Respiratory Physiology Worksheet: Lung Volumes & Hemoglobin
advertisement

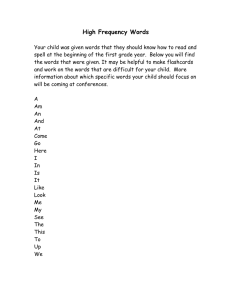
1 What are the effects of surfactant secretion in the lungs? Decreased alveolar surface tension, increased compliance, and decreased work of inspiration 2 Name five important molecules produced by the lungs. Surfactant, prostaglandins, histamine, angiotensin-converting enzyme, and kallikrein 3 In addition to inactivating bradykinin, what other reaction does angiotensin-converting enzyme catalyze? The conversion of angiotensin I to angiotensin II 4 Angiotensin-converting enzyme inhibitors increase bradykinin, which leads to which two common adverse effects? Cough and angioedema 5 A deficiency of surfactant leads to what neonatal condition? Respiratory distress syndrome 6 Give the equation for calculating collapsing pressure. Collapsing pressure = 2 × tension / radius 7 What is the effect of histamine on the airways in the lung? Increases bronchoconstriction 8 In the lung, _____ (angiotensin-converting enzyme/kallikrein) inactivates bradykinin, _____ (angiotensin-converting enzyme/kallikrein) activates bradykinin. Angiotensive converting enzyme; kallikrein 9 What is the term for the volume of air in the lungs after maximal expiration? Residual volume 10 What is the term for the volume of air that can still be breathed out after normal expiration? Expiratory reserve volume 11 What is the term for the volume of air that moves into the lungs with each quiet inspiration? Tidal volume 12 How much is the typical tidal volume? 500 mL 13 What is the term for the volume of air in excess of tidal volume that moves into the lung on maximum inspiration? Inspiratory reserve volume 14 What is the term for the maximum volume of air that can be inhaled and exhaled? Vital capacity 15 Vital capacity equals the sum of what three lung volumes? Tidal volume, inspiratory reserve volume, and expiratory reserve volume 16 The residual volume plus the expiratory reserve volume equals what? The functional reserve capacity 17 Describe the functional reserve capacity. The volume left in the lungs after normal expiration 18 The inspiratory reserve volume plus the tidal volume equals what? Inspiratory capacity 19 The inspiratory reserve volume plus the tidal volume plus the expiratory reserve volume plus the residual volume equals what? Total lung capacity 20 What is the term for the lung volume that includes all capacity except the residual volume? Vital capacity 21 Which lung volume cannot be measured on spirometry: inspiratory reserve volume, tidal volume, expiratory reserve volume, or residual volume? Residual volume 22 What is the formula for calculating dead space volume given an arterial blood gas and a measurement of exhaled carbon dioxide? Dead space volume = tidal volume × [(partial arterial pressure of carbon dioxide - partial expiratory pressure of carbon dioxide) / partial arterial pressure of carbon dioxide] 23 Physiological dead space includes the anatomical dead space of the _____ (conducting/respiratory) airways plus the functional dead space in _____ (alveoli/bronchioles). Conducting; alveoli 24 Which section of the healthy lung contributes more to functional dead space: the apex or the base? The apex 25 Describe the natural tendency of movement of the lung and chest wall. The lungs tend to collapse inward and chest wall springs outward 26 At the point of functional residual capacity (i.e., at the end of a normal expiration), what is the value of the air pressure within the lungs? At functional residual capacity, the pressure within the lungs is equal to atmospheric pressure 27 What balances the inward elastic pull of the lung at the point of functional residual capacity (i.e. at the end of a normal expiration)? The outward pull of the chest wall 28 How many polypeptide subunits make up hemoglobin? Four 29 Adult hemoglobin is formed from two _____ subunits and two _____ subunits. α; β 30 What are the two conformational forms of hemoglobin? Relaxed and taut 31 Which form of hemoglobin has a low affinity for oxygen, relaxed or taut? Taut 32 Which form of hemoglobin has a high affinity for oxygen, relaxed or taut? Relaxed 33 Fetal hemoglobin is composed of two ____ subunits and two ____ subunits. α; γ 34 Does hemoglobin have positive or negative cooperativity with respect to oxygen binding and affinity? Positive; the more oxygen molecules bind, the more affinity hemoglobin has for additional oxygen molecules 35 Does fetal hemoglobin have a higher or lower affinity for oxygen compared with adult hemoglobin? Higher; as a result, fetal blood can draw oxygen across the placenta 36 Does fetal hemoglobin have a higher or lower affinity for 2,3-biphosphoglycerate compared with adult hemoglobin and what is the result? Lower; increased affinity for oxygen 37 An increase in which five factors will favor the taut form of hemoglobin over the relaxed form and decrease affinity for oxygen? Chloride, hydron, carbon dioxide, 2,3-bisphosphoglycerate, and temperature 38 Which form of hemoglobin will lead to decreased oxygen unloading? The relaxed form (remember: "When you're Relaxed, you do your job better [carry oxygen]") 39 With respect to cooperativity and affinity for oxygen, what are the differences between hemoglobin and myoglobin? Myoglobin has high affinity for oxygen but does not display cooperativity of oxygen binding because it has only a single subunit 40 Does hemoglobin contain iron in the oxidized state or in the reduced state; Fe2+ or Fe3+; ferric iron or ferrous iron? The reduced state; Fe2+; ferrous iron 41 Does methemoglobin contain iron in the oxidized state or the reduced state; Fe2+ or Fe3+; ferric iron or ferrous iron? The oxidized state; Fe3+; ferric iron 42 Hemoglobin contains _____ (ferric/ferrous) iron, whereas methemoglobin contains _____ (ferric/ferrous) iron. Ferrous; ferric 43 What are the mechanisms of action of nitrites and thiosulfate in the treatment of cyanide poisoning? Nitrites oxidize the iron in hemoglobin to form methemoglobin; methemoglobin then binds to cyanide ions, which in turn allows cytochrome oxidase to function; after administering nitrites, thiosulfate is used to bind to the cyanide-methemoglobin complexes, to form thiocyanate, which is renally excreted 44 When another molecule, such as CO, binds to hemoglobin in place of oxygen, what are the systemic effects? This leads to tissue hypoxia from decreased oxygen saturation and decreased oxygen content in the blood 45 Which has a higher affinity for oxygen, hemoglobin or methemoglobin? Hemoglobin 46 What is the treatment for toxic levels of methemoglobin? Methylene blue (remember: METHemoglobinemia can be treated with METHylene blue) 47 Which has a higher affinity for cyanide, hemoglobin or methemoglobin? Methemoglobin 48 What is the name of a form of hemoglobin in which carbon monoxide is bound instead of oxygen? Carboxyhemoglobin 49 In treating cyanide poisoning, ______ is the compound used to bind cyanide, forming _____ which is a renally excretable compound. Thiosulfate; thiocyanate 50 What is the treatment for cyanide poisoning? Nitrites, and subsequently thiosulfate 51 Does carbon monoxide or oxygen have a greater affinity for hemoglobin? Carbon monoxide has 200 times the affinity of oxygen 52 What is the shape of the oxygen-hemoglobin dissociation curve? Sigmoidal 53 When the oxygen-hemoglobin dissociation curve shifts to the right, what happens to the affinity of hemoglobin for oxygen? A right shift decreases the affinity of hemoglobin for oxygen 54 When the oxygen-hemoglobin dissociation curve shifts to the right, what happens to the P50? A right shift increases the P50, indicating that higher oxygen pressure is required to saturate hemoglobin 55 A shift of the oxygen-hemoglobin dissociation curve to the right facilitates what process in tissue? The unloading of oxygen to tissue 56 When the oxygen-hemoglobin dissociation curve shifts to the left, what happens to the affinity of hemoglobin for oxygen? A left shift increases the affinity of hemoglobin for oxygen 57 When the oxygen-hemoglobin dissociation curve shifts to the left, what happens to the P50? A left shift decreases the P50; hemoglobin is saturated at lower pressures of oxygen 58 A decrease in the partial pressure of carbon dioxide causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Left 59 A decrease in temperature causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Left 60 A decrease in pH causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Right 61 A decrease in 2,3-diphosphoglycerate causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Left 62 The oxygen-hemoglobin dissociation curve for fetal hemoglobin is shifted in what direction? Left; fetal hemoglobin has higher affinity for oxygen than adult hemoglobin 63 An increase in the partial pressure of carbon dioxide causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Right 64 An increase in temperature causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Right 65 An increase in pH causes a ______ (left/right) shift in the oxygen-hemoglobin dissociation curve. Left 66 High altitude induces what change in the oxygenhemoglobin dissociation curve? A right shift 67 An increase in 2,3-diphosphoglycerate causes a _____ (left/right) shift in the oxygen-hemoglobin dissociation curve. Right 68 In the oxygen-hemoglobin dissociation curve, what values are represented by the x and y axes? The partial pressure of oxygen represents the x axis, while hemoglobin saturation represents the y-axis 69 Hemoglobin can bind four oxygen molecules and has a higher affinity for each subsequent oxygen molecule bound. What is the term for this phenomenon? Positive cooperativity 70 An increase in the amounts of which six factors causes a right shift of the oxygen-hemoglobin dissociation curve? Study These Flashcards CO2, hydrogen ions (therefore acidity), altitude, 2,3-DPG, metabolic needs (eg, exercise), and temperature (remember: CADET face right: CO2, Acid/Altitude, DPG [2,3-DPG], Exercise, Temperature) 71 Normally, pulmonary circulation is a _____ (high/low) resistance, _____ (high/low) compliance system. Study These Flashcards Low; high 72 Within the lungs, a decrease in the partial pressure of oxygen in arterial blood causes what process to occur within the vasculature in the area? Study These Flashcards Hypoxic vasoconstriction; in the rest of the body hypoxia causes vasodilation 73 Within the lungs, hypoxic vasoconstriction serves what physiologic function? Study These Flashcards It shifts blood away from the poorly ventilated regions of the lung to the well-ventilated regions of the lung 74 Under normal, healthy conditions, is oxygen a perfusionlimited gas or a diffusion-limited gas? Study These Flashcards Perfusion-limited gas 75 Is carbon dioxide a perfusion-limited gas or a diffusionlimited gas? Study These Flashcards Perfusion-limited gas 76 Is nitrous oxide a perfusion-limited gas or a diffusionlimited gas? Study These Flashcards Perfusion-limited gas 77 Is carbon monoxide a perfusion-limited gas or a diffusionlimited gas? Study These Flashcards Diffusion-limited gas 78 Under conditions of strenuous exercise, is oxygen a perfusion-limited gas or a diffusion-limited gas? Study These Flashcards Diffusion-limited gas 79 Under perfusion-limited conditions, where along the length of the pulmonary capillary do the partial pressures of a gas equilibrate? Study These Flashcards Early; gas exchange is not limited by its ability to cross the membrane, only by the supply of blood 80 Under perfusion-limited conditions, how can gas exchange be increased? Study These Flashcards By increasing blood flow 81 Under what three conditions is oxygen a diffusion-limited gas? Study These Flashcards Exercise, emphysema, and fibrosis 82 Under diffusion-limited conditions, where along the length of the pulmonary capillary does the gas equilibrate? Study These Flashcards It does not equilibrate; the characteristics of the gas cause it to diffuse slowly across the alveolar membrane 83 What are the cardiac complications of pulmonary hypertension? Study These Flashcards Cor pulmonale and right ventricular failure 84 What are three signs of right ventricular heart failure due to cor pulmonale? Study These Flashcards Jugular venous distention, edema, and hepatomegaly 85 What is the equation for diffusion of a gas across a membrane? Study These Flashcards Vgas = A/T × Dk(P1 - P2), where A = area, T = thickness, and Dk(P1 - P2) = difference in partial pressures 86 In the equation for gas diffusion, which variable is affected by emphysema and how? Study These Flashcards Area of membranes available for gas transfer is decreased in emphysema, causing a decrease in diffusion 87 In the equation for gas diffusion, which variable is affected by pulmonary fibrosis and how? Study These Flashcards Thickness of the membrane is increased in pulmonary fibrosis, causing a decrease in diffusion 88 What is normal pulmonary arterial pressure? Study These Flashcards 10-14 mm Hg 89 What pulmonary artery pressures define pulmonary hypertension? Study These Flashcards 25 mm Hg or greater during rest and >35 mm Hg during exercise 90 Primary pulmonary hypertension is caused by what? Study These Flashcards An inactivating mutation in the BMPR2 gene, which normally functions to inhibit vascular smooth muscle proliferation 91 What is the prognosis for a patient diagnosed with primary pulmonary hypertension? Study These Flashcards Very poor; the disease is progressive and fatal 92 What are some of the potential causes of secondary pulmonary hypertension? Study These Flashcards Chronic obstructive pulmonary disease, left-to-right shunt, mitral stenosis, recurrent thromboemboli, autoimmune disease (ie, systemic sclerosis), sleep apnea, or living at high altitudes 93 What are three pathological changes in the vasculature are caused by pulmonary hypertension? Study These Flashcards Atherosclerosis, medial hypertrophy, and intimal fibrosis of the pulmonary arteries 94 How does chronic obstructive pulmonary disease cause pulmonary hypertension? Study These Flashcards By the destruction of lung parenchyma and subsequent vasoconstriction due to hypoxia 95 How does mitral stenosis cause pulmonary hypertension? Study These Flashcards By increasing resistance to blood flow in the left heart; thus causing a buildup of pressure starting in the left atrium and backing up to the pulmonary vasculature 96 How do recurrent thromboemboli cause pulmonary hypertension? Study These Flashcards By decreasing the total cross-sectional area of the pulmonary vascular bed 97 How can autoimmune disease cause pulmonary hypertension? Study These Flashcards Processes such as systemic sclerosis lead to inflammation, then to intimal fibrosis, which in turn leads to medial hypertrophy in the pulmonary vasculature 98 How does left-to-right shunt cause pulmonary hypertension? Study These Flashcards By causing increased shear stress (due to increased blood volume in the pulmonary vasculature) and thus endothelial injury 99 How do sleep apnea or living at high altitudes cause pulmonary hypertension? Study These Flashcards Sleep apnea and living at high altitudes cause hypoxia, which in turn causes pulmonary vasoconstriction 100 What are the sequelae of pulmonary hypertension if left untreated? Study These Flashcards Severe respiratory distress, causing right ventricular hypertrophy and cyanosis . This results in decompensated cor pulmonale which leads to death 101 How is pulmonary vascular resistance calculated? Study These Flashcards Pulmonary vascular resistance = (pressure in the pulmonary artery minus pressure in the left atrium) divided by the cardiac output 102 How is left atrial pressure measured? Study These Flashcards It is approximated by wedge pressure 103 Pulmonary vascular resistance is _____ (directly/inversely) related to vessel length and _____ (directly/inversely) related to vessel radius. Study These Flashcards Directly; inversely 104 What is the equation for resistance, given vessel length, diameter, and blood viscosity? Study These Flashcards R = (8ηl) / (πr4), where η = viscosity of blood, l = vessel length, and r = vessel radius 105 How is the oxygen content of the blood calculated? Study These Flashcards Oxygen content of the blood = (oxygen-binding capacity × percent saturation) + dissolved oxygen 106 How much oxygen can 1 g of hemoglobin bind? Study These Flashcards 1.34 mL 107 What is the average amount of hemoglobin in normal blood? Study These Flashcards Approximately 15 g/dL 108 What is the normal oxygen-binding capacity of the blood? Study These Flashcards Approximately 20.1 mL oxygen/dL of blood 109 When the hemoglobin level rises, the oxygen content of the blood _____ (rises/falls). Study These Flashcards Rises, because oxygen-binding capacity depends on the total amount of hemoglobin 110 When the hemoglobin level falls, the percent oxygen saturation of the blood ______ (rises/falls/remains stable). Study These Flashcards Remains stable; the blood can still be 100% saturated but there will be less oxygen-binding capacity and therefore lower total oxygen content 111 A decrease in hemoglobin will have what effect on partial oxygen pressure: decrease, increase, or no change? Study These Flashcards No change 112 Visible cyanosis typically results when deoxygenated hemoglobin is at what level? Study These Flashcards > 5 g/dL 113 Why does arterial partial pressure of oxygen decrease with chronic lung disease? Study These Flashcards Physiologic shunt decreases the oxygen extraction ratio 114 What is the formula for oxygen delivery to tissues? Study These Flashcards Oxygen delivery to tissues = cardiac output × oxygen content of blood 115 Will a patient with anemia become cyanotic at a higher or lower oxygen saturation than a normal patient? Study These Flashcards An anemic patient will have a lower oxygen saturation by the time she appears cyanotic; the blue coloration of cyanosis is proportional to the concentration of deoxyhemoglobin, which is lower in anemic patients (as are the concentrations of all types of hemoglobin) 116 What is the alveolar gas equation? Study These Flashcards Alveolar partial pressure of oxygen (in mm Hg) = the partial pressure of oxygen in inspired air minus (alveolar partial carbon dioxide pressure divided by the respiratory quotient); or, PAO2 = PIO2 - (PACO2/R) 117 How can the alveolar gas equation be simplified and approximated (assuming that the patient is breathing ambient air)? Study These Flashcards Alveolar partial pressure of oxygen = 150 - (arterial partial pressure of carbon dioxide / 0.8) 118 By using the alveolar gas equation, what important measure of pulmonary function can be determined? Study These Flashcards The alveolar-arterial gradient (the A-a gradient) 119 What is the normal alveolar-arterial gradient? Study These Flashcards 10-15 mmHg 120 What three pathological processes can lead to increased Aa gradient? Study These Flashcards Shunting, ventilation/perfusion mismatch, and fibrosis of the lungs 121 Name five processes that can lead to hypoxemia (ie, decreased arterial oxygen). Study These Flashcards High altitude, hypoventilation, ventilation/perfusion mismatch, diffusion limitation, and right-to-left shunt 122 Name five processes that can lead to hypoxia (ie, decreased oxygen delivery to tissue). Study These Flashcards Decreased cardiac output, hypoxemia, anemia, cyanide poisoning, and carbon monoxide poisoning 123 Name two processes that can lead to ischemia (i.e. loss of blood flow). Study These Flashcards Impeded arterial flow, and reduced venous drainage 124 What is the difference between hypoxemia and hypoxia? Study These Flashcards Hypoxemia refers to decreased arterial partial pressure of oxygen and can lead to hypoxia, which is defined as decreased oxygen delivery to tissue 125 Which 2 processes lead to hypoxemia with a normal A-a gradient? Study These Flashcards High altitude and hypoventilation 126 Which 3 processes can lead to hypoxemia with an increased A-a gradient? Study These Flashcards Ventilation/perfusion mismatch, diffusion limitation, and right-to-left shunt 127 What is the ideal ratio of ventilation to perfusion to maximize gas exchange? Study These Flashcards 1 to 1 128 Within what part of the lung does ventilation/perfusion equal approximately 3? Study These Flashcards The apex of the lung 129 In the apex of the lung, there is wasted _____ (perfusion/ventilation). Study These Flashcards Ventilation 130 Within what part of the lung does ventilation/perfusion equal approximately 0.6? Study These Flashcards The base of the lung 131 In the base of the lung, there is wasted _____ (perfusion/ventilation). Study These Flashcards Perfusion 132 Is ventilation greater at the base of the lung or the apex of the lung? Study These Flashcards The base of the lung 133 Is perfusion greater at the base of the lung or the apex of the lung? Study These Flashcards The base of the lung 134 The vasodilation of the apical capillaries of the lung that occurs with exercise results in what change to the ventilation/perfusion ratio? Study These Flashcards The ventilation/perfusion ratio approaches 1, maximizing gas exchange to meet the metabolic demands of exercise 135 Microorganisms that thrive in high-oxygen environments, such as tuberculosis, flourish in which part of the lungs? Study These Flashcards The apex 136 A ventilation/perfusion ratio that approaches 0 for a given area of lung indicates that what is occurring in that area? Study These Flashcards Airway obstruction, creating a shunt of blood flow that does not participate in gas exchange 137 What is the name for the process whereby airway obstruction leads to perfusion with no ventilation within an area of the lungs? Study These Flashcards Shunt 138 A ventilation/perfusion ratio that approaches infinity for a given area of lung indicates that what is occurring in that area? Study These Flashcards Blood flow obstruction (ie, pulmonary embolus) 139 When blood flow (but not airflow) into an area of the lungs is obstructed such that the ventilation/perfusion ratio approaches infinity, the area can be considered what type of space? Study These Flashcards Physiologic dead space 140 Which zone of the lung is associated with wasted ventilation? Study These Flashcards Zone 1 141 Which zone of the lung is associated with wasted perfusion? Study These Flashcards Zone 3 142 In hypoxia due to _____ (dead space/shunting), 100% oxygen does not improve the partial pressure of oxygen in the blood; while in hypoxia due to increased _____ (dead space/shunting), there is an improvement in the partial pressure of oxygen in the blood. Study These Flashcards Shunting; dead space 143 In the lung apex (zone 1), arrange the following in order of increasing pressure: artery, vein, alveolus. Study These Flashcards Vein < artery< alveolus 144 In zone 2 of the lung, arrange the following in order of increasing pressure: artery, vein , alveolus. Study These Flashcards Vein < alveolus < artery 145 In the lung base (zone 3), arrange the following in order of increasing pressure: artery, vein, alveolus. Study These Flashcards Alveolus < vein < artery 146 What process causes the ventilation at the apex of the lungs to be considered "wasted?" Study These Flashcards The high alveolar pressure at the apex causes compression of the capillaries, and thus an inability to undertake gas exchange with the blood vessels 147 In which forms is carbon dioxide transported from the tissues to the lungs? Study These Flashcards Three forms: (1) as bicarbonate, (2) bound to hemoglobin as carbaminohemoglobin, and (3) dissolved 148 Ninety percent of the carbon dioxide transported from the tissues to the lungs is in what form? Study These Flashcards Bicarbonate, the creation of which is catalyzed by carbonic anhydrase 149 Other than as bicarbonate, in what two other ways is carbon dioxide transported from the tissues to the lungs? Study These Flashcards Bound to hemoglobin as carbaminohemoglobin and dissolved in blood 150 What percentage of carbon dioxide gets transported from the tissues to the lungs as carbaminohemoglobin; as dissolved carbon dioxide? Study These Flashcards Approximately 5%; approximately 5% 151 After it is inside a red blood cell, each carbon dioxide molecule combines with which molecule in a reaction catalyzed by carbonic anhydrase? Study These Flashcards Water 152 What enzyme catalyzes the conversion of carbon dioxide and water into carbonic acid? Study These Flashcards Carbonic anhydrase 153 Within a red blood cell, the carbonic acid formed from the combination of carbon dioxide and water dissociates into what two compounds? Study These Flashcards Hydrogen and bicarbonate ions 154 What is the fate of the bicarbonate that results from the deprotonation of carbonic acid within an red blood cell? Study These Flashcards It gets exchanged out of the red blood cell for a chloride molecule that enters the red blood cell 155 In the lungs, the oxygenation of hemoglobin promotes what? Study These Flashcards The dissociation of a proton from hemoglobin and therefore a decrease in pH, which favors formation of carbon dioxide from bicarbonate 156 What is the name for the effect in which the oxygenation of hemoglobin within the lungs promotes the dissociation of carbon dioxide from hemoglobin? Study These Flashcards The Haldane effect 157 Regarding carbon dioxide transport, in which direction will the lower pH of peripheral tissues (compared to the lungs) shift the oxygen dissociation curve? Study These Flashcards To the right, favoring dissociation of oxygen from hemoglobin 158 In peripheral tissues, the right shift of the oxygen dissociation curve that results from decreased pH causes an unloading of oxygen. What is this effect called? Study These Flashcards The Bohr effect 159 What happens to ventilation as a response to high altitude in acute situations; chronic situations? Study These Flashcards Ventilation is increased in both cases 160 What happens to erythropoietin levels as a response to high altitude? Study These Flashcards Erythropoietin levels are increased as are hematocrit and hemoglobin 161 What happens to the level of 2,3-diphosphoglycerate in response to high altitude? Study These Flashcards The 2,3-diphosphoglycerate level increases 162 What substance binds to hemoglobin so that hemoglobin releases more oxygen as a physiologic response to high altitude? Study These Flashcards 2,3-Diphosphoglycerate; increased concentrations shift the hemoglobin dissociation curve to the right 163 What cellular changes occur in response to high altitude? Study These Flashcards There is an increase in mitochondria 164 Increased renal excretion of what substance occurs in response to high altitude? Study These Flashcards Bicarbonate 165 The increased renal excretion of bicarbonate that is seen in response to high altitude compensates for what? Study These Flashcards The respiratory alkalosis that occurs as a result of increased ventilation 166 The increased renal excretion of bicarbonate that is seen in response to high altitude can be augmented using what? Study These Flashcards Acetazolamide; the drug is a carbonic anhydrase inhibitor that makes the urine more basic 167 In response to high altitude, chronic hypoxic pulmonary vasoconstriction results in what condition? Study These Flashcards Right ventricular hypertrophy 168 As a result of exercise, what happens to carbon dioxide production in muscles; oxygen consumption? Study These Flashcards Both are increased 169 What happens to the V/Q ratio as a response to exercise? Study These Flashcards It becomes more uniform from apex to base; hence gas exchange is more efficient 170 What happens to pulmonary blood flow as a response to exercise? Study These Flashcards It increases due to increased cardiac output 171 How does the pH of the body change during strenuous exercise? Study These Flashcards pH decreases during strenuous exercise due to lactic acidosis 172 PaO2 and PaCO2 _____ (increase/decrease/remain stable) in response to exercise, whereas venous CO2 content _____ (increases/decreases/remains stable). Study These Flashcards PaO2 and PaCO2 do not change in response to exercise but venous CO2 content increases e.g. MCAT, pharma, bar exam, Sp SearchGo Decks in S1 - Respiratory Class (4): Respiratory Anatomy Respiratory Pathology Respiratory Pharmacology Respiratory Physiology Key Links Pricing Corporate Training Teachers & Schools iOS App