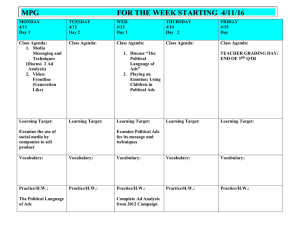
ORIGINAL ARTICLE Characteristics of Escitalopram Discontinuation Syndrome: A Preliminary Study Norio Yasui-Furukori, MD, PhD, Kojiro Hashimoto, MD, PhD, Shoko Tsuchimine, PhD, Tetsu Tomita, MD, PhD, Norio Sugawara, MD, PhD, Masamichi Ishioka, MD, PhD, and Kazuhiko Nakamura, MD, PhD Background: Antidepressant discontinuation syndrome (ADS) frequently occurs in patients who undergo an abrupt discontinuation of their antidepressant medication. Methods: We evaluated 25 consecutive outpatients with depression who discontinued their use of escitalopram. The presence of ADS was evaluated according to the Antidepressants Discontinuation Syndrome checklist. Results: Antidepressant discontinuation syndrome was observed in 14 of 25 patients. Frequent symptoms were dizziness (44%), muscle tension (44%), chills (44%), confusion or trouble concentrating (40%), amnesia (28%), and crying (28%). The treatment doses and plasma concentrations of escitalopram were significantly higher in patients with ADS than in patients without ADS. No group differences were observed regarding age, sex, or duration of escitalopram treatment before the discontinuation. Conclusions: These findings suggest that a higher dose and lower clearance of escitalopram lead to a higher risk of ADS. Very slow tapering is recommended for all patients. Key Words: escitalopram, antidepressant discontinuation syndrome, dose, concentrations (Clin Neuropharm 2016;39: 125–127) A ntidepressant discontinuation syndrome (ADS) occurs in approximately 20 percent of patients after an abrupt discontinuation of an antidepressant medication that was taken for at least 6 weeks.1,2 Typical ADS symptoms include flu-like symptoms, insomnia, nausea, imbalance, sensory disturbances, and hyperarousal. These symptoms are usually mild, last for 1 to 2 weeks, and are rapidly mediated with a reinstitution of the antidepressant medication.1,2 Long-term use of selective serotonin reuptake inhibitors (SSRIs) increases the synaptic levels of serotonin via blockade of the serotonin reuptake pump.3 The block results in a downregulation of postsynaptic receptors.3,4 A temporary deficiency of synaptic serotonin may occur after an abrupt withdrawal of SSRIs.3,4 This deficiency is compounded by the fact that the down-regulated receptors will remain in their relatively hypoactive state for days or even weeks.3,4 This down-regulation may directly or indirectly result in ADS via the downstream effects on other Department of Neuropsychiatry, Graduate School of Medicine, Hirosaki University, Hirosaki, Japan. Address correspondence and reprint requests to Norio Yasui-Furukori, MD, PhD, Department of Neuropsychiatry, Graduate School of Medicine, Hirosaki University, Hirosaki, 036-8562, Japan; E-mail: yasufuru@hirosaki-u.ac.jp Conflicts of Interest and Source of Funding: Funded by a Grant-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Research (JSPS, 15 K19239, 15 K19710, and 15H04754) and a grant from the Hirosaki Research Institute for Neurosciences. Norio Yasui-Furukori has received grant/research support or honoraria from and has worked with Asteras, Dainippon, Eli Lilly, GSK, Janssen-Pharma, Meiji. Mochida, MSD, Otsuka, Pfizer, Takada, and Yoshitomi. The other authors declare that they have no competing interests. The funders had no role in the study design, data collection or analysis, decision to publish, or preparation of the manuscript. Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved. DOI: 10.1097/WNF.0000000000000139 Clinical Neuropharmacology • Volume 39, Number 3, May/June 2016 neurotransmitter systems (eg, norepinephrine, dopamine, and γaminobutyric acid) that are implicated in depressive and anxiety disorders.3,4 Because tricyclic antidepressants and monoamine oxidase inhibitors are also serotonergically active, the same mechanism is implicated for the respective ADSs. However, tricyclic antidepressants also affect the cholinergic system.3,4 Thus, rapid discontinuation may cause parkinsonism symptoms and balance problems. Because monoamine oxidase inhibitors alter α2-adrenergic and dopaminergic receptors, discontinuation may cause agitation and psychosis.3,4 Escitalopram is used to treat patients with anxiety and major depressive disorders.5 This drug exerts a highly selective, potent, and dose-dependent inhibitory effect on human serotonin transport.6 By inhibiting the reuptake of serotonin into presynaptic nerve endings, the drug enhances the activity of serotonin in the central nervous system. Escitalopram contains serotonin norepinephrine reuptake inhibitors, including racemic citalopram.7,8 Escitalopram is approved for use at clinical doses of 10 and 20 mg (5 mg in certain subpopulations or as an initial dose). When administered orally, escitalopram reaches Tmax within 5 hours and is 56% protein bound. Escitalopram reaches steadystate concentrations in the blood within 1 to 2 weeks.9,10 The risk factors of ADS after escitalopram treatment are poorly understood.11,12 Therefore, we evaluated the characteristics of ASD induced by escitalopram withdrawal, including its pharmacokinetic profile, in a series of 25 consecutive depression patients. METHODS The subjects included 25 consecutive Japanese outpatients with depression who discontinued their use of escitalopram. The patients who had a repeated recurrence of depression, who had had residual depression symptoms, or in whom we could not confirm medication compliance were excluded from the study. The subjects in the present study had been treated with more than 10 mg/d of escitalopram for longer than 6 months. After careful confirmation of remission for at least 3 months, the doses were tapered to 5 mg/d, and each time interval between dose alterations was greater than 4 weeks. For example, a dose of 20 mg/d was decreased to 15 mg/d for at least 4 weeks, subsequently decreased to 10 mg/d for at least 4 weeks, then decreased to 5 mg/d for at least 4 weeks, and finally discontinued. The dose tapering regime was determined by the psychiatrists in charge of the patients on the basis of their clinical observations. No drugs other than some hypnotics such as brotizolam (n = 3) and zolpidem (n = 4) were taken by the subjects. The study was approved by the ethics committee of Hirosaki University, and all participants provided written informed consent. To evaluate the discontinuation syndrome, we used the discontinuation-emergent signs and syndromes (DESS) checklist.13 The DESS checklist is a patient-rated instrument that queries for signs and symptoms associated with the discontinuation of an SSRI treatment. Assessment of possible discontinuationemergent events was conducted using the DESS checklist. The 43-item list was developed by the investigators on the basis of www.clinicalneuropharm.com Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved. 125 Clinical Neuropharmacology • Volume 39, Number 3, May/June 2016 Yasui-Furukori et al TABLE 1. Percentage of DESS Reported by 10% of Patient in a Previous Report by Rosenbaum et al13 Prevalence in Prevalence in No. Total Subjects Total Subjects Subjects (N = 25) With ASD (n = 14) Dizziness Muscle tension Chills Confusion or trouble concentrating Crying Amnesia Emotional lability Dreaming Diarrhea Shaking Worsened mood Nervousness Depersonalization Unsteady gait Irritability Agitation Trouble sleeping Anger Muscle aches Vomiting Headache Nausea Sweating Fatigue Panic Sore eyes 11 11 11 10 44 44 44 40 79 79 79 71 7 7 6 6 6 6 5 5 5 5 4 4 4 4 4 4 3 3 3 1 1 1 28 28 24 24 24 24 20 20 20 20 16 16 16 16 16 16 12 12 12 4 4 4 50 50 43 43 43 43 36 36 36 36 29 29 29 29 29 29 21 21 21 7 7 7 an evaluation of signs and symptoms reported in the available literature. Among the 43-item list, we selected 25 items from the DESS that are reported by more than 10% of patients on the basis of a report by Rosenbaum et al,13 including agitation, amnesia, anger, chills, confusion or trouble concentrating, crying, depersonalization, diarrhea, dizziness, dreaming, emotional lability, fatigue, headache, irritability, muscle ache, muscle tension, nausea, nervousness, panic, shaking, sore eyes, sweating, difficulty sleeping, unsteady gait, vomiting, and worsened mood. The DESS checklist was given to all patients on the day of medication discontinuation. The DESS checklist was collected at every clinic visit, usually at 2-week intervals. For confirmation, we asked each patient to answer the following question: “During the past 14 days, have you experienced any changes in the following symptoms?” Patients chose 1 of 5 responses (new symptoms, old but worsened symptoms, old but improved symptoms, old and unchanged symptoms, symptoms not present). Discontinuation symptoms were observed until 4 weeks after the discontinuation. We defined discontinuation syndrome as 3 simultaneous, new, or worsened signs and symptoms because there are no criteria for discontinuation syndrome using DESS in previously reported studies. No signs or symptoms were confirmed before the discontinuation in our subjects. Blood samples (5 mL) were obtained 14 to 16 hours after the last 5-mg/d dose of escitalopram (just after discontinuation). The plasma samples were frozen and maintained at −20°C until analysis. The plasma concentrations of escitalopram and desmethylescitalopram were analyzed in duplicate using highperformance liquid chromatographic methods that were developed in our laboratory.14 The lowest limit of detection was 1.0 ng/mL, and the intra-assay and interassay coefficients of variation were less than 8.9% for both compounds. The statistical analyses were performed using χ2 and Student t tests. A P value of 0.05 or less was regarded as significant. SPSS 21.0 for Windows (SPSS Japan Inc, Tokyo) was used for statistical analyses. RESULTS Discontinuation syndrome after escitalopram treatment was present in 14 (56%) of 25 patients in our study. Frequent symptoms included dizziness (44%), muscle tension (44%), chills (44%), confusion or trouble concentrating (40%), amnesia (28%), and crying (28%) (Table 1). We readministered escitalopram because of severe discontinuation syndrome symptoms in 2 of 14 patients. Age, sex, and duration of escitalopram treatment did not differ between the ADS and non-ADS groups before dose tapering. The duration of tapering was significantly longer in patients with ADS than in patients without ADS. The treatment dose and the plasma concentrations of escitalopram were significantly higher in patients with ADS than patients without ADS (Table 2). DISCUSSION More than 50% of our patients developed escitalopraminduced ADS. We expected to observe a lower incidence of ADS. TABLE 2. Characteristics of Subject With and Without ADS Induced by Escitalopram Age, y Sex, male, n (%) Treatment dose, mg/d Duration of treatment dose, d* Duration of tapering, d Plasma levels of ECIT, ng/mL† Plasma levels of EDCIT, ng/mL† Without ADS (n = 11) With ADS (n = 14) Significance 35.4 (19.7) 5 (45) 14.1 (4.9) 188 (149) 49 (39) 14.2 (19.7) 3.8 (1.9) 35.6 (10.7) 4 (29) 18.6 (3.1) 196 (123) 136 (89) 36.5 (29.4) 10.2 (15.5) NS NS P < 0.05 NS P < 0.05 P < 0.05 NS *Duration of treatment dose just before the tapering. †Steady-state plasma levels at 5 mg/d of escitalopram just before discontinuation. ECIT indicates escitalopram; EDCIT, esdesmethylcitalopram; NS, no significant. 126 www.clinicalneuropharm.com © 2016 Wolters Kluwer Health, Inc. All rights reserved. Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved. Clinical Neuropharmacology • Volume 39, Number 3, May/June 2016 Generally, ADS is more common in patients who discontinue therapeutic agents with relatively short half-lives, such as paroxetine (15–20 hours), than in patients who discontinue agents with longer half-lives, such as fluoxetine (4–6 days).15 This evidence suggests that the use of therapeutic drugs with a relatively short half-life is a risk factor for development of ADS after discontinuation. The basic pharmacokinetic properties of escitalopram are described herein. Escitalopram is metabolized in parallel by at least 2 CYP enzymes, CYP3A4 and CYP2C19 (and to a lesser extent by CYP2D6).10 The elimination half-life of escitalopram is 27 to 33 hours, which is longer than that of paroxetine but shorter than that of fluoxetine.15 In our study, a diagnosis of ADS was made if a patient presented with at least 1 sign or symptom included in the DESS checklist. We may have overestimated the percentage because ADS, anxiety, and depressive symptoms are very similar. To confirm our findings, additional doubleblind, active control trials are required with larger samples. The results of this study demonstrated that a higher dose of escitalopram is associated with a higher prevalence of ADS. Age, sex, and duration of escitalopram treatment did not differ between groups before tapering. Antidepressant discontinuation syndrome was observed in 1 of 7 patients treated with 10 mg/d and 13 of 18 patients treated with more than 15 mg/d (P = 0.0213 in 2-tailed analysis). Therefore, it is reasonable to conclude that a higher dose of escitalopram is a risk factor for developing ADS. Antidepressant discontinuation syndrome occurred in many patients despite that we used a longer period of tapering in patients who received relatively higher doses of escitalopram and that we administered 5-mg/d escitalopram to all patients for at least 4 weeks before discontinuation. We observed that a relatively high steady-state concentration of escitalopram (at a dose of 5 mg/d) is a risk factor for ADS. Because clearance is approximately inversely proportional to the elimination half-life, patients with relatively high concentrations of escitalopram tend to have lower clearance and a longer elimination half-life. This observation does not agree with the long-accepted theory that ADS is more common in patients who discontinue the use of agents with relatively short half-lives. Because of the high dose and concentrations of escitalopram at 5 mg/d, we assume that these patients had a very high concentration of escitalopram during the treatment. Therefore, a longterm high concentration of escitalopram may be a risk factor for ADS. Plasma concentrations of escitalopram are significantly higher in poor CYP2C19 metabolizers than in patients who are extensive CYP2C19 metabolizers.16 The primary reason for the higher ADS prevalence in the present study may be a higher proportion of poor CYP2C19 metabolizers (among Japanese subjects).17 This study has several limitations. First, we did not apply a double-blind, placebo-active, controlled study design. Such a design would be better for determining the prevalence of ADS because symptoms and signs of recurrence are very similar to those of ADS. Second, we did not evaluate the clinical symptoms during treatment. Himei and Okumura suggested that ADS with paroxetine in depressed patients is associated with adverse reactions to paroxetine during the early treatment phase.18 Third, we did not measure the plasma concentration of escitalopram during treatment (especially important at the dose of 20-mg/d escitalopram). We also did not identify which patients had the CYP2C19 genotype. Finally, this study was conducted with a very small number of subjects. Therefore, we could not apply logistic regression analyses. For these reasons, our findings are preliminary. Future studies with a polished design and a large © 2016 Wolters Kluwer Health, Inc. All rights reserved. Escitalopram Discontinuation Syndrome number of subjects are required to overcome these disadvantages and to confirm our preliminary findings. In conclusion, our results suggest that ADS induced by escitalopram withdrawal is common. Relatively high doses and/or high concentrations of escitalopram are risk factors for ADS. Very gradual tapering over an extended period of time is recommended for all patients. REFERENCES 1. Haddad PM. Antidepressant discontinuation syndromes. Drug Saf 2001;24:183–197. 2. Bogetto F, Bellino S, Revello RB, et al. Discontinuation syndrome in dysthymic patients treated with selective serotonin reuptake inhibitors: a clinical investigation. CNS Drugs 2002;16:273–283. 3. Blier P, Tremblay P. Physiologic mechanisms underlying the antidepressant discontinuation syndrome. J Clin Psychiatry 2006;67(Suppl 4):8–13. 4. Haddad P. Newer antidepressants and the discontinuation syndrome. J Clin Psychiatry 1997;58(Suppl 7):17–21. 5. Garnock-Jones KP, McCormack PL. Escitalopram: a review of its use in the management of major depressive disorder in adults. CNS Drugs 2010;24:769–796. 6. Baldwin D, Woods R, Lawson R, et al. Efficacy of drug treatments for generalised anxiety disorder: systematic review and meta-analysis. BMJ 2011;342:d1199. 7. Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 2009;373(9665):746–758. 8. Kirino E. Escitalopram for the management of major depressive disorder: a review of its efficacy, safety, and patient acceptability. Patient Prefer Adherence 2012;6:853–861. 9. Pastoor D, Gobburu J. Clinical pharmacology review of escitalopram for the treatment of depression. Expert Opin Drug Metab Toxicol 2014;10: 121–128. 10. Rao N. The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet 2007;46:281–290. 11. Fava GA, Gatti A, Belaise C, et al. Withdrawal symptoms after selective serotonin reuptake inhibitor discontinuation: a systematic review. Psychother Psychosom 2015;84:72–81. 12. Baldwin DS, Montgomery SA, Nil R, et al. Discontinuation symptoms in depression and anxiety disorders. Int J Neuropsychopharmacol 2007;10:73–84. 13. Rosenbaum JF, Fava M, Hoog SL, et al. Selective serotonin reuptake inhibitor discontinuation syndrome: a randomized clinical trial. Biol Psychiatry 1998;44:77–87. 14. Herrlin K, Yasui-Furukori N, Tybring G, et al. Metabolism of citalopram enantiomers in CYP2C19/CYP2D6 phenotyped panels of healthy Swedes. Br J Clin Pharmacol 2003;56:415–421. 15. Hiemke C, Härtter S. Pharmacokinetics of selective serotonin reuptake inhibitors. Pharmacol Ther 2000;85:11–28. 16. Chang M, Tybring G, Dahl ML, et al. Impact of cytochrome P450 2C19 polymorphisms on citalopram/escitalopram exposure: a systematic review and meta-analysis. Clin Pharmacokinet 2014;53:801–811. 17. Kurose K, Sugiyama E, Saito Y. Population differences in major functional polymorphisms of pharmacokinetics/pharmacodynamics-related genes in Eastern Asians and Europeans: implications in the clinical trials for novel drug development. Drug Metab Pharmacokinet 2012;27:9–54. 18. Himei A, Okamura T. Discontinuation syndrome associated with paroxetine in depressed patients: a retrospective analysis of factors involved in the occurrence of the syndrome. CNS Drugs 2006;20:665–672. www.clinicalneuropharm.com Copyright © 2016 Wolters Kluwer Health, Inc. All rights reserved. 127