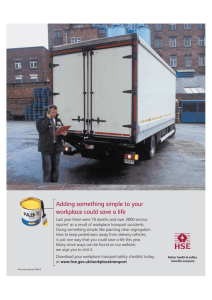
Discussion Creating a successful workplace health promotion program model is a methodical process that encompasses four (4) primary stages. Stage 1- Assessment and Analysis of Workforce To elucidate, for a workplace health program to be successful, it must be tailored to the needs of its employee population, and ergonomic, aiding in achieving personal and organizational goals of said population. This stage is the foundational phase and can be completed by means of a workplace health needs assessment (HNA). A health needs assessment (HNA) aims at ascertaining the habitual inclinations of the workforce when it comes to their health such as lifestyle choices, potential health and wellbeing challenges, and factors that lead to such like, physical working conditions and social support, personal issues, and at the organizational level, culture, policies, and practices, as well as identifying and assessing current health interventions in the workplace. The assessment allows for interventions to be planned while addressing the ascertained needs. The assessment is done by permitting a group of persons to analyze the health needs of the workers. This said group must include individuals that are impartial and unprejudiced, that are appointed by the workforce or the trade union. Moreover, this process should be a natural and a consultative one that can either be informal or formal. Systematic routes that possess the trait of being informal encompass garnering information through conversations, and setting up throughout the workplace, opinion boxes and bulletin boards. Also, emails can be sent requesting ideas. The aforementioned encourages input from the workforce, so the health promotion program would achieve the status of being a customized one. A more formal approach would be conducting pre-prepared employee health surveys or environmental audits. Furthermore, the surveys prepared must be of a manageable length and possess a user-friendly layout that contains logical, unambiguous, comprehensive questions that are related to the workforce so, their health and wellbeing, working hours, job types, and their working environments. It must also include a copious amount of employee input so opinion boxes should be included. The period following the conduction of the surveys from the large cohort should be spent with the employees in health circles. This fosters open-ended discussions that address the health concerns of the staff and find The discussion outcomes are documented and disseminated to all employees, so employee involvement is encouraged once more. On the other hand, the environmental audits would involve collecting and monitoring relevant organizational data such as employee demographics, performance appraisals, absenteeism reports, overtime hours, injury and disability rates and root cause analyses. To elaborate further, root cause analyses investigate the source of misfortunes in the health of the employee population as it relates to their environments. The ambient surroundings heavily influence a person’s behavior. To illustrate, if a person lives in a household of smokers and considers themselves to be a smoker as well, simply commanding them to quit smoking without knowing relevant background information would not suffice. Here, the likelihood of recurrence occurring is high and this would impede the program from being successful. Therefore, both approaches should advisedly be participative, encouraging employee involvement from the beginning because only through such can the shared responsibility and commitment the employee and the organization have to employee health be upheld. In conclusion, the health needs assessment (HNA) must ascertain the health issues of the workforce, employee interests, analyze the current health and policy interventions, so that a successful workplace health program can be created and enacted. Stage 2 – Planning the Program After the workplace health needs assessment has been conducted, a meticulous planning stage must follow in preparation for the implementation of the program. The planning stage deals with prioritizing the goals and outcomes for workplace health programs, identifying tasks, and constructing effective planning strategies for the implementation of the program. Moreover, goals are established for the workplace health program that play an integral role. These goals can be viewed as the desired health outcomes or current health risks for employers. When establishing goals, it is advised to use the SMART criteria, which define goals as Specific, Measurable, Achievable, Relevant, and Timely. Apart from setting goals, the overall planning stage must be supervised keenly. This would require a basic governance structure that would use their ingenuity, experience and knowledge to administer, manage health promotion activities, make strategic decisions, write reports, and provide impetus for these interventions. Hence, a steering group is a necessity. An ideal steering group is representative of the organization, consisting of different employee groups in the organization. Also, size of steering groups may vary according to the size of organizations. The group must adhere to the following organizational strategies to prevent any contingencies from occurring: An individual must be appointed to serve under the senior leadership role, acting as the role model, that supervises all activities pertinent to the program. Junior members must be given specific tasks to improve efficiency and productivity. Such tasks may include the adequate allocation of organizational resources for the health program, encouraging input from the workforce during the planning phase, budgetary planning, coordinating group activities etc. Moreover, a hierarchical structure can be established among the junior members for easier designation of tasks and operationalization of the program elements. A member could be appointed as the workplace health coordinator that oversees the group activities. In relation to activities related to the financial aspect of this program, it is advised to remain provident. Additionally, a workplace health improvement action plan and theory of change should be drawn up with the available organizational resources. Throughout this process, consistent communication with all employees must be upheld. Communication between employers, employees and those leading the development of the interventions is key to the success of all stages of the development and delivery of workplace health interventions. Communication is necessary because it prevents employees from acting in oblivion in relation to the program and it builds rapport and engagement. Communication can be facilitated through face-to-face meetings, health days, electronic and printed media. These approaches ensure that information is distributed to the entire employee population. Lastly, information about the workforce should still be collected for planning and evaluation. In addition, is advised that focus is placed on at least one or two programs at first and build on those in lieu of a profuse number of failed trials in the beginning. In conclusion, it should be noted that a program’s success is not measured by its adherence to all these strategies but through the intricate planning process that is tailored to the workforce. Stage 3 – Implementation When improving the health of the workforce, most employers pursue the thought of what the employees themselves can do. These actions include exercising regularly, quitting smoking, and eating balanced diets. However, much to their disillusionment, this strategy is frequently very loosely followed, producing failed attempts at curbing the health issues. Therefore, it is of utmost importance that whilst it is imperative that the issue is dealt with at a personal scale, it requires a broader vantage point that takes into the consideration, employees’ ambient surroundings. When paraphrased, the diligent statement by WHO claims that health is more than the absence of a mere disease or infirmity, it is the social, mental, and physical wellbeing. Actions influence a person’s health, but health is also determined by the environments in which those actions take place. Root cause analyses would rule these out in the assessments, so that possible solutions could be developed and implemented in this stage. Hence, by simply adjusting the work environment, the health status of the workforce can improve. The implementation stage includes ensuring the steering group continuously monitors program’s progress, and properly deals with arising issues, all while keeping the target group’s best interest at hand. During implementation, the steering group must remain active by clearly defining roles so that the program is carried out smoothly and if possible, arrange a trial for the program with a small group before having it be tested on the organization’s entire employee population. From this trial, results obtained should be evaluated and the program should be adjusted accordingly. Moreover, this stage must quickly succeed the planning stage so that employees deliver a fast response to their concerns addressed in the assessment phase. In conclusion, the implementation stage encompasses the steering group piloting and closely monitoring the program’s progress. Stage 4 –Evaluation The evaluation stage deals with assessing the impact of the program on the workforce (employees and management), surplus values and return on investment. Good evaluation methods are not time consuming and produce findings that assist in refining the existing program. They identify gaps in the program and describe the effectiveness of the invested resources. Since, evaluation is an important stage that also aims to examine issues such as healthcare costs, absenteeism, health outcomes, productivity etc, it requires good evaluation methods. The first of these methods involves comparing data obtained to the theory of change. The theory of change is defined as a tool that aids in describing the issue to be addressed, the preferrable changes (key outcomes) and the activities to be carried out in implementing the program. Through comparison, areas such as engagement, awareness can be improved. Secondly, carefully formulated evaluation questions should be answered to measure the success of the existing program. These questions should be salient, and entirely logical. This method measures impacts for example behavioral changes. For instance, if a question was based on the return on investment, direct, detailed answers would be given. Moreover, return on investment (ROI) is considered the metric gold standard for evaluating workplace health intervention outcomes and calculates the money saved from implementing the program relative to money invested into the program. The final method is to create an evaluation design. This design aims to determine whether the goals have been achieved and if any other factor played a role in the program’s fate. Once intended outcomes are agreed, a decision on evaluation methods can be made. However, a method should only be selected after considering the timeframe of the evaluation, available skills and other resources. Furthermore, the organizational context should be reviewed during the evaluation stage. Organizational events such as changes in management, downsizing, promotional periods should be noted when evaluating the program. interventions. Lastly, lessons learnt from the current evaluation stage should be recorded and made available for future health programs. This would serve as a reflective process that fosters more insight into the many intricacies of implementing a health program. In conclusion, the evaluative stage assesses the processes, its economic and physical and mental impact of the program. Overall, it aids in refining the existing workplace health program and future models.