Airway
management in adults
MODERATOR- Dr. Mijanur Rahaman
SPEAKER- Dr. Payel Mitra
Nilratan Sircar Medical College and Hospital
introduction
Airway management refers to practice of establishing & securing a patent airway
Failure to secure a patent airway can result in hypoxic brain injury or death in few
minutes
Analysis of ASA “closed claims project” has shown that development of airway
emergencies increases odds of death or brain damage by 15 fold
Reports published in 2013, defines “difficult airways” as ‘the clinical situation in which a
conventionally trained anesthesiologist experiences difficulty with ventilation of upper
airway by mask,tracheal intubation or both’
Successful airway management requires a range of knowledge and skill sets
Difficult tracheal intubation accounts for 17% of the respiratory related injuries and
results in significant morbidity and mortality.
Estimated that up to 28% of all anaesthetic related deaths are secondary to the inability
to mask ventilate or intubate.
Prediction of the difficult airway allows time for proper selection of equipment,
technique and personnel experienced in difficult airways
Functional airway anatomy
Airway can be divided into:
1. Upper airway- nasal cavity, oral cavity, pharynx, larynx
2. Lower airway- tracheobronchial tree
NASAL CAVITY:
Airway begins functionally at naris(ext opening of nasal passages);
into right & left passages by nasal septum;
nasal cavity div
septal deviation commom in adult-So more potent side is preferred
for instrumation.
Lateral wall: 3 turbinates present form 3 meatus;
inf Meatus preferred pathway for nasal airway devices;
Roof- formed by cribriform plate & part ethmoid bone,
Fragile: if fracture result in communication b/w nasal & intracranial cavities.
Nasal mucosal lining highly vascular,apply vasoconstrictor topically before instrumentation to avoid
epistaxis.
Oral cavity
Oral cavity leads to oropharynx, inferiorly bounded by tongue, superiorly by hard & soft palate.
Tongue is attached to various structures by extrinsic muscles, imp is genioglossus-connects
tongue to mandible.
“Jaw thrust” maneuvar uses sliding component of TMJ to move mandible &attached tongue
anteriorly: relieving the airway obstruction by posterior displacement of tongue into
oropharynx.
PHARYNX
Muscular tube extend from base of skull to cricoid cartilage,
Connects nasal and oral cavities to larynx & esophagus;
Pharyngeal muscles in awake patients helps maintaining airway patency,loss of which is main
cause of obstruction. A “chin lift” increases longitudinal tension in muscles,counteracting the
tendency of airway to collapse.
Pharynx(contd.)
Pharynx divided into nasopharynx, oropharynx & hypopharynx
Nasopharynx-ends at soft palate, velopharynx is common site of
airway obstruction in both awake & anesthetized patients.
Oropharynx-begins at soft palate, inferiorly extends to epiglottis,
lateral wall contains palatoglossal(anterior) &
palatopharyngeal(posterior) folds-
which contain palatine tonsils: hypertrophy of
which causes airway obstruction.
Hypopharynx –begins at epiglottis & terminates
at level of cricoid cartilage where it is
continuous with esophagus.
larynx
Complex structure of cartilage,muscles & ligaments;
serves as a inlet to trachea; function- phonation & airway protection.
9 cartilaginous structures- thyroid,cricoid,paired arytenoid,
Corniculate & cuneiform cartilages & epiglottis.
Thyroid –largest; sup thyroid notch & laryngeal prominence
(Adam’s apple)landmark for percutaneous airway techniques &
laryngeal nerve block.
Cricoid cartilage(C6) is inferior limit of larynx, anteriorly
connected to thyroid by cricothyroid membrane (CTM);only complete cartilage ring
Space inferior to laryngeal inlet is laryngeal cavity,
ventricular folds(false vocal cords)-most superior structure of laryngeal cavity,
beneath is true vocal cords: space b/w vocal cords Is glottis,
part above glottis is vestibule, inferior- subglottis
Tracheobronchial tree
Trachea begins at C6 vertebra(cricoid cartilage) & extends
to level of carina(T5 vertebra)-length 10-15cm in adults.
Consists of 16-20 C-shaped cartilaginous structures that are
opened posteriorly & joined by fibroelastic tissue(trachealis
muscle forms posterior wall of trachea)
At carina, trachea bifurcates into right & left main bronchi.
In adults right main bronchi are more vertical angle,
resulting in greater chance of foreign bodies & ETT entering
right bronchus.
Upper aiway serves to warm & humidify air- bypassing via
ETT: essential to provide humidified air/gas for
spontaneous breath or mech ventilation.
Upper airway most vulnerable to obstruction- loss of tone
in anesthetised pt.
Lower airway serves to air conduction, gas
exchange,removal of foreign bodies.
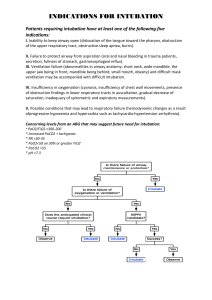
Pathology causing difficult airway
Lower airway
Upper airway
Facial anomalies- maxillary or mandibular
hypoplasia
TMJ-ankylosis,reduced movement due to
trauma
Anomalies of mouth-burns,trauma,Ludwig
angina.
Dentition-missing teeth,protruding teeth
Anomaly of nose-DNS,hypertrophic
turbinates,choanal atresia
Palate- cleft defects, arched palate
Pharynx-hypertrophic
tonsils,adenoid,tumors
Larynx- tumors, FB, stenosis, odema
Tracheal pathology- trachea esophageal
fistula, tracheal stenosis, trachea
malacia, FB
Bronchial pathology- mass in
mediastinum, FB, tumors.
Airway assessment
Airway assessment should start with direct patient history.
Previous easy airway history does not rule out possibility of
difficult ventilation & intubation.
Visual inspection-
prominent upper incisors, receding chin,edentulous
edema, blood, vomits, tumor, infection
short chin-to-larynx distance, bull neck, large tongue, small mouth
Dysmobity of TMJ and cervical spine = ‘stiff joint syndrome’
Large goiters,abcess, skin contractures,cervical spine instability
Massively obese or pregnant
Beards +/- tubes(Presence of beard associated with difficult ventilation due to difficulty in obtaining
mask seal)
Neck circumference >43cm(17 inches)- associated with difficult ventilation.
Assessment of cervical & atlanto occipital joint function-
Direct assessment: laryngoscopic view is easier if neck flexed on chest by 25˚-35˚,
a-o joint extend by 85˚.(sniffing /magill’s position)
Assess by asking patient to touch manubrium sterni with chin(neck flexion 25-30˚)
Ask to look at ceiling without raising eyebrows(a-o joint): reduction of extension
no reduction
one third reduction
two third reduction
complete reduction
2/3rd or complete reduction of extension is pointer of difficult rigid laryngoscopy.
Delikan test:- assess a-o joint extension
Prayer sign= inability to approximate palmer surface of phalangeal joints despite maximal
efforts in stiff joint syndrome of diabetes.
Mouth opening- difficulty:- ankylosing spondylitis,rheumatoid
arthritis,TMJ trauma, tumors, burns etc.
interincisor distance<3cm: difficult intubation.
Mallampatti classification I to III assigned based on visibility of
uvula,pillars & soft palate(pt upright,head neutral,mouth opened
tongue protruded,no phonation).
Modified mallampatti classification:
Class I:faucial pillars,uvula,soft palate visible
Class II: uvula,soft & hard palate visible
Class III: base of uvula,soft & hard palate visible
Class IV: hard palate only visible
A mallampatti zero classification has been proposed when
epiglottis can be visualized .
INTER-INCISOR DISTANCE
Inter-incisor distance with maximal mouth opening
Normal value > 5 cm / admits 3 fingers.
Significance :
Positive results: Easy insertion of a 3 cm deep flange of the laryngoscope blade
< 3 cm: difficult laryngoscopy
< 2 cm: difficult LMA insertion
Affected by TMJ and upper cervical spine mobility
UPPER LIP BITE TEST(CATCH TEST)
Class I:
Lower incisors can bite the upper lip above vermilion line
Class II:
can bite the upper lip below vermilion line
Class III:
cannot bite the upper lip
Significance
Assessment of mandibular movement and dental architecture
Difficult ventilation
The inability of a trained anesthetist to maintain the oxygen saturation > 90% using a
face mask for ventilation and 100% inspired oxygen, provided that the pre-ventilation
oxygen saturation level was within the normal range.
DIFFICULT INTUBATION
Proper insertion of tracheal tube with conventional laryngoscopy requires
More than 3 attempts
Longer than 10min
Failure of best attempt
Airway assessment(contd.)
Poor dentition & loose teeth increases the risk of dental trauma & teeth dislodgement
with subsequent aspiration; cosmetic dental work such as caps,crowns are liable to
damage; edentulous is easy intubation but potential difficult ventilation.
Ideal position for DL-cervical flexion & atlantooccipital extension; ‘sniffing position’.
Assessment of neck mobilty- sternomental (distance between
sternal notch & point of chin with head full extension &
mouth closed) < 12.5 associated with difficult intubation.
Assessment of submandibular space- thyromental distance
(from thyroid notch to lower border of mentum) <6.5(3 finger’s
breadth) associated with difficult intubation.
Assessment of mandibular prognathism- inability to protrude lower incisors
beyond upper indicative of difficult laryngoscopy; upper lip bite test(ULBT)
‘SAVVA TEST’
Predictors of difficulty to face mask ventilate
(OBESE/MOANS)
The Obese (body mass index > 26 kg/m2)
The Bearded
The Elderly (older than 55 y)
The Snorers
The Edentulous
(=BONES)
Mask seal difficult due to receding mandible,syndromes with facial abnormalities,burn
stricture etc.
Obesity, upper airway Obstruction
Advanced age
No teeth
Snorer
Lemon law
5 simple reproducible,rapid assessment methods
Look for anatomic features suggesting difficulty
Examine airway anatomy:- 3-3-2
oral opening 3 fingers
ability of mandlible to accommodate tongue 3 fingers b/w mentum & hyoid
assess high larynx-2 fingers b/w thyroid & mandlible
Mallampati grade
Obstruction of airway
Neck mobility
Ali magboul’s 4 M’s
Assess difficult airway:- 4 M’s
Mallampati
Measurement
Movement
Malformation & STOP
skull =(hydro or micro cephalus)
teeth=(protruded or loose teeth)
obstruction=(obesity,bull neck,swellings)
pathology=(craniofacial anomalies)
Physiologic concept for airway management
PREOXYGENATION: Hypoxemia quickly develops with the induction of anesthesia due to
hypoventilation; decrease in functional residual capacity owing to supine position,
muscle paralysis & direct effects of anesthetic drugs.
It is a process of replacing nitrogen in the lungs with oxygen; provides an increase in
length of time before haemoglobin desaturaion occurs in apnea patient(apnea time).
Adequate preoxygenation is essential when mask ventilation or,intubation is
anticipated to be difficult(increases the safety margin).
Performed via facemask attached to anesthesia machine,100% o2 given at a flow rate high
enough to prevent rebreathing(10-12litr/min) & no leaks,head-up position.
2 primary methods- 1. uses tidal vol. ventilation through facemask for 3 minutes,allows
gas exchange of 95% in lungs ;
2. uses vital capacity breaths to reach adequate preoxygenation(8
breaths over 60secs)
Pulmonary aspiration of gastric contents:
Patients who are scheduled for elective procedures requiring sedation, regional & general
anesthesia were instructed to remain NPO after midnight to reduce risk of regurgitation.
ASA 1999 guidelines, recommend clear liquids upto 2 hrs prior to elective ot is allowed.
ASA 2011 guidelines, recommend 4hrs of fasting from breast milk & 6hrs of fasting from solid
food,infant formula & nonhuman milk.
Routine use of drugs as prophylaxis for aspiration pneumonitis is not recommended by ASA;
specific risk factors such as full stomach, symptomatic GERD,hiatus hernia,nasogastric
tube,obese,diabetic gastroparesis or pregnancy.
Goal of aspiration prophylaxis-2 fold-decrease gastric vol & increase gastric pH
Uses antacids(eg bicitra),promotility drugs(eg. Metoclopromide), H2 receptor
antagonist
Airway reflexes & response to intubation:
Reflex is triggered by sensory receptors in glottic & subglottic mucosa & result in strong
adduction of vocal cords.
An exaggerated response leads to laryngospasm;a potential complication of airway
management. Laryngospasm is provoked by glossopharyngeal or vagal stimulation
attributable to airway instrumentation & vocal cord irritation,in light plane of
anesthesia(stage II of guedel classification).
Treatment – removal of airway irritants,deepen plane of anesthesia, administer NMBAs
such as succinylcholine, continuous positive airway pressure with 100% o2,
bilateral pressure between condyle of mandible & mastoid process.
Tracheobronchial tree possess reflexes to protect lungs from noxious stimuli;lower airway
irritation leads to constriction of bronchial smooth muscle resulting in bronchospasm.
Treatment – deepen plane of anesthsia with Propofol or volatile agent,beta 2 agonist or
anticholinergic drugs, iv lidocaine
Airway management after induction of general anesthesia
Standard iv induction with NMBAs m/c technique,muscle relaxation achieved by NMBD improves
intubating conditions by preventing reflex laryngeal cough & closure after intubation.
m/c iv induction drug is Propofol,followed by etomidate,ketamine,thiopentone & midazolam. (choice
of drugs depends on pt hemodynamic status,comorbidities,allergies,pharmacokinetic effects,physician
preference.
Succinylcholine is m/c NMBD used for routine induction; but recent non depolarising NMBD are
preferred owing to side effects of succinylcholine-bradycardia, hyperkalemia,myalgia,increased
intracranial pressure; benefit is rapid onset& short duration of action(desired in suspected difficult
airway)
Non depolarising NMBD most frequently used-rocuronium,vecuronium,cis atracurium; limitation is
primarily long duration of action,so functional airway must be established first to avoid hypoxia.
Sugammadex –selective relaxant binding agent for rocuronium,ability to reverse profound NMB rapidly
NMBDs must be withheld till secure mask ventilation established,if ventilation by mask cannot be
achieved,pt can resume spontaneous ventilation or awaken.
Rapid sequence induction & intubation of trachea
Defined as administration of fixed dose of induction agent & short action muscle relaxant after
preoxygenation & intubation of trachea without superimposed assisted ventilation
It is a speciased method of commonly used when a frequent risk of gastric regurgitation & pulmonary
aspiration of gastric contents is present.
Method-adequate preoxygenation & cricoid pressure(sellick maneuvar) is applied,iv induction agent
given with 1-1.5mg/kg iv succinylcholine,trachea intubated without PPVs while cricoid pressure
applied.(10N when awake and 30N after LOC)
Goal-to achieve optimal intubating conditions rapidly to minimise length of time b/w loss of
consciousness(LOC) & securing airway with cuffed ETT.
RSII widely practiced in patients with full stomach & bowel obstruction,recommended for pregnant
patients,poorly controlled GERD,morbid obese,diabetic gastroparesis,difficult mask
ventilation,edentulous,bearded patients.
When succinylcholine is contraindicated,non depolarising NMBDs used(rocuronium 1-1.2mg/kg or
vecuronium 0.3mg/kg)
Modified RSII-use of mask ventilation in conjunction with cricoid pressure,indicated in patients with
risk of hypoxemia(obese,pregnant,critically ill,pediatric patients)
Inhalational induction of anesthesia
Common used in pediatric patients, maintainance of spontaneous ventilation, gradual
changes in depth of anesthesia & respiratory and CVS effects.
Sevoflurane is m/c used, due to lack of pungency & low blood gas solubility allowing
smooth induction.
Two methods- 1. tidal volume induction: patient breathe normally through face mask
2. vital capacity induction: patient exhale to residual volume and take vital capacity
breathe from facemask.(delivery concentration 8%); N2O can be used to speed up
effect due to second gas effect.
Halothane can also be used-but due to high blood gas co efficients, long induction
time. Also myocardial depression,halothane induced hepatitis.
Airway management in awake patient
Benefits of awake airway management-preservation of pharyngeal muscle
tone,patency of upper airway, maintainance of spontaneous ventillation,abilty to
obtain quick neurologiic examination,safeguard against aspiration.
Indications-risk of severe aspirations of gastric contents,facial trauma,severe
hemodynamic instability,cervical spine pathologic instability.
Most useful technique for awake intubation is flexible scope intubation(FSI); other
methods-video laryngoscopes,optical stylets,intubating LMAs,retrograde
intubation(RI).
Topicalization-lidocaine m/c local anesthetic(rapid onset & high therapeutic index).
Primarily focused on base of tongue(pressure receptors here act as gag
reflex),oropharynx,hypopharynx & laryngeal structures. If nasotracheal
intubation,nasal cavity should be topicalised.
Before topicalization- anticholinergic should be administered to dry
secretions;improving visualisation(glycopyrrolate preferred-less vagolytic effect than
atropine)
Topicalisation of larynx achieved by aspiration of local anesthetic or by spray-as-you-go
(SAYGO)method-intermittent injecting local anesthetics through suction port or working
channel of FSI.
Glossopharyngeal nerve supplies sensory innervation to posterior
third of tongue,vallecula,anterior surface of epiglottis, posterior &
lateral walls of pharynx & is the afferent pathway of gag reflex.
To block the nerve-tongue is displaced medially,forming a groove,
25G spinal needle is inserted at base of tongue,to a depth of 0.5cm.
After negative suction,2ml of 2% lidocaine is injected,the process is
repeated on contralateral side.
Superior laryngeal nerve,a branch of vagus,provides sensory input
From lower pharynx & upper part of larynx,including glottic surface
Of epiglottis & aryepiglottic folds.
Block of the nerve-using either the superior cornu of hyoid
or superior cornu of thyroid cartilage,25G spinal needle is
placed of the cornu anteriorly toward thyrohyoid ligament.
Resistance is felt as the needle is advance through ligament,
at a depth of 1-2cm. After negative suction,1.5-2ml of
2%lidocaine is injected & repeated in opposite side.
Third landmark-imp for obese patient,needle is inserted
2cm lateral to superior thyroid notch & directed posteriorly
and cephalad direction 1-1.5 cm depth,2ml lidocaine injected.
Translaryngeal block-
provides anesthesia to trachea & vocal cords, 20-22G needle attached to 5ml
syringe,directed posteriorly & caudially until air is aspirated,4ml of 2% or 4% lidocaine
injected quickly, patient to cough.
Drugs used for awake intubation
Mechanism
Ventilation via facemask
Use of facemask facilitate delivery of oxygen or anesthetic gas from
a breathing system to a patient by creating airtight seal with patients face.
Parts-body, seal/rim & connector with retaining hooks.
Rim of mask is contoured & fits to various facial features.
The seal is air filled,
High volume low pressure cushion.
Mask’s 22mm orifice attaches to breathing circuit of anesthesia
machine through right angled connector.
Transparent mask allows observation of exhaled humidified gas & immediate recognition
of vomitus.
Retaining hooks can be attached to head strap so that mask need not to be held in place
continually.
Effective ventilation requires tight fit mask & patent airway. Improper technique result in
deflation of anesthesia reservoir bag when the adjustable pressure limiting valve is
closed,due to leak around the mask.
Mask is held in left hand,right hand used to generate positive pressure ventilation by
sqeezing the breathing bag.
Contd.
Mask held against face by downward pressure with left thumb
& index finger.(C shape)
The middle & ring finger grasp mandible to facilitate
extension of atlanto oocipital joint.(finger pressure on bony mandible
& not on soft tissue)
Little finger placed under angle of jaw,used to thrust jaw anteriorly
(most imp method to allow ventilation.){E shape}
In difficult situations,two hands held to adequate jaw thrust & to creat mask seal.
Assistant required to sqeeze the bag.
Difficult to form adequate mask fit with cheeks of edentulous patients.
Positive pressure ventilation using mask should normaly be limited to 20cm of H2O to avoid
stomach inflation.
Long periods of mask ventilation may cause pressure injury to branches of trigeminal or facial
nerves.
Eyes should be taped shut to minimize the risk of corneal abrasion.
Mask ventilation is non invasive technique for airway manangement.
Primary mode of ventilation for anesthesia of short duration.
Administration of oxygen via facemask is common for
preoxygenation.
It is valuable rescue technique when tracheal intubation is difficult.
It is very imp in ASA “difficult airway algorithm”.
Contraindicated when risk of regurgitation is increased,no
protection against aspiration.
Oral/nasal AIRWAYS
Supraglottic airway devices
Used with both spontaneously & ventilated patients during anesthesia, employed when both
BMV & endotracheal intubation failed.
Blindly inserted into pharynx to provide a patent conduit for ventilation,oxygenation &
delivery of anesthetic drugs without need for tracheal intubation.
Advantages – 1. less invasive than endotracheal intubation
2.can be used for spontaneous ventilation or PPV.
3.ease & speed of placement.
4. improved hemodynamics
5. reduced anesthetic drug requirement
6. lack of need for muscle relaxant.
Disadvantages – smaller seal pressure than ETT,lead to
Ineffective ventilation, no protection from laryngospasm, little
Protection from gastric regurgitation.
LMA- one of the first SGAs,by Dr. Archie Brain,
introduced to clinical practice in1988
Laryngeal mask airway
LMA –wide bore tube, proximal end connects to
breathing circuit(15mm) connector,distal end attached
to a elliptical cuff which is inflated through a pilot tube.
Deflated cuff is lubricated on posterior surface,inserted blindly into
hypopharynx ,inflated with min effective volume of air(40-60cm H2O),
cuff forms a low pressure seal around larynx.
This requires anesthetic depth greater than oral airways.
Ideal position-cuff is bordered by base of tongue
superiorly,pyriform sinuses laterally,upper esophageal
sphincter inferiorly.
LMA partially protects larynx from pharyngeal
secretions(but not gastric); it should remain in place
until patient has regained airway reflexes(signalled
by coughing & mouth opening)
LMA contraindications
Pharyngeal pathology(abcess)
Pharyngeal obstruction
Full stomach(pregnancy,hiatal hernia)
Low pulmonary compliance(restrictive airway disease)
Variations of LMA:
Proseal LMA- permits passage of gastric tube to decompress
I-Gel LMA- uses gel occlude rather than inflated cuff
Fastrach intubation LMA- designed to facilitate endotracheal intubation
LMA Ctrach- incorporate camera to facilitate passage of ETT
Confimation of position- gentle PPV & check capnography,auscultation,quantifying the
inspiratory pressure at which leak is audible(18-20cm H2O).
Esophageal-tracheal combitube
Consists of two fused tubes,each with a 15mm connector
at the proximal end
Longer blue tube has occluded distal tip that forces gas
to exit through series of side perforations & shorter clear
tube has open tip with no perforation.
Inserted blindly,advanced two black rings on the shaft lies b/w upper & lower teeth.
2 inflatable cuffs-100ml proximal & 15 ml distal
KING LARYNGEAL TUBE
Consists of small esophageal balloon & a larger
balloon for placement in hypopharynx
(both inflate through one line)
Suction port distal to esophageal balloon is present
for decompression of stomach
TRACHEAL TUBES:
Endotracheal intubation
made from polyvinyl chloride, marked I.T or Z-79(indicates non-toxicity)
Shape & rigidity can be altered using stylet; patient end bevelled(visualisation);
Murphy eye(to decrease risk of occlusion)
TT size usually designated in millimetres of internal diameter(choice of size b/w
maximising flow with larger size & minimising trauma with smaller size)
Cuff inflation system consist of-valve, pilot balloon, inflating tube & cuff
Valve prevents air loss after cuff inflation. Balloon indicates cuff inflation.
Uncuffed tubes are used in infants & young children to minimise risk of pressure
injury & postintubation croup.
2 major types of cuff- 1. high pressure(low volume):- associated with more ischaemic
damage to tracheal mucosa(problem in long surgeries)
2. low pressure(high volume):- increase chances of sore
throat,aspiration,spontaneous extubation(preferred)
Variations of ETT:
Various special applications:-
Flexible, armoured tubes( to resist kinking & valuable in head & neck surgeries),
Microlaryngeal tubes, double lumen ETT(to facilitate lung isolation & one lung ventilation),
metal tubes designed for laser airway surgeries(to reduce fire hazards), preformed curve
tubes(nasal & oral intubation in head & neck surgeries)
laryngoscopes
Instrument to examine larynx & facilitate intubation of trachea.
PARTS-
handle containing batteries to light bulb on blade tip;
blades- Macintosh & Miller(curved & straight blade respectively)
Most commonly used technique for intubation is DL(Direct Laryngoscopy); involves direct
visualisation of glottis with assistance of laryngoscope.
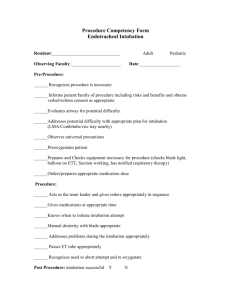
Direct laryngoscopy
PREPARATION & POSITIONING
Adequate preoxygenation,availability of equipments-laryngoscopes; tracheal tubes; stylets;
syringe for inflating cuff; a suction; mask ventilation; oxygen source; a skilled assistent (to
help with external laryngeal manipulation by BURP ie backward upward and rightward pressure
& stylet removal etc)
First attempt is the best attempt.
positioning
For successful DL; line of sight from mouth to larynx
should be achieved.
Alignment of three anatomical axis- oral,pharyngeal
& laryngeal.
Positioning in sniffing position approximates this alignment.
Cervical flexion aligns pharyngeal & laryngeal axis;
head extension at atlantooccipital joints brings oral
axis closer into alignment.
35 degree of cervical flexion(7-9cm elevation of head
on a firm cushion)
Obese patients often require elevation of shoulders & upper back to accomplish adequate
cervical flexion(achieved by ramped position)
Confirm horizontal alignment of EAM with sternal notch is useful for optimal head elevation in
both obese & non obese patients.
technique
Opening of mouth, inserting laryngoscope blade in right side,flange used to sweep
tongue to left,positioning of blade tip, applying a lifting force exposing the
glottis(force oriented at 45 degrees angle up using deltoid & triceps not by radial
flexion as it can cause dental damage),care to be taken not to impinge upper lips in
between laryngoscope, insert a tracheal tube in pen holding position with right hand
through the vocal cords into trachea.
Passage of ETT can be accomplished by shaping ETT with malleable stylet into
hockey stick shape(approx. 60 degree angle formed 4-5cm from distal end)
Whether to use a Macintosh or Miller blade is multifactorial; macintosh is used in
adults, Miller is used in pediatric patients.
Curved blades provide room for passage of ETT, straight blades are preferred in
patients with short thyromental distance & usually provide better view of glottis of
long & floppy epiglottis.
Miller blade inserted by paraglossal technique described by Henderson.(advanced
along paraglossal gutter & tongue,laryngoscope passed posterior to epiglottis.
Grade II can be further differentiated to IIA(partial view of glottis) & IIB (arytenoids or posterior
vocal cords only visible)
Intubation rarely difficult in grade I and IIA; IIB and III are difficult and have higher rates of
failed intubation; IV requires alternate method.
POGO scale- alternate method of grading laryngoscopic view; percentage of vocal cords from
anterior commissure to arytenoid notch that is visualised.
Inadequate laryngeal view- VERIFY
Optimal position
Ext laryngeal manipulation provided
Proper insertion of scope
Proper size of laryngoscope(larger or alternate blade)
ETT cannot be passed:-
Attempt at blind passage(which risk trauma,bleeding,airway obstruction)
Use of intubating stylet
Difficult airway algorithm
Nasotracheal intubation technique
Indications- oral tumours, faciomaxillary surgeries,difficult oral intubation etc
Technique-patent nare selected,nasal mucosal vasoconstrictor applied,nasal ETT lubricated,
inserted with bevelled end facing away from midline to decerase avulsion of turbinates, ETT in
oropharynx use DL method, ETT is guided in larynx inlet with help of Magill forceps.
CONFIRMATION OF ETT PLACEMENT
ETT cuff adequately inflated, ETT fixed in placed
with tape to facial skin(maxilla preferred)
Patient manually ventilated-chest rise,visible condensation in tube
Breath sounds bilaterally equal
Appropriate compliance of reservoir bag
Most important & definite indicator of endotracheal intubation is
normal Capnogram
Endo bronchial intubation-
Hypoxemia, asymmetric chest rise, absence of breath sounds over one lung,
increased airway pressure.
DIFFICULT AIRWAY ALGORITHM
Flexible fibreoptic bronchoscope
Most common indirect laryngoscopy device.
Technique of choice:- difficult airway,unstable neck extension
like cervical spine fractures,increased dental
Injury risk,limited mouth opening like poor range of
temporomandibular joint motion & facial burns,
Congenital & acquired upper airway abnormality.
• Allows indirect visualisation of larynx,in cases where awake
intubation is planned.
• Bronchoscopes are constructed of coated glass fibres that
transmit light & images by internal reflection.
The insertion tube contains 2 bundle of fibres, each containing of 10000 & 15000 fibres.
One bundle transmit light from light source which is either external to device or
contained in handle; other provides high resolution image.
Directional manipulation of insertion tube done by angulation wires.
Aspiration channels allows suctioning of secretions, insufflation of oxygen, instillation
of local anesthetics.( if not properly cleaned serves as nidus for infection).
FLEXIBLE FIBREOPTIC INTUBATION
Awake FOI: predicted inability to ventilate by mask, upper airway obstruction.
Asleep FOI: failed intubation, desire for minimal C spine movement.
Oral FOI: facial, skull injuries.
Nasal FOI: a poor mouth opening.
Technique:-
Patients should be informed for awake intubation as part of informed consent
process.
Airway is anesthetised with local anesthetic spray(dexmedetomidine has advantage in
preserving respiration while providing sedation).
If nasal FOI is planned, nostrils prepared with vasoconstrictive drops; o2 is insufflated
through suction port of FOB to improve oxygenation & blow secretions away from
nose.
Lubricated shaft of FOB is introduced through TT lumen. As it passes through the
distal end of TT,epiglottis is visible,then passed through abducted cords. FOB then
inserted within sight of carina.
Presence of tracheal rings & carina is proof of proper positioning.
TT is pushed of FOB- proper position confirmed by viewing tip of tube at appropriate
distance from carina.
Video laryngoscopy
Their use standard not only for difficult airways but also for
routine airways.
Has shown to improve glottic visualization compared with
DL.
Intubation success rates 94% as a rescue modality after
failed DL.
Divided into 3 groups- (1) design based on Mac Intosh
blades
blade
(2) highly curved/distally angulated
(3) incorporate an ETT guided channel
Macintosh blade type include C-Mac laryngoscope
associated with shorter intubation time & greater ease of
use.
Highly curved blade permit ‘look around the
corner’;provides improved laryngoscopic view without
manipulation of cervical spine. Eg Glidescope.
Airtraq – VL with highly curved blades having integrated
tube guiding channels to facilitate intubation.
SURGICAL AIRWAY TECHNIQUES
Invasive airways required when “can’t intubate, can’t ventilate”.
Options- surgical cricothyrotomy,needle cricothyrotomy, transtracheal catheter with jet
ventilation, retrograde intubation.
Surgical cricothyrotomy- surgical incision on CTM & placement of breathing tube.
Needle or catheter cricothyrotomy- horizontal incision made on CTM, seldinger
catheter/wire/dilator attached to a syringe is inserted across CTM, air is aspirated &
guidewire is passed through the catheter into trachea, dilator then passed over the
guidewire & breathing tube is inserted.
Transtracheal catheter with jet ventilation- 16 – 14G iv canula is attached to syringe &
passed though CTM toward carina, air is aspirated, jet ventilation is attached, catheter
must be secured( else it will cause subcutaneous emphysema).
Retrograde intubation- wire passed via catheter in CTM cephalad direction & emerges
through nose or mouth,distal end secured to prevent passing from CTM, then ETT maybe
passed over catheter into trachea.
Problems following intubation
Intubation require immediate attention- MUST confirm that tube is correctly
placed, with bilateral ventilation.
Gold standard remains detection of end tidal CO2.
Decrease in oxygen saturation- endobronchial intubation, inadequate oxygen
delivery.
When saturation declines- auscultate to confirm bilateral tube placement,
breathing circuit is checked.
Sudden end tidal CO2 decrease- decline in cardiac output,leak in circuit, pulmonary
or venous air embolism.
Rising end tidal CO2- hypoventilation, malignant hyperthermia,sepsis,breathing
circuit malfunction.
Increase airway pressure- obstructed or kinked ETT,reduced pulmonary compliance.
Low airway pressure- leaks in breathing circuit or sudden extubation.
CAPNOGRAM – graphic
representation of partial pressure
of carbon dioxide over time.
Techniques of extubation
Extubation performed when patient either deeply anesthetised or awake.(risk
benefit,Bailey maneuver-exchanging ETT with SGA)
Adequate recovery from NMBA should be ensured prior to extubation.
Extubation in light plane of anesthesia increases risk of laryngospasm.
Hemodynamic stability, normotherapy, adequate analgesia.
100% O2 at high flow rate
Remove secretion of trachea or pharynx.
Turn patient to lateral side-to prevent pulmonary aspiration
Standard position-sniffing, head up in obese
Deflate cuff & remove tube during inspiration.
Continue 100% O2 by facemask.
Complication of extubation
Complications of laryngoscopy & intubation
THANK YOU