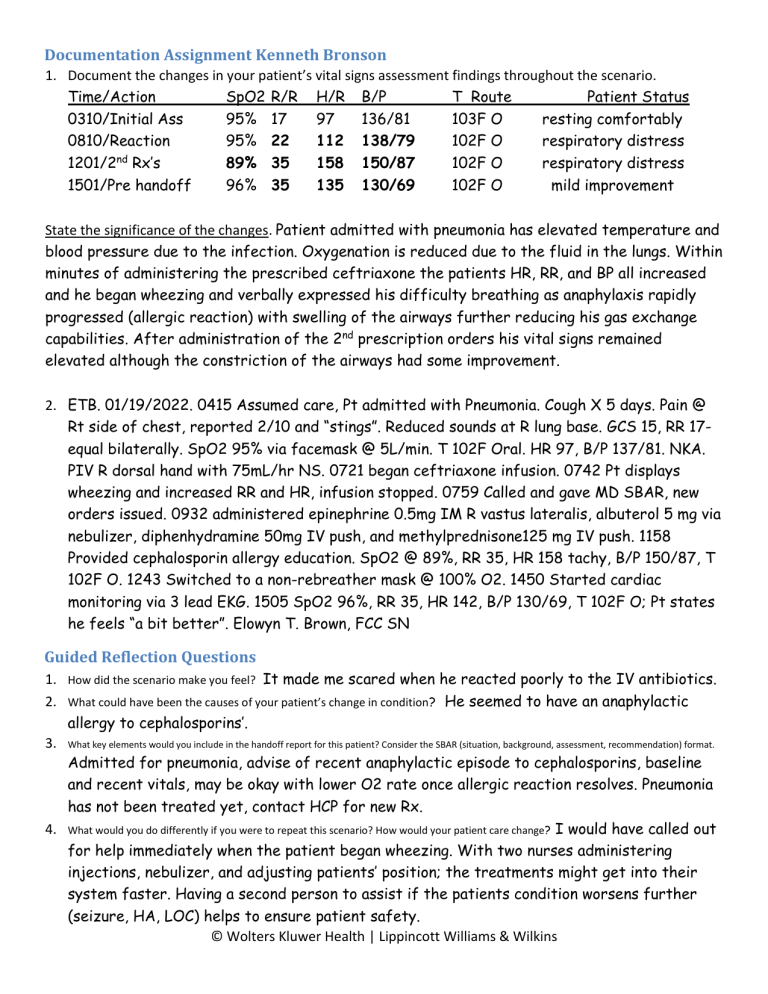
Documentation Assignment Kenneth Bronson 1. Document the changes in your patient’s vital signs assessment findings throughout the scenario. Time/Action SpO2 R/R H/R B/P T Route Patient Status 0310/Initial Ass 95% 17 97 136/81 103F O resting comfortably 0810/Reaction 95% 22 112 138/79 102F O respiratory distress nd 1201/2 Rx’s 89% 35 158 150/87 102F O respiratory distress 1501/Pre handoff 96% 35 135 130/69 102F O mild improvement State the significance of the changes. Patient admitted with pneumonia has elevated temperature and blood pressure due to the infection. Oxygenation is reduced due to the fluid in the lungs. Within minutes of administering the prescribed ceftriaxone the patients HR, RR, and BP all increased and he began wheezing and verbally expressed his difficulty breathing as anaphylaxis rapidly progressed (allergic reaction) with swelling of the airways further reducing his gas exchange capabilities. After administration of the 2nd prescription orders his vital signs remained elevated although the constriction of the airways had some improvement. 2. ETB. 01/19/2022. 0415 Assumed care, Pt admitted with Pneumonia. Cough X 5 days. Pain @ Rt side of chest, reported 2/10 and “stings”. Reduced sounds at R lung base. GCS 15, RR 17equal bilaterally. SpO2 95% via facemask @ 5L/min. T 102F Oral. HR 97, B/P 137/81. NKA. PIV R dorsal hand with 75mL/hr NS. 0721 began ceftriaxone infusion. 0742 Pt displays wheezing and increased RR and HR, infusion stopped. 0759 Called and gave MD SBAR, new orders issued. 0932 administered epinephrine 0.5mg IM R vastus lateralis, albuterol 5 mg via nebulizer, diphenhydramine 50mg IV push, and methylprednisone125 mg IV push. 1158 Provided cephalosporin allergy education. SpO2 @ 89%, RR 35, HR 158 tachy, B/P 150/87, T 102F O. 1243 Switched to a non-rebreather mask @ 100% O2. 1450 Started cardiac monitoring via 3 lead EKG. 1505 SpO2 96%, RR 35, HR 142, B/P 130/69, T 102F O; Pt states he feels “a bit better”. Elowyn T. Brown, FCC SN Guided Reflection Questions 1. How did the scenario make you feel? It made me scared when he reacted poorly to the IV antibiotics. 2. What could have been the causes of your patient’s change in condition? He seemed to have an anaphylactic allergy to cephalosporins’. 3. What key elements would you include in the handoff report for this patient? Consider the SBAR (situation, background, assessment, recommendation) format. Admitted for pneumonia, advise of recent anaphylactic episode to cephalosporins, baseline and recent vitals, may be okay with lower O2 rate once allergic reaction resolves. Pneumonia has not been treated yet, contact HCP for new Rx. 4. What would you do differently if you were to repeat this scenario? How would your patient care change? I would have called out for help immediately when the patient began wheezing. With two nurses administering injections, nebulizer, and adjusting patients’ position; the treatments might get into their system faster. Having a second person to assist if the patients condition worsens further (seizure, HA, LOC) helps to ensure patient safety. © Wolters Kluwer Health | Lippincott Williams & Wilkins