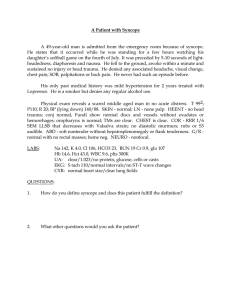
• • • • • The Heart • The heart does not rest for more than a fraction of a second at a time. During a lifetime, it contracts more than 4 billion times. To support this active state, the coronary arteries supply more than 10 million liters of blood to the myocardium and more than 200 million liters to the systemic circulation. Cardiac output can vary under physiologic conditions from 3 to 30 L/min, and regional blood flow can vary by 200%. This wide range occurs without any loss of efficiency in the normal state. The major heart disease Symptoms of cardiac disease coronary heart disease, hypertension, rheumatic heart disease, bacterial endocarditis, congenital heart disease. • Chest pain • Palpitations • Dyspnea • Syncope • Fatigue • Dependent edema • Hemoptysis Chest pain. Questions. • • • • • • • "Where is the pain?" "How long have you had the pain?" "Do you have recurrent episodes of pain?" "What is the duration of the pain?" "How often do you get the pain?" "What do you do to make it better?“ "What makes the pain worse? breathing? lying flat? moving your arms or neck?" Chest pain. Questions. • "How would you describe the pain? burning? pressing? crushing? dull? aching? throbbing? knife-like? sharp? constricting? sticking?" • "Does the pain occur at rest? with exertion? after eating? when moving your arms? with emotional strain? while sleeping? " • "Is the pain associated with shortness of breath? palpitations? nausea or vomiting? coughing? fever? coughing up blood? leg pain?" Angina pectoris • Angina pectoris literally means a strangling sensation (angina) in the chest (pectoris). It is a gripping or crushing central chest pain (or discomfort) that may be felt around the whole chest or deep within the chest. The pain may radiate into the neck or jaw and, rarely, into the teeth, back or abdomen. It is associated with heaviness, paraesthesia or pain in one (usually the left) or both arms. It is typically provoked by exercise and is promptly relieved by rest. Angina pectoris • Angina pectoris is the true symptom of CHD. Angina is commonly the consequence of hypoxia of the myocardium resulting from an imbalance of coronary supply and myocardial demand. Angina pectoris • Angina of increasing frequency, or coming on at rest or unpredictably is called unstable (or crescendo) angina. A pain of similar distribution and type also occurs at rest in myocardial infarction. The mechanism of the pain is myocardial hypoxia secondary to inadequate coronary blood flow. Levine's sign • Commonly, a patient may describe the angina by clenching the fist and placing it over the sternum. This is a pathognomonic sign of angina commonly referred to as Levine's sign. Palpitations • Palpitations are the uncomfortable sensations in the chest associated with a range of arrhythmias. Patients may describe palpitations as "fluttering," "skipped beats," "pounding," "jumping," "stopping or "irregularity." The normal heartbeat is sensed when the patient is anxious, excited, exercising, or lying on the left side. Palpitations • The most common arrhythmias felt as palpitations are premature ectopic beats and paroxysmal tachycardias. Determine whether the patient has had similar episodes and what was done to extinguish them. Palpitations are common and do not necessarily indicate serious heart disease. Any condition in which there is an increased stroke volume, as in aortic regurgitation, may be associated with a sensation of "forceful contraction." Palpitations • "How long have you had palpitations?" • "Do you have recurrent attacks?" If so, "How frequently do they occur?" • "When did the current attack begin?" • "How long did it last?" • "What did it feel like?" • "Did any maneuvers or positions stop it?" • "Did it stop abruptly?" Palpitations Palpitations • "Could you count your pulse during the attack?" • "Can you tap out on the table what the rhythm was like?" • "Have you noticed palpitations on exertion? • while lying on your left side? after a meal? when tired?" • "During the palpitations, have you ever fainted? had chest pain?" • "Was there an associated flush, headache, or sweating associated with the palpitations?" In addition to primary cardiovascular causes • thyrotoxicosis, • hypoglycemia, • fever, • anemia, • pheochromocytoma, • and anxiety states are commonly associated with palpitations. Dyspnea • Dyspnea is an abnormal awareness of breathlessness, and can be due to cardiac or respiratory causes. • Patients report that they have "shortness of breath" or that they "can't get enough air." It occurs on exertion or may be present at rest. Example "The patient has had 1-block DOE (Dyspnea on exertion) for the past 6 months. Before 6 months ago, the patient was able to walk 4 blocks without becoming short of breath.” Dyspnea • Left ventricular failure causes dyspnea because of a rise of pressure in the left atrium and pulmonary capillaries leading to interstitial and alveolar edema. This makes the lungs stiff (less compliant), which increases the amount of respiratory effort necessary to breathe. Usually a fast breathing rate (tachypnoea) is also present owing to stimulation of the pulmonary stretch receptors. Orthopnea Orthopnea is a form of breathlessness that occurs when the patient lies flat, and occurs because lying flat results in redistribution of blood, leading to an increased central and pulmonary blood volume. Orthopnea • Patients usually cope with orthopnea by propping themselves up with pillows. Inquire of all patients, "How many pillows do you need in order to sleep?" To help quantify the orthopnea, you can state, for example, "3-pillow orthopnea for the past 4 months." Paroxysmal nocturnal dyspnea • Paroxysmal nocturnal dyspnea (PND) occurs when there is an accumulation of fluid in the lungs (pulmonary edema) at night. • The patient is woken from sleep fighting for breath, a dramatic and frightening experience. Paroxysmal nocturnal dyspnea Syncope • Sitting on the side of the bed or getting up may relieve the breathlessness. Sometimes the patient will get up and open a window to gasp for fresh air. Wheezing, due to bronchial endothelial edema, is common (cardiac asthma), and a cough, often productive of frothy or blood-tinged sputum, usually occurs. Initially these episodes terminate spontaneously. • Fainting, or syncope, is the transient loss of consciousness that is due to inadequate cerebral perfusion. Ask patients what they mean by "fainting" or "dizziness." Syncope may be related to cardiac as well as noncardiac causes. Syncope • "What were you doing just before you fainted?" • "Have you had recurrent fainting spells?" If so, "How often do you have these attacks?" • "Was there an abrupt onset to the fainting?" • "Did you lose consciousness?" Syncope • "In what position were you when you fainted?" • "Was the fainting preceded by any other symptom? nausea? chest pain? palpitations? confusion? hunger?" • "Did you have any warning that you were going to faint?" • "Did you have any black, tarry bowel movements after the faint?" Syncope Syncope • The activity that preceded the syncope is important because some cardiac causes are associated with syncope during exercise (e.g., valvular aortic stenosis, idiopathic hypertrophic subaortic stenosis, and primary pulmonary hypertension). If a patient describes palpitations before the syncope, an arrhythmogenic cause may be present. Cardiac output may be reduced by arrhythmias or obstructive lesions. • The position of the patient just before fainting is important because this information may help determine the cause of the syncope. For example, if a patient fainted after rising suddenly from bed in the middle of the night to run to answer the telephone, orthostatic hypotension may be the cause. Orthostatic hypotension is a common form of postural syncope and is the result of a peripheral autonomic limitation. Syncope Micturition syncope • There is a sudden fall in systemic blood pressure resulting from a failure of adaptive reflexes to compensate for an erect posture. Symptoms due to orthostatic hypotension include dizziness, blurring of vision, profound weakness, and syncope. Many drugs can cause orthostatic hypotension by leading to changes in intravascular volume or tone. The geriatric patient is most prone to orthostatic hypotension. • Micturition syncope usually occurs in men during straining with nocturnal urination. It may occur after considerable alcohol consumption. Vasovagal syncope Vasovagal syncope • Vasovagal syncope is the most common type of fainting and is one of the most difficult to manage. It has been estimated that 40% of all syncopal events are vasovagal in nature. Vasovagal syncope occurs during periods of sudden, stressful or painful experiences, such as receiving bad news, surgical manipulation, trauma, the loss of blood, or even the sight of blood. • It is often preceded by pallor, nausea, weakness, blurred vision, lightheadedness, perspiration, yawning, diaphoresis, hyperventilation, epigastric discomfort, or a "sinking feeling." There is a sudden fall in systemic vascular resistance without a compensatory increase in cardiac output as a result of an increased vagotonia. If the patient sits or lies down promptly, frank syncope can be aborted. Carotid sinus syncope Post-tussive syncope • Carotid sinus syncope is associated with a hypersensitive carotid sinus and is seen more commonly in the aged population. Whenever a patient with carotid sinus syncope wears a tight shirt collar or turns the neck in a certain way, there is an increased stimulation of the carotid sinus. This causes a sudden fall in systemic pressure, and syncope results. Two types of carotid sinus hypersensitivity exist: a cardioinhibitory (bradycardia) type and a vasodepressor (hypotension without bradycardia) type. • Post-tussive syncope generally occurs in patients with chronic obstructive lung disease. Several mechanisms have been postulated to explain its occurrence. It is generally accepted that coughing produces an increase in intrathoracic pressure, which decreases venous return and decreases cardiac output. There may also be a rise in cerebrospinal fluid pressure, producing a decreased perfusion to the brain. Fatigue • Fatigue is a common symptom of decreased cardiac output. Patients with congestive heart failure and mitral valvular disease frequently complain of fatigue. Fatigue, however, is not specific for cardiac problems. The most common causes of fatigue are anxiety and depression. Other conditions associated with fatigue include anemia and chronic diseases. The examiner must attempt to differentiate organic from psychogenic fatigue. • "How long have you been tired?" • "Was the onset abrupt?" • "Do you feel tired all day? in the morning? in the evening?" • "When do you feel least tired?" • "Do you feel more tired at home than at work?" • "Is the fatigue relieved by rest?" Dependent Edema • Swelling of the legs, a form of dependent edema, is a frequent complaint of patients. Heart failure results in salt and water retention. Retained fluid accumulates in the feet and ankles of ambulant patients and over the sacrum of bed-bound patients. The edema associated with heart failure becomes progressively worse during the day and is often absent on initial rising as the fluid is reabsorbed on lying down. When severe, the calf and thigh may become edematous and ascites or pleural effusion may develop. Dependent Edema • "What kind of medications are you taking?" • "Is there a history of kidney, heart, or liver disease?" • "Do you have shortness of breath?" If so, "Which came first, the edema or the shortness of breath?" • "Do you have pain in the legs?" • "Do you have any ulcers on your legs?" Hemoptysis • In addition to the pulmonary causes, mitral stenosis should not be forgotten as an important cause of hemoptysis. Rupture of the bronchial veins, which are under high back pressure in mitral stenosis, produces the hemoptysis. Dependent Edema • • • • "When was the swelling first noted?" "Are both legs swollen equally?" "Did the swelling appear suddenly?" "Is the swelling worse at any time of the day?" • "Does it disappear after a night's sleep?" • "Does elevation of your feet reduce the swelling?" Dependent Edema • The patient with congestive heart failure has symmetric edema of the lower extremities that worsens as the day progresses. It is least in the morning after sleeping with elevation of the legs in bed. If the patient also complains of dyspnea, it is helpful to determine which symptom came first. In patients with dyspnea and edema secondary to cardiac causes, the dyspnea usually precedes the edema. Bedridden patients may have dependent edema in the sacral area.