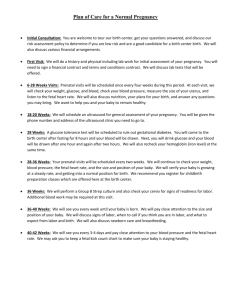
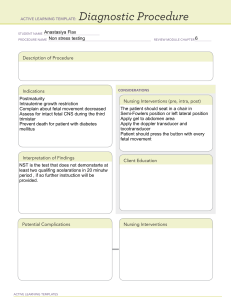
Preconception Care Targets all women of childbearing age ● After puberty and before menopause Goals ● Improve health ● Identify goals to meet before pregnancy ● Develop a lifestyle of wellness Key Targets ● Healthy spacing ○ 18-24 months ● Nutrition and exercise ○ Folic acid (for nervous system of fetus) ■ Deficiency could cause spina bifida due to neural cord defects ○ Iron ○ Healthy BMI ● Screenings ○ Pap smear ○ Mammogram ○ Dental care (high risk for periodontal infections) Nursing Interventions ● Safe spacing ● Substance abuse ● Exercise ● Nutrition ● Exposure to infectious disease ● Mental health ● Support system ● Readiness ● Preventative care ● Environmental conditions Fetal Growth and Development Human Gestation ● 40 weeks after last menstrual period (actually 38 because of ovulation period) ● 38 weeks after conception ● Due date, EDC (estimated date of confinement), EDD (estimated due date), EGA (estimated gestational age) Trimesters ● First: conception to 13 weeks ● Second: 14 weeks to 26 weeks ● Third: 27 weeks to birth Conception ● 2 zygotes: sperm and egg Sperm 1 ● ● Ovum ● ● Lifespan in the female reproductive tract: 48 to 72 hours Can reach the ova in as little as 30 minutes Oogenesis begins during fetal development (longer genetic lifespan then more risk) Ovulation ○ Ovarian follicle ruptures and releases ovum ○ Corpus luteum remains on ovarian surface to temporarily provide necessary hormones until the placenta is large enough to take over (about 7 weeks) ■ Ex: hard boiled egg shell with 2 layers ● Ovum fertile for 24 hours after ovulation ● Cannot move on its own Fertilization ● Ovum and sperm unite at ampullary portion of the fallopian tube ● Once 1 sperm enters, ovum closes to additional sperm ● Zygote ● Propelled along the tube through the peristaltic movements of the fallopian tube and the tube’s cilia (hairlike that wave through tube) Process ● Day 1: zygote ● Day 2: embryo ● Day 3: embryo moves further through fallopian tube ● Day 4: morula ● Day 5: blastocyst ○ Cells differentiate, fluid filled blob, gestational sac ● Day 6: implantation ○ In endometrium and beginning of placenta ● Takes 5 days to make it to the uterus to implant Blastocyst ● 3 primary germ layers ○ Ectoderm (skeleton) ○ Mesoderm (organs) ○ Endoderm (inner lining of organ) Implantation ● 6 days after fertilization ● Occasionally, implantation bleeding occurs as the blastocyst implants in endometrial lining and decidua differentiates Support Structures ● Begin to form at implantation ○ Placenta ○ Amniotic membranes ○ Amniotic fluid ○ Umbilical cord Placenta ● Develops at the site of implantation 2 ● ● ● ● Fetal tissue Originates from chorionic villi (hairlike) Syncytial layer produces hormones (HCG and HPL) 0-20 weeks ○ Grows rapidly ○ Covers a large portion of the inner uterine surface ● 20-40 weeks ○ Will only grow thicker for remainder of pregnancy and proportionately less of the inner uterine surface ● No exchange of maternal/fetal blood in health pregnancy ○ 2 distinct circulatory systems ○ Passage of smaller molecules ● Adequacy of maternal circulation will affect adequacy of fetal perfusion ● Hypertension, diabetes, and kidney disease could impact maternal fetal exchange ● Functions ○ Respiratory unit ■ Oxygen and carbon dioxide ○ Nutritional unit ■ Glucose, amino acids, vitamins, minerals, fatty acids, water ○ Elimination unit ■ Don’t poop Amniotic Membranes ● Chorion (outer) and amnion (inner) become amniotic membranes ○ Like hard boiled eggs ● Produces amniotic fluid ● Decidual layer produces prostaglandins ● Barrier from infection Amniotic Fluid ● Fluid produced across the membranes ● Protects fetus and umbilical cord ● Regulates the temperature of the fetus (newborns need help) ● Aids in muscular development allowing the fetus to move ● Enables symmetrical development and growth (can be different if not enough fluid) ● Prevents adherence of membranes to fetus ○ Amniotic bands ■ Abnormality in growth and cuts off circulation of limb ○ Potter syndrome ■ No fluid ■ Not viable ● At term, normal fluid volume is 800-1200mL, average 1000 ● Amniotic fluid volume will affect the size of uterus ○ If not enough fluid, baby’s skin could adhere to placenta and cause abnormalities ● Decreased fluid= decreased birth weight Umbilical Cord 3 ● ● Connects the embryo to the chorionic villi of the placenta Wharton’s Jelly ○ Around vessels of cord (thick jell-o) is cushion to protect especially during birth ● Coils if healthy ● Level 2 ultrasound on high risk pregnancies to see coils in cord Fetal Circulatory System ● Opposite from adult circulation ● 2 arteries: carry unoxygenated blood and waste products from the fetus to the placenta ● 1 vein: carries oxygenated blood, nutrients from the placenta to the fetus Embryonic Stage ● Implantation to 8 weeks gestation ● Begins about the time of the missed period ● Critical period of organogenesis ● Placenta/support structures present ● Maternal/fetal perfusion ● Risk for teratogenicity Teratogens ● Any agent that can disturb the development of an embryo or fetus ● Drugs and chemicals ● Maternal medical conditions ○ Diabetes: hyperglycemia from pregestational diabetes in embryonic fetal development, DKA ● Infections agents ● Environmental ● Zika: most concerning during first 8 weeks ● Drugs ○ Nicotine (cigarettes) ○ Alcohol ○ Marijuana ○ Isotetinoin (acne) ○ Warfarin (blood thinner) ○ Ace inhibitors/-prils (blood pressure) ● Infectious agents ○ Cytomegalovirus ○ Rubella ○ Varicella (chickenpox) ○ Toxoplasmosis ○ Listeria (foodborne illness) ○ Zika (mosquitoes) ● Environmental ○ Ionizing radiation ■ Xray, CT scan, PET scan, MRI ○ Hyperthermia ■ Sauna, hot tub (infection risk) 4 6 to 8 weeks ● Critical period ● Eyes, ears, and nose develop ● Brain and cranial nerves ● GI ● Cardiac septum and valves ● Liver making RBCs ● Development of fetal circulation ● Organogenesis ● FHR: 110-160 ● Increased cardiac output ● Fetal hemoglobin (pick up oxygen easier) ○ Higher affinity for oxygen, carries 20-30% more oxygen than adult hemoglobin ● Higher concentration of hemoglobin (hematocrit) ● Fetal circulation (3 shunts) Fetal Circulatory System ● Primary goal: oxygenated blood perfused to all fetal body parts ○ Ductus venosus ■ Bypasses the liver ■ Takes oxygenated blood from the umbilical vein to the vena cava and heart ○ Foramen ovale ■ Temporary opening between the right and left atria ○ Ductus Arteriosus ■ Bypasses the lungs ■ Temporary vessel connecting aorta to pulmonary trunk ● All shunts close after baby born Fetal Stage ● 9th week of gestation until birth ● Refining structures ● Perfecting function ● Growing ● Gaining weight ● Less vulnerability to teratogens (except CNS) ○ Marijuana, nicotine, alcohol risky still 12 weeks ● Fetal heart tones by handheld doppler ● Fetal movements ● Early reflexes ● Tooth buds ● Bone ossification (femur) ● Liver producing RBCs (continuing) ● Kidneys begin secreting urine (fetal urine is typically same as amniotic fluid) 16 weeks 5 ● Uterus into maternal abdomen ● Immunoglobulin M (IgM) ● Lanugo: hair ● Pancreas ● Swallowing ● Lower GI tract begins to produce meconium (dark brown/black tarry fetal waste product) ● Sex can be seen on ultrasound ● Start feeling flutters ● 16 to 20 mom can feel the baby move 20 weeks ● Quickening (EDC check) ● Hair formation on the head ● The upper intestine contains meconium ● Muscle development ● GI tract→ lower to upper development 24 weeks ● Eyelids open ● Eyebrows and eyelashes ● Vernix Caseosa secreted by sebaceous glands ○ Thick waxy white substance on skin to protect from fluid ● Lecithin surfactant (lungs) ○ Breath and open alveoli ○ Have to have to survive ○ Surfactant reduces surface tension ● Alveoli ● Threshold of viability 28 weeks ● Brain developing rapidly ● Developmental delays born before 28 weeks due to brain developing ● Alveoli are starting to mature (lungs) ● Immunoglobulin G (IgG) ○ Begins to cross the placenta and provide passive immunity ● Retinal blood vessels start to form, highly susceptible to damage ● Give TDAP because IgG can pass through placenta ● Micropremies: blindness due to increase supplemental oxygen 32 weeks ● Subcutaneous fat is deposited ● Iron, calcium, phosphorus stores are starting to develop ○ Prime bone ossification ● CNS causes rhythmic breathing movements ○ Inhale and exhale amniotic fluid by medulla ● Helps with temperature control ● Can be on CPAP and breath on own Lungs 6 ● ● ● Last system to mature Pulmonary surfactants, made by fetus, present in amniotic fluid Sphingomyelin ○ Remains constant ● Lecithin ○ Begins around 21 weeks ○ Increases ● L/S ratio reaches 2:1 lungs are considered mature (approx 32-36 weeks) ○ Run lab to see if the baby can breath on its own ● Decreased maternal blood flow can accelerate fetal lung maturity ○ Fetal stress release cortisol (amps up surfactant production and lung maturity) ● Diabetes and insulin resistance can delay fetal lung maturity ○ Gestational and prior diabetes 36 weeks ● Distinct sleep/wake cycles ● Additional subcutaneous fats are deposited ● Lung surfactant ratios improve ● One or two creases are present at the sole of the foot ○ Smooth if preemie but creases if full term ● Lanugo starts to diminish (bald spots) ● Meconium accumulation ● Vertex presentation (head down) 40 weeks ● Vernix caseosa mostly gone ● The soles of the feet have creases that cover at least ⅔ of the surface ● CNS and neurological Multifetal pregnancy ● 1 in 43 births ● Fraternal same sex ● Fraternal different sex ● Identical same sex Dizygotic twins (fraternal) ● 2 mature ova are released and fertilized by 2 separate sperm ● 2 amnions, 2 chorions, 2 placentas ● Incidence increases with family history, race (nonwhite), maternal age (>35 years old), number of times mother has given birth, fertility treatments (IVF) ● Lower risk than identical Monozygotic twins (identical) ● 1 ovum fertilized by 1 sperm ● Divides into 2 zygotes ● Identical twins ● Same sex and genotype ● 1 or 2 amnions ● 1 or 2 placentas 7 ● 4 in 1000 births Psychosocial Changes in the Pregnant Family Developmental tasks for the family ● Dependent upon age of oldest child Nursing assessment of maternal readiness ● Intendedness ○ Planned vs. unplanned ○ Wanted vs. unwanted vs. mistimed ● Ambivalence ○ Fears about assuming a new role ● Acceptance ○ Quickening and altered physical appearance ■ Around when people begin to notice the “baby bump” ● Introversion ○ Turning in on oneself ● Mood swings/emotions ● Changes in body image ○ How are they coping? Developmental progression of the mother/child relationship 1. Acceptance of the biological fact of pregnancy (positive pregnancy test) 2. Acceptance of the growing fetus as distinct from herself (i am pregnant) 3. Realistic preparation for birth and parenthood (i am having a girl) Psychological tasks of the mother ● Motivation of behavior, goals women strive for ○ Ensuring safe passage through pregnancy, labor, and birth ○ Seeking of acceptance of this child by others (baby’s name) ○ Seeking of commitment and acceptance of self as mother to the infant ○ Learning to give oneself on behalf of one’s child (selfless) Pregnant woman’s relationship with her mother ● Woman who was well nurtured by her mother may view her mother as a role model and emulate her ● Woman who views her own mother as a “bad mom” may worry that she will make similar mistakes Paternal adaptation ● Accepting the pregnancy ○ Couvade syndrome ■ Nausea ■ Weight gain ● Identifying with the father role ○ Financial security ○ Image of father, hanging out with father friends ● The role of the nurse ○ Acknowledge them 8 Supporting the non pregnant partner ● Not the biological father ● Same sex couple ● Role of the nurse ○ Include them in care Sibling adaptation ● 1 year old ○ Largely unaware ● 2 year old ○ May notice a change in mother’s appearance ○ Clingy behavior ○ Regression in toilet training or eating ● Preschooler ○ May want to learn about their own growth and development ○ May struggle to understand how fetus is fed or clothed ● School age ○ “How did the baby get there?” ○ “How will the baby get out?” ● Adolescents ○ May feel embarrassed ○ May present a more challenging relationship with family ■ Especially in a blended family ● Role of the nurse ○ Include the sibling Grandparent adaptation ● Most grandparents adjust well to their new role ● Some may inadvertently decrease the self-esteem of parents-to-be ● Can be a very influential person in the transition to parenthood Managing Maternal and Fetal Health Presumptive signs of pregnancy ● Amenorrhea (loss of period) ● Nausea and vomiting (morning sickness) ● Breast tenderness ● Urinary frequency ● Fatigue ● Quickening (16 to 20 weeks) ● Weight gain ● Breast and abdominal enlargement ● Skin changes ● Pelvic changes ● Elevated basal body temperature (slightly increased because of increased metabolism) ● Natural family planning ○ Check temperature for ovulation 9 ○ Get pregnant then stays high if pregnant Probable signs of pregnancy ● Uterine enlargement ● Braxton-hicks contractions ● Uterine souffle ○ Swishing of moms blood entering into placenta ● Pregnancy test ○ Urine or blood ○ HCG ● Ballottement ○ Assess solid object with fluid filled environment and jiggle Positive indicators of pregnancy ● Visualization of fetus by ultrasound ● Fetal movements palpated by examiner ● Fetal heart rate distinct from mother (faster) ● Ultrasound ○ 6 weeks ● Handheld doppler ○ 10 weeks ● Fetoscope ○ 16 weeks Pregnancy tests ● Early detection= early care ● Human chorionic gonadotropin (HCG) ● Maternal serum: 6 to 11 days post conception ● Maternal urine: 10 to 14 days post conception ○ Use first morning urine that is more concentrated ● Patient education and timing Hormones of pregnancy ● Human chorionic gonadotropin (HCG) ○ Originates in the trophoblast layer of the blastocyst ○ Stimulates the corpus luteum to release estrogen and progesterone until the placenta is big enough to take over (around 7 weeks) ● Estrogen ○ Originates in the corpeus luteum until the placenta takes over ○ Stimulates uterine growth ○ Breast development ○ Estrogen levels rise when close to birth ● Progesterone ○ Low levels can cause miscarriage or preterm labor ○ Originates in the corpus luteum until the placenta takes over ○ “Pro-gestation” (keeps the woman pregnant) ○ Relaxes smooth muscles (calms uterus) ○ Prepares breasts for lactation 10 ○ Progesterone levels lower when close to birth ● Relaxin ○ Ripens the cervix ○ Originates in the corpus luteum, then in the placenta ○ Softens tissues, joints, and pelvic ligaments ○ Aids in cervical ripening ● Human placental lactogen (HPL) ○ Originates in placenta ○ Insulin antagonist (increase in mom’s blood sugar) ○ Ensures glucose availability for fetus ● Oxytocin ○ Originates in the posterior pituitary ○ Stimulates uterine contractions ○ Produces milk ejection (let down reflex) ○ “Bonding” hormone ○ Can happen with nipple stimulation and sex ● Prostaglandin ○ Originates in the decidual layers of endometrium/placenta ○ Stimulate smooth muscle contractions ○ Stabilizes maternal blood pressure Cardiovascular system changes in pregnancy 1. Protects women's normal physiological functioning 2. Meets metabolic demands of pregnancy 3. Provides for fetal growth and developmental needs Cardiovascular system ● Anatomical changes ○ Slight cardiac hypertrophy (larger heart) ○ Diaphragm displaced upward (1st trimester) ○ Systolic murmur ● Pulse rate ○ Increases to 10 to 15 beats per minute ● Palpitations, premature atrial contractions ○ Increase amount of blood ● Blood pressure ○ Less than 130/80 ○ 1st trimester ○ 12 to 20 weeks: progesterone exerts effect on peripheral vasculature ○ Diastolic changes ○ Not normal for BP to increase in pregnancy due to smooth muscle relaxers ○ 135/85 is a high BP ○ Eclampsia: giant seizure or vasospasm ○ Supine hypotension syndrome ■ > 20 weeks ■ Never lay flat on back 11 ● ● ● ● ● ● ■ Weight of fetus compresses the inferior vena cava ■ C section not centered due to adjusting weight onto side Blood volume ○ Increases 40-50% above non pregnancy levels to meet metabolic demands ○ Peaks at 32 to 34 weeks ○ Epistaxis and gums bleeding is normal Hemodilution ○ Plasma volume and RBC production ■ Makes more more plasma and more RBC ○ Pregnancy hemoglobin and hematocrit ■ Below 11 is concerning ■ Lower in pregnant women ○ Pseudoanemia of pregnancy Normal CBC in pregnancy ○ Hgb: greater than 11 ○ Hct: greater than 33 ○ WBC: 5,000 to 15,000 ■ Immune system is ramped up Cardiac output ○ Increases by 30-50% by 32 weeks then it is maxed out ○ Positioning ■ Anticipatory guidance ■ Should sleep on left or right side or semi-fowlers Colloid osmotic pressure ○ Decreases gradually during 1st and 2nd trimesters ○ Changes fluid and electrolyte balance ○ Causes a fluid shift from intra to extravascular space in normal pregnancy ■ Dependent edema (toes, feet, and ankles) ■ Carpal tunnel syndrome ○ Patient education ■ Decrease sodium intake ■ Splint ■ Keyboard and phone usage Edema above the waist is not normal ■ Significant increase in weight from edema is not normal Coagulation times ○ Protective effects to minimize bleeding ■ Clotting factors increased ■ Blood coagulation increased ■ Fibrinolytic activity is decreased ○ Risk of thrombosis ■ 5 to 6 fold increase ○ Patient education ■ Road trip: stop every 2 hours to walk around and empty bladder 12 ■ Airplane: get up once an hour ■ Anxious→ increased respirations→ chest pain→ increased heart rate→ pulmonary embolism→ check pulse oximetry ■ Calf pain→ check for DVT Respiratory changes ● Diaphragm displaced upwards ● Hormonal effect: ligaments of ribcage to relax ○ Band size of bra permanently changes ● Elevation of basal metabolic rate ○ Increased respirations and some shortness of breath ○ No lifting heavier than 20 lbs Breasts ● 1st trimester: fullness, sensitivity, tingling, heaviness, pain ● Montgomery’s tubercles more prominent ○ Release sebaceous fluid to toughen nipples ● Increased pigmentation ○ Darker nipples ● Colostrum formed as early as 16 weeks Uterine physiological changes ● Endocrine effect ● Growth results ○ Increased vascularity and dilation of vessels ○ Hyperplasia and hypertrophy of fibers ■ Cells get larger and more cells ○ Mechanical pressure of growing fetus ■ After 12 weeks Uterus ● Growth occurs at a predictable rate ● 1st trimester: bimanual palpation ● 12 to 14 weeks: symphysis pubis ● 20 weeks: umbilicus ● 36 weeks: xiphoid process ● 40 weeks: fetus flips and engages ● Top of uterus is the fundus ● Fundal height after 20 weeks in equal to cm give or take 2 cm ○ Example: 26 weeks would be 24 to 28 cm ● Round ligament (bikini line) ○ Very stretched and sacral stretched ○ May feel sharp sudden pain/cramping ● Hegar’s sign ○ Possible indication of pregnancy ○ Soften isthmus ● Uterine changes due to hormones 13 ● ○ Cramping with vaginal bleeding is not normal Quickening and lightening ○ Quickening: 16 to 20 weeks ■ Maternal palpation of fetal movements ■ Tentative clue to dating a pregnancy ○ Lightening: 36 to 40 weeks ■ Subjective feeling of decreased abdominal distention as the fetal presenting part settles into the pelvis (baby dropped) Cervix ● Goodell sign ○ ● ● relaxin→ cervix softening Chadwick sign ○ Changes color to bluish tone Friability ○ Tap cervix and starts to bleed which is normal because increased blood volume and relaxed muscles Vagina ● Leukorrhea: white mucoid discharge ○ WBC released in vagina ● Screening and education ○ Leaking of fluid ○ Water breaking: clear fluid ○ Not normal for gushing fluid Renal ● Hormonal influence ○ Increased GFR by 50% (lots of filtration) ■ Normal glycosuria: trace or 1+ (100 mg/dL) ■ Normal proteinuria: trace (30 mg/dL) ● Uterine pressure ○ Urinary reflux and stasis ○ Decreased ureter tone ○ Urine backs up in kidneys ● Consequences of pregnancy related changes ○ Collaborate with urologist ● Patient education ○ Don’t hold urine ○ Hydrate ○ UTI or kidney stones possible Gastrointestinal ● Slower (constipation) ● Morning sickness: hypoglycemic effect ● Hormonal effects ● HCG and progesterone ● Delayed gastric emptying and motility 14 ● ● ● Ptyalism: more saliva in mouth GERD: common because sphincter is relaxed Hyperemesis gravidarum ○ Go into ketosis ○ Less efficient ○ Lose weight ○ Large number of ketones ○ Can be a teratogen ● Blood sugar ○ Drops in 1st trimester ○ Raises in 2nd and 3rd trimesters Musculoskeletal ● Relaxin: muscles relaxing ● Diastasis recti: 3rd trimester, ab muscles burst open ○ 6 weeks post birth start doing crunches to strengthen core ● Lordosis: lumbar vertebra curving and can cause back pain Peripheral vascular ● Physiological edema ○ Third spacing due to colloid osmotic pressure ● Varicose veins ○ In rectum: hemorrhoids ○ Caused by progesterone ○ Temporary ○ Increased blood volume ○ Dilated and relaxed veins Skin ● Chloasma ○ Release more melanin ○ Butterfly pattern ○ Temporary ● Linea nigra ○ Dark line down abdomen ○ Temporary ● Palmar erythema ○ Sweaty ○ Red ○ Increased blood volume ● Striae gravidarum ○ Stretch marks ○ Genetics (collagen) ○ Post baby are silvery Nursing Care during Pregnancy Establishing dates 15 ● ● Last menstrual period: first day Naegele’s rule 1. Establish 1st day of last menstrual period 2. Add 7 days 3. Subtract 3 months 4. Add 1 year Describing pregnancy ● Gravida ○ Any pregnancy, regardless of duration ● Para ○ Number of births (at least 20 weeks) ○ Includes stillbirth ● Primigravida ○ Pregnant for the first time ● Multigravida ○ Pregnancy for at least the second time ● Primiparous ○ Giving birth for the first time ● Multiparous ○ More than 1 birth TPAL ● T: number of term pregnancies (37 weeks and beyond) ● P: number of preterm pregnancies (36 weeks and 6 days and less) ● A: number of pregnancies aborted before 20 weeks (miscarriage or abortion) ● L: number of children now living Example: A.S. is 10 weeks pregnant, history of 2 miscarriages, 1 elective abortion, a daughter born at 38 weeks, twin sons born at 35 weeks, and a 3 year old born on his due date ● G: 7 ● T: 2 ● P: 1 ● A: 3 ● L: 4 Prenatal visit schedule ● Initial visit: 1st trimester ● Visits every 4 weeks until 28 weeks then ● Visits every 2 weeks until 36 weeks ● At 36 weeks, visit every week until delivery ● Variation at discretion of provider ○ Pregnancy complications usually occur in 3rd trimester At every visit ● Apply the nursing process ○ Assess ○ Form nursing diagnosis ○ Establish goals 16 ○ Establish plan of care ● Watson’s carative factors Initial visit ● History obtained ○ Gravida, para, TPAL ○ Current pregnancy ○ OB/GYN ○ medical/surgical ○ Nutritional ○ drug/alcohol use (legal and illicit) ○ Family ○ Social and cultural ○ Abuse Initial examination ● Cardiovascular ● Respiratory ● Breast ● Abdomen ● Pelvic ○ Lithotomy position: can be done on side for abuse victims ○ Speculum exam ■ Pap smear, cultures, fern, nitrazine ● Lower extremity Vaginal leaking fluid ● Fern ○ Amniotic fluid ○ Swab on a slide ○ Increased sodium content, so no sodium crystals form ● Nitrazine ○ Strip to determine pH ○ Bright blue for amniotic fluid Initial laboratory tests ● Serum: CBC, blood type and Rh factor, antibody screening (indirect coomb’s test), hep B surface antigen, serology for syphilis (RPR or VDRL), rubella titer (MMR vaccine still working), HIV, sickle cell screening (hemoglobin electrophoresis), varicella titer (immunity from childhood) ● Urine: urinalysis for bladder infection and culture and sensitivity ● Other: purified protein derivative (PPD) tuberculin test Times sensitive tests and interventions ● 15 to 20 weeks: quad screen ○ Optional ○ Screen for down syndrome, spina bifida ○ Blood test ○ Can abort at this stage 17 ● 24 to 28 weeks ○ Screen for gestational diabetes and CBC ■ Check hemodilution ■ When HPL effects most ● 28 weeks ○ Antibody screen and RhoGam, if indicated ● 35 to 37 weeks ○ Group B beta strep recto-vaginal culture right before labor ■ Can be part of normal flora ■ Penicillin wipes out step through IV Q4h before in labor ● Repeat STD screening ● DV screening every trimester ○ Violence typically increases during pregnancy ○ Screening rules out problems but does not diagnose problems Health promotion ● Vaccinations in pregnancy ● Safe except for live virus vaccines ○ Rubella ○ Varicella At every follow up visit ● BP ● Weight ● Urinalysis: protein and glucose due to GFR ○ Shows nitrates, specific gravity (dehydrated), ketones ● Fetal heart tones ● Fundal height Fundal height measurement ● First trimester, the uterus is a pelvic organ ● Second and third trimester, uterus becomes an abdominal organ ● At 20 weeks, FH measurement beings with cm tape ○ 24 to 36 weeks fundal height is +/- 2 cm ○ After 20th week, fundal height grows 1 cm a week Warning signs and symptoms ● First trimester ○ Severe vomiting (greater than 24 hours) ○ Chills and fever (check temperature, fever is greater than 100.4 degrees) ○ Burning with urination ○ Diarrhea ○ Abdominal cramping with vaginal bleeding ● Second and third trimester ○ Persistent, severe vomiting ○ Sudden vaginal discharge less than 37 weeks ○ Vaginal bleeding ○ Abdominal pain 18 ○ ○ ○ ○ ○ ○ ○ ○ Chills and fever Dysuria Diarrhea Decreased fetal movement Contractions, pressure, or cramping less than 37 weeks Facial swelling ■ Colloid osmotic pressure will affect dependent edema Headaches Epigastric pain ■ Upper right quadrant pain→ preeclampsia (liver) ○ At 28 weeks, the baby should move and be felt every single day and if not, then come to the hospital Second and third trimester discussions ● Labor signs and symptoms ● Birth plan ● Analgesia and anesthesia ● Childbirth education ● Infant care ○ Feeding method ○ Tests ○ Circumcision ○ Pediatrician selection Postpartum ● 4 to 6 week exam ● Family planning ● Return to work ● Healing from c section ● Birth control ● How feeding is going ● Ab exercises ● Childcare Ongoing education and counsel ● Education by trimester ○ Common discomforts ○ Common concerns Assessment of Fetal Health Fetal assessment ● Ultrasound ● Chorionic villus sampling ○ Sample from placenta to detect defects ● Amniocentesis ● Multiple marker screen (quad screen) ● Fetal movement counts (mom counts) 19 ● Non stress test ○ Reactive or nonreactive ● Contraction stress test ● Biophysical profile (do in between NST and CST) Ultrasound ● Use of high frequency sound waves to visualize internal structures ● No documented risk to fetus ● Equipment: ultrasound machine and gel ● Screening (level 1) vs. targeted (level 2) ○ Sonographer ○ Routine for level 1 ○ High risk for level 2 ● First trimester ultrasound ○ Confirm pregnancy and viability ○ Determine location of pregnancy ○ Determine gestational age ○ Detect multiple gestation (twins) ○ View maternal anatomy and evaluate for abnormality (can get a cyst) ○ Guidance for CVS and PUBS ○ Ectopic: can implant in fallopian tube which is life threatening ○ Intra vs. extra uterine pregnancy ● Second trimester ultrasound ○ Evaluate fetal growth pattern ■ Compare and contrast ○ Detect fetal anomaly ■ 18 to 20 weeks to screen baby anatomy ○ Determine placental location ■ Did not attach near cervix ○ Measure amniotic fluid volume ■ Black indicates liquid and white indicates bone ○ Guidance for amniocentesis ● Third trimester ultrasound ○ Determine fetal position ■ Breech ○ Evaluate fetal and placental maturity ■ Perfusion and breathing ○ Evaluate fetal growth ■ Compare measurement and percentiles ○ Detect placenta previa or abruptio placentae ○ Guidance during external version and biophysical profile Chorionic villus sampling ● 10 to 14 weeks ● For genetic diagnosis ● 1:100 risk of loss 20 ● placenta→ fetal tissue not moms Amniocentesis ● Performed after the 14th week ● Sample of amniotic fluid ● Obtained from thin needle inserted through the abdominal and uterine wall ● 1:200 or 1:400 risk of loss ● Fetal skin cells in amniotic fluid and check surfactant Indications of amniocentesis ● Early pregnancy ○ Genetic diagnosis ○ Follow up for abnormal serum quad screen ● Middle pregnancy ○ Identify several of maternal-fetal (Rh) blood compatibility ● Late pregnancy ○ Determine fetal lung maturity Percutaneous umbilical blood sampling ● Fetal blood sampling ● Fetal transfusion ● CBC, H&H, blood transfusions Complications of invasive procedures ● Maternal or fetal hemorrhage: abruptio placentae ○ Detaches from wall ● Amniotic fluid leakage ○ Bag of waters ● Infection ○ Can cause miscarriage or preterm labor ● Spontaneous abortion or preterm labor ● Maternal organ damage ● Fetal injury ● Amniotic fluid embolism ○ Needle caused bubble of amniotic fluid to get in mom’s circulation (like a clot) ○ Smoke, pulmonary embolism ● Nursing care ○ Confirm true and informed consent ● Discharge instructions ○ Water leak (ruptured membranes) ○ Fever (infection) ○ Results from test (how to see/get) Quad screen ● Maternal serum test ○ Alpha- fetoprotein (AFP) ○ Unconjugated estriol ○ Human chorionic gonadotropin (HCG) ○ Inhibin A 21 ○ ○ Timing: 15 to 20 weeks Indication: screening for down syndrome and neural tube defects, anencephaly, spina bifida ○ Interpretation: not diagnostic ○ Follow up: cfDNA (cell free DNA), invasive testing ○ Good news, no bad news ○ Compares with all other general population of pregnant women Prenatal cell free DNA screening ● Fetal DNA in maternal blood (noninvasive) ○ Fetal Rh status ○ Fetal gender ○ Genetic disorders ● 10+ weeks gestation ○ Boy or girl ● Expense ● Insurance coverage ○ Maternal age ○ Positive quad screen ● Baby blood type ● Down syndrome ● Decreased accuracy ○ Multiples (twins) ○ Donor egg ○ Maternal obesity ○ Heparin, lovenox Fetal movement count ● Routine intervention for all patients ● Maternal assessment of fetal movement ● Third trimester: 28 weeks and beyond ● 10 kicks in 1 hour→ if not, go to the hospital Nonstress test ● Routine NSTs begin at 32 weeks ● Can be administered anytime in third trimester ● 20 minute evaluation of the fetal heart rate with an external electronic fetal monitor ● Indication: no movement felt ● Position of women: not flat, side or semi fowlers or sitting ● High risk: 2x week ● 1 belt: fetal heart rate ● 1 belt: uterine activity ● Interpretation ○ Acceleration: sudden increase in fetal heart rate ■ Peaking at least 15 beats above baseline ■ Lasting at least 15 seconds ■ Look for hills 22 ● Acceleration in fetal heart rate at least 15 x 15 is big enough to consider an acceleration ○ Results= reactive and nonreactive ● 2 possible outcomes ○ Reactive ■ 2 or more accelerations of 15 bpm above baseline ■ Accelerations last at least 15 seconds ■ Reassurance of fetal well being ○ Nonreactive ■ Less than 2 accelerations ■ Follow up: non-reassuring but not bad Biophysical profile ● Physical examination of 5 fetal parameters using an ultrasound ○ Indication: nonreactive NST (lose 2 points) ○ Closely correlated with apgar score ● Fetal assessment 1. FHR and reactivity (NST) 2. Fetal breathing movements 3. Gross fetal body movements 4. Fetal tone 5. Amniotic fluid index (AFI) BPP evaluation ● Normal (8-10) ● Equivocal (6) ● Abnormal (< 4) Contraction stress test ● Oxytocin ● Nipple stimulation (endogenous oxytocin) ● Absence of fetal distress indicates fetal wellbeing and tolerance of the stress of labor ● Should not see any deceleration History and Trends in Nursing of Women, Families, and Communities Scope of maternal-infant nursing, and the nursing of women and family health ● Community health nursing ● Involves primary prevention with mother and infant ● Health promotion and disease prevention ● Pregnancy (antepartum), labor (intrapartum), after birth and 6 weeks after (postpartum), newborn/infant ● Newborn stage is 0 to 28 days ● Infant stage is up to 12 months Definition of maternal-infant nursing and healthcare of women and family health ● All stages ○ Antepartum (pregnancy) ○ Intrapartum (labor) 23 ○ Postpartum (after delivery for 6 weeks) ■ Vaginal delivery: 6 weeks ■ C section: sooner Levels of practitioner in specialty area ● Staff nurses ○ L&D, clinics, physician offices ● Nurse practitioner ○ CNM (certified nurse midwife) ○ NNP (neonatal nurse practitioner) ○ CRNA (certified registered nurse anesthetist) Standards of care ● Definition: appropriate level of practice that a prudent nurse would provide in a particular situation or circumstance ● Assessment ● Diagnosis ● Outcome identification ● Planning ● Implementation ● Evaluation Increased specialization and certification ● Home health care/managed care ● Consumer involvement ● Emphasis on prevention ● Early prenatal care with high technology ○ Once they suspect they are pregnant or after positive test ○ Baseline assessment ○ Preeclampsia assessment ○ Consistently ○ Q4 Weeks until 28 weeks ○ Then Q2 Weeks until 36 weeks ○ Then Q1 Week until delivery ● High costs: technology and liability ● Access to healthcare/healthcare barriers ○ Transportation ○ Insurance ● Telemedicine Major healthcare issues ● Medical errors ○ DRTIMD ○ 2 nurses sign off for blood and certain medications ● Health disparities ● Health literacy Ethical or legal issues with impact the health of women and families ● Right of mother vs. rights of fetus 24 ○ Abortion ○ HIV+ and substance abuse ● Informed consent ○ Fetal surgery ○ Embryonic stem cell research ○ Treatment of very low birth weight ● Allocation of resources ○ Fetal tissue research ○ Fertility/reproductive assistance ○ Cord blood banking ○ Human genome project Define high-risk pregnancy ● Definition: life or health of mother and/or offspring is jeopardized or threatened ● Examples ○ Preeclampsia ○ Advanced maternal age ○ Obesity ○ Multiples ○ Teen pregnancy ■ Increased chance of low birth weight (5 lbs 8 oz.=2500g) ■ Increased chance of prematurity ■ Increased chance of trauma or birth injury (smaller pelvis) ■ Increased chance of stillbirth Mortality rate ● Maternal: number of maternal deaths from pregnancy 6 weeks after delivery (per 100,000) ○ Key factors: deaths from complications of pregnancy, childbirth, or puerperium ○ Increased age ○ Decreased prenatal care ○ Decreased education ○ Unmarried ○ Noncaucasian ○ Hypertension disorders (worldwide) ○ Infection (worldwide) ○ Hemorrhage (worldwide) ○ Gestational hypertension (USA) ○ Pulmonary embolism (USA) ○ Hemorrhage (USA) ● Infant: up to 12 months of age ○ Decreased prenatal care ○ Disparities between blacks and whites ○ Decreased education ○ Unmarried ○ Poverty 25 ○ ○ ○ ○ ○ Lack care Poor nutrition Smoking Alcohol use Maternal health conditions Nursing Assessment and Care of Family with Newborn Goal of care ● Assessment, protection, nurturance, and stimulation ● Nurse assess the newborn ● Positioned correctly and no loose objects ● Feeds regularly and adequately ● Talk and interact with infant ● Baby sees 8-10 inches ahead Transition to extrauterine life ● First 24 hours ○ Q 30 Mins x 4 assessment= 2 hours ○ Q1hour x 4 assessment= 4 hours ○ Frequent assessments for first 6 hours of babies life, then Qshift ○ Vitals, behavior, wake and sleep, activity Stimuli for newborn respirations via lungs ● Crying ● Sensory: bright light ● Biomechanical: CO2 build up, decreased O2 ● Thermal: cold room, wet body ● Mechanical: squeezing through birth canal Initial and priority care in the delivery room ● Establishing and maintaining respirations ● Preventing heat loss ○ Skin to skin or radiant warmer ● Physical assessment and evaluation ● Identification ○ 2 bands on newborn, 1 on mom, 1 on support person ● Initial and ongoing care and treatment Apgar score Sign Score 0 Score 1 Score 2 Respiratory effort Absent Weak cry Strong lusty cry Heart rate (apical) Absent Slow (<100) >100 Muscle tone Flaccid, limp Some flexion of extremities Full flexion of extremities Reflex irritability No response Grimace, weak Strong response, cry 26 Color Pale or cyanotic response or withdraw Acrocyanosis Completely pink ● Acrocyanosis is normal in the first 48 hours ● Normal: 8, 9, 10 ● Depression: 5, 6, 7 ● Resuscitation: 0, 1, 2, 3, 4 ● Do in 1st minute, repeat after 5 minutes ● If score is bad first time and decent the second time, do again in 10 minutes ● APGAR stands for appearance, pulse, grimace, activity, and respirations Maternal history ● Antepartal course ○ Meds ○ Complications ● Intrapartum ○ Fetal heart response ○ Health status Factors in hypothermia ● Large body surface relative to mass ● Limited subcutaneous tissue ● Vasomotor instability (cannot dilate or constrict) ● Limited metabolic capacity ● Thermal neutral environment ● Nonshivering thermogenesis ○ Heat production through lipolysis (metabolism) of brown fat ■ Metabolic acidosis and uses glucose Mechanisms of heat loss ● Conduction ○ Direct contact to cooler surface ○ Put on mom for body temp or warmer ● Radiation ○ Nearby solid object cooler than body (cold wall) ○ Put closer to moms body ● Convection ○ Air current/room temperature ○ Radiant warmer with sensor for heat output (37 degrees celsius) ■ Monitor on lower left side of newborn’s stomach ○ Diaper and cap under warmer (stay with baby) ■ Check temperature Q15 Minutes ○ 97.7-99 degrees fahrenheit is normal ○ Lower than 97.7→ check glucose Infant behavioral states ● Sleep 27 ○ Deep: barely moving, early hours of age, sleep 2-3 hours, mom can rest ○ Light: movement but does not open eyes ● Awake ○ Drowsy: eating, breast feeding, skin to skin, heavy eyelids ○ Quiet alert: ate well before nap, eyes open, look around, comfortable ○ Crying: hungry, tired, full diaper, uncomfortable, vocalizing, miss mom or dad, family responds to infant’s cry, bonding General appearance of newborn ● Observe at rest→ symmetry, face equality, neonatal infant pain score ● Weight ○ 2.2 lbs= 1 kg ○ 7 lbs and 8 oz= 3405 grams ○ Initial weight loss is less than or equal to 10% ○ Has to be less than 10% to go home ○ Initial weight minus discharge weight ○ In 7 to 10 days the baby should be back to birth weight ○ Baby is away from maternal hormones that cause fluid retention so they lose weight ○ Preemies may lose 15% of weight Length ○ 2.5cm= 1 inch ○ 18 to 22 inches= 45cm to 55cm (20 inches or 50 cm is average) ○ Weight and length taken in delivery room Head and chest circumference ○ Head: 12.5 to 14.5 inches (32 to 37cm) ○ Chest: 12.5 inches (32cm) ○ Head should be 2cm larger than chest Vital signs ○ Temperature (axillary): 97.7 to 99 degrees ■ If increased, remove clothing or could be from breastfeeding ○ Respiratory rate: 30 to 60 breaths per minute ● ● ● ■ Obligatory nose breather→ nose occluded→ get help if blue→ stimulate baby to make cry because crying is breathing ■ ■ ■ ■ ○ Abdominal breathers (rise and fall of abdomen) Count for a full minute Irregular breathing with brief periods of apnea then fast (cheyne-stokes) Signs of respiratory distress ● Nasal flaring ● Sternal retractions ● Thoracic wall goes up and abdominal wall goes down (seesaw breathing) ● Grunting Heart rate: 110-160 beats per minute (fetus and newborn) 28 ○ ● ● ● Blood pressure: indicated if heart murmur is heard (3rd and 4th intercostal space for point of maximum impulse) ■ Take on upper and lower extremities Gestational age assessment (ballard) ○ Done once ○ Physical assessment then ballard ○ High risk based on size and age ○ Can be SGA (small), LGA (large), or AGA (average) SGA ○ Hypothermia ○ Don't eat as much ○ Hypoglycemia LGA ○ If postterm, placenta gets too old and can cause problems ■ Respiratory ■ Elimination ■ Nutrition ● ● Can become hypoxic→ meconium in amniotic fluid Color of skin ○ Acrocyanosis ■ No longer than 48 hours ■ Minus 1 in APGAR score ■ Hands and feet are blue ○ Pale/cyanotic ■ Respiratory or cardiac concerns ■ Stimulate crying ○ Cutis marmorata (mottling) ■ ○ Immature blood vessels→ cool temperatures ■ Lace like appearance ■ Go away in 1 week Jaundice ■ Yellow looks the same for physiological and pathological Physiological - After 24 hours Normal change 2 to 3 days of age Immature liver Breakdown of fetal RBC - Release bilirubin Gone within 7 days Pathological - Before 24 hours of age Begins in utero Origin often found in blood compatibility - Baby could die without prenatal care - Give rhogam for temporary immunity if there are no antibodies formed Example for Rh: mom is Rh negative, baby is 29 Rh positive→ mom exposed to Rh positive blood and makes antibodies which go into fetal circulation and destroy RBC (permanent)--> coombs test Example for type: mom is O, so there are no antigens, but there are A and B antibodies, so there would be an issue if the baby was A or B blood→ destroys RBC Direct bilirubin (normal) Indirect bilirubin (physiological and pathological jaundice) - Conjugated Metabolized Water soluble Able to be excreted through normal - routes→ urine and stool Level: < 1mg ● - Unconjugated Not metabolized Unbound to protein Fat soluble Unable to be excreted via normal routes Has an affinity to brain cells and tissue Level: 12 mg/dL - Very ill baby, brain damage Characteristics of skin ○ Turgor ■ Test in the abdomen (central) ■ Assesses hydration status ● ○ ○ ○ ○ Fontanelles can also be used→ sunken and depressed Desquamation ■ Peeling skin in newborn ■ Post mature exposed to amniotic fluid without enough vernix caseosa (protects skin) Vernix ■ Increased amount with prematurity ■ Cream like substance around 28 weeks, mostly gone by 38 weeks ● Can still be seen in creases and folds Lanugo ■ Increased amount with prematurity ■ Cannot be wiped away ■ Full term will only be on upper back and shoulders Milia ■ Looks like whiteheads ■ Clogged sebaceous glands 30 ■ ● Go away within a week ● Cleanse face 2-3 times a day with plain water ○ Erythema toxicum ■ Newborn baby rash ■ Red area with white in center ■ Benign skin variation ■ Goes away within a week ○ Petechiae ■ Pinpoint red dots ■ From pressure during labor ■ Go away within a week Birthmarks ○ Telangiectatic nevi (stork bites) ■ Gone by 2 years old ■ ○ ■ Found on neck, eyelids, and bridge of nose ■ Common Nevus flammeus (port-wine stain) ■ Nonelevated sharply outlined red-purple plexus of new capillaries ■ ○ ● Over the face→ can have removed within first year of age→ laser surgery Hemangiomas (strawberry marks) ■ Raised, rough, protrudes ■ Occupies dermal and subdermal ■ ○ Pale pink to red dilated capillary→ blanch Hypertrophy→ increase in size over years ■ School age years it will layer off and be gone Mongolian spots ■ Bruise looking (green and purple) ■ Infants of color ■ Point out to parents ■ Can last 4 to 6 years of age Head ○ Molding (cone head) ■ Head fitting through pelvis ■ Overlap parietal bones ■ Accomodation to fit through birth canal ■ By the next day, head is normal shaped ○ Cephalohematoma ■ Collection of blood over 1 of the parietal bones and periosteum ■ Several hours after birth (takes a while for blood to leak out) ● Head delivered quickly and vessel breaks ● Tool used to pull out baby ■ Does not cross suture line ■ No intervention needed but takes weeks to go away 31 ○ ○ ● Face ○ ■ Bloody has to absorb into bone and increase in diameter Caput succedaneum ■ Skull cap ■ Present at birth ■ Stuck in birth canal ■ Resolves without intervention in 1 to 2 days Fontanelles ■ Flat and soft ■ Anterior (18 months) ● Assess hydration ■ Bulging→ CSF fluid ■ Posterior (triangle) ● Half size of anterior ● Lasts for 2 months Eyes ■ ■ ■ ■ ○ Ears ■ ■ ○ Psuedostrabismus ● Not synced in movement ● Lagging ● In utero, nothing to focus on so eye muscles are weak Subconjunctival hemorrhage ● Scleral hemorrhage ● No intervention required ● Bleed in white of eye ● Blood vessel injured and bursts Ophthalmia neonatorum ● Eye infection ● Inflamed conjunctival sac from chlamydia or gonorrhea ● Erythromycin ointment (not the best prophylaxis) ○ Can lead to blindness Reflexes ● Blink ● Pupillary Height ● Even from inner to outer canvas to ears ● Can indicate genetic disorders if not even Shape/appearance ● Pinna differences ● Unique fold ● Document and report to pediatrician ● Renal system and ear develop simultaneously so could have renal issue as well Mouth 32 ■ ○ ○ ○ Epstein’s pearls ● White inclusion cysts ● Go away in weeks ● Not teeth but on palate of gums ■ Precocious teeth (2 bottom teeth) ● If loose, baby is at risk for aspiration so they are extracted ● Baby only has suck reflex, not biting, so this does not affect breastfeeding ■ Tongue-tied ● Short frenulum ● Short string under tongue ● Can effect pronunciation and breast feeding ■ Thrush ● White in mouth ● Does not wipe away ● Candida contracted from birth canal ● Untreated yeast infection ● Use medications to treat ● Wash nipples well between feedings Chest and abdomen ■ Symmetry and size (2cm less than head) ■ Breast enlargement/hypertrophy ● Witch’s milk ■ PMI 3rd to 4th intercostal space ■ Protruding abdomen ■ Nondistended ■ Bowel sounds in all 4 quadrants ■ Abdominal breathing ■ Synchronous rise and fall of chest and abdomen Genitalia ■ Male (scrotal sac, testicular descent, hydrocele, hypospadias or epispadias) ● Full term: prinulous, hanging, elongated sac, testes are on bottom of scrotal sac, deep rugae ● Pre term: shortened testes partially descended (one is higher than the other), lighter rugae ■ Female (labia and pseudomenstruation) ● Full term: labia majora covers clitoris and labia minora, lining of the uterus can shed because baby is used to mom’s hormones ○ Void pink mucous: uric acid crystal ● Pre term: both labias and clitoris showing Extremities ■ Polydactyly/syndactyly ● True extra digit= bone present 33 ■ ■ ● Tie to cut off circulation then falls off= no bone present Hip dysplasia ● Ortolani’s sign: flex and abduct the hip joint (ball and socket) ● Knee height and skin creases over the posterior aspect of legs ○ Supine with feet flat on the surface, then prone to look at creases for symmetry Talipes deformity (clubfoot) ● Feet inverted ● Not a lot of space in the womb for feet to develop ● ○ ○ ○ ○ ○ xray→ if significant ROM loss→ braces Back ■ Pilonidal (dimple/hair tufts) ■ Cervical spine down ■ Indentations ■ Indicative of incomplete closure of cerebral spinal column Infant bathing (delayed vs. early) ■ 12 to 24 hours ■ Decreases risk of infection ■ Stabilize glucose ■ Temperature control ■ Maternal fetal bonding ■ Increased breast feeding ■ Lubricates skin Cord care ■ Cleanse thoroughly at initial bath ■ Ensure cord is cut short enough to dry and fall off by 7 to 10 days ■ Keep exposed to air ■ Do not cover with diaper Circumcision care ■ Ensure to active bleeding after circumcision ■ Apply petroleum jelly to head of penis to decrease irritation from diaper Infant reflexes ■ Moro: startles them ■ Palmar grasp: grab finger ■ Tonic neck: fence player stance ■ Plantar: point toes down ■ Rooting: illicit when trying to get them to breastfeed, swipe cheek to turn and open mouth ■ Sucking or swallowing: important for feedings ■ Stepping: one foot touches ground, other picks up 34 Nursing Management of the Family in Childbirth (Intrapartum Period) The four P’s of labor – pg. 100 ● Passageway ○ Includes bony pelvis ■ Size large enough for fetus ○ Cervical dilation ■ Soft tissue ○ Vaginal canal ○ Muscles of perineal floor ● Passenger ○ Size of fetus ○ Angle ○ Body part coming first ● Powers ○ Uterine contractions ○ Forces that cause fetus to move down to cervix ○ Helps dilate to 10cm ○ Mom pushing ● Psyche ○ Maternal disposition ○ Excited, experienced, new mom, unprepared, scared ○ Anxious, difficult to communicate ○ Medicate to help ● Position of mother ○ Semifowlers ■ More frequent contractions but less intense ○ Side lying ■ More intense contractions but less frequent ○ Change positions every 1 hour to get baby to rotate if face is facing up Terms used to describe labor ● Definition: signs or signals that indicate labor is coming soon ● Preterm labor – 21 weeks (beginning) and 36 +6 (ending) ● Dystocia – abnormal labor (contraction) pattern Premonitory (Preliminary) signs of labor – pg. 102 ● Lightening ○ Baby dropping ○ Breathing easier ○ Bladder is compressed ○ Baby getting into position ○ Few weeks before labor ● Braxton-Hicks ○ Week before true labor ○ Can change cervix 35 ○ Do not typically hurt ○ Last for a while ○ Could help dilate ● Discharge of mucus plug ○ Barrier to bacterial invasion ○ Braxton-Hicks could dislodge the plug ○ Clear or white mucus ○ Cervical change ● Energy spurt ○ Nesting behaviors ○ Last couple weeks or days ○ Wave of energy ○ Accomplish tasks before birth ○ Get up and moving to help prepare the body for labor ● Rupture of membranes ○ All fluid does not leak ○ Leaks slow over time ○ Assess fetal heart tones ○ If decreased heart tones, could indicate prolapsed cord ■ Emergency situation ■ Cord comes out first ○ Know color ■ Clear, bloody, or meconium stained can be present ■ Should not have odor ○ Patient can walk until they rupture membranes ● Weight loss ○ Fluid weight loss ○ Decreased progesterone at term so water does not retain anymore True vs. false labor False labor True labor Frequency (Ex: every 12 mins) Remains constant Intervals Increase in frequency (Ex: 10 min, 6 min, 4 min, 2 min) Level of intensity stays the same Intensity More intense with each contraction Lower abdomen Location Lower back and radiates to lower abdomen Walk fast Smiling Contractions go away with walking Effect of activity Walking intensifies contractions Have to stop walking when contraction comes 36 No bloody show Bloody show There is a bloody show Mucous that is blood tinged (pink) is a normal finding Change for a little and then stop Cervical changes Continuous cervical change Keeps dilating and thinning out Stages of labor – pg. 103 ● Stage one ○ Dilation stage ○ 0cm- 10cm ■ Multiparas: 6 to 8 hours ■ Primiparas: 12 to 14 hours ○ Phase one ■ Latent ● 0cm- 3cm dilated ■ Active ● 4cm- 10cm dilated ○ Transition period ■ 8cm- 10cm dilated ○ Nurse has to be aware of the progression of labor and responsive to change ● Stage two ○ Birth of baby ■ Multiparas: 30 minutes to 1 hour ■ Primiparas: 1 to 2 hours ■ Grand: 5 or more births before ● Very fast delivery ● Patient could deliver from sneezing or coughing ○ No more cervix around head ● Stage three ○ Delivery of placenta ○ Same for vaginal births and c sections ○ Should take 3 to 6 minutes ■ Maximum of 30 minutes then scrape out in OR ● Stage four ○ Recovery ○ 1 to 4 hours ■ Make sure they recover from anesthesia and have sensory and motor skills back ○ Same for all vaginal births ■ 2 hour recovery ○ Same for all c section births ■ 3 hour recovery 37 ● ● ● 1st hour assessments ○ Q15 minutes 2nd hour assessments ○ Q30 minutes Assessment includes ○ Pulse ○ Respirations ○ Blood pressure ○ Oxygen saturation ○ Temperature once in 4 hours unless abnormal ○ Fundus: consistency and location ■ Top should be at umbilicus ■ Palpate firm ■ Midline or off to side due to bladder distention ● Bladder pushes uterus because there is usually 300 to 500 mL or urine in bladder, so the patient is straight cathed ■ Ensure no bleeding is occuring ○ Vaginal bleeding ■ Lochia: scant, rubra, light (normal) ● Abnormal to have foul smells or clots ○ Recovery for anesthesia Stage 1 of Labor – pg. 104 + notebook page Criteria Phase 1 (Latent) more effacement and little fetal descent Phase 2 (Active) increased cervical dilation and increased fetal descent Dilation 0cm to 3cm 4cm up to 10cm Contraction Pattern 1. Frequency (beginning of one contraction to the beginning of another one) 2. Duration (beginning to end of contraction) 3. Intensity (assess at the peak) 1. 5 to 10 minutes 2. 30 seconds 3. Mild 1. Every 2 to 3 minutes 2. 45 to 60 seconds 3. Moderate Maternal Behaviors - - - Frequency or level of discomfort Excited Talkative Good time to give information Able to respond Serious Focused In pain Quieter 38 Breathing Pattern - - Deep chest breathing (inhale in nose and blow out through mouth) Abdominal massage could help - Nursing Management - ● ● ● Assess and document every 30 to 60 minutes Comfort Positioning - Shallow chest breathing “Hehe”s Rapid breathing Deep breath and fall back into pillows Hyperventilation can cause respiratory alkalosis Use paper bag if hyperventilating Assess and document every 30 minutes for mother and every 15 to 30 minutes for fetal heart rate Transition stage ○ 8cm to 10cm (complete dilation) ■ Anterior lip and rim ○ Only if there is no epidural ○ Contractions ■ Frequency: 1.5 to 2 minutes ■ Duration: 60 to 90 minutes ■ Intensity: strong ○ Maternal behaviors ■ Strong urge to push ● Can cause laceration or pinch and swelling ■ Blow off urge ○ Nursing management ■ Assess and document every 15 to 30 minutes for mother and fetus Pitocin ○ Always piggyback ○ Can use normal saline as fluids if pitocin needs to be stopped Cervical and fetal changes – pg. 105 ○ Effacement: thinning of cervix ○ Fetal station ■ Breech or regular ● 36 week cervical check ● If breach, c section or try to turn the baby (version) ■ Landmark: mid portion of pelvis or ischial spine ○ Fetal position ■ Left occiput anterior: favorable ■ Right occiput anterior: favorable 39 ■ ■ Occiput anterior: favorable Left or right occiput posterior: not favorable ● Maternal pelvis – pg. 108 ○ 3 planes ■ Inlet ● Separates true and false pelvis ■ Midplane ■ Outlet ○ 0 station: engagement ■ Successfully went through 2 of 3 planes ■ At ischial spine Assessing the passenger (fetus) ● Landmarks on fetal head ○ Sagittal suture (right down middle) ○ Frontal bone (front of head) ○ Parietal bones (either side of head) ○ Occipital bone (back of head) ● Adaptations of fetal head ○ Molding (elongated head, overriding bones) ○ Cephalohematoma (blood vessel bursts) ○ Caput succedaneum (edema resolved in a few days) ● ● Leopold’s maneuvers – pg. 111 ○ Fetal lie: aligning with maternal spine (should be parallel) ○ Fetal presentation: 36 weeks, which side is coming out ○ Fetal descent: check externally, false pelvis or true pelvis ○ Locate fetal back: closest to head is best, FHR Maneuver’s ○ First ■ Assess fundus (palpates) ■ Soft and angular ● Buttocks, trunk moves with it ○ Second ■ Assess fetal back ■ Stabilize one side, palpate the other ■ Firm and smooth ● Back ■ Nodules ● Fists, knees, elbows ○ Third ■ Assess lower uterus ■ Hard and rounded ● Head, moves independently of trunk 40 ○ Fourth ■ ■ ■ ■ ■ Assess fetal descent Alongside uterus towards mother’s feet Bring hands together over presenting part Out over symphysis pubis, hands out over ● True pelvis Hands come together ● False pelvis ● Fetal station ○ Risk for prolapsed cord (-2 or false pelvis) ○ Check FHR after membranes rupture ■ Do not let labor go more than 24 hours after rupture of membranes ■ Know color, odor, amount, and time assessment ○ Unexplained jaundice Fetomaternal relationships ● Attitude ○ Relationship of fetal body parts to themselves ■ Flexion or extension ● Lie ○ Long axis (spine) to long axis of mother ■ Longitudinal (normal) vs. transverse (not normal) ● Presentation ○ Vertex (normal), breech, shoulder ○ Attitude effects presentation ● Position ○ OA: normal and favorable ○ OP: change positions every 1 hour, back labor, side lying ● Station ○ 0: engaged ○ +3: crowning ○ +5: delivering head ● Properties of Uterine Contractions – pg. 114 ○ Phases: ■ Increment ■ Acme ■ Decrement ○ ○ ○ Frequency Duration Intensity ○ Friedman’s curve 41 ● ● Maternal and Fetal Changes during Childbirth – pg. 115 ○ Cardiovascular System ○ Gastrointestinal System ○ Urinary System ○ Fluid and electrolytes ○ Hematopoietic System ○ Respiratory System Fetal response during labor 42 Fetal oxygenation factors – pg. 118 ● Normal maternal blood flow ○ Affected by hypertension ● Normal oxygen saturation in maternal blood ○ Affected by anemia ● Adequate exchange of oxygen and carbon dioxide in placenta ● An open circulatory path between the placenta and fetus through vessels in the umbilical cord ○ No cord compression ● Normal fetal circulatory and oxygen-carrying function Conditions associated with fetal compromise ● FHR outside range of 110 to 160 ● Slowing over FHR after contraction ended ○ Late onset and late recovery puts baby in jeopardy ● Contraction lasting longer than 90 seconds ● Incomplete relaxation between contractions ○ Relaxation replenishing nutrients ● Maternal hypotension or hypertension ○ Take blood pressure often ● Meconium- stained amniotic fluid ○ Signals baby had hypoxic episode ● Foul odor to amniotic fluid Fetal assessment in labor ● Two aspects of FHR during labor ○ FHR baseline ■ Without the influence of contractions ■ Can be normal or abnormal ○ Periodic FHR ■ Fetal heart rate in response to uterine contractions ■ Early decels are not problematic ■ Late and variable decels are problematic Three tiered interpretation system ● Category 1: normal fetal heart response ○ Want to see ● Category 2: indeterminate ○ Don't need to know ● Category 3: abnormal fetal heart response ○ Deliver baby ASAP Category 1 ● Normal fetal heart response ● Baseline rate: 110 to 160 ● Baseline variability is moderate ○ Sympathetic: raises HR ○ Parasympathetic: slows HR 43 ● No late or variable decels ● Early decels are okay ● Accelerations are possible and good signs Category 3 ● Abnormal fetal heart response ● Absent baseline variability and any of the following ○ Recurrent late decels ○ Recurrent variable decels ○ Bradycardia (less than 110 and headed to 0) ● Sinusoidal ○ Fetal jeopardy ○ Severe anemia or cardiac defect ● CNS is deprived or sedated Fetal monitoring – pg. 120 ● FHR baseline ○ Fetal heart rate is average rate in 10 minute segment, excluding periodic or episodic changes, such as early or late decelerations or in the absence of uterine contractions ■ Baseline variability ● Parasympathetic and sympathetic nervous system ■ Baseline heart rate ● Baseline variability ○ Definition: fluctuations in fetal heart rate over a few seconds and over several seconds ■ Reflects the interplay of sympathetic and parasympathetic nervous systems on fetal heart rate ○ Moderate variability ■ Want to see ■ Shows adequate oxygenation ○ Factors for diminished variability ■ Fetal sleep ● HR doesn’t change so less variability ● Can use vibroacoustic stimulator to wake baby up ■ Maternal drugs ● Analgesics in IV which can go to fetus ● Can cause respiratory depression ● Make sure drug done by the time of delivery so lungs can be used ■ Fetal hypoxia and acidosis ○ Minimal variability ■ Fetal sleep ■ Morphine ■ Any analgesics ○ Absent variability 44 ■ Flat line ■ So oxygen deprived→ deliver baby immediately ■ Severe fetal hypoxia Fetal heart rate baseline rate changes – pg. 124 ● Tachycardia: fetal heart rate baseline exceeds 160 bpm for more than 10 minutes ○ Causes: infection of mother or baby, fetal anemia ○ Treatment: do not treat until baby comes out ○ Gradually increases ○ Permanent relocates high ○ Mom’s body temp increases so her heart rate and fetus heart rate increases ○ Mom group B positive→ fetus tachy due to exposure ● Bradycardia: fetal heart rate baseline below 110 for 10 minutes or more ○ Causes: prolonged cord compression or maternal hypotension ○ Treatment: intrauterine resuscitation, maternal reposition (switch sides), expedite delivery if no change from positioning, give mom oxygen via face mask (8-10 liters) ○ Headed to 0 bpm ○ Immediate intervention ○ Do not wait 10 minutes if FHR is dropping ○ Increase volume that gets to fetus (IV fluids) and quality Periodic or episodic fetal heart rate response ● Periodic definition: FHR response with uterine contractions (3 of them) ○ Fetal head compression ○ Not problematic ○ Begins and ends with uterine contractions ○ Mirror image of uterine contractions ○ Nadir: decreased point of FHR ○ Apne: increased point of contraction ○ Early decels ■ Benign pattern ■ No intervention required ○ Late decels ■ Uteroplacental insufficiency ■ Late onset of decel pattern ■ Causes: preeclampsia, hypertension, and smoking ■ After beginning of contraction and lasts until after end of contraction ■ Decreased perfusion to placenta to begin with and takes a while to recover ■ Atypical (nonreassuring) ■ Treatment ● Intrauterine resuscitation ● Turn off pitocin, increase maintenance IV fluid rate 45 ● ● Oxygen 10 liters via face mask Lateral recumbent position ○ ● Either side→ avoid compression of IVC ● Check baseline variability ● Notify practitioner ● Increase vascular volume and oxygenate blood ○ Variable decels ■ Umbilical cord compression ■ Irregular and abrupt ■ Varies in shape and where it onsets in relation to contraction ■ Atypical (nonreassuring) ■ Treatment ● Intrauterine resuscitation ● Turn off pitocin, increase maintenance IV fluid rate ● Oxygen 10 liters via face mask ● Turn to opposite side first and if no improvement, knees to chest ○ Baby goes back towards fundus ○ Leave for a little while and ease to side lying ● Evaluate baseline variability ● Notify practitioner Episodic definition: FHR without contractions, accelerations 46 Analgesia and Anesthesia of Childbirth – pg. 130 Sources of pain ● Stage 1: cervical dilation and cervical stretching ● Stage 2: stretching and distention of perineal tissues and floor ● Stage 3: same as stage one Non Pharmacological options for pain management ● Cutaneous stimulation methods ○ Walking ○ Rocking ○ Acupuncture ○ Hydrotherapy ○ Effleurage or counterpressure ○ Backrub ○ Massage ● Sensory stimulation techniques ○ Aromatherapy ○ Music ○ Using focal points ○ Imagery ● Cognitive strategies ○ Childbirth education ○ Hypnosis Pharmacological options for pain management ● Narcotic (opioid agonist) analgesics ○ Know cervical exam: do not give if less than 2 hours of labor left ○ IV ○ Used most often: sublimaze, ultiva, demerol ○ Sometimes used: sufenta, dilaudid, morphine ○ Baseline variability will decrease with analgesics from moderate to minimum ○ Administer narcan (naloxone) if overdose ■ Administered to newborn to counter if baby is delivered less than 2 hours from the last dose ○ Block neurological understanding of pain ● Narcotic agonist/ antagonist ○ Used most often: nubain ■ Will give if no epidural ■ Works for about 1.5 hours ○ Sometimes used: stadol ○ Less respiratory depression risk ○ If given to heroin or fentanyl abuser, immediate withdraw will happen ● Ataractics co- drugs ○ Given with analgesics to enhance ○ Benzodiazepines ■ Major adverse effect: maternal amnesia 47 ● ● ● ■ Examples: valium and ativan ○ Phenothiazines ■ Examples: phenergan, reglan, vistaril, zofran Sedatives ○ Hypnotics ■ Examples: nembutal, seconal ● Used with 2 day inductions Regional anesthesia ○ Lumbar epidural ■ Antacid beforehand ■ Epidural space ■ IV bolus before to increase volume since blood vessels dilate ■ Blocks pathway for pain ■ Xiphoid process to toes are numb ■ Stage 1 to 4 (repair lacerations) ■ Fetus not effected as long as mom does not get hypotensive ■ Can give before 4cm dilated ■ Can feel pressure not pain ■ C section easier ■ Maternal hypotension risk ● Monitor every 2 minutes ○ Spinal block ■ L3, L4, L5 ■ Sooner than epidural ■ For 2nd stage ■ C section ■ Difficult vaginal birth ■ Increased caffeine= increased CSF production ■ Adverse effects ● Maternal hypotension ● Spinal headache (like migraine) ○ Pudendal block ■ By provider (midwife or OB) ■ Injection into pudendal nerves ■ 2nd stage of labor ■ No effect on fetus ○ Local ■ Stage 2, 3, and 4 ■ Inject in direct area wanting numb (like dentist) ■ Laceration ■ No effect on fetus Nitrous oxide ○ Laughing gas ○ Short half life 48 ● ● ● ○ Minimal effect on baby General anesthesia ○ Risks for mom ■ Aspiration ■ Respiratory depression ■ Asphyxiation ■ Uterine relaxation ○ Risks for fetus ■ Respiratory depression ■ Get out before reaching fetus Postpartum morphine (Duramorph) ○ Intrathecal ○ Indication/use ■ Pain ○ Itching can be side effect ○ Monitor oxygen, pulse, and respiratory rate Nursing management of the cesarean birth and selected intrapartal procedures – pg. 136 ○ Indications for cesarean birth? Common reasons for c-section? ○ Distinguish b/w variations in incision types on skin and uterus for cesarean delivery. Type of incidion needed for VBAC? ○ Type of anesthesia for cesarean birth? ○ NM indicated preop/postop for cesarean? ○ NB affected delivered by c-section over vaginal? ○ Difference b/w 1st, 2nd, 3rd, and 4th degree laceration to the perineum? ○ Forceps or vaccum extraction, how’s mother affected? Baby? 49 Nursing Care of the Postpartum Mother – pg. 137 Postpartum ● Puerperium ● Fourth trimester of pregnancy ● Approximately 6 weeks after birth Maternal psychosocial adjustment ● Attachment: the process by which a parent comes to love and accept a child and a child comes to love and accept a patient ● Mutuality: infant elicits a corresponding response from the parent ○ Mom sticks out tongue→ baby sticks out tongue ● ● ● Acquaintance: eye contact, touching, talking Claiming process identification of newborn: likeness, differences, uniqueness Promotion ○ Early skin to skin contact ○ Modeling ○ Rooming in: baby needs to be around mom to learn hunger cues, initiate breastfeeding, resolves intervention around these adjustment Maternal adjustment ● Taking in ○ Taking time for one's own needs ○ Taking care of self before taking care of baby ● Taking hold ○ Focused and obsessed with baby ○ Forgets about self ● Letting go ○ Take baby to nursery or babysitter Normal Postpartum Physiologic Changes – pg. 143 Endocrine changes ● Expulsion of placenta ○ Estrogen and progesterone drop markedly ○ Estrogen drop causes postpartum diuresis of extracellular fluid accumulated ■ Urine output increases for first 2 to 3 days (3000 mL/ day) ■ Increased perspiration ○ HPL drop reverses the diabetogenic effects of pregnancy ■ Gestational diabetes goes away ● Thyroid function returns to normal in 3 months ● Prolactin ○ Breastfeeding hormone ○ Influenced by frequency and duration of feedings, amount of formula supplemented ○ Suppresses ovulation and menses→ 1st period around 6 month ○ Mean time to ovulation in breastfeeding women is 6 months 50 ○ Void every 1 to 2 hours even if do not feel like it Uterus ● Involution process ○ Back to pre pregnancy uterus ● Oxytocin induces contractions ○ Compresses vessels and promotes hemostasis at placental site ○ Fundus decreases 1cm a day ○ Afterpains ■ More common in multiparous or overdistention of uterus ■ Interventions: massage, position, NSAIDs, and hot packs ● Assessment ○ Position and preparation for accuracy ■ Supine and void prior ○ Height in regard to umbilicus ○ Consistency ■ Firm or boggy (bleeding) ■ Look at lochia for boggy ○ Location ■ Midline ■ Deviated could be from a full bladder Vagina/Perineum ● Assessment ○ Positioning, REEDA ■ R: redness ■ E: edema ■ E: ecchymosis ■ D: drainage ■ A: approximated ● Pericare ○ Peri Bottle (squirt bottle) ■ Front to back with warm tap water everytime in the bathroom ○ Cold packs ■ Any point in time ○ Warm sitz bath ■ 18-24 hours after ■ 20 mins 3x/day ■ Good for 3rd and 4th degree lacerations ○ Medications ■ Epifoam (3x/day) ● Lochia ○ Rubra: first 3 to 4 days ○ Serosa: day 3 to 10 post partum ○ Alba: 10 days to 6 weeks ○ Amount 51 ■ ■ ■ Heavy= hemorrhage ● Saturating pad in less than 1 hour ● Subjective Scant, light, and moderate is normal Heavy is abnormal Urinary ● Pelvis muscle support ○ Stress incontinence ○ Can be strengthened ○ Physical therapy ○ Kegel exercises ■ Squeeze muscles that stop the flow of urine ■ Hold for 3 secs, then relax for 3 secs ■ Do 10 contractions, 3 times a day ■ Increase hold by 1 second a week ■ Work up to 10 second holds ● Urethra and bladder ○ Lacerations, anesthesia can result in decreased urge to void ○ May sting and burn for first void ○ Use KY jelly on urethra to help → usually healed by 24 hours Abdomen and GI system ● Decreased peristalsis and decreased muscle tone in the intestines during labor, NPO, dehydration ○ Hypoactive bowel sounds ● Constipation ○ Stool softeners, can set off uterus, bad uterine cramping, mild laxatives, may reduce after pains ● BM may not occur for 2 to 3 days after birth ● Diastasis recti ○ Obvious in fundal assessment ○ Do not lift anything heavier than newborn baby ○ Slender, multiparous women are easier to feel Breasts ● First 24 hours ○ Colostrum: clear yellow looking ■ Blue tinged sometimes ■ Baby needs for immunity ● 24 to 72 hours ○ Colostrum gradually transitions to mature milk ○ “Milk coming in” ○ Breasts become fuller and heavier ○ Tingling sensation ● Breastfeeding mothers ○ Establish adequate supply 52 ○ Frequent on demand feedings ○ Skin to skin (kangaroo care) ○ Avoid supplemental formula if baby is healthy ○ Wear strong bra ● Non breastfeeding mothers ○ Assessment ○ Teaching ■ Binding ATC for 72 hours, no nipple stimulation Respiratory and cardiovascular system ● Blood volume ○ 300 to 500 mL blood loss for vaginal ○ 500 to 1000 mL blood loss for cesarean ■ Get EBL during report ○ Occasional orthostatic hypotension ■ ● Labs ○ ○ ○ 1st and 2nd time getting up → someone go with them H/H drops moderately for 3 to 4 days after birth Clotting factors and fibrinogen elevated in immediate postpartum period WBCs can increase to 20,000-25,000 in the first week after birth because of the stress of labor→ immune system on overdrive ● Varicosities of legs and hemorrhoids regress quickly ○ Heal very quickly Postpartum vital signs – pg. 145 ● Temperature: > 100.4 degrees, assess for pain and collaborate ● Pulse: > 90 requires further investigation related to postpartum hemorrhage ○ Assess lochia and fundus ○ Bradycardia 50 to 70 is a normal adaptation in the first week postpartum ● Respiratory depression can occur after epidural or spinal anesthesia ○ Especially if duramorph is used ● Tachypnea requires further investigation for pulmonary embolism ○ Get pulse oximetry reading ● BP > 140/90 requires further investigation related to postpartum preeclampsia ○ Neuro check ● BP < 90/60 requires further investigation related to postpartum hemorrhage ○ Assess for orthostatic hypotension and fundus and lochia ● MAP < 70 indicates limited perfusion related to postpartum hemorrhage ○ Assess fundus and lochia Health promotion ● Rhogam ● MMR vaccination ● Varicella vaccination 53 Postpartum Care Following Cesarean Birth Pain management ● Spinal/epidural (duramorph) ○ Chemically modified morphine to last 18 hours given intrathecal route ○ Nursing priorities: monitor respiratory rate and pulse oximetry ● General anesthesia ● IV and PO opioids or NSAIDS ● Splinting of incision with assessment of fundus and ambulating ○ Gloved hand or pillow splints incision for low transverse while palpating to reduce pain ● Assess fundus after pain meds ○ During peak of pain medication ● Ambulation ○ Early in stable postoperative patients ○ GI system starts moving ○ Promote bonding between mother and baby ● Reduce intestinal gas ○ Simethicone ○ No straws until passing flatus ■ Significantly lower pain ratings because less air that is sucked in ● Venous thromboembolism prevention ○ SCDs until ambulation on own ○ Lovenox to decrease risk for clots Incision ● First 24 hours, assess dressing for shadowing ○ Significant drainage causes shadowing (outline it, initial, date, time, document) ● Dressing is usually removed at 24 hours ○ No orthostatic hypotension then patient can get up ● REEDA assessment ○ R: redness ○ E: edema ○ E: ecchymosis ○ D: drainage ○ A: approximation ● Staples provide best approximation and strongest hold, glue, subcuticular (internal) stitches, steri strips perpendicularly ○ Risk for dehiscence (diabetics, morbidely obese) will typically have staples Grief ● Feel like a failure after c section ● Anticipated vaginal and less pain and faster recovery→ did not go as planned Promotion of bonding ● C section can cause lack of bonding 54 Abnormal Postpartum – pg.147 Postpartum depression ● Baby blues ○ Moodiness that resolves in first 2 weeks postpartum ○ No impairment in functioning ● Depression ○ Intense sadness ○ Severe mood swings ○ Feelings of guilt or inadequacy ○ Sleep disturbances ○ Difficulty bonding with infant ○ Impaired functioning continues for several weeks or months after birth ○ Incidence 10% to 15% ■ Less eye contact ○ Screening tool for ALL patients 1. I have been able to laugh and see the funny side of things 2. I have looked forward with enjoyment to things 3. I have blamed myself unnecessarily when things went wrong 4. I have been anxious or worried for no very good reason 5. I have felt scared or panicky for no very good reason 6. Things have been getting on top of me 7. I have been so unhappy that i have had difficulty sleeping 8. I have felt sad or miserable 9. I have been so unhappy that i have been crying 10. The thought of harming myself has occured to me ● Risk factors ○ History of anxiety of depression ○ Younger age ○ Unintended pregnancy ○ Limited social or financial support ○ Substance abuse ○ Stressful life events in the previous year ■ Divorce, death, moving ○ Domestic violence ○ NICU admission is a huge risk ● Interventions ○ Collaborative (social worker and provider) who can connect patients with a support group and give medications ○ Educate significant other ■ Usually able to identify first Postpartum psychosis ● Hallucinations ● Delusions ● High levels of impulsivity 55 ● ● ● Significant risk for suicide or infanticide Incidence 0.1-0.2% Requires immediate EMS and hospitalization Breastfeeding concerns ● Nipple cracks, pain ○ Monitor, correct latch position ○ Baby needs to latch around edges or areola ● Discuss risk for infection ○ Risk for mastitis ○ Hand wash not hand sanitizer ● Engorgement ○ Hard, uncomfortable breasts ○ From increased milk production and increased blood and lymphatic fluid starts around day 3 ○ Cold, cabbage leaves (absorb fluid from breast glands) can reduce ○ Frequent feeding can also help reduce engorgement Mastitis ○ Definition: infection of ductal breast tissue ○ Contributing factors are incorrect latch, trauma to nipple, and incorrect handwashing ○ Assessment ■ Temperature > 100.4 degrees ■ Reddish, swollen, tender and mobile lump in the breast ■ May see a red streaky spot ■ Fatigue, malaise, and flu like signs and symptoms ○ Nursing and collaborative management ■ Rx: antibiotic safe for breastfeeding ■ Continue to breastfeed during recovery Subinvolution ○ Definition: delayed return of the enlarged uterus to normal size and function ○ Caused by: retained placental fragments or infection ○ Can cause: late postpartum bleeding after hospital discharge ■ Patient teaching very important about massage, involution, and lochia ○ Larger than normal uterus, prolonged or excessive lochia, reversal of lochia colors are all bad signs ○ D/C teaching about abnormal signs Uterine atony ○ Fundus is soft and boggy ■ Not contracting, shrinking, or expelling lochia ○ Retained placental fragments ■ Fundus high and firm ● Way too high Endometritis 56 ○ ○ ○ ○ Uterine infection Risks ■ C section ■ Operative vaginal delivery ■ Prolonged rupture of membranes ■ Multiple vaginal exams after rupture of membranes ■ Internal monitoring of fetus or contractions Assessment findings ■ Fever ■ Tachycardia ■ Fatigue ■ Uterine tenderness ■ Heavy lochia ■ Foul smelling lochia Interventions ■ Collaborative: report to provider ■ Broad spectrum IV antibiotics Postpartum hemorrhage related to uterine atony – pg. 151 ○ Large venous areas exposed after placenta separates from the uterine wall ○ If uterus is dysfunctional, flaccid, and relaxed, and then heavy venous bleeding occurs ○ This loss of muscle tone is called atony ○ Uterine atony is the leading cause of early postpartum hemorrhage ○ Boggy uterus= heavy lochia Postpartum hemorrhage ○ Risk factors (conditions which overstretch the uterus) ■ Fetal macrosomia ■ Multiple gestation ■ Polyhydramnios ○ Additional risk factors making it hard for uterus to contract ■ Magnesium sulfate→ relaxes muscles in the uterus ■ ■ ■ Rapid or prolonged labor (rapid= precipitous) Use of large amounts of pitocin in labor (oxytocin receptors saturated) High parity ● 5 or more births is a significant risk Postpartum hemorrhage related to uterine atony ○ Decreased voiding + postpartum diuresis = bladder distention ○ Excessive bleeding can occur because a distended bladder pushes up and to the side and prevents it from contracting firmly Oxytocics/Uterotonics ○ Pitocin IV ■ Primary prevention used in routine care ○ Methergine (Methylergonovine Maleate) IM 57 ■ ■ ■ Drug of choice for hemorrhage Increases blood pressure Contraindications: hypertension or preeclampsia ● Can cause to stroke out ○ Prostaglandin F2A (Hemabate) IM ■ Contraindications: asthma ● Can cause bronchospasms from prostaglandin ○ Misoprostol (Cytotec) Rectal, buccal, or oral ■ Can be used for cervical ripening ■ Increased dose to stop hemorrhage ■ Category X drug ● Do not use during pregnancy or loss of baby can occur ● Can use postpartum Additional interventions for postpartum hemorrhage ● Manual removal of retained placenta ○ Analgesics during procedure ● Surgical D&C (dilation and curettage) ○ Under anesthesia ● Tranexamic acid (TXA, lysteda) ○ Inhibits fibrinolysis ○ Use extreme caution due to hypercoagulation ● Antibiotics in infection ○ Increase risk for infection ● Bakri balloon tamponade ○ Inflated with sterile water or saline by provider Soft tissue hematoma ● Bleeding into a concealed tissue area, usually vulva or vagina ○ Forceps or vacuum use increases risk ● Painful ● May not be visible ● Associated with operative vaginal delivery ● Requires immediate provider intervention ● Take a set of vitals ● Can bleed to death internally C section (C/S) wound dehiscence – pg. 154 ● Fever ● Pain ● Increased tenderness ● Drainage ● Poor approximation ● Infection usually occurs after discharge 58 ● Discharge teaching important about warning signs to report to provider ● Risk factors ○ Catheterization ○ Regional anesthesia ■ Urinary stasis ○ Vaginal exams ○ C section Signs and symptoms ○ Dysuria ○ Frequency ○ Urgency ○ Hematuria Interventions ○ Collaborative antibiotic ○ Wipe front to back ○ Do not hold urine ○ Drink water UTI ● ● Postpartum thromboembolic disorders – pg. 155 ● Cause: increased coagulation factors and immobility ● Risks ○ C section ○ Obesity ○ Smoking ○ Advanced maternal age ● Superficial venous thrombosis ○ Unilateral pain, warmth, and tenderness in lower extremity ○ Visible enlarged hardened vein ● Deep vein thrombosis ○ Risk of travelling ○ Unilateral leg pain, swelling, warmth, redness ○ Anticoagulation medication ○ Gradual resumption of activity ■ Bedrest or up with assist according to provider orders ● Pulmonary embolism ○ Dyspnea, tachycardia, fever, cough, pleurisy, diaphoresis, pallor, weakness ■ Get vitals and pulse oximetry ● Medication ○ Coumadin (warfarin) is contraindicated in pregnancy and is a teratogen, but can be used postpartum with breastfeeding Hypertensive Disorders of Pregnancy – pg. 157 59 Gestational Hypertension ● Without proteinuria or other systemic changes ● Specific to pregnancy Preeclampsia ● Goal is to prevent eclampsia (seizures) Eclampsia ● Seizures Chronic hypertension ● Medication outside of pregnancy Chronic hypertension with superimposed preeclampsia ● Hand in hand Preeclampsia ● Definition: hypertensive syndrome which manifests after 20 weeks gestation including ○ Hypertension: 140/90 or greater ■ Two separate occasions at least 4 hours apart ■ Assess for increased BP postpartum ○ Proteinuria: greater than a trace/1+ ■ In the absence of proteinuria assessment ● Thrombocytopenia ● Impaired liver function ● New renal insufficiency ● Pulmonary edema ● New onset of cerebral or visual disturbances ○ Cerebral: headaches ○ Generalized edema ■ Fluid in tissues ■ Above the waist ■ Organ edema ■ Not diagnostic for preeclampsia ■ ○ ○ Pathological descent→ does not go away with rest, must treat it Hypertension and proteinuria are diagnostic These can manifest for the first time up to 48 hours after birth ● Incidence ○ 2-7% of all pregnancies in the united states ○ 10-15% maternal mortality worldwide ○ Leading cause of maternal and perinatal morbidity and mortality in the united states and canada ● Etiology ○ Unknown ● Associated/risk factors 60 ○ ○ ○ ○ ○ ○ ○ ○ ○ ○ First pregnancy Non-Caucasian Greater than 40 years Pregnancy with assisted reproductive technology ■ Increase risk when changes partners or IVF Increased exposure to placental tissue ■ Multiple gestation or trophoblastic disease ● Trophoblastic disease: egg and sperm meet but empty ovum, so dies early on or never there, but placenta continues to grow Interpregnancy interval greater than 7 years ■ Long time in between Poor outcome in previous pregnancy ■ Low birth weight is increased risk Pre-Existing disease ■ Diabetes ● Endocrine and vascular disorder ■ Renal disease ■ Collagen disease ■ Medical or genetic conditions ■ Chronic hypertension Family history and/or personal history Periodontal disease ■ ○ ○ ○ Inflammatory response→ preeclampsia Obesity or gestational diabetes ■ Could later develop type 2 diabetes ● Exercise and diet can prevent from developing Antiphospholipid antibody syndrome Factor V Leiden mutation ● Pathophysiology ○ Arterial vessel walls in uterus remain thick contributing to decreased placental perfusion and placental ischemia ■ Placenta blood vessels are thick and do not perfuse well ○ Placenta ischemia: endothelial cell dysfunction by stimulating the release of a substance toxic to endothelial cells ■ Trigger than sends toxins in blood vessels to endothelial lining causing vasoconstriction and vasospasms ■ Leads to generalized vasospasms, increased peripheral resistance ■ Increased endothelial cell permeability, poor perfusion in all organ systems ● Management of mild preeclampsia -- pg.160 ○ BP stable ■ Stays the same, does not keep elevating 61 ○ ○ ○ ○ ○ ● Urine protein less than or equal to 1+ Fetal evaluation: FMC, NST, BPP ■ Fetal movement counts ● Start at 28 weeks ● 10 movements every 1 hour ● Same time of day each time ● If level of movement decreases, go to hospital ■ Non stress test ● 2x a week ■ Biophysical profile ● Every week or every other week ● Good: 8 or 10 ● Bad: 6 or below Watch for subjective signs and symptoms to report ■ Headache ■ RUQ pain ■ Generalized edema ● Daily weight (no more than 1 lb a week) Activity restriction ■ Avoid prolonged sitting or standing ■ Rest often (every 2 hours for 30 mins) ■ Rest side lying to avoid compression of IVC Diet ■ Hydration: help vascular volume and perfusion ■ Protein: increased amount due to loss or protein in urine ■ Low salt: to help avoid retention and decrease edema Severe preeclampsia ○ BP greater than 160/110 ○ Proteinuria greater than 5g in 24 hours (3+ or 4+) ○ Oliguria less than 400 mL in 24 hours or less than 30 mL an hour ○ Hyperreflexia of 3+ or 4+ ○ Clinical symptoms ■ Visual changes ■ Generalized edema ■ Dyspnea ● Pulmonary edema ■ Epigastric pain or N/V ● Liver damage ■ Anxiety ● Cerebral hypoxia or edema ■ Irritability ○ Medication 62 ■ Magnesium sulfate ● Magnesium sulfate therapy ○ Required hourly assessments ■ Respiratory rate ■ DTR’s ■ Urine output ● Only way to excrete is through kidneys ○ Toxicity ■ Less than 12 respirations a minute ■ No DTR response ■ Less than 30 mL of output in an hour ○ Antidote ■ Calcium gluconate ● 10% solution in 10 mL administered IV over 3 to 5 minutes ● Stop magnesium sulfate ● If pushed to fast, can cause cardiac arrest or arrhythmia ○ Foley bag with urometer ■ Measures urine output every hour ■ Will tell us about renal failure ■ Build up means CNS is severely depressed ■ 30 mL/hour or more means kidneys functioning at bare minimum ● Nursing care ○ Monitor VS and FHR ○ Decreased external stimuli ○ Monitor: UO, urine protein, and specific gravity ○ Assess for generalized edema ○ Assess for premature placenta separation (abruptio placenta) ■ Very painful ■ Premature separation of placenta from wall of uterus→ severe hypoxic fetus→ bradycardia ● ○ ○ ○ ○ Calm environment to decrease seizure risk Padded side rails No visitors Specific gravity (kidney function for concentrating urine) ○ Kidneys failing → more dilute so 1.030 (higher specific gravity) HELLP – pg. 162 ○ Hemolysis ■ Of red blood cells ■ Order labs ■ CBC for RBC check and platelets 63 ○ ○ ○ ○ ● ■ Liver enzymes (ALT and AST) Elevated Liver enzymes Low Platelets ■ Less than 100,000 ■ Another complication of preeclampsia Lab studies ○ CBC (includes platelets) ○ Clotting studies ○ Bleeding time and fibrinogen ■ Prolonged bleeding ○ Liver enzymes ■ LDH (45-90 units/L) ■ AST (4-20 units/L) ■ ALT (3-21 units/L) ○ Chemistry ■ BUN ■ Creatinine ■ Uric acid ■ Glucose ■ All related to renal function 64 Placenta – pg. 172 Placenta abruptio ● Definition: premature separation of a normally implanted placenta from wall of uterus ● Incidence: 1 in 120 births or 1% ● Types ○ Marginal overt ■ At margin or edge of placenta and bleeding visible ■ Late decels and goes from moderate to minimal to absent variability ○ Central concealed ■ From center, blood trapper behind placenta ■ Late decels ○ Complete concealed ■ Detached and blood pooled behind ■ Bradycardia ● Associated factors ○ Hypertension or preeclampsia ■ 60% or higher chance ○ Physical trauma ■ Accident ■ Abuse ○ Alcohol abuse; smoking ■ Due to decreased blood flow ○ Excessive or sudden changes in intrauterine pressure ■ Airplane (usually cannot fly after certain gestation) ○ Increased maternal age and parity ■ Blood flow connection ○ Cocaine abuse ■ Some dose before labor if addicted ● Clinical manifestations ○ Dark red bleeding visible ○ Painful ○ More RBC and oxygen ○ Sometimes not visible ○ Go to hospital ● Clinical signs ○ Vaginal bleeding dark ○ Abdominal pain ○ Uterine hyperactivity with poor relaxation between contractions ○ Uterine tenderness ● S/S of concealed hemorrhage 65 ○ ○ ○ ○ ○ Increased fundal height Hard board-like abdomen High uterine baseline tone Persistent abdominal pain Progressive late decels in FHR and/or decreasing baseline variability ■ Any periodics ■ Signals decrease blood flow change Placenta previa ● Definition: abnormal implantation of the placenta by location ○ Placenta is abnormally located somewhere near cervix ● Incidence ○ 1 in 200 pregnancies; 0.5% ● Types ○ Low-lying ■ Does not cover cervix ○ Partial ■ Some covering the cervix ○ Complete ■ Covers complete cervix ■ Deliver via c section ● Associated factors – pg. 173 ○ Decreased vascularity of upper uterine segment ○ Multiparity with decreased spacing ■ Less than 18 months between pregnancies ○ Scar tissue from previous surgery ■ Fibroids that can leave scar tissue (not ideal) ○ Advanced maternal age ■ Bad blood flow or perfusion ● Clinical manifestations ○ Bright red bleeding ■ Always visible ○ Painless or silent bleeding ■ From dilation ○ Uterine shape abnormal ■ Abnormal fetal lie ● More common if complete previa ● May have transverse fetal lie S/S of early hemorrhage – pg. 177 ● Tachycardia, decreased peripheral pulses ● Increased respirations 66 ● ● ○ Increased oxygenation to blood Normal or slightly elevated BP ○ Late sign, including MAP (=70) ○ Trying to increase perfusion ○ Vasoconstriction and shunting Cool, pale skin S/S of late hemorrhage ● Falling blood pressure ○ HR stays tachycardic but cannot keep blood pressure up ● Pallor, skin cold and clammy ● Urine output less than 30 mL/ hour ○ Not enough blood to renal system ● Restlessness, agitation, decreased mentation ○ Cerebral hypoxia Additional hemorrhage problems of childbearing ● Uterine rupture ○ Complete or incomplete ● Uterine inversion ○ Partial or complete ● Uterine atony ○ Failure of the uterine muscle to contract after delivery ● DIC (disseminated intravascular coagulation) ○ Cause or related factor to above problems ○ Causative: placenta abruptio, IUFD, sepsis, amniotic fluid embolism, thrombi in organs secondary to PIH ○ Treatment: delivery, replacement of clotting factors, and physiological support for hemorrhage ● Nursing care ○ IV access with lactated ringers ○ Vitals ○ Attach fetal monitor externally ○ Assess bleeding ○ Assess pain ○ Oxygen 8 to 10 liters via facemask ○ Foley with urometer ○ Ultrasound ○ Order labs ○ Palpate fundus ○ Nothing internally ○ Vaginal or c section ■ Check fetal oxygenation 67 68 Diabetes in Pregnancy – pg. 179 Metabolic changes associated with pregnancy ● Glucose is transported across the placenta by carrier-mediated facilitated diffusion ○ Back and forth ● Glucose levels in the fetus are directly proportional to maternal levels ● Although glucose can cross the placenta, insulin does not ● At approximately 10 weeks the fetus begins to secrete its own insulin First trimester ● HCG hypoglycemic effect ● May contribute to maternal fatigue and nausea and vomiting Second and third trimester ● Human placental lactogen (HPL) ○ Blocks efficacy of maternal insulin ○ Primary hormone that causes insulin resistance ○ Insulin resistance is a glucose sparing mechanism that ensures an abundant supply of glucose for the growing fetus ○ “Diabetogenic” effect on maternal metabolism ■ Any pregnancy has the potential to develop gestational diabetes ● Only when pregnant ■ All women must be screened for diabetes in pregnancy Postpartum ● At birth, expulsion of the placenta prompts an abrupt drop in hormones ● Maternal tissues quickly regain their pre pregnancy sensitivity to insulin White’s classification of pregestational diabetes (present BEFORE pregnancy) ● Endocrine dysfunction→ affects multiple systems ● Class B ○ Onset of disease occurs after age 20 ○ OR duration of illness less than 10 years Class C ○ Onset of disease occurs between age 10-19 ○ OR duration of illness 10-19 years Class D ○ Onset of disease occurs before age 10 ○ OR duration of illness greater than 20 years Class F, R, T Diabetes begins as an endocrine dysfunction, and over time will affect multiple systems, due to vascular changes ● ● ● ● 69 ● ● Class A ○ Pregnancy only ○ No known diabetes before pregnancy ○ Diet controlled Class A2 ○ Pregnancy only ○ No known diabetes before pregnancy ○ Requires medication for blood glucose control Gestational diabetes and common newborn complications ● Poor glycemic control layer in pregnancy (particularly in women without vascular disease) increases the incidence of LGA ● Increased risk ○ Birth trauma ○ Shoulder dystocia ■ Head comes out but shoulders are stuck ○ Operative vaginal birth ■ Forceps and vacuum ○ C section (CPD) ● Newborn hypoglycemia ○ Less than 40 mg/dL ○ Altered temperature and respirations ● Respiratory distress syndrome ○ Excess fetal insulin can delay surfactant production ■ Opens alveoli for breathing Gestational diabetes risk factors – pg. 183 ● Family history of diabetes ● History of unexplained intrauterine fetal demise (IUFD) ● History of macrosomic infant ● History of infant with congenital anomaly ● Personal history of gestational diabetes ● Ethnicity other than white ● Age greater than 25 ● BMI greater than 30 ● Hypertension ● Recurrent vulvovaginal candidiasis ○ ● ● ● ● Yeast infection→ yeast eats sugar Glycosuria on more than one occasion Polyhydramnios ○ Excess amniotic fluid Excessive maternal weight gain Fundal height greater than expected 70 Gestational diabetes screening ● 24 to 28 weeks routine screening ● Glucose challenge test ○ Random 1 hour post 50 gram glucola ○ Plasma values below 130 to 140 rule out diabetes ■ 135 is the cut off Gestational diabetes diagnosis ● Glucose tolerance testing ○ Fasting 100 gram glucola ■ FBS: 95 ■ 1 hour: 180 ■ 2 hour: 155 ■ 3 hour: 140 ○ GDM: elevated FBS or any 2 elevated values ○ Fail 2 of them to have diabetes Gestational diabetes plan of care ● Blood glucose monitoring ○ 4 to 5 times a day ○ Documentation ● Dietary changes ○ 3000 calories/day ○ Only 50% carbohydrates ● Exercise ○ 1x/day after biggest meal ○ 30 min gentle walk ○ Should be able to talk through workout ● Serial growth ultrasounds ● Twice weekly NSTs ○ 20 minutes on monitor ○ 15 bpm for 15 seconds 2 times in 20 minutes Gestational diabetes goal ● HbA1C less than 6% ● Euglycemia: 70 to 110 ○ Very strict because patient is carrying fetus ● Fasting blood sugar less than 95 ● 1 hour postprandial blood sugar less than 140 ○ After meals Pharmacological vs. non-pharmacological ● 75% of gestational diabetes patients controlled by diet and exercise alone ● Those who cannot achieve euglycemia by diet alone will require medication ○ Oral hypoglycemic therapy ■ Glyburide or metformin 71 ○ Insulin ■ If oral medication does not control blood sugar Nursing interventions – pg. 186 ● Promoting compliance ○ Blood glucose monitoring and documentation (4 to 5 times a day) ○ Diet ○ Medication ● Education on the importance of screening and diagnostic process ○ Explain rationale ● Coordinating healthcare team Intrapartum management ● Hourly glucose monitoring ○ Stress response and not eating during labor ● Risk for ○ Should dystocia, operative delivery, c section ○ Put in McRoberts position for shoulder dystocia ■ Knees to ears ■ Opens up pelvis outlet 2 to 3 cm more Postpartum management ● Fasting blood sugar morning after delivery ○ Should be less than 95 and then they can be changed to a regular diet ● 6 week postpartum screening ○ 2 hour OGTT or FBS to make sure patient is not a Type 2 diabetic ● Establishment of PCP for continued screening ● Increased risk of Class B (Type 2) Diabetes later in life ● Newborn care ○ Careful musculoskeletal assessment for birth trauma ■ Bruising or fractures ○ Initiate early breastfeeding in first hour of life to prevent hypoglycemia ○ Increased risk for newborn hypoglycemia ■ Assess for warning signs ● Shaky, hypothermia ■ Monitor glucose levels before meals ● Important especially in first 24 hours Pregestational diabetes – pg. 188 ● Diabetogenic state of pregnancy + pregestational diabetes = serious implications ● During the first trimester there may be a decreased need for insulin ○ Can cause morning sickness ● But insulin resistance begins in second trimester 72 Complications ○ Increased risk for DKA in pregnancy → can be teratogenic ● DKA precipitated by ○ Infections ○ Illness or stress ○ Poor compliance ○ Tocolysis (Terbutaline) ○ Corticosteroids (Betamethasone) ○ DKA can lead to IUFD/stillbirth (10%) ● Placental insufficiency ○ Particularly in women with vascular disease ○ Intrauterine growth restriction ○ Intrauterine fetal demise ● Extended periods of hyperglycemia in the first trimester ○ Teratogenic effects ■ Spontaneous abortions/miscarriages ■ Congenital malformations ● Cardiovascular (heart defects) ● Central nervous system ○ Level 2 ultrasound for more details Plan of care ○ In addition to GDM management ○ Early PNC (prenatal care) ○ Early dating ultrasound ○ Eye exam (optic vasculature is very fragile) ○ Level 2 ultrasound ○ Fetal echocardiogram 73 74 Heart Disease and Anemia in Pregnancy – pg. 191 Review: Normal Fluid Shifts in Pregnancy Increased intravascular volume (more blood circulating) Decreased systemic vascular resistance (3rd spacing + more edema) Increased CO Functional Classification of Heart Disease 1. Asymptomatic at normal activity level 2. Symptomatic at increased activity 3. Symptomatic at ordinary activity 4. Symptomatic at rest (Do they have symptoms at these levels?) Contraindications to Pregnancy Pulmonary hypertension Marfan’s syndrome (genetic condition affecting connective tissue, even of the heart) Complex cyanotic congenital heart disease (cyanosis in body) Aortic coarctation, complicated by aortic dissection (rupture) Poor ventricular function (CHF) Cardiac Decompensation in Pregnancy Increasing fatigue and/or difficulty breathing during usual activities Feeling of being smothered Frequent cough Palpitations (reports of it getting worse) Progressive generalized edema (face, arms, not full body) Irregular, weak, rapid pulse Bilateral crackles in bases (of lungs) Orthopnea (discomfort when breathing while lying down) Rapid respirations Moist cough Cyanosis of lips and nail beds Prenatal Care Nursing Diagnosis o Ineffective tissue perfusion o Activity intolerance o Knowledge deficit o Self-care deficit o Fear Interventions o Education on warning signs o Nutrition 75 o o Wellness, reduction of infection exposure Medication changes (routes/ doses tweaked) Restrictions (based on functional classification) 1. 8-10 hours of sleep/day with naps 2. Avoid heavy exertion; eliminate certain activities 3. Bed rest for much of the day 4. Initiative efforts to improve cardiac status to continue pregnancy (Admit to hospital) Labor & Birth Pain control Positioning in labor and birth Decrease length of 2nd stage o Laboring down (may be at 10cm but may want them to wait like an hour to push) Open glottis pushing o Valsalva reduces ventricular filling and overflow Beta Adrenergics: Terbutaline (Brethine) o Contraindicated: tachycardia Endocarditis Prophylaxis Postpartum Hemodynamic monitoring (CCU) Vital signs Ergot Alkaloids (Methergine) contraindicated Avoid hemorrhage or infection Monitor for warning signs of cardiac decompensation Breastfeeding o Monitor NB carefully if diuretics used Nursing Diagnosis - Ineffective family coping - R/T Maternal Infant separation - R/T Alterations in breastfeeding Discharge Plan - Help and support at home - Rest and sleep - Activity - Diet - Medications - Continued breastfeeding support - Contraception Anemia – pg. 197 76 Iron deficiency anemia Pathologic anemia of pregnancy o Hemoglobulin less than 11 o Normal Hgb Electrophoresis (no hemoglobinopathy – sickle cell) Iron supplementation o Ferrous Sulfate o Ferrous Gluconate Iron Supplementation Vitamin C increases absorption Bran, tea, coffee, milk, spinach, swiss chard, and egg yolk decreases absorption of iron Iron is best absorbed on empty stomach o With Vitamin C if possible Constipation (cause) o Fiber o Water 77 Perinatal Infections – pg. 199 Sexually transmitted infections (STI) ● Infections or infectious disease syndromes primarily transmitted by close, intimate contact ○ Do not assume how patient got it ● Screening and treatment recommendations ○ Centers for disease control and prevention ○ CDC.gov/STD ● Risks ○ Age >25 years old ○ Multiple partners ○ Non use of barrier contraception ■ Condoms ○ Low socioeconomic status ○ IV drug use (viral) ○ Anal sexual activity ■ Tissues in rectum are much more fragile ○ Intercourse with commercial sex workers ○ Sex with partners with any of the above characteristics ○ Annual screening of STIs is recommended for patients with risk factors ○ Test of cure ● Nursing care: primary prevention ○ Aims to avoid the development of a disease or disability in healthy individuals ○ A: abstinence, delayed sexual debut for adolescents ○ B: be faithful, partner reduction ○ C: condoms, factual information regarding condom use ● Nursing care: secondary prevention ○ Early disease detection ○ Prevent the worsening of the disease and the emergence of symptoms ○ Minimize complications and limit disabilities before the disease becomes severe ○ Detection of disease in asymptomatic patients with screening or diagnostic testing ○ Preventing the spread of communicable diseases ○ Screening ○ Notification and treatment of partners and family ● ○ Expedited partner therapy→ give prescription to partner even if not a patient ○ Referral and reporting to community agencies Reporting and confidentiality ○ Reportable STDS ■ Syphilis 78 ○ ○ ■ Gonorrhea ■ Chlamydia ■ HIV ■ Hepatitis ■ Zika Transplacental STDs ■ Syphilis ■ HIV ■ Herpes ■ Zika Toxoplasmosis ● History ○ Sexual health history: 5 P’s ■ Partners ■ Pregnancy prevention ■ Protection from STD ■ Practices ● Oral, anal, vaginal ■ Past history of STDs ● Symptom analysis – pg. 203 ○ Flu like symptoms ○ Irritation, itching, or vaginal pain ○ Abdominal or pelvic pain ○ Vaginal odor ○ Green or bloody vaginal discharge ○ Upper reproductive tract symptoms ○ Pain with intercourse (dyspareunia) ○ Urinary symptoms (frequency, urgency, dysuria) ○ Sores, bumps ○ Self care to date ○ Partner symptoms Infections and preterm delivery ● Births occurring prior to 34 weeks are much more frequently accompanied by clinical or subclinical intra-amniotic infection compared to births after 34 weeks Bacterial infections ● Chlamydia ● Gonorrhea ● Syphilis ● Bacterial vaginosis 79 Chlamydia ● Transmission ○ Vaginal, anal, or oral sex ● Symptoms ○ More obvious in men than women ○ Can be asymptomatic ○ Vaginal, rectal, or penile pain or discharge ○ Dysuria more common in males ● Screening recommendations ○ Cervical, vaginal, urine DNA probe ○ Annually and with first pregnancy visit ● Treatment if not pregnant ○ Doxycycline PO ● Treatment if pregnant ○ Azithromycin (zithromax) PO ○ PTL or PPROM (preterm labor or preterm premature rupture of membranes) ● Fetus/newborn ○ In birth canal ○ Ophthalmia neonatorum ■ Newborn blindness ○ Pneumonia Gonorrhea ● Transmission ○ Vaginal, anal, or oral sex ● Symptoms ○ Can be asymptomatic ○ Vaginal, rectal, or penile pain or discharge ○ Dysuria ● Screening recommendations ○ Cervical, vaginal, urine DNA probe ○ Annually and with first pregnancy ● Treatment ○ Ceftriaxone (rocephin) IM ■ For pregnant and nonpregnant patients ● Pregnancy ○ PTL, PPROM Pelvic inflammatory disease (PID) ● Infection of the upper reproductive tract ○ Trying to avoid ● Causative organisms ○ Gonorrhea ○ Chlamydia 80 ● Long term complications ○ Ectopic pregnancy ○ Infertility ○ Chronic pelvic pain/low back pain Syphilis ● Transmission ○ Direct contact with a syphilis sore during vaginal oral sex ○ Vertical transmission (mother to baby) ○ Can pass through placenta ● Symptoms ○ Primary: painless chancre (some patient may not know about it) ○ Secondary: flat, maculopapular rash ○ Tertiary: multiple organs affected ● Screening ○ Serum RPR: rapid plasma reagin ○ Serum VDRL: venereal disease research laboratory ● Treatment ○ Penicillin G PO ● Pregnancy ○ Low birth weight ○ Preterm labor ○ Still born, intrauterine fetal demise (IUFD) ● Fetus/newborn ○ Cataracts ○ Deafness ○ Neurological complications ● Pregnancy ○ Crosses placenta ○ Screening at first prenatal visit and 28 weeks Bacterial vaginosis ● Has been found in virgins ● Caused by a disturbance in the vaginal ecosystem ○ Introduction of an infectious organism ○ A disturbance that allows the pathogens normally residing in the environment to proliferate ● Symptoms ○ Thin white or gray discharge ○ Dead fish smell, particularly after sex ■ Anaerobes rupture ○ Vaginal pain, itching, or burning ○ Dysuria ● Screening 81 ● ● ● ○ Wet prep ○ Whiff test based on symptoms Treatment ○ Metronidazole (Flagyl) PO or vaginal ■ Do not drink alcohol until 1 week after finishing medication Pregnancy ○ Associated with preterm labor and preterm premature rupture of membranes Fetus/newborn ○ Low birth weight Fungal Infections: Candidiasis ● Fungal infection or yeast infection ● Caused by disturbance in the vaginal ecosystem ○ Introduction of an infectious organism ○ A disturbance that allows the pathogens normally residing in the environment to proliferate ● Symptoms ○ Vaginal itching, irritation, burning, dysuria ○ Thick white, clumpy discharge ● Screening ○ We prep based on symptoms ● Treatment ○ Miconazole cream or suppositories ○ Diflucan PO (antifungal) ● Pregnancy ○ No known complications ● Fetus/newborn ○ Oropharyngeal infection ■ Thrush ○ Rarely, a life-threatening systemic infection occurs in the newborn, these infants are most often immunologically compromised or debilitated, and the mortality is high Viral infections – pg. 209 ● HIV ● Hepatitis B ● Herpes simplex virus (HSV) ● Human papillomavirus (HPV) ● Zika virus Human immunodeficiency virus (HIV) ● Transmission ○ Blood and bodily fluids ○ Iv drug use ○ Transmission of virus is higher when other infections are present 82 ■ ● ● ● ● ● ● Especially syphilis, chlamydia, and rectal gonorrhea Symptoms ○ Within 2 to 4 weeks after infection ○ Fever, chills, rash, night sweats, muscle aches, sore throat, fatigue, swollen lymph nodes, or mouth ulcers ○ Can last anywhere from a few days to several weeks Screening recommendations ○ Patients aged 13 to 64 years in all health care settings Treatment ○ Antiretroviral therapy to decrease viral load ○ No cure Pregnancy ○ Oral antiretrovirals after 14 weeks gestation ■ If untreated, 30% placental/fetal transmission rate ■ With treatment, 2% transmission rate Labor and birth ○ Goal: diminish time elapsed from rupture of membranes to birth ○ Goal: reduce fetal/newborn exposure to vaginal mucosa ■ Avoid internal monitoring ■ Intrapartal antiretroviral therapy ● IV high dose during labor ○ Vaginal vs. c section Newborn care and feeding ○ Bathe at birth ○ Breastfeeding is contraindicated ○ 6 weeks antiretroviral therapy prophylaxis Hepatitis B ● Transmission ○ Activities that involve percutaneous or mucosal contact with infectious blood or body fluids ● Symptoms ○ Asymptomatic ○ Flu like symptoms ● Treatment ○ Antivirals to decrease viral load ○ No cur ● Screening ○ Pregnant women (HBsAg only is recommended) ■ HBsAg is elevated if there is an infection of Hep B (called Hep B surface antigen) ○ Infants born to HBV-infected mothers ● Pregnancy ○ Vaccine safe 83 ● ● Newborn care ○ Precautions at birth ○ Avoid internal monitoring ○ Immediate bath ○ Hep B immunoglobulin (HBIG) 0.5 mL IM within 12 hours of birth in Hep B positive mothers ○ Hep B vaccine 0.5 mL IM within 12 hours of birth in all babies ○ IM selection site: vastus lateralis Breastfeeding safe ○ Can start immediately ○ Very small amount of Hep B shed, GI system acidity will destroy ○ Benefits outweigh the risks Hepatitis C ● Transmission ○ Iv drug use ○ Sexual transmission is possible but rare ● Symptoms ○ The majority of infected persons might not be aware of their infection because they are not clinically ill ○ For some people, Hep C is a short-term illness but for 70% to 85% of people who become infected, it becomes long-term and chronic ● Screening recommendations ○ Baby boomers (1945-1965) ○ Iv drug users ○ Long term dialysis ○ HIV and Hep C comorbidity ○ Babies born to Hep C positive mothers ■ Can go through placenta ● Treatment ○ Requires genotyping and antiviral medications ○ No vaccine ● Pregnancy ○ 4% to 7% chance of vertical transmission ● Fetus/newborn ○ Vertical transmission Human papillomavirus (HPV) ● Transmission ○ Vaginal, anal, or oral sex ● Symptoms (according to type) ○ Condyloma (genital warts) ○ Cervical, vaginal, penile, anal, or oropharyngeal cancer ● Screening recommendations ○ Only cervical cancer screening 84 ● ● Treatment ○ TCA, aldara, for condyloma ○ Cervical atypia: LEEP Pregnancy ○ No significant risk ○ Vaccination safe in pregnancy Herpes simplex virus (HSV) ● Transmission ○ A herpes sore ○ Saliva or genital secretions ○ Skin in the oral area if your partner has an oral herpes infection or skin in the genital area if your partner has a genital herpes infection ○ From a sex partner who does not have a visible sore ○ Oral herpes caused by HSV-1 can be spread from the mouth to genitals through oral sex, this is why some cases of genital herpes are caused by HSV-1 ● Symptoms ○ Small blisters that break and leave painful ulcers on the genitals, rectum, or mouth ○ Primary infection ■ Symptoms within 2 to 3 days of exposure ■ Fever, body ache, swollen lymph nodes ○ Recurrent infection ■ Prodromal symptoms: tingling, itching, shooting pain may occur before recurrent lesions ● Screening recommendations based on symptoms ○ Serum IGG ○ Viral cultures of lesions ● Treatment ○ Valacyclovir or acyclovir (pregnancy category B) ● Pregnancy ○ Primary infection in pregnancy passes to placenta ○ Spontaneous abortion (miscarriage) ○ Preterm labor ○ Recurrent infection in pregnancy: rare, remote risk to fetus ○ Suppression at 36 weeks gestation ■ Decreased likeliness of outbreak for vaginal birth ■ ○ ○ C section→ if outbreak Goal: prevent newborn contact with active lesion Neonatal herpes= life threatening Zika virus ● Transmission ○ Mosquito (vector) bites and sexual contact 85 ● ● ● ● ● ● Risk factors ○ Travelling ○ Sexual intercourse with someone who has recently traveled Symptoms ○ Fever, rash, headache, joint and muscle pain, conjunctivitis (pink eye) Screening recommendations ○ Symptomatic patients who have traveled to high risk areas or had sex with those who have, need screening Treatment ○ None Pregnancy/fetus/newborn ○ Can cause microcephaly and other severe brain defects ■ Teratogenic during implantation to 8 weeks gestation Nursing interventions in primary and secondary care ○ Pregnant women should not travel to areas with risk of zika ○ Prevent mosquito bites ■ Mosquito repellent is safe for pregnancy ○ Prevent getting zika through sexual contact TORCH ● Toxoplasmosis ● Other (varicella. parvovirus) ● Rubella ● Cytomegalovirus ● Herpes ○ Few symptoms ○ Lack effective therapy ○ Major consequences for fetus ○ Providers may screen for these infections if unexplained complications occur in pregnancy Parasites – pg. 216 ● Toxoplasmosis ● Trichomoniasis Toxoplasmosis ● Transmission ○ Fecal/oral ● Most common foodborne illness ● Present in raw meat and cat (vector) feces ○ Do not change litter box ● Symptoms ○ Very few have symptoms because the immune system usually keeps the parasite from causing illness ● Screening based on pregnancy complications→ usually too late 86 ● ● ● Treatment ○ None Pregnancy/fetus/newborn ○ Can be teratogenic from implantation to 8 weeks Prevention ○ Nursing interventions in primary and secondary care ■ Have support person clean litter box ■ Wear gloves when gardening ■ Wash hands with soap and water ■ Teach children the importance of washing hands to prevent infection ■ Cook meat to at least 165 degrees ■ Avoid cross contamination when preparing food ● Cutting boards ■ Wash fruits and vegetables before consumption Trichomoniasis ● Transmission ○ Vaginal, anal, or oral sex ● Symptoms ○ Itching, burning, redness, or soreness of the genitals ○ Discomfort with urination ○ A change in their vaginal discharge that can be clear, white, yellowish, or greenish with an unusual fishy smell ● Screening ○ Wet prep ○ Whiff test based on symptoms ● Treatment ○ Flagyl (metronidazole) PO → anaerobic cells ○ ● Precautions ■ Do not drink until 1 week after medication is done Pregnancy/fetus/newborn ○ Preterm delivery ○ Low birth weight Perinatal infections that are at risk to the fetus and route of transmission ● Transplacental ○ Syphilis ○ HIV ○ Herpes (primary) ○ Zika ○ Toxoplasmosis ● Infects during birth ○ Gonorrhea ○ Chlamydia 87 ● ● ○ Hep B ○ Hep C ○ Herpes ○ HIV Transmitted through breast milk ○ Hep B ○ HIV Associated with preterm labor ○ Trichomonas ○ Bacterial vaginosis ○ Gonorrhea ○ Chlamydia Periodontal disease ● One of the most common chronic infectious disease known in humans ● Associated with adverse perinatal outcomes such as ○ Spontaneous abortion ○ Preeclampsia ○ Low birth weight ○ Preterm birth ○ Still birth ● Patient education ○ Daily brushing and flossing ○ Dental problems can cause significant problems in pregnancy 88 Preterm Labor and Birth – pg. 220 Incidence ● 11.55% in the US in 2012 ● WHO worldwide 9.6% ● Rates are highest in Africa and North America ● Lowest in Europe ● Prematurity is the leading cause of infant mortality ● Average cost of a preterm birth in Ohio is $30,000 ● 20 weeks to 36 weeks 6 days 3 things causing ● Cervical change ● Uterine contractions ● Rupture of membranes Risk factors ● Nonwhite race ● Decreased socioeconomic status ● Domestic violence ● Lack of education ● Lack of access to prenatal care ● Smoking ● Substance abuse ● Periodontal disease ● History of previous preterm delivery ● Age less than 18 or greater than 35 ● Genitourinary infections ● Multifetal gestation ● Polyhydramnios ● Second trimester bleeding ● Obese or underweight BMI ● First degree female relative with a preterm birth ● History of multiple elective or spontaneous abortions ● Cervical surgery (LEEP) ○ Removal of cervical atypia ● Uterine anomaly ○ Mullerian Pathophysiology ● Multifactorial, maternal/fetal stress ● Infection ○ Genitourinary ○ Periodontal disease ● Antepartum hemorrhage 89 ● ● ● ● ○ Results in uteroplacental ischemia or hemorrhage Uterine overdistention Decreased progesterone ○ Helps keep woman pregnant (relaxes smooth muscles) Allergic reaction ○ Immune response Genetic Symptoms – pg. 222 ● Persistent pelvic pressure between legs or lower belly ● Menstrual like cramping in lower abdomen or back ● Low dull back ache ● Sharp painful tightenings ● Contractions, or tightening of the abdomen, with or without pain, 4 to 6 times and hour ● Feeling like baby is “balling up” ● Diarrhea ● Vaginal spotting or bleeding ● Watery, clear, pink, or red vaginal discharge ● Feeling like something is not right ○ Sense of impending doom Prevention ● Early prenatal care ○ Have you ever had a baby born a month or more early? ○ Have you ever had a baby in the NICU? ○ Have you ever had a miscarriage after 4 months? (preterm birth) ● Risk factor analysis ○ If patient is poor historian, may need to request previous delivery records from past hospital ○ Empower patients by educating them on the warning signs of preterm labor, the risks of preterm birth, and the advantages of preventive medication for current and future pregnancies Nursing assessment – pg. 224 ● History of preterm birth ● Risk factors ● EGA weeks and days ● Symptoms assessment (which ones do they have?) ● Social support, family, domestic violence screening ○ Can come from difficult circumstances Fetal fibronectin (fFN) ● Glycoprotein produced by the fetus ● 24 to 34 weeks 90 ● ● Related to placental inflammation and preterm labor Positive swab could indicate early delivery Maternal assessment ● Vital signs ● Uterine activity ● Cervix→ dilates from inside out ● ● ● ○ Digital: finger tips ○ Ultrasound Fetal fibronectin, CBC, UA, vaginal/cervical cultures Toxicology screens Evaluation for ROM ○ Fern test ○ Nitrazine test to check pH Fetal assessment ● Fetal heart rate, BPP, NST if appropriate EGA ● Amniotic fluid volume, placenta by ultrasound ● Fetal lung maturity ○ Sometimes amniocentesis to determine L/S ratio Inpatient hospital care with diagnosis of ACE/ACD (advanced cervical effacement/dilation) ● Activity restriction ● Pelvic rest ○ No sex ● Hydration ○ IV ○ Oral ● Tocolysis ● Continued monitoring for infection, ROM ● Prophylactic or therapeutic antibiotics Vaginal cerclage ● Surgical procedure to close cervix ● Timing of placement ○ 12 to 14 weeks for prophylactic ○ Rescue/emergent ■ Keep baby in, also reverse trendelenburg ● Timing of removal ○ 37 weeks ○ Or at start of preterm labor Antenatal corticosteroid therapy 91 ● ● ● ● ● ● Stimulates fetal lung maturity by promoting release of enzymes that induce production or release of lung surfactant 24 to 34 weeks gestation Betamethasone ○ Given in preterm labor, help breathe significantly better ○ 12 mg IM for 2 doses, 24 hours apart ■ Hold baby in for 24 hours Dexamethasone ○ If shortage of betamethasone ○ 6 mg IM for 4 doses, every 12 hours ■ Increased blood glucose levels ■ Extremely careful in diabetic patients Maternal effects ○ Transient (72 hours) increase in WBCs ○ Hyperglycemia Nursing considerations ○ Deep IM in vastus lateralis ○ Injection is painful ○ Assess blood glucose levels ○ Diabetics may require increase insulin doses for several days Progesterone ● Relaxes smooth muscle of uterus ● Prophylactic (can hold off for 2 weeks) ● Significantly reduces the risk of delivery before 37 weeks in patient with risk factors ● 16 to 36 weeks ● For women with a short cervix or previous preterm birth ● Category A: no known teratogenic effects ● Vaginal capsules or suppositories (every day) ● Equivalent to hydroxyprogesterone caproate (MAKENA) 250 mg IM weekly ● Nurses role: give shots starting at 16 weeks Tocolytics ● Toco: contraction ● Lytics: break up ● Anti Contraction medication or labor suppressant ● Mitigates symptoms ● Relaxation effect on smooth muscle ● Opposite of oxytocics or uterotonics which induce labor Magnesium sulfate – pg. 229 ● Different indication than preeclampsia ● CNS depressant→ alters seizure threshold ● Leading dose less than preeclampsia 92 ● ● Maintenance dose less than preeclampsia May prevent neonatal neurologic complications (cerebral palsy) ○ ● Give to preemie before born → protects brain Nursing assessment for toxicity ○ Maternal ■ Hot flushes, sweating ■ Nausea and vomiting ■ Lethargy ■ Transient hypotension ○ Fetal ■ Reduced FHR baseline variability ■ Decreased breathing movements Terbutaline (Brethine) ● Beta-adrenergic agonist (beta-mimetic or bronchodilator) ● 0.25 mg SQ every 4 hours ● PO ● Adverse effects ○ Tachycardia (maternal and fetal) ○ Hyperglycemia ○ Hypotension ● Nursing considerations ○ May need to withhold medication based on maternal HR greater than 110 ○ Cardiac disease ○ Diabetes ○ Hemorrhage ■ Will cause to bleed out due to dilation Indomethacin (Indocin) ● Prostaglandin synthetase inhibitor (NSAID) ● PO every 6 hours ● Adverse effects ○ Nausea and vomiting ○ Heartburn ● Nursing considerations ○ Administer with food to limit GI distress ○ Asthma ○ Hemorrhage Nifedipine (Procardia, Adalat) ● Calcium channel blockers (antihypertensive) ● PO every 3 to 6 hours ● Long-acting formulations every 8 to 12 hours ● Adverse effects (rare) 93 ● ○ Hypotension Nursing considerations ○ Do not combine with other tocolytics ○ Hemorrhage PROM, PPROM ● Premature rupture of membranes ○ Spontaneous rupture of the amniotic sac and leakage of amniotic fluid beginning before the onset of labor, at any gestational age ● Preterm premature rupture of membranes ○ Rupture of membranes at 20 weeks to 36 weeks 6 days ○ 10% of all preterm births in the US ○ Pathological weakening of the amniotic membranes caused by inflammation, stress from uterine contractions, or other factors that cause increased intrauterine pressure ○ Infection of the urogenital tract is a major risk factor ○ Symptoms ■ Leaking of fluid: sudden gush or slow leak ○ Assess maternal temperature ○ Check fetal baseline for tachycardia ○ Patient education on diagnostic process ■ Nitrazine and fern test ■ CBC ■ Ultrasound ○ Induction of labor greater than 34 weeks ○ 32 to 34 weeks risk/benefit analysis ○ Conservative, expectant management if less than 32 weeks ○ Home care as indicated 94 Hemolytic Disease in the Newborn – pg. 234 Erythroblastosis Fetalis ● Rh negative mom has Rh positive partner, so makes Rh antibodies that destroy fetal RBC ● Causes spleen and liver enlargement ● Decreased colloid osmotic pressure which causes third spacing ● Goal: transfusion in utero to prevent if needed or delivery ABO incompatibility ● Mother is O blood group ○ No antigens ■ Will not spark antibody response ○ Anti A and B antibodies ● Fetus/newborn ○ Has blood group A (more prevalent) or group B ● Check for first pregnancy ● Does not increase in severity ● Does not require intrauterine transfusion ● Protection from Rh disease Mothers who are O blood group ● Once they give birth, fetal cord is tested for 1. Blood group 2. Rh factor 3. Coomb’s test (direct) ● Positive coomb’s test indicates antibodies in baby’s blood from the mom ○ Pathological jaundice ○ Can cause permanent brain damage if not treated for increased bilirubin levels (unconjugated) ○ Get it bound to protein to be excreted through urine and stool ● Treatment ○ Feed for protein ○ Stool normally ○ Phototherapy Hemolytic disease – pg.236 ● Occurs when there is hemolysis of fetal RBC by antibodies coming from the mother’s blood as the result of maternal sensitization ○ Try to prevent sensitization ● Definition: a primary disorder of fetus/neonate caused by maternal sensitization to fetal red blood cell antigens ● Occurs with the inheritance by baby of a RBC antigen from father, not present in mother 95 ● Risk ○ ○ ○ ○ ○ ○ Rh negative mother, Rh positive father, baby is Rh positive 50% risk Worry about mom and baby, not dad Amniocentesis Incorrect blood transfusion Rupture of blood vessels Maternal sensitization ● Mother who is Rh negative is exposed to Rh positive blood and perceived as a foreign substance and responds by making antibodies which are permanent Ways mother becomes sensitized ● Transfusion with Rh positive blood ● Placental separation ● Transplacental hemorrhages ● Spontaneous abortion ● Amniocentesis ● Previous pregnancy Prenatal management ● Identify Rh negative mothers at first prenatal ● Determine if sensitization has occurred ○ Indirect Coombs test ■ Negative: does not have Rh antibodies Coombs test ● An antibody titer which looks for the presence of antibodies ● Desired test result: negative (no antibodies made) Negative Coombs – pg. 240 Do nothing until 28 weeks gestation (7 months) Repeat Coombs at 28 weeks, if negative: o Give expectant mother Rhogam At birth, test baby’s blood for: o Blood type o Rh factor o Coombs test (antibodies) Baby’s blood test: -- pg. 240 IF baby has: o Rh POSITIVE blood o No antibodies from mother (negative direct Coombs) Then: o Mother is administered Rhogam (within 72 hours of birth) 96 Prevent mother (who has just been exposed to babies blood) from making antibodies – PREVENTION It’s just for future pregnancies Even if we don’t have babies blood type Can also happen with amniocentesis Given even if a miscarriage occurs Criteria for Rhogam Admin after childbirth: NEWBORN is RH+ Direct Coombs (on fetal cord/baby’s blood) is NEGATIVE Baby’s blood test (cont’d): -- pg. 241 IF baby has: o Rh NEGATIVE blood o NEGATIVE Coombs (no antibodies in blood) Then: o Mother does NOT receive Rhogam Sequence: -- pg. 241 1st prenatal visit o Mother’s blood type and Rh, and Coombs 28 weeks o Repeat Coombs Birth of baby o Baby’s blood type and Rh, and Coombs On basis of baby’s blood tests, Rhogam is administered to the mother or not. Prevention of Hemolytic Disease from Rh Incompatibility Blood type + Rh + Indirect Coombs (antibody titer) If Maternal Sensitization has occurred = POSITIVE indirect coombs test – pg. 242 Indirect Coombs is repeated until level reaches a critical value o Serial assessment of fetal anemia via access to the fetal middle cerebral artery Sensitization o Antibody titer: 1:8 to 1:16 Hemolytic Disease in the Neonate (Hemolytic Anemia) – pg. 243 (See PICTURE on slide) Goal of Nursing for Infants with Hyperbilirubinemia PREVENT KERNITERUS o Encephalopathy caused by deposit of lipid-soluble, unconjugated, unbound to protein into the brain cells o Assess level – transcutaneous bilirubin on skin of baby’s chest 97 o o o Baby’s age and hours 20mg/dl – Term 15mg/dl – Preterm Need to be eating and stooling May order phototherapy to decrease excess S/S of Kerniterus o Lethargy o Hyporeflexia o Hypotonia o Seizure (sometimes) Nursing Care with Phototherapy Protect infant’s eyes Prevent hypothermia Prevent respiratory distress Avoid hypoalbuminemia Prevent sepsis Support feedings, hydration, and elimination Support adequate protein and calorie intake Wallaby Blanket 98 PAGE 240-246 PAGE 271-280 Vaginal Ecosystem Good bacteria vs. bad bacteria ● Lactobacilli ○ Good bacteria ○ Healthy acidic pH ○ Vaginal mucosa intact ○ Protects vaginal epithelial wall ● Anaerobes ○ Bad bacteria ○ pH altered ○ Fungus and parasites proliferate ○ Vaginal mucosa disrupted ○ Epithelial wall damaged or inflamed ○ Greater risk for other STIs Maintaining a healthy ecosystem ● Mild soap without fragrances or colors ● Rinse well with warm water ● Avoid bubble baths, douching, feminine washes or wipes ● Shaving causes microscopic routes of entry for infectious agents ● Use a hair dryer to dry the skin after bathing ● Avoid layers of tight clothing ● Cotton underwear ○ Allows oxygen to get in Ectopic Pregnancy ● Definition: implantation of blastocyst in a site other than in the endometrial lining ○ Tubal: 90%, most common ■ Stuck and grows in the fallopian tube ■ Recognize before it becomes hemorrhagic ● Incidence: 1% to 2% of first trimester pregnancies in the US ○ 6% maternal mortality ○ Leading cause of infertility ● Risk factors ○ History of STDs ■ Chlamydia ■ Gonorrhea ■ Can be asymptomatic to females ■ Spreads to uterus and fallopian tubes and causes inflammation ○ History of PID ■ Pelvic inflammatory disease 99 ○ ○ ● ● History of previous ectopic pregnancy IUD use ■ Can cause inflammatory response ○ Smoking ■ Unfavorable environment Clinical signs ○ Amenorrhea ○ Breast tenderness ○ Nausea and vomiting ○ Most common: abdominal pain, delayed menses, and abnormal vaginal bleeding ○ With rupture: sharp one sided pain, low abdominal pain, vaginal bleeding, syncope, referred shoulder pain, adnexal tenderness ○ 6 to 12 weeks before rupture if narrow part or 16 weeks if in larger part Clinical management ○ Surgical management: removal, if narrow preserve ovaries ■ Tuboplasty to enable patency ○ Medical management: methotrexate, anti folic acid that destroys rapidly dividing cells 100