency, acute pancreatitis Liver disease & Kidney failure Severe infections or burns Sepsis &Rhabdomyolysis ‣ Vitamin D deficiency Assessment & Physical Findings Cardiac: Arrhythmias, hypotension, bradycardia Musculoskeletal: Chvostek’s & Trossou's sign, paresthesia, tetany, facial spasms, abdominal cramps, muscle cramps, spasmodic contractions Resp: Dyspnea GI: Increased GI motility, diarrhea Neuro: Anxiety, irritability, twitching around, mouth, laryngospasm, Seizures Interventions Monitor Cardiac rate and rhythm & respiratory status, including airway Monitor Serum electrolyte levels, especially calcium, phosphorus, and magnesium Implement seizure precautions Obtain IV access site Monitor Signs and symptoms of hypocalcemia and hypercalcemia Education Proper administration of calcium supplements Ingest foods high in calcium Frequent lab testing for alterations in calcium levels Increase vitamin D. This promotes absorption of calcium Do not take OTC antacids or laxatives without speaking to your HCP Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 83 lOMoARcPSD|11334620 84 ELECTROLYTE IMBALANCES Magnesium Excess: Hypermagnesemia Expected Laboratory Findings Patho Magnesium enhances neuromuscular integration and stimulates parathyroid hormone secretion, thus regulating intracellular fluid calcium levels. Magnesium may also regulate skeletal muscles through its influence on calcium utilization by depressing acetylcholine release at synaptic junctions. Magnesium almost always first effects the muscles. Treatments Magnesium level test is greater than 2.5 mEq/L. Potassium level (serum) may be elevated. Calcium level may be decreased. Creatinine clearance test result is less than 30 mL/minute Arterial blood gas analysis may reveal respiratory acidosis Assessment & Physical Findings IV fluids, such as normal saline or lactated Ringer solution Loop diuretics such as furosemide (Lasix) Calcium gluconate to act as a magnesium antagonist when symptoms are severe IV glucose and insulin to shift magnesium into the cells Drugs That Cause Hypermagnesemia Cardiac: Bradycardia, weak pulse, hypotension, heart block, increased PR interval, QRS complex, and Q-T interval , cardiac arrest Musculoskeletal: Diminished reflexes, muscle weakness, flaccid paralysis, respiratory muscle paralysis, facial, paresthesia Neuro: Drowsiness, flushing, lethargy, Confusion, diminished sensorium, fixed and dilated pupils Magnesium containing antacids Laxatives that contain magnesium Magnesium supplements Lithium Causes Acid-base imbalances Addison's disease Adrenocortical insufficiency Chronic renal insufficiency Overcorrection of Hypomagnesemia Untreated diabetic ketoacidosis Hypothyroidism Hypoparathyroidism Lithium intoxication Tumor lysis syndrome Interventions Monitor serum potassium levels Assess cardiac rate and rhythm Monitor Intake and output, i Monitor vital signs Maintain I.V access site Monitor hypokalemia Education Decrease intake of magnesium Educate on the signs and symptoms of magnesium toxicity Diet : avoids foods high in magnesium Avoid laxatives Monitor lithium levels Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 84 lOMoARcPSD|11334620 85 ELECTROLYTE IMBALANCES Magnesium Deficit: Hypmagnesemia Expected Laboratory Findings Patho Magnesium enhances neuromuscular integration and stimulates parathyroid hormone secretion, thus regulating intracellular fluid calcium levels. Magnesium may also regulate skeletal muscles through its influence on calcium utilization by depressing acetylcholine release at synaptic junctions. Treatments Magnesium gluconate orally or magnesium sulfate I.V. Potassium and calcium supplementation (if hypokalemia or hypocalcemia is present) Benzodiazepines for seizures with severe hypomagnesemia Calcium gluconate I.V. if overcompensation of magnesium correction causes low calcium levels Serum magnesium level test is less than 1.5 mEq/L. Potassium level (serum) is below normal. Calcium level is below normal. EKG: Torsades de Pointes Assessment & Physical Findings Cardiac: Arrhythmias, vasomotor changes, occasionally hypertension Neuromuscular: Hyper-irritability, tetany, leg and foot cramps Neuro: Confusion, Delusions, hallucinations, seizures Drugs That Cause Hypomagnesemia Aminoglycoside antibiotics Amphotericin B deoxycholate Cetuximab, panitumumab Cisplatin CycloSPORINE Insulin Laxatives Loop or thiazide diuretics, such as bumetanide, furosemide, or torsemide Pentamidine isethionate Causes Acute injury Chronic alcoholism, chronic diarrhea, Diabetic acidosis, excessive release of adrenocortical hormones Hyperaldosteronism, Malabsorption syndrome, nasogastric suctioning Prolonged diuretic therapy/Severe dehydration Starvation or malnutrition Interventions Monitor Vital signs Monitor serum electrolyte levels, especially magnesium, calcium, and potassium Monitor intake and output Monitor cardiac rate and rhythm Monitor Neurologic status, including level of consciousness Respiratory status Education Increase intake of foods high in magnesium such as: legumes, green leafy veggies, nuts, seeds, whole grains Avoid over the counter diuretics Avoid alcohol consumption ‣ Improve glucose control Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 85 lOMoARcPSD|11334620 86 ELECTROLYTE IMBALANCES Chloride Excess: Hyperchloremia Expected Laboratory Findings Patho Chloride level (serum) is greater than 108 mEq/L. Chloride accounts for two-thirds of all serum anions. Chloride is secreted by the stomach mucosa as hydrochloric acid; it provides an acid medium that aids digestion and activation of enzymes. Chloride helps maintain acid-base and body water balances. An inverse relationship exists between chloride and bicarbonate. When the level of one goes up, the level of the other goes down. With metabolic acidosis, arterial blood gas analysis shows pH is less than 7.35, carbon dioxide level is less than 22 mEq/L, and the anion gap is normal Sodium level (serum) is greater than 145 mEq/L Assessment & Physical Findings Treatments Sodium bicarbonate I.V. I.V. fluid therapy with lactated Ringer solution Loop diuretics to address fluid overload Mineralocorticoids for aldosterone deficiency and to prevent heart failure Cardiac: Pitting edema, Dyspnea, rapid deep breathing, tachypnea, hypertension, signs of heart failure with pulmonary edema Musculoskeletal: Weakness, musculoskeletal difficulties Neuro: Agitation Drugs That Cause Hyperchloremia AcetaZOLAMIDE Ammonium chloride Sodium polystyrene sulfonate Salicylates Triamterene Causes Hypernatremia Hyperparathyroidism Loss of pancreatic secretion Diabetes insipidus Autoimmune disorders Metabolic acidosis Prolonged diarrhea Renal tubular acidosis Interventions Serum electrolyte levels, especially sodium, chloride, and potassium levels Respiratory status Signs of metabolic alkalosis Intake and output Daily weight Location and extent of edema Neurologic status Cardiopulmonary status, including cardiac rhythm ABG levels Education Avoid foods high in chloride: tomato juice, bananas, dates, eggs, cheese, milk, salty broth, canned veggies Avoid free water w/out electrolytes if excreting large amount of chloride (sweating) 86 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 87 ELECTROLYTE IMBALANMCES Chloride Deficit: Hypochloremia Expected Laboratory Findings Patho Chloride accounts for two-thirds of all serum anions. Chloride is secreted by the stomach's mucosa as hydrochloric acid; it provides an acid medium that aids digestion and activation of enzymes. It participates in maintaining acid-base and body water balances, influences the osmolality or tonicity of extracellular fluid, plays a role in the exchange of oxygen and carbon dioxide in red blood cells, and helps activate salivary amylase. Treatments Fluid resuscitation with I.V normal saline solution Electrolyte replacement therapy, including potassium chloride (K-Lor) and sodium chloride Nonsteroidal anti-inflammatory drugs (NSAIDs), such as indomethacin(Indocin) Carbonic anhydrase inhibitors such as acetaZOLAMIDE (Diamox) Chloride level (serum) is less than 98 mEq/L Sodium level, serum, is less than 135 mEq/L Potassium level (serum) may be decreased Assessment & Physical Findings Cardiac: Cardiac arrhythmias Musculoskeletal: Muscle weakness, twitching, tetany, hyperactive deep tendon reflexes, muscle cramps Integumentary: Dry skin Respiratory: Shallow, depressed breathing Drugs That Cause Hypochloremia Loop Diuretics Osmotic Diuretics Thiazide Diuretics Causes Addison disease Administration of dextrose I.V. without electrolytes Loss of hydrochloric acid in gastric secretions due to vomiting, gastric suctioning, or gastric surgery Prolonged diarrhea or diaphoresis Diuretics Salt-restricted diets Interventions Neurologic status assessment, including level of consciousness Muscle strength and movement Cardiac rate and rhythm Fluid balance Serum electrolyte levels Respiratory status Signs and symptoms of metabolic alkalosis and metabolic acidosis Respiratory status Education Increase foods high in chloride and sodium tomato juice, bananas, dates, eggs, cheese, milk, salty broth, & canned veggies Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 87 lOMoARcPSD|11334620 88 ELECTROLYTE IMBALANCES Phosphate Excess: Hyperphosphatemia Expected Laboratory Findings Patho Functions of phosphate: Exists in combination with calcium in teeth and bones. In extracellular fluid, supports many metabolic functions (B vitamin use, acidbase homeostasis, bone formation, nerve and muscle activity, cell division, transmission of hereditary traits, and metabolism of carbohydrates, proteins, and fats. Treatments I.V. fluid hydration with normal saline solution Oral phosphate binders, such as sevelamer hydrochloride (Renagel), sevelamer carbonate (Renvela), or lanthanum carbonate (Fosrenol) Calcium-based phosphate binders such as calcium carbonate or calcium acetate (PhosLo) Aluminum salts (not given to patients with kidney disease because they may contribute to aluminum-related osteomalacia) Loop diuretics with normal saline Replacement to enhance urine excretion Chloride level (serum) is less than 98 mEq/L. Sodium level, serum, is less than 135 mEq/L. Potassium level (serum) may be decreased. Arterial blood gas (ABG) analysis may show metabolic alkalosis: pH is greater than 7.45. Bicarbonate level is greater than 26 mEq/L. Assessment & Physical Findings Cardiac: Hypotension Musculoskeletal: Hyperreflexia, abdominal spasm, Tetany Neuro: Altered mental status, presence of Chvostek or Trousseau sign, cataracts, visual impairment, seizure Drugs That Cause Hyperphosphatemia Enemas such as Fleet enemas Laxatives containing phosphorus or phosphate Oral phosphorus supplements Parenteral phosphorus supplements (sodium phosphate, potassium phosphate) Vitamin D supplements. Causes Acid-base imbalance Trauma, burns, crush injuries, or heat-related illnesses Severe infections Hypocalcemia Hypoparathyroidism Overuse of laxatives with phosphates or phosphate enemas Kidney failure ‣ Acidosis ‣ Rhabdomyolysis Interventions Monitor vital signs Monitor cardiac rhythm Monitor phosphorus and calcium levels Monitor neurologic status Monitor neuromuscular status Monitor intake and output Monitor hydration Monitor kidney function Education Decrease intake of phosphate rich foods such as Hard cheese Meat, nuts, dried fruit and Veggies, sardines, milk, whole grains, & sweet bread 88 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 89 ELECTROLYTE IMBALANCES Phosphate Deficit: Hypophosphatemia Expected Laboratory Findings Patho Phosphate level (serum) is less than 2.5 mg/dL Decrease in phosphate levels may affect: Calcium in teeth and bones. Metabolic functions such as including use of B vitamins; acid-base homeostasis; bone formation; nerve and muscle activity; cell division; transmission of hereditary traits; and metabolism of carbohydrates, proteins, and fats. Treatments Oral or I.V. phosphate salts (for severe hypophosphatemia) Vitamin D preparations, Cinacalcet hydrochloride (Sensipar) for treatment of hyperparathyroidism as the cause of hypophosphatemia Assessment & Physical Findings Chest pain Bone pain Tissue hypoxia Nystagmus Paresthesia Muscle weakness Tenderness Confusion Seizures Drugs That Cause Hypophosphatemia AcetaZOLAMIDE Thiazide diuretics Loop diuretics Antacids Bisphosphonates Cisplatin Bevacizumab Carmustine Ifosfamide Insulin Laxatives. Causes Chronic diarrhea Chronic use of antacids containing aluminum hydroxide Hypomagnesemia Inadequate dietary intake of phosphorus Intestinal malabsorption of phosphorus related to malnutrition resulting from a prolonged catabolic state or chronic alcoholism Renal tubular defects Interventions Respiratory status Neurologic status and seizures Serum phosphorus and calcium levels Nutritional intake Intake and output Signs and symptoms of hypocalcemia, hypercalcemia, hypophosphatemia, and hyperphosphatemia Education Increase intake of phosphate rich foods such as ; hard cheese, meat, nuts, dried fruit and veggies, sardines, milk, whole grains, sweet bread Take Renvela with food Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 89 lOMoARcPSD|11334620 90 ELECTROLYTE IMBALANMCES Sodium Excess: Hypernatremia Expected Laboratory Findings Patho Sodium is the major cation (90%) in extracellular fluid, and potassium is the major cation in intracellular fluid. Sodium cation functions include maintaining tonicity and concentration of extracellular fluid, acid-base balance (reabsorption of sodium ion and excretion of hydrogen ion), nerve conduction and neuromuscular function, glandular secretion, and water balance. Treatments Hemodialysis for serum sodium levels greater than 200 mEq/L Oral water if the patient is alert & responsive Administration of salt-free solutions (such as dextrose in water), followed by infusion of half-normal saline solution to prevent hyponatremia I.V. fluids for hydration: Isotonic saline or lactated Ringer solution for hypovolemia Hypotonic fluids for excess sodium Desmopressin acetate (DDAVP) intranasally for neurogenic diabetes insipidus Chlorothiazide (Diuril) for nephrogenic diabetes insipidus Serum sodium level is greater than 145 mEq/L. Urine sodium level is less than 40 mEq/24 hours, with high serum osmolality Assessment & Physical Findings Cardiac: Hypertension, tachycardia, pitting edema, excessive weight gain Musculoskeletal: Flushed skin, dry, sticky membranes Resp: Dyspnea, respiratory distress, death GI: Rough, dry tongue, intense thirst GU: Oliguria Neuro: Fever, agitation, restlessness, seizures, gait disturbances Drugs That Cause Hypernatremia Antacids with sodium bicarbonate Antibiotics such as ticarcillin disodium-clavulanate potassium Salt tablets Sodium bicarbonate injections I.V. sodium chloride Laxatives Causes Decreased ADH Dehydration Cushing syndrome Excess hypertonic solution infusion GI fluid loss Diabetes insipidus Interventions Serum sodium levels Urine osmolality Cardiopulmonary status Renal function Intake and output Daily weight Hydration status Neurologic status Education Decrease sodium intake Contact HCP if you feel dizzy, have excessive weight gain, or high heart rate Avoid foods such as: Bacon, butter, canned food, cheese, frankfurters, ketchup, lunch meat, milk, mustard, processed foods, snack foods, soy sauce, table salt, white and whole wheat bread 90 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 91 ELECTROLYTE IMBALANCES Sodium Deficit: Hyponatremia Expected Laboratory Findings Patho Sodium is the major cation (90%) in extracellular fluid (potassium is the major cation in intracellular fluid). During repolarization, the sodium-potassium pump continually shifts sodium into the cells and potassium out of the cells; the reverse occurs during depolarization. Treatments Sodium replacement Demeclocycline: chronic hyponatremia due to SIADH Vasopressin receptor antagonists: conivaptan hydrochloride, tolvaptan for hypervolemic hyponatremia and SIADH Hypertonic saline solution (with serum sodium levels below 110 mEq/L); isotonic saline solution for hypovolemia Drugs That Cause Hyponatremia ANTICONVULSANTS carbamazepine ANTIDIABETICS chlorpropamide & tolbutamide ANTINEOPLASTICS cyclophosphamide & vinCRIStine sulfate (VCR) ANTIPSYCHOTICS fluphenazine decanoate, thioridazine hydrochloride thiothixene DIURETICS bumetanide, ethacrynic acid, furosemide, thiazides SEDATIVES barbiturates & morphine sulfate Causes Acid-base imbalances Cushing syndrome Excessive GI or urinary losses, such as from vomiting, gastric suction, diarrhea, dehydration, anorexia, or chronic laxative abuse Low-potassium diet Hyperaldosteronism Severe serum magnesium deficiency Serum sodium level is less than 135 mEq/L. Urine specific gravity is less than 1.010. Osmolality (serum) is less than 280 mOsm/kg (dilute blood). Urine specific gravity: increased Blood urea nitrogen-creatinine ratio is less than 20:1 in euvolemic hyponatremia and greater than 20:1 in hypovolemic hyponatremia. Assessment & Physical Findings Cardiac: Hypotension, Tachycardia, vasomotor collapse, thready pulse Respiratory: Cold, clammy skin, decreasing skin turgor, Cyanosis GI: Nausea, Vomiting, abdominal cramps GU: Oliguria or anuria Neuro: Anxiety, Headaches, muscle, twitching weakness, seizures Interventions Restrict water intake as appropriate; limit the patient's free access to fluids. Give prescribed IV fluids; Ensure patent IV access. Assess skin turgor and mucous membranes Assess the patient's neurologic status closely and frequently for changes. Institute seizure precautions. Education Increase sodium intake Eat foods high in sodium Signs and symptoms of hyponatremia Medication regimen Symptoms of hypernatremia If on lithium educate on the importance of a steady salt intake 91 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) lOMoARcPSD|11334620 92 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.13 NURSE ANGIE 2018 ENDOCRINE DISORDERS: CUSHING’S DISEASE A metabolic disorder characterized by Excess glucocorticoid secretion, increased secretion of ACTH and large doses of corticosteroids. Physiology Assessment When stimulated by ACTH, the adrenal gland secretes cortisol and other steroid hormones. ACTH is produced by the pituitary gland and released into the petrosal venous sinuses in response to stimulation by corticotropin-releasing hormone (CRH) from the hypothalamus. S: High sugars A: Androgen hormone increase R: Resistance to infection low A: Apple shape H: Hypertension I: Intense mood swings S: Sodium increase S: Serum calcium increased A: A buffalo hump L: Looks like the moon ( face) T: Lines and striations on the skin Y: Yes they are obese in the trunk Derm: Purple striations on the skin, poor resistance to infections, moon face, buffalo hump, easily bruised skin. Heart: hypertension. ENDO: Edema, truncal obesity, hirsutism, hyperglycemia, hypernatremia. CNS: Mood swings. MS: Muscle wasting, weakness, osteoporosis, thin extremities. Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Skull films CT MRI Serum sodium and glucose elevated Serum potassium lowered Plasma cortisol will be increased ACTH stimulation test Urinary hydrocortisone and ketocorticoids will be increased CAUSES ‣ Tumor that grows on the pituitary releasing ACTH. ‣ Adrenals release excess amounts of cortisol. ‣ Stress and cortisol build up from medications ( cushing's syndrome). ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Treatments INTERVENTIONS Education Monitor vital signs esp. BP Monitor intake and output Monitor labs esp. WBC Meticulous skin care Provide emotional support Administer chemotropic agents Prepare client for radiation Prepare client for removal of pituitary tumor if indicated Avoid OTC. ‣ Eat a high fiber diet ‣ Notify HCP if you notice sweet tasting drainage ‣ Surgical removal of the pituitary gland is the treatment of choice. ‣ Hypophysectomy ‣ Adrenalectomy ‣ Ketoconazole ‣ Metyrapone ‣ Reduce steroid therapy ‣ Adhere to fluid and sodium restrictions 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 92 lOMoARcPSD|11334620 93 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.14 NURSE ANGIE 2018 Adrenal cortex disorders: Primary Hyperaldosteronism Hyper-secretion of aldosterone from the adrenal cortex of the adrenal glands. Pathophysiology Assessment The pathophysiology of primary aldosteronism still remains unknown. COMPLICATIONS ‣ Neuromuscular irritability, tetany, and paresthesia ‣ Seizures ‣ Left ventricular hypertrophy, heart failure, and death ‣ Metabolic alkalosis, nephropathy, and azotemia Laboratory Findings: ‣ ‣ ‣ ‣ Decreased Serum potassium levels Elevated Serum sodium levels Urinary specific gravity increased Metabolic alkalosis from elevated Bicarbonate levels H: Hypertension Y: Yes they drink a lot P: Polyuria E: Excretion of potassium R: Reabsorption of sodium GU: Low urine gravity, increased aldosterone levels Heart: Hypertension ENDO: Symptoms of hypokalemia and hypernatremia CNS: Paraesthesia, polydipsia and polyuria, visual changes Treatments ‣ Spironolactone to hold potassium ‣ Potassium supplements ‣ Calcium channel blockers ‣ ACE inhibitors ‣ Thiazide diuretics Surgery ‣ Adrenalectomy INTERVENTIONS Causes ‣ Bartter's syndrome ‣ Benign aldosteroneproducing adrenal adenoma (in 70% of patients) ‣ Bilateral adrenocortical ‣ hyperplasia or carcinoma (rarely) Conditions that produce a sodium deficit ‣ ‣ ‣ ‣ ‣ ‣ ‣ Education Monitor vital signs especially BP. Monitor intake and output. Monitor potassium and sodium. Monitor intake and output. Monitor urine specific gravity. Sodium restriction. Administer glucocorticoid therapy if ordered post adrenalectomy. Avoid OTC medications ‣ Use of diuretics ‣ Weight maintenance ‣ symptoms of hyperkalemia ‣ Medication regimen ‣ When to call the doctor Conditions that reduce ‣ renal blood flow and extracellular fluid volume (renal artery stenosis) ‣ Heart failure ‣ Hepatic cirrhosis with ascitesNephrotic syndrome ‣ 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 93 lOMoARcPSD|11334620 94 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.15 NURSE ANGIE 2018 Adrenal medulla disorders: Pheochromocytoma A catchelcholemine producing tumor usually found in the adrenal medulla. Pathophysiology Assessment Pheochromocytoma is usually a non malignant tumor that causes extreme elevations in blood pressure. They secrete catecholamines from the medullary cells of the adrenal glands which increase metabolism, increases thermogenesis, and heart rate. These patients feel they are in fight or flight. Heart: Paroxysmal HTN, palpitations, chest pain. CNS: Sweating, heat intolerance, tremors and headache, tinnitus, blurred vision, air hunger, impending doom. GI: Abdominal pain, nausea and vomiting. ENDO: Hyperglycemia. 5 H’s: Hypertension Hypermetabolism Hyperglycemia Hyperhidrosis Headache Complications of Pheochromocytoma ‣ ‣ ‣ ‣ ‣ Laboratory Findings: ‣ 24 h urine collection for vanillylmandelic acid ‣ Metanehpirne ‣ Cholecatchimines up to 14 mcg/100 ml of urine ‣ ‣ ‣ ‣ CAUSES INTERVENTIONS Education ‣ PCCs cause the affected adrenal gland to release hormones that cause high blood pressure. If left untreated, a PCC can harm the body, especially the cardiovascular system. ‣ Monitor vitals ‣ Monitor BP ‣ No smoking, no caffeine, do not change positions suddenly ‣ Prepare to administer beta blockers ‣ Monitor serum glucose ‣ High calorie, vitamin, and mineral diet Avoid OTC. • Eat a high calorie diet • Avoid caffeine and Hypertensive crisis Hypertensive retinopathy Nephropathy Heart failure Increased platelet aggregation Stroke Heart enlargement MI EKG changes smoking because of vasoconstriction 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 94 lOMoARcPSD|11334620 95 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.8 NURSE ANGIE 2018 Pancreatic Disorders: Diabetic ketoacidosis A life threatening complication of type 1 diabetes. Develops when severe insulin deficits occur. Pathophysiology Assessment Occurs when a person with type 1 diabetes becomes dehydrated. As the body produces a stress response, hormones (unopposed by insulin due to the insulin deficiency) begin to break down muscle, fat, and liver cells into glucose (sugar) and fatty acids for use as fuel. F: Fruity breath R: Respirations ( kussmal ) U: Unbalanced electrolytes I: Insulin low T: Tachycardia Treatment Normal saline or 0.45% NaCl Regular insulin IV Potassium as soon as kidney function is satisfactory. 02 depending on respiratory status. Sodium bicarb pending ABG’s. Hyperglycemia Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Can be caused by stress, injury, infection, food, too little insulin, thirst, decreased BP, Loc changes, hot dry skin, poor turgor, fruity breath, potential ketoacidosis Serum glucose > 300 mg/dl Osmolality: Varies Serum ketones: Positive Serum PH < 7.35 Serum HCO3 <15 mEq/ L Serum NA : Low, normal or high Serum K: Normal, elevated with acidosis and low with dehydration BUN >20 mg/dl due to dehydration Creatinine: >1.5mg/dl due to dehydration Urine Ketones: Positive CAUSES ‣ Infection ‣ Illness can cause your body to produce higher levels of certain hormones, such as adrenaline or cortisol. ‣ Pneumonia ‣ Urinary tract infections EDUCATION ‣ Take insulin or oral anti diabetic meds as prescribed ‣ Test urine ketones every 3-4 hours ‣ Soft foods 6-8 times a day ‣ Consume liquids every 30 minutes iv excess vomiting or diarrhea occur ‣ Educate the client on the signs and symptoms of hyperglycemia ‣ Notify the HCP if blood glucose levels exceed 250-300 mg/ dl ‣ Ketonuria over 24hrs INTERVENTIONS ‣ Monitor vitals ‣ Monitor i&O ‣ Monitor potassium and glucose ‣ Monitor for signs of ICP 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Hypoglycemia Excess insulin, lack of food, alcohol, overexertion. Increased respirations, decreased bp, increased HR, hunger, anxiety, confusion, cold and clammy skin, weakness, blurred vision seizures. 95 lOMoARcPSD|11334620 96 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.7 NURSE ANGIE 2018 pancreatic disorders: Diabetes mellitus A permanent disorder of food metabolism where the amount of insulin required by the body and the amount of insulin produced is inconsistent causing a rise in blood glucose. Pathophysiology Assessment The beta cells of the pancreas produce insulin and protein where they are stored and released into the bloodstream as blood glucose levels become elevated. When there is an insulin deficit essential nutrients can not cross the cell membrane. ‣ Heart: CAD, PVD, HTN ‣ CNS: Retinopathy, cataracts, paraesthesia ‣ RESP: Pulmonary edema, frothy sputum, sob, infections, decreased bronchomotor tone, pulmonary HTN ‣ GU/GI: Kidney failure ‣ MS: Muscle wasting, weight loss, thin limbs with fatty deposits around the face , neck and abdomen ‣ DERM: Feet and leg ulcers, unhealed or infected wounds ‣ Reproduction: Erectile dysfunction, decreased vaginal lubrication, decreased libido Medications TYPES ‣ TYPE 1: Insulin dependent, “juvenile” usually acute onset, balance meds, nutrition, activity and accucheck QID. ‣ TYPE 2: Oral or injectable insulin, may be regulated with nutrition, gradual onset, monitor BG as ordered. ‣ Gestational: Develops during pregnancy from an increase in the production of hormones. ‣ Surgical: Surgery on the pancreas can cause organ dysfunction. Laboratory Findings: ‣ ‣ ‣ ‣ Hemoglobin (A1C) Under 6% Urinalysis: glucose in the urine Random blood sugar test: Under 200 mg/dl Fasting blood sugar test: Less than 100 mg/dL (5.6 mmol/L) is normal, If it's 126 mg/dL (7 mmol/L) or higher on two separate tests, you have diabetes. ‣ Oral glucose tolerance test: A reading of more than 200 mg/dL (11.1 mmol/ L) after two hours indicates diabetes. 3 P’s: Polydipsia, polyuria, polyphagia INTERVENTIONS CAUSES ‣ ‣ ‣ ‣ ‣ Genetic Autoimmune disorders Lifestyle Type 1: Contributed to an autoimmune response causing beta cells to not be produced leading to no insulin production. Type 2: Onset is accelerated by obesity and sedentary lifestyle, there is little or no insulin production. EDUCATION ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Eliminate smoking Med administration Rotate injection sites Monitor blood glucose as ordered Regulate diet Skin and foot care Sick days guidelines Know s/s of hyper/ hypoglycemia ‣ Give regular insulin ‣ Balance fluids ‣ Electrolyte replacement ‣ ‣ ‣ ‣ ‣ ‣ Calorie restriction Count carbs 50-60% Low protein low sodium Artificial sweeteners Increase fiber For hypoglycemia give OJ, graham crackers, sugar candy ‣ Ensure your client eats a carb after taking insulin & before they workout 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) SubQ ‣ Humalog, lispro : Rapid acting, 15min onset, .5-1.5hr peak, 2-6 hour duration give 5-15 min after meals. ‣ Humulin R, Regular: Short acting, 30-60 min onset, 2-3 hr peak, 3-10 hr duration give 30 min after meals. ‣ Humulin N, NPH: Intermediate acting, 2-4 hr onset, 3-10hr peak, 10-18 hr duration. ‣ Lantus : All day insulin, no peak, lasts 24 hr. Oral ‣ Sulfonylureas: slows the release of insulin from the pancreas. ‣ Alpha-glucosidase inhibitors: slows carb breakdown in the small intestine. ‣ Biguanides: Decrease hepatic glucose output. ‣ Thiazolidinediones: Decrease insulin resistance ‣ Byetta: used to improve glycemic control. 96 lOMoARcPSD|11334620 97 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.9 NURSE ANGIE 2018 Pancreatic Disorders:Diabetic Hyperglycemic Hyperosmolar Nonketotic Syndrome A complication of type 2 Diabetes Mellitus. It involves extremely high blood sugar (glucose) level without the presence of ketones. Assessment Pathophysiology Ketosis and acidosis do not occur with HHNS. Enough insulin is made to prevent the breakdown of fat, thus preventing ketosis. ‣ Blood sugar level of 600 milligrams per deciliter (mg/dL) or 33.3 millimoles per liter (mmol/L) or higher. ‣ Excessive thirst. ‣ Dry mouth. ‣ Increased urination. ‣ Warm, dry skin. ‣ Fever. ‣ Drowsiness, confusion ‣ Hallucinations. Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Serum glucose > 800 mg/dl Osmolality: > 350 mOsm/ L Serum ketones: Negative Serum PH >7.4 Serum HCO3 >20 mEq/ L Serum NA: Low, normal Serum K: Normal, low BUN >20 mg/dl Creatinine: >1.5mg/dl Urine Ketones: Negative CAUSES ‣ Infection ‣ Illness can cause your body to produce higher levels of certain hormones, such as adrenaline or cortisol. ‣ Pneumonia ‣ Urinary tract infections Treatment EDUCATION ‣ Take insulin or oral antidiabetic meds as prescribed ‣ Test urine ketones every 3-4 hours ‣ Soft foods 6-8 times a day ‣ Consume liquids every 30 minutes iv excess vomiting or diarrhea occur ‣ Educate the client on the signs and symptoms of hyperglycemia ‣ Notify the HCP if blood glucose levels exceed 250-300 mg/ dl ‣ Ketonuria over 24hrs INTERVENTIONS ‣ Monitor vitals ‣ Monitor i&O ‣ Monitor potassium and glucose ‣ Monitor for signs of ICP 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Normal saline or 0.45% NaCl ‣ Regular insulin IV less critical role than in DKA ‣ Potassium as soon as kidney function is satisfactory. ‣ 02 depending on respiratory status. 97 lOMoARcPSD|11334620 98 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.10 NURSE ANGIE 2018 Pituitary Disorders:Diabetes Insipidus Most common pituitary disorder resulting from a deficit of ADH. Pathophysiology Assessment Diabetes insipidus is a dysfunction in levels of antidiuretic hormone (ADH), also known as vasopressin. Produced in the hypothalamus and stored in the pituitary gland, ADH helps to regulate the amount of fluid in the body. The disease cannot be controlled by limiting fluid intake, because the high-volume loss of urine continues even without fluid replacement. Complications ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Hypovolemia Hyperosmolality Circulatory collapse Loss of consciousness CNS changes Bladder distention Hydroureter Hydronephrosis Laboratory Findings: ‣ ⬆Hemoglobin and Hematocrit. ‣ ⬆BUN. ‣ ⬆Urine output with low gravity less than 1.010. ‣ The fluid deprivation test is carried out by withholding fluids for 8 to 12 hours or until 3% to 5% of the body weight is lost CAUSES ‣ Head injury ‣ Pituitary tumor ‣ Craniotomy INTERVENTIONS Education ‣ Monitor fluids and electrolytes ‣ Prevent constipation ‣ Record strict intake and output ‣ Monitor skin integrity ‣ Daily weights ‣ Monitor blood pressure, pulse, and temp ‣ Signs and symptoms of hyponatremia ‣ Signs and symptoms of dehydration ‣ Monitor weight ‣ Drink water 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ ‣ ‣ ‣ ‣ ‣ H: Hypotension E: Excess urination P: Poor turgor E: Excess thirst E: Extra dry mucous membranes ‣ S: Skin turgor poor Treatments ‣ Desmopressin acetate nasal spray ‣ Vasopressin tannate: Sub Q or IM injection ‣ Chlorpropamide ‣ Thiazide diuretics ‣ Prostaglandin inhibitors Classifications Nephrogenic diabetes insipidus: Is the inability of the kidneys to respond to AVP results in functional AQP deficiency. Resulting in affected patients having constant diuresis and producing large volumes of dilute urine. Primary diabetes insipidus: Known as dipsogenic diabetes insipidus or psychogenic polydipsia. This can cause excretion of large volumes of dilute urine. Primary Polydipsia can be the result of abnormal thirst caused by damage to the thirst mechanism, in the hypothalamus. Drug related diabetes insipidus: Some drugs, such as lithium or antiviral medications such as, cidofovir and foscarnet (Foscavir) can also cause nephrogenic diabetes insipidus. 98 lOMoARcPSD|11334620 99 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.11 NURSE ANGIE 2018 Pituitary Disorders: siadh A condition in which excess ADH is released but not needed. Pathophysiology Assessment A disorder of impaired water excretion caused by the inability to suppress the secretion of antidiuretic hormone (ADH) causing electrolyte imbalances ( dilutional hyponatremia) & fluid volume excess. Complications ‣ Water intoxication ‣ Cerebral edema ‣ Severe hyponatremia ‣ Heart failure ‣ Seizures ‣ Coma ‣ Death B: Weight gain ( bloated) L: Long time between voids O: Overabundance ADH A: Anorexia T: Tachycardia E: Electrolyte imbalance D: Disorientation Meds that cause SIADH ‣ ‣ ‣ ‣ Vinchristine Phenothiazines Nicotine Thiazide diuretics Medical Management ‣ ‣ ‣ ‣ Fluid restriction IV Saline Lasix Demeclocycline Laboratory Findings: ‣ Monitor fluid and electrolytes especially serum sodium < 115 mEq/L ‣ Monitor urine osmolality CAUSES ‣ Trauma ‣ Stroke ‣ Lung or pancreas malignancies ‣ Medications ‣ Stress INTERVENTIONS Education ‣ Monitor fluids and electrolytes ‣ Monitor vitals and neuro status ‣ Provide a safe environment ‣ Strict intake and output ‣ Restrict fluid intake ‣ Monitor serum lithium levels if indicated ‣ demeclocycline may take up to 1 week to work ‣ Weigh self daily ‣ Alcohol withdrawal ‣ Hypothyroidism 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 99 lOMoARcPSD|11334620 100 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.1 NURSE ANGIE 2018 Thyroid disorders :Hypothyroidism Disease of the thyroid characterized by low secretion of thyroid hormone and decreased rate of metabolism Pathophysiology Assessment Decreased thyroid hormone production is the most common cause of hypothyroidism. Decreased production of T4 causes an increase in the secretion of TSH by the pituitary gland. COMPLICATIONS ‣ ‣ ‣ Myxedema coma: Rare but serious. Results from persistently low thyroid production Assessment: Hypotension, bradycardia, hypothermia, hyponatremia, hypoglycemia, general edema, respiratory failure, cardiovascular collapse, shock, coma. Interventions: Maintain patent, institute aspiration precautions, IV hypertonic saline, administer levothyroxine IV, IV glucose, corticosteroids, assess hourly temp, keep the client warm, monitor LOC and electrolytes/ glucose. ‣ Atrophy of thyroid gland ‣ ‣ Radioactive iodine, Iodine compounds,Iodine deficiency and iodine excess ‣ ‣ ‣ Thyroidectomy is the most common cause. ‣ ‣ ‣ Treatments ‣ Hormone replacement Synthroid, levothroid: Monitor cardiovascular status, can cause dysrhythmias and tachycardia. Meds that can alter Thyroid lab tests INTERVENTIONS ‣ C: Constipation O: Orbital edema L: Lethargy / low BMR D: Dry skin ‣ Lithium, Antithyroid medications ‣ Radiation related to head and neck cancers ‣ Infiltrative diseases of the thyroid (amyloidosis, scleroderma, lymphoma) ‣ T3 Resin Uptake Test: Indirect measure of unsaturated TBG Normal value: 25% to 35% < than 35% hyperthyroid, >25% hypothyroid. ‣ Thyroid Antibodies: Antibody titers are normally present in 5% to 10%. Fine-Needle Aspiration Biopsy: Use of a small-gauge needle to sample the thyroid tissue. ‣ Thyroid Scan, Radio Scan, or Scintiscan: Scintillation detector or gamma camera moves back and forth across the area to be studied, commonly used isotopes of iodine are 123 and iodine 131, helpful in determining the location, size, shape, and anatomic function of the thyroid gland, particularly when thyroid tissue is substernal or large. ‣ Serum Thyroglobulin: Used to detect persistence or recurrence of thyroid carcinoma. ‣ Autoimmune disease (Hashimoto’s thyroiditis, post-Graves’ disease) G: Goiter (maybe) E: Edema T: Temperature decrease S: Alopecia Meds that can cause hypothyroidism Laboratory Findings: CAUSES H: Heart failure E: Enlarged heart Education Monitor vital signs esp. HR and rhythm. Administer thyroid medication and monitor for OD. Diet, low calorie, low cholesterol, low saturated fat. Monitor for constipation. Provide a warm environment. Avoid sedatives and opioids as these worsen constipation Support cardiac and respiratory function. Know medication interactions. ‣ Replacement therapy is lifelong ‣ Levothyroxine is to be taken in the AM prior to breakfast do not skip doses ‣ Monitor blood glucose ‣ HRT’S potentiate anticoagulants, antidepressants , and digoxin 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ amiodarone aspirin cimetidine diazepam furosemide Heparin lithium phenytoin and other anticonvulsants propranolol 100 lOMoARcPSD|11334620 101 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.2 NURSE ANGIE 2018 Thyroid disorders: Hyperthyroidism Overproduction of thyroid hormones T3 and T4 and an increased basal rate of metabolism. Pathophysiology Assessment Hyperthyroidism, also called thyrotoxicosis, excess production of thyroid hormone by the thyroid gland. S: Soft skin H: Hypertension E: Exophthalmos (pug eyes) COMPLICATIONS ‣ ‣ ‣ Laboratory Findings: ‣ T3 Resin Uptake Test: Indirect measure of unsaturated TBG. Normal value: 25% to 35% < than 35% hyperthyroid, >25% hypothyroid. ‣ Thyroid Antibodies: Antibody titers are normally present in 5% to 10%. ‣ Fine-Needle Aspiration Biopsy: Use of a small-gauge needle to sample the thyroid tissue. ‣ Thyroid Scan, Radio Scan, or Scintiscan: Scintillation detector or gamma camera moves back and forth across the area to be studied, commonly used isotopes of iodine are 123I and iodine 131, helpful in determining the location, size, shape, and anatomic function of the thyroid gland, particularly when thyroid tissue is substernal or large. ‣ Serum Thyroglobulin: Used to detect persistence or recurrence of thyroid carcinoma. Thyroid storm: An acute life threatening condition in a client with uncontrolled hyperthyroidism. Can be caused by manipulation of the thyroid gland during surgery. anti thyroid meds, beta blockers glucocorticoids can be given before surgery to prevent occurrence. Assessment: Elevated temp, tachycardia, systolic HTN, nausea vomiting and diarrhea, agitation, tremors, seizures, delirium, and coma. Interventions: Maintain open airway and proper ventilation, give antithyroid meds, beta blockers, and glucocorticoids, monitor vitals, monitor EKG for dysrhythmias. G: GI loss (diarrhea) E: Enlarged thyroid gland T: Temperature increases S: Shakiness H: High BMR O: Overproduction of sweat T: Thin (weight loss) Medications that alter Thyroid lab tests ‣ amiodarone ‣ aspirin ‣ cimetidine ‣ diazepam ‣ furosemide ‣ Heparin ‣ lithium ‣ phenytoin ‣ and other anticonvulsants ‣ propranolol Treatments ‣ SSKI ‣ methimazole ‣ Sodium or potassium CAUSES ‣ Graves' Disease ‣ Functioning adenoma and toxic multinodular goiter (TMNG) ‣ Excessive intake of thyroid hormones ‣ Abnormal secretion of TSH. ‣ Thyroiditis (inflammation of the thyroid gland) INTERVENTIONS ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Education ‣ Take medications with meals ‣ Medication should be taken at regular divided doses ‣ Thionamides are taken for 1-2 years ‣ Report jaundice to the HCP right away ‣ Follow instructions on intake of iodine Provide adequate rest Administer sedatives as ordered Make the environment cool and quiet Monitor daily weight Do not give stimulants (caffeine) Administer antithyroid meds as ordered Administer iodine preps as indicated Give propranolol for tachycardia Iodide ‣ PTU ‣ Dexamethasone ‣ Beta blockers ‣ Propylthiouracil ‣ Irradiation ‣ Thyroidectomy ‣ Excessive iodine intake 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 101 lOMoARcPSD|11334620 102 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.3 NURSE ANGIE 2018 Thyroid disorders: Hypoparathyroidism Decreased amounts of parathyroid hormone are secreted from the parathyroid gland. Pathophysiology Assessment Hypoparathyroidism is caused by a parathyroid hormone (PTH) deficiency or resistance, leading to hypocalcemia and hyperphosphatemia. H: Hypotension E: EKG changes S: Spasms bronchus and laryngeal T: Trousseaus I: Irritability G: Great amount of phosphate H: Hypocalcemia T: Tingling Interventions Laboratory Findings: ‣ Positive chvostek’s and trousseau's sign “carpopedal spasm” ‣ Dangerously low calcium levels & High phosphate levels. ‣ X-rays of bone show increased density ‣ Sulkowitch test: Tests for calcium in the urine CAUSES TREATMENTS ‣ Injury to or removal of the parathyroid glands ‣ Radical neck dissection ‣ Parathyroidectomy ‣ DiGeorge syndrome, which is a genetic disorder that affects development of certain body systems ‣ Genetics ‣ Autoimmune disease ‣ Cancer radiation treatment. ‣ Low magnesium levels ‣ Calcium Gluconate IV 1.5-3g/day ‣ Emergency tx: calcium gluconate or chloride over iv over 10-15 mins ‣ Vit D, Calcitriol, ergocalciferol 50,000 to 400,000 units daily ‣ Phenobarbital Education ‣ Take the prescribed amount of vitamin D ‣ Avoid dark green veggies and milk ‣ Increase intake of calcium 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Quiet environment, no drafts bright lights or sudden movements. ‣ Diet high in vitamin D to help absorb calcium, except; No milk or Milk products, or spinach as these contain high amounts of phosphate. ‣ Diet high in calcium and low in phosphate ( green leafy veggies, tofu, soybeans. ‣ Have trach set and suction equipment at bedside. ‣ Initiate seizure precautions. ‣ Prepare to administer calcium gluconate IV. ‣ Prepare to administer phenobarbital to decrease neuromuscular excitability. ‣ Monitor voice for hoarseness, this could indicate damage to the larynx which can be a complication of removal of the parathyroid glands. Nursing Diagnosis ‣ Risk for injury ‣ Knowledge deficit 102 lOMoARcPSD|11334620 103 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.12 NURSE ANGIE 2018 Adrenal cortex disorders: Addison’s Disease Adrenal insufficiency characterized by decreased secretion of adrenal cortex hormones. Pathophysiology Assessment Addison's disease is caused by too little or absent cortisol release from the adrenal cortex. Remember in Addison’s disease you add cortisol. Patients will also have low sodium and increased potassium levels. Medications that can cause a need to increase glucocorticoid dosage ‣ phenytoin (dilantin), barbiturates, rifampin ‣ (Rifadin), and antacids. in addition estrogen inhibits steroid metabolism H: Hypotension E: Emaciation S: Serum sodium and glucose low T: Tan skin A: Alopecia N: No feelings (depression) Treatments ‣ ‣ ‣ ‣ Hydrocortisone IV 5% dextrose in normal saline Vasopressors Antibiotics Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ Skull films CT MRI Elevated potassium levels Plasma cortisol will be low ACTH stimulation test Urinary hydrocortisone and ketocorticoids will decrease CAUSES ‣ Autoimmune disease ‣ Infections such tuberculosis, HIV, or fungal infections. ‣ Hemorrhage into the adrenal glands Complications INTERVENTIONS Education ‣ Monitor vital signs esp. HR and rhythm and intake and output. ‣ Monitor WBC count. ‣ Monitor sodium, potassium and glucose levels. ‣ High protein diet, high carbs and high sodium and low potassium diet. Avoid OTC. ‣ Monitor addisonian crisis caused by stress, trauma or infection. ‣ Client will need life long corticosteroid therapy. ‣ Adverse effects of corticosteroid therapy and prevention techniques ‣ Special instruction for patients who are diabetics and management of blood glucose when taking corticosteroids 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ ADDISONIAN CRISIS : ‣ Acute adrenal insufficiency ‣ Assessment: severe Hypotension, shock, severe lower back, abdominal and leg pain. Severe headache. ‣ Interventions: prepare to administer glucocorticoids IV, hydrocortisone succinate. Then oral glucocorticoids and mineralocorticoids. Monitor BP and neuro status, monitor I&O, monitor sodium, potassium, and glucose. IV fluids, bed rest and quiet environment. Prevent infection. 103 lOMoARcPSD|11334620 104 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.5 NURSE ANGIE 2018 Pituitary disorders: Hyperpituitarism Acromegaly/Giantism Hyper-secretion of growth hormone by the anterior pituitary gland. Pathophysiology Assessment Acromegaly is characterized by hyper-secretion of growth hormone (GH), which is caused by the existence of a secreting pituitary tumor in more than 95% of acromegaly cases. Leads to cushing's diseases. COMPLICATIONS ‣ ‣ ‣ ‣ ‣ ICP Bleeding meningitis Hypopituitarism CSF leak Infection Laboratory Findings: ‣ Insulin-like growth factor-1 (IGF-1): Normally if this is high the body stops producing growth hormone, if growth hormone is present with a high GF1 reading then the client may have acromegaly. ‣ Oral Glucose Tolerance Test (OGTT): Test results similar to GF1 test, GH usually stops being produced when levels are high unless, the client may be suffering from acromegaly. ‣ Pituitary tumor T: Too much pain in joints A: arthritis L: Long hands and feet L: Long protruding jaw Treatments ‣ Hypophysectomy: First line treatment. ‣ NSAIDs: For joint pain. ‣ Somatostatin Analogs (SSAs): Somatostatin analogs are synthetic (manmade) versions of the body's natural hormone somatostatin. ‣ Growth Hormone Receptor Antagonists: They work by blocking GH from doing one of its jobs—making IGF-1. ‣ Dopamine Agonists: Works by stopping the release of GH from the pituitary tumor. Hypophysectomy Education ‣ Removal of a pituitary tumor via craniotomy or transsphenoidal approach. ‣ long-acting forms of somatostatin analogues require I.M. injection approximately every 4 weeks for octreotide and INTERVENTIONS CAUSES H: Hypertension E: Enlarged organs ‘ S: Sweating and oily skin ‣ ‣ ‣ ‣ Provide emotional support Provide frequent skin care Provide pain relief Prepare the client for radiation if planned ‣ Prepare the client for hypophysectomy if planned once every 7 to 14 days for lanreotide ‣ potential adverse effects of dopamine agonists ‣ Avoid activities that increase ICP ‣ Breathe through the mouth if nasal packing is in place 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 104 lOMoARcPSD|11334620 105 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.6 NURSE ANGIE 2018 Pituitary Disorders: Hypopituitarism Hypo-secretion of one or more of the following hormones: LH, FSH, GH, TSH, ACTH, ADH. Pathophysiology Assessment A rare disorder usually caused by a tumor, where your pituitary gland either fails to produce one or more of its hormones or doesn’t produce enough of them causing dwarfism in children. H: Hypotension O: Obesity R: Really bad headaches M: More tired O: Output ( cardiac) decreased N: Non fertile E: Eating uncontrollably S: Sexual dysfunction Treatments ‣ Corticosteroids. These drugs, such as hydrocortisone or prednisone, replace the adrenal hormones that aren't being produced because of an adrenocorticotropic hormone (ACTH) deficiency. ‣ Levothyroxine (Levoxyl, Synthroid, others). ‣ Sex hormone replacement. ‣ Growth hormone replacement. Dwarfism ‣ Synthetic thyrotropinreleasing hormone (TRH) Laboratory Findings: ‣ ‣ ‣ ‣ CT or MRI, with contrast Free T4 and TSH levels ACTH stimulation test Insulin tolerance test CAUSES ‣ Head trauma ‣ Pituitary tumors ‣ Encephalitis ‣ Autoimmunity ‣ Stroke INTERVENTIONS EDUCATION ‣ Provide emotional support. ‣ Client may need hormone replacement. ‣ Monitor blood glucose for hyperglycemia ‣ Monitor for pituitary apoplexy ‣ Daily weights ‣ Prep for surgery if a tumor is involved ‣ Children will reach their adult height just at a slower pace ‣ Growth hormone is given subcutaneously ‣ Educate the client on need for extra cortisone if they become over stressed or a fever of over 101.1 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Dwarfism can be caused by any of more than 200 conditions. Causes of proportionate dwarfism include metabolic and hormonal disorders such as a growth hormone deficit. Dwarfism Assessment ‣ A large head with a prominent forehead ‣ A flattened bridge of the nose ‣ Protruding jaw ‣ Crowded and misaligned teeth ‣ Forward curvature of the lower spine ‣ Bowed legs ‣ Flat, short, broad feet ‣ "Double-jointedness" 105 lOMoARcPSD|11334620 106 MEDICAL SURGICAL NURSING: ENDOCRINE 1.8.4ß NURSE ANGIE 2018 Thyroid disorders: Hyperparathyroidism Increased amounts of parathyroid hormone are secreted from the parathyroid gland. Pathophysiology Assessment H: Hypertension E: Epigastric pain Hyperparathyroidism is caused by a parathyroid hormone(PTH) overproduction leading to hypercalcemia and hypophosphatemia. Complications ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Osteoporosis Subchondral fractures Traumatic synovitis Renal calculi and colic Renal insufficiency and failure Cholelithiasis Cardiac arrhythmias Vascular damage Hypertension Heart failure Muscle atrophy Depression F: Fatigue E: Electrolyte imbalances L: Low phosphate L: Low bone density F: Fractures A: Anorexia S: Stones ( renal) T: Tender bones Treatments ‣ IV furosemide and saline to promote calcium excretion ‣ IV phosphate for rapid lowering of calcium ‣ Bisphosphonate to increase bone density ‣ Parathyroidectomy Laboratory Findings: ‣ ‣ ‣ ‣ ‣ Dangerously high calcium levels above 10.2 mg/dl. Decreased phosphate levels less than 4.5 mg/dl. X-rays of bone show decreased density. DEXA bone scan. Sulkowitch test: test for calcium in the urine. Nursing Diagnosis INTERVENTIONS CAUSES ‣ Benign tumor ‣ Vitamin D deficit ‣ Long term Kidney disease Education ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Relieve pain Prevent formation of renal calculi Increase fluid intake Offer acid ash diet Prevent fractures Promote body alignment Safety precautions Monitor potassium levels counteracts calcium on cardiac muscles ‣ Parathyroidectomy care ‣ Increase fluids ‣ Decrease calcium intake ‣ Signs and symptoms of hypercalcemia ‣ Symptoms of respiratory distress ‣ Need for blood testing fro electrolyte levels ‣ avoid calcium-containing antacids and thiazide diuretics 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Risk for injury ‣ Impaired urinary elimination ‣ Nutrition less than body requirements ‣ Constipation 106 lOMoARcPSD|11334620 107 MEDICAL SURGICAL NURSING: EYES 1.8.1 NURSE ANGIE 2018 Legal Blindness A visual acuity of 2/200 or less in the effected eye Pathophysiology Complications ‣ Injury ‣ Sensory deprivation occurs when a person has central visual acuity (vision that allows a person to see straight ahead of them) of 20/200 or less in his or her better eye with correction. With 20/200 visual acuity, a person can see at 20 feet, what a person with 20/20 vision sees at 200 feet. CAUSES ‣ Glaucoma ‣ Cataracts ‣ Macular degeneration ‣ Head injury ‣ Hypertensive retinopathy ‣ Diabetic retinopathy ‣ Retinal vascular occlusion ‣ Increased intracranial pressure INTERVENTIONS EDUCATION ‣ Use a normal tone of voice ‣ Speak before approaching ‣ Allow the patient to use touch to orient to the room ‣ Use the clock to describe placement on the plate at meal times ‣ Provide radios, television and clocks that tell time orally provide a braille watch ‣ Allow the patient to hold on to you when ambulating ‣ Instruct the client to use assistive devices ‣ Support groups ‣ To sweep the cane prior to taking a step ‣ Instruct on proper cane use General Eye Assessment ‣ PERRLA ‣ Cardinal fields of gaze ‣ Confrontation ‣ Visual acuity ‣ Accommodation ‣ Corneal light reflex ‣ Sclera color ‣ Conjunctiva color ‣ Look for strabismus and nystagmus ‣ Eyebrows ‣ Eyelids and lashes ‣ Eyeballs ‣ Bulbar Conjunctiva and Sclera ‣ Palpebral Conjunctiva (stressful and uncomfortable usually done only if a complaint) Eversion of the Upper Lid ‣ Lacrimal Apparatus ‣ Use braille ‣ Provide a safe environment by removing trip hazards 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 107 lOMoARcPSD|11334620 108 MEDICAL SURGICAL NURSING: EYES 1.8.3 NURSE ANGIE 2018 Cataracts Opacity of the lens that distorts the image projected into the retina Pathophysiology Risk Factors The lens loses its transparency through degenerative changes in the crystalline cell structure. The clouded lens blocks light shining through the cornea. Images cast onto the retina are blurred. The brain interprets a hazy image. ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Age Smoking Use of alcohol Prolonged exposure to sunlight Intrauterine infection Exposure to ionizing radiation such as X-rays or cancer radiation treatment Occupation involving infrared energy Metabolic syndrome Diabetes Corticosteroid use Long-term use of antidepressants Complications ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Priority! Assess for complaints of a sudden increase in pain, accompanied by restlessness and increased pulse rate, which may signal increased intraocular pressure. CAUSES ‣ Aging ‣ Heredity ‣ Trauma INTERVENTIONS Complete vision loss Infection Loss of vitreous fluid Wound dehiscence Hyphema Pupillary block glaucoma Retinal detachment Macular or corneal edema Bleeding Dislocated intraocular lens EDUCATION ‣ Lens extraction ‣ Extracapsular cataract extraction ‣ Intracapsular cataract extraction (rarely used in the United States) ‣ Phacoemulsification ‣ Monitor for pain ‣ Monitor for increased discharge ‣ Do not bend at the waist ‣ Avoid sneezing ‣ Wear eye shield ‣ Do not touch eye 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) Assessment ‣ Milky white pupil on inspection with a penlight ‣ Grayish white area behind the pupil Red reflex lost ‣ Change in color of lens (may appear slightly yellow or brown) Poor vision overall (cloudy, blurred or dim) ‣ Painless, gradual vision loss ‣ Colors seem faded ‣ Blinding glare from headlights with night driving; halo may appear around lights ‣ Poor reading vision ‣ Annoying glare from sun or lights ‣ Poor vision in bright sunlight ‣ Better vision in dim light than in bright light (central opacity) Medications ‣ ‣ ‣ ‣ Corticosteroids NSAIDS Antibiotics Mydriatics 108 lOMoARcPSD|11334620 109 MEDICAL SURGICAL NURSING: EYES 1.8.1 NURSE ANGIE 2018 Refractive Errors Refraction is the bending go light rays any problem with eye length can lead to reaction errors Pathophysiology Myopia: Near sightedness, refraction is too strong. Bent images fall on the retina. Risks ‣ Older age ‣ Young age ‣ Genetics Astigmatism: irregular curvature of the cornea, images are focused at two points in the retina Hyperopia : farsightedness, refraction is too weak. Image is focused behind the retina Presbyopia: Loss of elasticity in the lens related to the aging process. Images fall behind the retina Complications ‣ Complications are usually related to surgery. ‣ Inability to read up close or far away ‣ Fatigue ‣ Grades may go down Assessment ‣ Diagnosed with a process known as refraction. ‣ An eye chart is viewed while various lenses with different strengths are systematically placed in front of the eye. Image will sharpen or blur ‣ decrease distance visual acuity (VA) ‣ squinting ‣ near visual acuity is often okay but PT may need to hold books closer Surgical intervention CAUSES The eyes inability to bend light and focus clearly on the retina INTERVENTIONS EDUCATION ‣ Eyeglasses ‣ Contacts ‣ Educate on post operative interventions ‣ Radial keratotomy ‣ Photo refractive keratotomy ‣ LASIK ‣ Corneal ring ‣ Avoid bright light ‣ Avoid sneezing 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 109 lOMoARcPSD|11334620 110 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.7 NURSE ANGIE 2018 Peritonitis Acute inflammation of the peritoneum Pathophysiology Bacteria invade the peritoneum after inflammation and perforation of the GI tract. Fluid containing protein and electrolytes accumulates in the peritoneal cavity.Peristalsis slows or stops.Respiratory problems can result from abdominal distention caused by fluid shifts to the peritoneal cavity. Assessment Risks ‣ ‣ ‣ ‣ ‣ ‣ Peritoneal dialysis History of cirrhosis Appendicitis Crohn disease Peptic ulcer disease History of peritonitis ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Complications ‣ ‣ ‣ ‣ ‣ ‣ Abscess, fistula formation Septicemia Respiratory compromise Bowel obstruction Shock Liver failure ‣ ‣ Rigid board-like abdomen Fever Tachycardia Hypotension Shallow breathing Change in mental status Signs of dehydration Positive bowel sounds (early); absent bowel sounds (later) General abdominal tenderness Rebound tenderness, guarding Typical patient positioning: Lying very still with knees flexed Treatments Labs & Diagnostics ‣ Abdominal x-ray ‣ Peritoneal lavage Elevated WBC Blood cultures CAUSES ‣ Bacterial or chemical inflammation ‣ GI tract perforation (from ‣ appendicitis, diverticulitis, peptic ulcer, or ulcerative colitis) ‣ Ruptured ectopic pregnancy ‣ Peritoneal dialysis INTERVENTIONS EDUCATION ‣ Daily weights ‣ Pain management ‣ Monitor vitals ‣ Wound care, drains ‣ Monitor I & O ‣ Signs of infection ‣ Positioning ‣ Broad-spectrum I.V. antibiotics based on the infecting organism ‣ Nasogastric (NG) intubation ‣ Correction of the underlying condition Nothing by mouth (NPO) until bowel function returns ‣ Gradual increase in diet ‣ Total parenteral nutrition if necessary Bed rest until the condition improves ‣ Semi-Fowler position ‣ Avoidance of lifting for at least 6 weeks postoperatively ‣ Assess bowel sounds 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 110 lOMoARcPSD|11334620 111 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.6 NURSE ANGIE 2018 Appendicitis Inflammation of the vermiform appendix, a bulge from the apex of the cecum Pathophysiology Risks ‣ Low fiber, high carbohydrate diet ‣ Family history ‣ Gastrointestinal infection ‣ Inflammatory bowel disease Mucosal ulceration triggers inflammation, which temporarily obstructs the appendix.increasing pressure in the distended appendix; the appendix then contracts. Fluids and mucus continue to be secreted and stagnate. Continued inflammation, pressure, and fluid collection can lead to perforation and spillage of the appendiceal contents into the peritoneal cavity. Complications ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Peritonitis (most common) Wound infection Dehiscence Intra-abdominal infection Fecal fistula Intestinal obstruction Incisional hernia Paralytic ileum Abdominal or pelvic abscess Death (rare) Labs & Diagnostics ‣ Elevated WBC count ‣ Ct showing enlarged appendix ‣ Ultrasound shows enlarged appendix CAUSES ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Barium ingestion Fecal mass Foreign body Mucosal ulceration Neoplasm Stricture Viral infection Inflammatory bowel disease INTERVENTIONS EDUCATION ‣ Monitor Vital signs ‣ Advance diet as tolerated ‣ Signs of shock ‣ Splinting surgical site ‣ Assess pain ‣ Turn cough deep breathe ‣ Monitor bowels ‣ Early ambulation ‣ Monitor surgical site ‣ I/S Assessment ‣ Periumbilical abdominal pain ‣ Rebound pain when pressure on the abdomen is released quickly ‣ Guarding ‣ Rigidity ‣ Fever ‣ Nausea, vomiting ‣ Right lower quadrant pain Treatments ‣ Surgical removal of the appendix ‣ NPO ‣ IV fluids ‣ Pain medication ( use cautiously to to maintain awareness of possible rupture) ‣ Antibiotic therapy Never apply heat to the right lower abdomen; this can cause the appendix to rupture. ‣ Monitor for signs of infection 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 111 lOMoARcPSD|11334620 112 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.5 NURSE ANGIE 2018 Ulcerative Colitis Ulceration and inflammation of the bowel that causes poor absorption of nutrients Pathophysiology Risks • Ulceration and inflammation of the bowel that causes poor absorption of nutrients. The colon becomes a rigid, foreshortened tube.In severe ulcerative colitis, areas of hyperplastic growth occur with swollen mucosa surrounded by inflamed mucosa with shallow ulcers.submucosa and circular and longitudinal muscles may be involved. • • • • Stress (may increase the severity of an attack and precipitate exacerbations) Family history Ashkenazi Jewish ancestry Nonsteroidal antiinflammatory drug use Dairy products Complications • • • • • • • • • • • • Labs & Diagnostics Nutritional deficiencies Perineal sepsis Anal fissure or fistula Perirectal abscess Perforation of the colon Hemorrhage Anemia Toxic megacolon Cancer Coagulation defects Arthritic diseases Death ‣ Perinuclear antineutrophil cytoplasmic antibody assay is positive in 60% to 80% of patients with ulcerative colitis. Medical treatment ‣ Hemoglobin : decrease ‣ Stool specimen analysis reveals blood, pus, and mucus, but no pathogenic organisms and is done to exclude other causes. ‣ ESR: elevated CAUSES May be related to an abnormal immune response in the GI tract, environmental factors, and possibly genetic factors. Assessment ‣ Liquid stools with visible pus, mucus, and blood ‣ Possible abdominal distention ‣ Abdominal tenderness ‣ Perianal irritation ‣ Jaundice ‣ Joint pain ‣ Tachycardia ‣ Fever ‣ Mild cramping and lower abdominal pain ‣ Recurrent bloody diarrhea as often as 25 times daily ‣ Nocturnal diarrhea ‣ Tenesmus ‣ Arthralgia ‣ Rectal urgency ‣ Occasional fecal incontinence MONITOR EDUCATION Vital signs Patients with active signs and symptoms of ulcerative colitis shouldn't undergo barium enemas because of the risk of precipitating toxic megacolon. • Nothing by mouth (if severe) • Well-balanced diet with adequate fluid intake • Parenteral nutrition (with severe disease) Pain, infection Fluid balance , nutritional status Electrolytes Bowel sounds , weights Stool characteristics 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ 5-ASA: Aminosalicylates, Sulfasalazine, Olsalazine, Mesalazine, Balsalazide ‣ Corticosteroids: Prednisone, prednisolone Methylprednisone, hydrocortisone (IV corticosteroid therapy) ‣ Immunosuppresants: Azathioprine, Cyclosporine Hospitalization if drug therapy does not work Low residue diet 112 lOMoARcPSD|11334620 113 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.8 NURSE ANGIE 2018 Colon Cancer Malignant tumor of the colon. Pathophysiology A premalignant lesion progresses to invasive adenocarcinoma that most often involves genetic alterations. Tumors tend to grow slowly and remain asymptomatic for a long time. Risks Assessment ‣ Smoking or tobacco use ‣ Excessive intake of saturated animal fat ‣ Age older than 50 ‣ History of inflammatory bowel disease ‣ Type 2 diabetes ‣ Family history of colon cancer ‣ Low-fiber diet ‣ Diet high in red meat or processed meats ‣ Obesity ‣ Sedentary lifestyle ‣ Alcohol use ‣ Black race ‣ Abdominal distention or visible mass ‣ Enlarged abdominal veins ‣ Abnormal bowel sounds ‣ Abdominal mass Generalized abdominal tenderness ‣ Right colon cancers: tend to be asymptomatic until palpable mass in lower right quadrant and blood mixed with stool becomes visible ‣ Left colon tumors produce pencil- Complications ‣ Anemia ‣ Rectal bleeding ‣ Bowel obstruction (left-sided tumors) ‣ Postoperative infection, stricture, abscess formation, pneumonia ‣ Adverse effects of chemotherapy or radiation Labs & Diagnostics ‣ Fecal occult blood test: may show blood in stools, ‣ Carcinoembryonic antigen may be elevated; permit patient monitoring before and after treatment to detect metastasis or recurrence. CAUSES ‣ Genetics ‣ Ulcerative colitis ‣ Iron deficiency anemia may be present. ‣ Computed tomography scanning (abdomen and pelvis) determines stage. Transrectal ultrasonography determines extent of rectal lesions. INTERVENTIONS EDUCATION ‣ Monitor Stool ‣ Diet Education ‣ Adverse effects of chemotherapy or radiation ‣ Diet high in whole grain fibers, vegetables, and fruits and low in processed meatsRadiation preoperatively and postoperatively to induce tumor regression ‣ Radio-frequency or ethanol ablation therapy ‣ Smoking cessation 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) shaped stool Treatments ‣ Chemotherapy, such as fluorouracil, oxaliplatin, irinotecan hydrochloride ‣ Targeted therapy: bevacizumab, ramucirumab, zivaflibercept ‣ Proctoscopy or sigmoidoscopy (flexible) permits visualization of the lower GI tract and can detect up to 66% of colorectal cancers. ‣ Colonoscopy permits visual inspection and photography of the colon up to the ileocecal valve and provides access for polypectomies and biopsies of suspected lesions. 113 lOMoARcPSD|11334620 114 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.2 NURSE ANGIE 2018 Gastritis Localized or patchy inflammation or erosion of the gastric mucosa Pathophysiology Localized or patchy inflammation or erosion of the gastric mucosa.May be acute (erosive or non erosive) or chronic, reactive, atrophic, reflux, hemorrhagic, or infectious. Most common stomach disorder (acute). ACUTE: The protective mucosal layer is altered due to a causative agent or factor. Acid secretion produces mucosal reddening, edema, and superficial surface erosion. CHRONIC: Gastric mucosa progressively thins and degenerates. Assessment Risks Age older than 55 Exposure to toxic substances Hemodynamic disorder Alcohol abuse Ingestion of NSAIDs, including aspirin ‣ Smoking ‣ Stress ‣ Peptic ulcer disease ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Achlorhydria Hypochlorhydria Hyperchlorhydria Grimacing Restlessness Pallor Tachycardia Hypotension Abdominal distention, tenderness, and guarding ‣ Normoactive to hyperactive bowel sounds ‣ Possible positive fecal occult blood test results Medical Treatment • Complications Hemorrhage, anemia Dehydration Obstruction ‣ ‣ ‣ Labs & Diagnostics ‣ Perforation Peritonitis ‣ Gastric cancer ‣ Peptic ulcer • • • ‣ Atrophic gastritis ‣ Occult blood found in vomitus or stools (or both) indicates gastric bleeding. ‣ Hemoglobin (Hb) level and hematocrit may be decreased. ‣ Urea breath test or H. pylori stool antigen test indicates the presence of H. pylori . • • • CAUSES ‣ ‣ ‣ ‣ ‣ Helicobacter pylori (H. pylori) infection Autoimmune response Damage to the stomach lining Crohn disease, sarcoidosis food allergies infections with viruses, parasites, fungi, and bacteria INTERVENTIONS EDUCATION ‣ Nothing by mouth if bleeding occurs ‣ Elimination of irritating foods, ‣ ‣ ‣ ‣ ‣ Elimination of irritating foods, such as caffeine and spicy foods ‣ prescribed drug therapy ‣ Avoidance of NSAIDS ‣ Antacids 1 hour after meals ‣ Avoid alcohol ‣ such as caffeine and spicy foods, or of irritating drugs Reduce anxiety Maintain fluid balance Pain relief Nutritional support 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) • • • • Elimination of cause (such as treatment of H. pylori with antibiotic, discontinuation of NSAIDs) Stomach acidreducing medications Smoking cessation Venous thromboembolism (VTE) prophylaxis if the patient is hospitalized For massive bleeding: Blood transfusion Iced saline lavage Angiography with vasopressin Histamine-2 (H2) receptor antagonists, such as cimetidine (Tagamet), ranitidine hydrochloride (Zantac), famotidine (Pepcid), and nizatidine (Axid) Antibiotics Antacids, such as aluminum and magnesium hydroxide Sucralfate (Carafate) Omeprazole (Prilosec) 114 lOMoARcPSD|11334620 115 MEDICAL SURGICAL NURSING: GASTRLOINTESTINAL 1.3.1 NURSE ANGIE 2018 GERD Characterized by backflow of gastric contents into the esophagus. Pathophysiology Presenting Symptoms Gastric motility is slowed which causes a delay in clearance of stomach acid. Gastric emptying is delayed which causes an increased volume of gastric fluids. Reflux occurs when the lower esophageal sphincter pressure is deficient . The lower esophageal sphincter relaxes causes Risks regurgitation of stomach contents into the esophagus Fatty foods Alcohol Anticholinergic drugs Morphine Calcium channel blockers Nasogastric (NG) intubation for more than 4 days ‣ Obesity, Smoking ‣ Connective tissue disorders ‣ ‣ ‣ ‣ ‣ ‣ • • • • • • • • • Pyrosis Dyspepsia Regurgitation Dysphagia Odynophagia Hypersalivation Esophagitis Think burning and trouble eating. Symptoms may mimic a heart attack Complications Peptic stricture Reflux esophagitis Esophageal stricture Esophageal ulcer Barrett esophagus Anemia from esophageal bleeding ‣ Reflux aspiration leading to chronic pulmonary disease ‣ ‣ ‣ ‣ ‣ ‣ Labs & Diagnostics • Esophageal acidity test reveals degree of gastroesophageal reflux. • Esophagoscopy and biopsy results confirm pathologic changes in the mucosa. Esophagogastroduodenoscopy reveals evidence of esophagitis. • CAUSES ‣ Laying flat ‣ Hiatal Hernia ‣ Pyloric surgery ‣ Pregnancy INTERVENTIONS Medications • Histamine h2 antagonist: famotidine, nizatidine, ranitidine. • Proton Pump Inhibitors: lansoprazole, rabeprazole, esomeprazole are used to decrease gastric secretions • Prokinetic agents: accelerate gastric emptying. Bethanechol, domperidone EDUCATION ‣ Elevate HOB 30 degrees ‣ No lying down for 2 to 3 ours after eating ‣ Avoid late night eating ‣ Evaluation of effectiveness of medications ‣ observing for adverse effects of medications ‣ ‣ Eat a diet low in fat and to avoid caffeine,tobacco, milk, beer, carbonated drinks, mint. Avoid eating or drinking 2 hours before bedtime ‣ Maintain normal body weight ‣ Avoid tight clothes ‣ Elevate the head of the bed and upper body 6-8’’ 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 115 lOMoARcPSD|11334620 116 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.3 NURSE ANGIE 2018 Irritable Bowel Syndrome A widespread condition involving recurrent abdominal pain and diarrhea or constipation Pathophysiology Assessment IBS manifests from a functional disorder of the bowel. Neuroendocrine changes may cause motility issues within the intestines however, there is no inflammation or tissue changes in the intestinal mucosa. Risks ‣ Young age ‣ female gender ‣ family history ‣ Alternating between constipation and diarrhea ‣ Pain ‣ ‣ mental health issues. Complications Poor quality of life Diverticulitis Hemorrhoids Malnutrition ‣ ‣ ‣ ‣ ‣ Depression Labs • • • Fecal occult blood test results are negative. Stool examination for ova and parasites is negative. Stool culture is negative for leukocytes and pathogenic bacteria. Complete blood count (CBC) with differential, serologic tests, serum albumin level test, and erythrocyte sedimentation rate test results are normal. Lactose tolerance blood test and celiac testing may be performed. • • CAUSES • GI motility • visceral hyperalgesia • psychopathology INTERVENTIONS ‣ Weight ‣ Diet ‣ Bowel elimination pattern Diet ‣ Initially, elimination diet ‣ Avoidance of sorbitol, non-absorbable carbohydrates, and foods that contain lactose or that are high gas-forming ‣ Gradual increase in fiber to prevent increased intestinal gas production ‣ Increased fluid intake (if constipation is predominant) ‣ Avoidance of large meals, fatty foods, and caffeine, which can exacerbate symptoms ‣ Small, frequent meals ‣ High-fiber diet ‣ Avoidance of alcohol, artificial sweeteners, and foods to which the patient is intolerant ‣ Decreased dairy EDUCATION Because this patient is not usually hospitalized interventions focus on teaching. Monitor: ‣ Bloating ‣ There is no cause or test for IBS ‣ Drink 8-10 glasses of water a day ‣ Implement relaxation ‣ Need for colorectal cancer screenings Medications Fiber supplements Lactase Probiotics Peppermint oil Tricyclic Antidepressants ‣ Anticholinergics ‣ ‣ ‣ ‣ ‣ and frequency of stool 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 116 lOMoARcPSD|11334620 117 MEDICAL SURGICAL NURSING: GASTROINTESTINAL 1.3.9 NURSE ANGIE 2018 Peptic Ulcer An excavated lesion of the mucosal wall of the esophagus, stomach, or duodenum Risks Pathophysiology ‣ Type A blood (for gastric ulcer) ‣ Type O blood (for duodenal ulcer) ‣ Gastric or duodenal mucosal defects ‣ Exposure to irritants ‣ Cigarette smoking or use of smokeless tobacco ‣ High stress ‣ Family history ‣ Psychogenic factors ‣ Use of certain medications ‣ Normal aging Results when gastric mucosal defenses become impaired and longer protect the epithelium from the effects of acid and pepsin. H. pylori bacteria releases a toxin that promotes mucosal inflammation and ulceration. Assessment ‣ Weight changes: loss with gastric ulcer, gain wire duodenal ulcer ‣ GI bleeding ‣ Coffee ground emesis ‣ Melena ‣ Perforation ‣ Tender, rigid board like abdomen ‣ Hypovolemic shock ‣ Epigastric pain that is worse with eating Complications ‣ GI hemorrhage ‣ Abdominal or intestinal infarction ‣ Ulcer penetration into attached structures ‣ Increased risk of gastric adenocarcinoma (in patients with H. pylori) ‣ Obstruction from scarring or acute inflammation ‣ Bowel perforation ‣ Peritonitis ‣ Anemia Labs & Diagnostics ‣ Low hemoglobin from bleeding ‣ Occult blood in stool ‣ Positive test for H. Pylori ‣ Endoscopy and Colonoscopy will show ulceration CAUSES H. pylori Nonsteroidal antiinflammatory drug (NSAID) or glucocorticoid use ‣ Pathologic hypersecretory states (rare) ‣ Genetics ‣ ‣ INTERVENTIONS EDUCATION ‣ Monitor vitals ‣ Diet modifications ‣ Monitor I & O ‣ Avoid NSAIDS ‣ Monitor bowel sounds ‣ Smoking cessation Treatment ‣ Histamine h2 blockers: Famotidine ‣ Proton pump inhibitors: omeprazole ‣ Mucosal barrier fortifers: sucralfate Prostaglandin analogue: misoprostol ‣ Diet : avoid dairy, spices, caffeine, and , alcohol ‣ NPO: if GI bleed is present ‣ Monitor stools for blood 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 117 lOMoARcPSD|11334620 118 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.2 OCTOBER 10, 2018 Jaundice Yellow or green tinged sclera and skin caused by elevated bilirubin levels. Pathophysiology Assessment: If the flow of bile is impeded or if there is excess destruction of red blood cells as a consequence of liver disease or bile ducts obstruction causes an increase in serum bilirubin. When serum bilirubin levels become abnormally elevated all of the tissues in the body will turn yellow or green. Complications ‣ ‣ ‣ ‣ Kernicterus Cerebral palsy Epilepsy Mental impairment ‣ Hemolytic: Usually asymptomatic. ‣ Hepatocellular: Mild or severe illness, lack of appetite, nausea, malaise, fatigue, weakness and weight loss, headache, chills, and fever if the cause is infectious. ‣ Obstructive: Light gray or clay colored stool, intense itching, dyspepsia, and intolerance to fatty foods. Treatments: Laboratory Findings: EDUCATION ‣ Educate the client on treatment regimen ‣ GGT elevation ‣ Increased serum bilirubin ‣ AST and ALT elevation ‣ Signs and symptoms of jaundice ‣ Encourage proper diet ‣ Encourage your client to keep u with appointments and lab CAUSES ‣ Increased production ‣ Decreased hepatic uptake ‣ Decreased conjugation ‣ Dysfunction of hepatocytes work INTERVENTIONS ‣ Causes of jaundice ‣ Interventions are associated with the cause of the jaundice. ‣ Long term jaundice can cause pigment stones, brain stem injury, and CNS dysfunction. ‣ Slowing of bile egress from the liver ‣ Encourage smoking and alcohol cessation if appropriate. ‣ Obstruction of extra-hepatic bile flow 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Jaundice itself requires no treatment in adults, if itching becomes an issue, the HCP may prescribe cholestyramine 2 to 8 g po bid. However, cholestyramine is ineffective in patients with complete biliary obstruction. Medical Treatments ‣ Jaundice induced by anemia may be treated by taking iron supplements or eating more iron rich foods. ‣ Jaundice induced by hepatitis requires steroid or antiviral medications. ‣ Jaundice caused by an obstruction can be surgically resolved by removing the obstruction. 118 lOMoARcPSD|11334620 119 MEDICAL SURGICAL NURSING: HEPATIC 1.4.3 NURSE ANGIE 2018 Ascites Albumin rich fluid build up in the abdomen of 25 mL or more, caused by portal hypertension resulting in increased capillary pressure and obstruction of venous blood flow. Pathophysiology Assessment: Portal hypertension leads to vasodilation, which causes a decrease in effective arterial blood volume. As the disease progresses, neurohumoral excitation increases, more renal sodium is retained, and plasma volume expands. This causes overflow of albumin rich fluid into the peritoneal cavity. ‣ Swollen, rounded abdomen, bulging flanks in he supine position ‣ Striae ‣ Weight gain ‣ Shortness of breath ‣ Distended veins ‣ Umbilical hernia ‣ Electrolyte and fluid imbalances hypovolemia Treatments: Laboratory Findings: ‣ Protein concentration under <250 cells/ uL ‣ High serum-to-ascites albumin concentration gradient ≥ 1.1 g/dL CAUSES ‣ Vasodilation of splanchnic circulation. Changes in the ability to metabolize aldosterone which increases fluid retention. ‣ Decreased albumin synthesis. Decreased serum osmotic pressure. ‣ Movement of albumin into the peritoneal cavity, causing a decrease in circulating protein. Pericarditis. Endocrine disorder INTERVENTIONS ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ EDUCATION ‣ Daily weights. Strict intake and output monitoring. Daily abdominal girth measurements. Monitor respiratory status. Monitor serum ammonia, creatinine, and electrolyte levels. Monitor client's response to therapy. Monitor for signs of encephalopathy. When potassium is decreased ammonia is increased causing encephalopathy. ‣ ‣ ‣ ‣ ‣ Educate the client on the plan of treatment. Avoid alcohol intake. Importance of adhering to a low sodium diet. Take their medications as ordered. State the importance of daily weights, more than 2kg a day is too much loss. Discuss the importance of avoiding NSAIDS, cough mixtures containing alcohol, antibiotics or antacids that contain salts. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Dietary restrictions: 2g sodium per day restriction, no salt substitutes because they contain potassium and ammonia. ‣ Bed rest: Semi fowlers. ‣ Diuretics: Spironolactone to prevent potassium loss. Lasix may be used cautiously to avoid sodium depletion. ‣ Paracentesis: removal of excess abdominal fluid under sterile conditions. Can take up to 4 L of fluid a day.have the client void prior to procedure, obtain baseline vitals, labs, weight and abdominal girth. Monitor for shock, bleeding, hematuria. Send Fluid to the lab. Apply sterile dressing and monitor vitals. ‣ Transjugular Intrahepatic Portosystemic Shunt: Cannula is threaded into the portal vein to reduce portal HTN. ‣ Administer salt poor albumin. 119 lOMoARcPSD|11334620 120 MEDICAL SURGICAL NURSING: CARDIOVASCULAR 1.2.2 OCTOBER 10, 2018 Cirrhosis Chronic, slowly progressive, fibrotic liver disease. Pathophysiology Assessment A chronic and progressive disease characterized by degeneration of hepatocytes. This destruction then causes the liver to become fibrosed causing destruction of liver lobules, leading to other complications. Complications Ascites Muscle wasting Coagulopathy Portal hypertension Bleeding esophageal varices ‣ Hepatic encephalopathy Hepatorenal syndrome ‣ Hepatocellular carcinoma ‣ Hepatic failure Death ‣ ‣ ‣ ‣ ‣ Risk Factors ‣ ‣ ‣ ‣ ‣ Laboratory Findings: ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Albumin: Decreases Serum AST, ALT, GGT: Increase Serum cholinesterase: Decrease Bilirubin: Increases Prothrombin time: Prolonged Ultrasound: Measures scar tissue. CT, MRI: Give info about liver size and blood flow. Liver biopsy: Confirms diagnosis ABG: May reveal a ventilation perfusion imbalance and hypoxia. Alcoholism Toxins Biliary obstruction Hepatitis Metabolic disorders Heart failure CAUSES ‣Excess alcohol consumption INTERVENTIONS ‣Cellular necrosis ‣ Identify precipitating factors ‣Nutritional deficits ‣ Promote alcohol cessation. Improve nutritional status, high calories, low sodium. ‣Portal issues ‣ Frequent position changes. Prevent falls and trauma. Daily weights. ‣Hepatotoxic medications EDUCATION ‣ Low in sodium, and ‣ Low saturated fat, trans fat and cholesterol. ‣ The client should read labels to identify heart-healthy foods. ‣Hepatitis ‣Biliary obstruction. ‣ Vitamin supplements ‣ Monitor for infection, bleeding, and fluid volume. ‣Bile stasis ‣Right sided heart failure 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Organs: Liver ‣ ‣ ‣ ‣ enlargement, portal obstruction, firm enlarged liver, splenomegaly. GI/GU: Ascites, GI varices, flatulent dyspepsia, abdominal pain, ascites, weight loss, gonadal atrophy. steatorrhea. Cardio: Portal obstruction, anemia, clubbing, hypotension, bleeding due to decrease in Vitamin K. CNS: Mental deterioration. Misc: Vitamin ABD deficits, intermittent fever, red palms, jaundice, muscle wasting, rash, itchiness, sparse body hair, white nails. Medical Treatments: ‣ Antacids & H2 antagonists: To relieve gastric distress. ‣ Vitamins: KADE to promote healing of the liver. ‣ Potassium sparing diuretics: To decrease ascites. ‣ Colchicine, angiotensin system inhibitors, statins, diuretics including spironolactone (Aldactone), immunosuppressants, and glitazones such as pioglitazone (Actos) or rosiglitazone (Avandia): Possess antifibrotic properties for the treatment of cirrhosis. ‣Milk thistle: Also is known to be an anti-inflammatory to treat jaundice and other symptoms of hepatitis. ‣Ursodeoxycholic Acid: Used to treat primary biliary cirrhosis. 120 lOMoARcPSD|11334620 121 MEDICAL SURGICAL NURSING: HEPATIC 1.4.4 NURSE ANGIE 2018 Esophageal varices Varicosities in the esophagus caused by increased pressure from the portal vein. Pathophysiology Assessment:History Esophageal varices develop when normal blood flow to the liver is blocked in the state of scar tissue, cirrhosis, or a clot in the liver. Obstruction of portal venous flow results in increased portal vein pressure. High pressure in the portal vein causes blood to be diverted into the smaller fragile veins of the esophagus as well as the stomach and rectum. Increased pressure in the smaller veins causes them to distend. Distended veins may rupture, which can cause life-threatening hemorrhage. Complications ‣ Variceal hemorrhage (may be fatal) ‣ Hypovolemic shock ‣ Encephalopathy ‣ Infection, sepsis ‣ Esophageal stricture after surgery or endoscopic therapy ‣ Aspiration pneumonia ‣ Acute kidney injury ‣ Acute or chronic liver failure ‣ Hepatitis B surface antibodies test and hepatitis C antibodies test results may determine the cause of liver disease. Laboratory Findings: ‣ Complete blood count (CBC) with differential may reveal anemia, leukopenia, and thrombocytopenia. ‣ Prothrombin time and partial thromboplastin time may be prolonged because of liver failure. ‣ Liver function test shows mild elevation in aspartate aminotransferase and alanine aminotransferase, which may occur because of cirrhosis. ‣ Blood urea nitrogen level test and creatinine level (serum) may be elevated. CAUSES ‣ Cirrhosis ‣ Heart failure ‣ Blood clots such as portal vein thromboses ‣ Sarcoidosis ‣ Schistosomiasis ‣ Wilson disease ‣ Hemochromatosis ‣ Weakness, tiredness, and general malaise ‣ Anorexia ‣ Nausea and vomiting ‣ Hematemesis ‣ Weight loss ‣ Abdominal pain ‣ Jaundice or dark-colored urine ‣ Ascites ‣ Pruritus ‣ Spontaneous bleeding and easy bruising ‣ Muscle cramps ‣ Melena Physical Findings ‣ ‣ ‣ ‣ ‣ ‣ ‣ ‣ Pallor Hypotension Tachycardia Dyspnea Jaundice Ascites Palmar erythema Spider nevi—clusters of tiny vessels on the skin resembling a spider Treatments: ‣ Treat for shock ‣ Administer electrolytes ‣ Vasopressin ‣ Somatostatin and octreotide ‣ Nitroglycerin with INTERVENTIONS ‣ Elevate the head of the bed ‣ Monitor for orthostatic hypotension. ‣ Monitor vitals and lung sounds. ‣ Administer O2 and IV liquids. ‣ Monitor hemoglobin, hematocrit EDUCATION ‣ Educate patent to avoid strenuous activities. ‣ vasopressin ‣ Beta-blockers ‣ Sengstaken-blackmore tube ‣ Sclerotherapy ‣ Ligation and coagulation factors. ‣ Gastric suctions. ‣ Start vitamin K therapy to promote clotting. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 121 lOMoARcPSD|11334620 122 MEDICAL SURGICAL NURSING: HEPATIC 1.4.5 NURSE ANGIE 2018 Hepatic encephalopathy A life threatening complication of liver disease that occurs in severe liver failure. Pathophysiology Assessment Hepatic insufficiency may result in encephalopathy due to a diseased liver that is unable to detoxify toxic by products of metabolism. Porto systemic shunting where collateral vessels are developed as a result of portal ‣ ‣ ‣ hypertension allows toxic substances extracted from the liver into the systemic circulation. Ammonia is considered the main factor in the development of hepatic encephalopathy. Ammonia enters the brain and excites benzodiazepine receptors causing CNS depression; which produce the sleep and behavior patterns noted in hepatic encephalopathy. Ammonia from digestion of dietary and blood proteins in the GI tract. ‣ ‣ ‣ Increases in ammonia from these sources can cause GI bleeding (including varices). ‣ Complications ‣ Aspiration pneumonia ‣ Hepatorenal syndrome ‣ Irreversible coma Cardiovascular collapse ‣ Cerebral edema ‣ Brain herniation Death Laboratory Findings: ‣ Serum ammonia level test results are elevated and, together with characteristic clinical features, strongly suggest hepatic encephalopathy. ‣ Serum bilirubin level test results are elevated. ‣ Prothrombin time is prolonged. ‣ Serum electrolyte levels may reveal hypokalemia, altered calcium levels, or hypomagnesemia. ‣ Chronic liver damage ‣ Suspected accumulation of neurotoxic substances in the brain due to inability of liver to break down toxins ‣ Blockage of blood supply to the liver ‣ Hepatitis B infection (uncommon) Treatments: ‣ Aimed at eliminating precipitating causes and minimizing potential complications. ‣ Lactulose reduces serum ammonia by trapping and expelling it in feces. 2-3 soft stools a day is indicative the lactulose is having a therapeutic effect. ‣ IV Glucose minimize protein breakdown. ‣ Vitamins to correct deficits and electrolyte imbalances. Incidence INTERVENTIONS CAUSES ‣ Mental status changes Confusion Sleepiness during the day May lapse into a coma or have seizures EEG changes Asterixis “liver flap” usually seen in stage 2 encephalopathy. Hyperactive DTR’s in early stages, flaccidity in late stages. Fetor hepaticus EDUCATION ‣ ‣ ‣ ‣ ‣ Assess neuro status frequently Keep a daily log of mental status I&O, daily weights, and vitals q4. Evaluate potential site of infection Monitor serum ammonia, electrolytes, and fluids. ‣ Discontinue sedatives, analgesics, and tranquilizers. Reduce ammonia levels by GI suctions, enema, or antibiotics. ‣ ‣ Educate on diet restrictions Educate in medication regimen 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ Hepatic encephalopathy can occur at any age. ‣ It occurs overtly in 30% to 45% of patients with cirrhosis; it will develop to some degree in up to 80% of patients with cirrhosis. ‣ It is present in nearly half of patients requiring liver transplantation. ‣ It occurs in 24% to 50% of patients with transjugular intrahepatic portosystemic shunts. 122 lOMoARcPSD|11334620 123 MEDICAL SURGICAL NURSING: HEPATIC 1.4.5 NURSE ANGIE 2018 Hepatitis An inflamation of the liver aused by drugs, alcohol use or a virus. Pathophysiology Assessment There are three hepatitis viruses and they cause similar liver damage. The inflammation process is initiated throughout the entire liver, and hepatocytes are destroyed by cytotoxic cytokines and natural killer cells, both parts of the inflammation process. Cellular necrosis takes place. If inflammation affects the periportal areas, cholestasis, or the interruption of the flow of bile takes place. The liver is usually able to repair itself and regain complete function if no other complications occur. CAUSES/TYPES ‣ A: Infectious hepatitis transmission is fecal oral route. ‣ Poor sanitation ‣ Person to person Laboratory Findings: ‣ Water ‣ Food ‣ ALT: Elevated into the thousands. Normal 10- 40 U/L. ‣ AST: Elevated into the thousands. Normal 10-30 U/L. ‣ Ammonia : Elevated. May lead to encephalopathy. Normal 10 mcg/dl. ‣ Total Bilirubin levels: Elevated in serum urine. Normal is lower than 1.5mg/dl. Preicteric : No jaundice yet, the patient will have flu like symptoms. ‣ Malaise ‣ Fatigue ‣ Nausea, vomiting, diarrhea ‣ Headache ‣ Muscle aches ‣ Polyartritis ‣ Elevated serum bilirubin and enzyme levels Icteric: Jaundice is present. ‣ Puritis ‣ Dark, tea colored urine ‣ Clay colored stools ‣ Decrease in pre-icteric symptoms ‣ Posticteric: Increased energy. ‣ Pain goes away ‣ Lessened GI symptoms ‣ Serum bilirubin and enzyme levels return to normal ‣ Possible contact with anal or oral sex ‣ B/C: Hepatitis B virus transmitted via blood. ‣ Sex ‣ Mother baby Medical Treatment ‣ Hep B: Alpha interferon, lamivudine (epivir), adenovir, bed rest, nutritional support, Hep B ‣ IV drug use INTERVENTIONS ‣ Management usually occurs at home. ‣ Help the patient cope with fatigue. ‣ Have the patient contact the HCP if symptoms worsen.. EDUCATION ‣ Eat small frequent meals, high in ‣ carbs, low in fats and avoid animal fats. ‣ Do not donate blood. ‣ Avoid close personal contact until results are negative. ‣ Alcohol cessation. ‣ Rest , increase activity gradually. ‣ Blood work. immune globulin, Hep B ‣ C: hepatitis C virus vaccine. Do not give the ‣ Transmitted via blood Hep B IG and vaccine in ‣ Blood transfusion ‣ Sex ‣ Drug paraphernalia ‣ D: Only those whom have contacted the same injection or the same site. ‣ Hep C: Interferon, Ribavirin, restrict animal protein. ‣ Hep B are at risk. ‣ E: Hepatitis E. Transmitted via fecal oral route. 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) 123 lOMoARcPSD|11334620 124 MEDICAL SURGICAL NURSING: HEPATIC 1.4.2 NURSE ANGIE 2018 Portal Hypertension When the portal venous system is obstructed or stenosed it causes a rise in portal pressure causing portal hypertension. Assessment: Pathophysiology Obstruction of portal blood flow, such as cirrhosis or portal vein thrombosis. In liver cirrhosis, increased intrahepatic vascular resistance to the portal flow elevates portal pressure and leads to portal hypertension. Complications ‣ ‣ ‣ ‣ GI Bleeding Varices rupture Ascites Hepatic Encephalopathy ‣ Varices ‣ Ascites ‣ Thrombocytopenia: early indicator of liver dysfunction ‣ Splenomegaly Treatments: ‣ Endoscopic therapy ‣ Esophageal balloon ‣ Nonselective beta-blockers Laboratory Findings: ‣ CBC: Low platelets ‣ Hemoccult: yield GI bleeding ‣ H&H: Low INTERVENTIONS ‣ Elevate the head of the bed to minimize SOB. ‣ Restrict sodium intake. ‣ Administer diuretics. ‣ Monitor intake and output. ‣ Weigh the client daily. ‣ Monitor LOC. ‣ Administer blood products if indicated. ‣ Monitor prothrombin time and coagulation studies. ‣ Administer Vitamin K if indicated. ‣ Administer lactulose if indicated. ‣ Avoid opioids, sedatives, and barbituates. EDUCATION CAUSES ‣ Blood clots in the portal vein. ‣ Blockage of the veins that carry blood from the liver to the heart. ‣ Focal nodular hyperplasia usually seen in HIV. ‣ Parasitic infection, schistosomiasis. ‣ Educate the client on the importance of alcohol cessation. ‣ Educate on medication regimen ‣ Educate on dietary restrictions 1 Downloaded by Kortney Mccullough (kmccullough1.km@gmail.com) ‣ ‣ ‣ ‣ Medical Treatment Surgery Radiology Dietary changes Endoscopic therapy 124