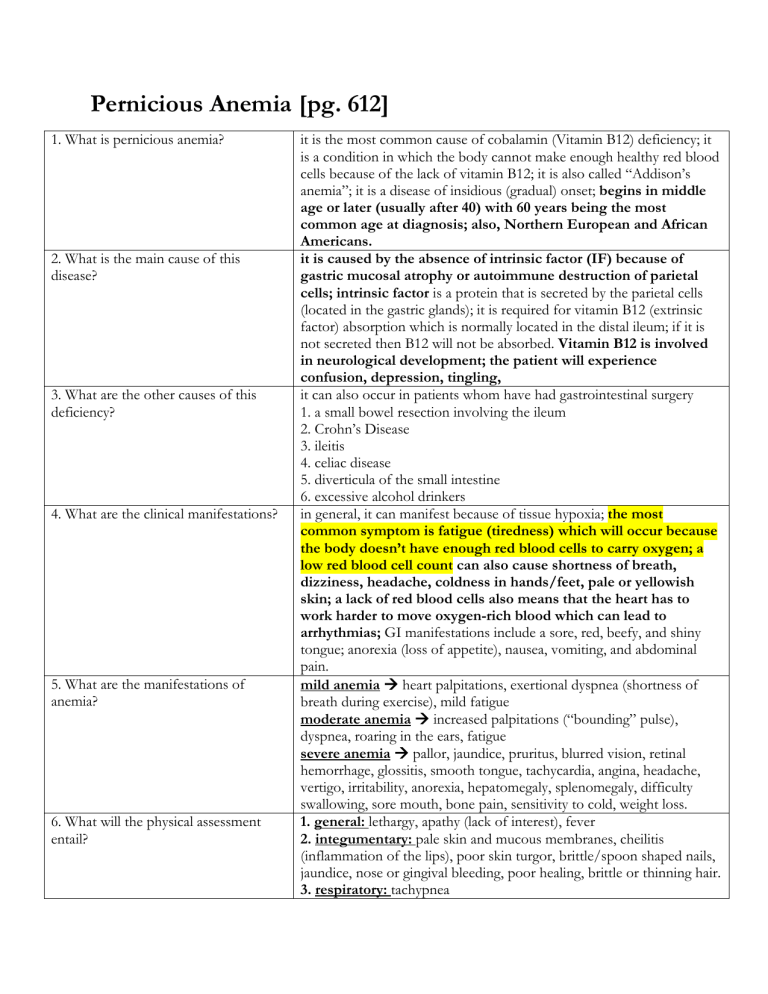
Pernicious Anemia [pg. 612] 1. What is pernicious anemia? 2. What is the main cause of this disease? 3. What are the other causes of this deficiency? 4. What are the clinical manifestations? 5. What are the manifestations of anemia? 6. What will the physical assessment entail? it is the most common cause of cobalamin (Vitamin B12) deficiency; it is a condition in which the body cannot make enough healthy red blood cells because of the lack of vitamin B12; it is also called “Addison’s anemia”; it is a disease of insidious (gradual) onset; begins in middle age or later (usually after 40) with 60 years being the most common age at diagnosis; also, Northern European and African Americans. it is caused by the absence of intrinsic factor (IF) because of gastric mucosal atrophy or autoimmune destruction of parietal cells; intrinsic factor is a protein that is secreted by the parietal cells (located in the gastric glands); it is required for vitamin B12 (extrinsic factor) absorption which is normally located in the distal ileum; if it is not secreted then B12 will not be absorbed. Vitamin B12 is involved in neurological development; the patient will experience confusion, depression, tingling, it can also occur in patients whom have had gastrointestinal surgery 1. a small bowel resection involving the ileum 2. Crohn’s Disease 3. ileitis 4. celiac disease 5. diverticula of the small intestine 6. excessive alcohol drinkers in general, it can manifest because of tissue hypoxia; the most common symptom is fatigue (tiredness) which will occur because the body doesn’t have enough red blood cells to carry oxygen; a low red blood cell count can also cause shortness of breath, dizziness, headache, coldness in hands/feet, pale or yellowish skin; a lack of red blood cells also means that the heart has to work harder to move oxygen-rich blood which can lead to arrhythmias; GI manifestations include a sore, red, beefy, and shiny tongue; anorexia (loss of appetite), nausea, vomiting, and abdominal pain. mild anemia heart palpitations, exertional dyspnea (shortness of breath during exercise), mild fatigue moderate anemia increased palpitations (“bounding” pulse), dyspnea, roaring in the ears, fatigue severe anemia pallor, jaundice, pruritus, blurred vision, retinal hemorrhage, glossitis, smooth tongue, tachycardia, angina, headache, vertigo, irritability, anorexia, hepatomegaly, splenomegaly, difficulty swallowing, sore mouth, bone pain, sensitivity to cold, weight loss. 1. general: lethargy, apathy (lack of interest), fever 2. integumentary: pale skin and mucous membranes, cheilitis (inflammation of the lips), poor skin turgor, brittle/spoon shaped nails, jaundice, nose or gingival bleeding, poor healing, brittle or thinning hair. 3. respiratory: tachypnea 7. What are the diagnostic studies? 8. What is the nutritional therapy? 9. What are nursing diagnosis associated with anemia? 10. What are the goals for patients with this disease? 11. What is the interprofessional care of pernicious anemia? 4. cardiovascular: tachycardia, dysrhythmias, postural hypotension, bruits (specifically carotid), intermittent claudication (cramping pain in the legs), ankle edema 5. gastrointestinal: glossitis, beefy red tongue, stomatitis, abdominal distention, anorexia 6. neurologic: headache, roaring in the ears, confusion, ataxia (balance) the RBC’s appear large (macrocytic) and have abnormal shapes; this structure contributes to erythrocyte destruction because the cell membrane is fragile. a serum test for anti-intrinsic factor antibodies may be done that is specific for pernicious anemia. ↓ Hemoglobin/ Hematocrit ↑ MCV (mean corpuscular volume) – measures the average red blood cell volume; the actual size of the cells ↓ Reticulocytes (new red blood cells in the body) ↑ serum iron ↑ Transferrin (main protein that blinds blood to iron) ↑ Ferritin (blood cell protein that contains iron) ↑ Bilirubin ↓ serum B12 red meats, especially liver, eggs, enriched grain products, milk, dairy, fish 1. fatigue related to inadequate oxygenation of the blood 2. imbalanced nutrition less than body requirements related to inadequate nutritional intake and anorexia 3. ineffective health management related to lack of knowledge about appropriate nutrition and medication regimen. the overall goals are that the patient with anemia will 1) assume normal activities of daily living; 2) maintain adequate nutrition; 3) develop no complications related to anemia instruct the patient on adequate dietary intake to maintain good nutrition; parenteral vitamin B12 or intranasal cyanocobalamin is the treatment of choice (without cobalamin administration these individuals will die in 1 to 3 years) a typical treatment schedule consists of 1000 mcg/day of cobalamin IM for 2 weeks and then weekly until the hemoglobin is normal, then monthly for life. Nausea and Vomiting [pg. 893-896] 1. What is nausea and vomiting defined? 2. When does it occur? 3. How does vomiting control center work? 4. What is the process of vomiting? 5. What is the chemoreceptor trigger zone (CTZ)? 6. What are the differences of regurgitation and projectile vomiting? 7. What are the clinical manifestations? 8. What does the characteristics of vomit indicate? these are the most common manifestations of GI disease which can occur independently and can be closely related which can be treated as one problem; nausea is the feeling of discomfort in the epigastrium with a conscious desire to vomit and vomiting is the forceful ejection of partially digested food and secretions (emesis) from the upper GI tract. it occurs in different situations 1. pregnancy 2. infection 3. central nervous system disorders (meningitis, tumor) 4. cardiovascular (myocardial infarction, heart failure) 5. metabolic disorders (diabetes mellitus 6. Addison’s disease 7. renal failure 8. postoperatively after general anesthesia 9. side effects of drugs the vomiting center in the medulla coordinates this action; this center receives input from various stimulus; the neural impulses reach the vomiting center via afferent pathways through branches of the autonomic nervous system; these pathways are located in the GI tract, heart, kidneys, and uterus; when it is stimulated these receptors relay information to the vomiting center which initiates the vomiting reflex. closure of the glottis deep inspiration with contraction of the diaphragm in the inspiratory position closure of the pylorus relaxation of the stomach and lower esophageal sphincter contraction of the abdominal muscles with increasing intraabdominal pressure it is an area in the medulla oblongata that receives input from bloodborne drugs or hormones, toxins, labyrinthine stimulation (motion sickness); communicates with other structures in the vomiting center to initiate vomiting; once stimulated the CTZ transmits impulses directly. regurgitation is an effortless process in which partially digested food slowly comes up from the stomach (material from the pharynx and esophagus). projectile vomiting is a forceful expulsion of stomach contents without nausea; it is a characteristic of CNS (brain and spinal cord) tumors. nausea is a subjective complaint; anorexia (lack of appetite) usually accompanies nausea; if nausea and vomiting occurs over a long period of time, dehydration can also develop rapidly (water and essential electrolytes are lost) which creates extracellular fluid volume loss, decreased plasma volume, and circulatory failure. metabolic alkalosis can result from loss of gastric hydrochloric acid. 1. emesis containing partially digested food several hours after the meal indicates gastric outlet obstruction or delayed gastric emptying. 2. presence of fecal odor suggests intestinal obstruction below level of the pylorus. 3. bile in the emesis indicates obstruction below the ampulla of Vater. 9. What does the color of vomit indicate? 10. What will the physical assessment entail? 11. What are the nursing diagnosis associated? 12. What are the nutritional therapy? 13. What are the goals for patients with nausea and vomiting? 14. What is the drug therapy for nausea and vomiting? 15. What is the nondrug therapy? 16. What is the interprofessional care for the acute care setting? bright red blood indicates active bleeding which can be due to a Mallory-Weiss tear is a condition marked by a tear in the mucous membrane or inner lining where the esophagus meets the stomach; it can cause serious bleeding. “coffee-ground” appearance is related to gastric bleeding; the blood changes to dark brown because of its interaction with HCL acid. 1. general survey: lethargy, sunken eyes 2. integumentary: pallor, dry mucous membranes, poor skin turgor 3. gastrointestinal: amount, frequency, character (projectile), content (undigested food, blood, bile, feces), and color of vomitus (red, “coffeeground”, green-yellow) 4. urinary: decreased output, concentrated urine 1. nausea related to multiple etiologies 2. deficient fluid volume related to prolonged vomiting 3. imbalanced nutrition less than body requirements related to nausea and vomiting. the patient that is severely vomiting will need IV fluid therapy with electrolyte and glucose replacement until able to tolerate oral intake; some patients will require a nasogastric tube (NG) and suction to decompress the stomach. the patient most likely will start with clear liquids once symptoms have subsided; water is the initial fluid of choice sip small amounts of fluids (5 to 15 mL) every 15 to 20 minutes; carbonated beverages with carbonation removed at room temp, warm tea; dry toast and crackers; eat food slowly; liquids taken between meals rather than with meals. the overall goals for this patient are 1) experience minimal or no nausea and vomiting; 2) have normal electrolyte levels and hydration status; 3) return to a normal pattern of fluid balance and nutrition intake. drugs to treat nausea and vomiting depends on the cause of the problem; antiemetic drugs act in the CNS via the CTZ to block the neurochemicals that trigger nausea and vomiting; serotonin antagonists are effective in reducing chemotherapy induced vomiting caused by delated gastric emptying and nausea and vomiting related to migraine headache, anesthesia, and anxiety; also aids in preventing postoperative nausea and vomiting; it is important to use these drugs with caution because they can mask the underlying disease process; ondansetron (Zofran) is a common drug [can cause constipation, diarrhea, headache, fatigue, malaise]. an alternative are use of herbals such as ginger and peppermint oil; also, breathing exercises, changes in body position, and exercise may help. if nausea and vomiting persist then hospitalization is necessary for stabilization; until the patient is diagnosed, they should be placed on NPO and given fluids by IV route. record intake and output, monitor vital signs, and assess for signs of dehydration; the risk of pulmonary aspiration is a concern when vomiting occurs in older and unconscious patients or in patients with conditions that impair the gag reflect; it may be beneficial to use semi-Fowler’s or side lying. 17. What is the interprofessional care for the ambulatory setting? it is important to teach the patient and caregiver 1) how to manage the unpleasant sensation of nausea; 2) methods to prevent nausea and vomiting; 3) strategies to maintain fluid and nutritional intake. avoid sudden changes in position; if food is the cause then help the patient identify the specific food that is causing it. Oral Cancer [pg. 898-900] 1. What are the two types of oral cancer? 2. What differentiates the two cancers? 3. Where do the lesions commonly grow? 4. What is the cause of oral cancer? 5. What are the types and characteristics of oral cancer based on location in the mouth? the two types of oral cancer are oral cavity cancer and oropharyngeal cancer; head and neck squamous cell carcinoma (HNSCC) is a broad term used for cancers of the oral cavity, pharynx, and larynx which account for 90% of malignant oral tumors. oral cavity cancer it is “mouth” cancer; which begins in the mouth and includes lips, inside lining of the lips and cheeks (buccal mucosa), teeth, gums, front two-thirds of the tongue, floor of the mouth below the tongue, and the hard palate. oropharyngeal cancer it is “throat” cancer; which starts in the oropharynx which is the area of the throat just behind the mouth; it starts where the oral cavity ends (base of the tongue, soft palate, the tonsils, and the side/back walls of the throat). lesions will commonly grow on the lower lip which is the most probable prognosis because of its location. the definitive cause of oral cancer is unknown; but there are risk factors that can lead to some of the carcinomas. these risk factors include tobacco products (smoking) and heavy alcohol use; this accounts for 7590% of the population. may cause the cancer to damage the DNA of cells that line the inside of the mouth and throat. DNA changes can turn off tumor suppressor genes and lead to cells growing out of control. 1. lip: caused by constant overexposure to sun, ruddy and fair complexions, recurrent herpetic lesions, syphilis, immunosuppression; it will show as an indurated, painless ulcers; treatment includes surgical excision and radiation. 2. tongue: caused by tobacco, alcohol, chronic irritation; it will show as ulcer or area of thickening, soreness or pain; increased salivation, slurred speech, dysphagia, toothache, earache. treatment includes hemiglossectomy/glossectomy (partial/full removal of tongue) and radiation. 3. oral cavity: caused by poor oral hygiene, tobacco use, chronic alcohol intake, chronic irritation (poor fitting prosthesis, jagged tooth, chemical/mechanical irritants, HPV); shown as a sore throat or feeling 6. What are the clinical manifestations for oral cancer? 7. What is leukoplakia? that something is stuck, difficulty chewing and speaking. treatment includes surgery and internal/external radiation. there can be nonspecific symptoms such as chronic sore throat, sore mouth, and voice changes; leukoplakia, erythroplasia (erythroplakia), and dysphagia are also common. the most common possible sign is a sore in the mouth that doesn’t heal or pain in the mouth that does not go away. it is also called a “smoker’s patch” which is a white patch on the mouth mucosa or tongue; it is a precancerous lesion however there is a less than 15% chance of these cells turning cancerous. it is the result of chronic irritation, specifically from smoking. 8. What is erythroplasia? it is a red “velvety” patch on the mouth or tongue; it is flat or slightly raised and often bleeds easily if scraped; it is also a precancerous lesion but more than a 50% chance of developing into cancer cells. the most common cause is smoking and chewing tobacco as well as poorly fitted dentures. 9. What are the diagnostic tests used to detect these cancers? diagnostic testing is utilized to identify oral dysplasia; dysplasia is graded as mild, moderate, or severe based on how abnormal the tissue looks under the microscope; knowing this degree will help to predict how likely it is to progress to cancer or go on away on its own or after treatment. oral exfoliative cytologic study involves scraping the suspicious lesion and spreading the scraping on a slide for examination; when a substance called toluidine, blue is applied to stain the area, the cancer cells will take up the dye color. other diagnostic tools are history/physical exam, biopsy, CT, MRI, and PET scans. 1. integumentary: indurated, painless ulcer on lip, painless neck masses 2. gastrointestinal: areas of thickening or roughness, limited movement of the tongue, increased salivation, drooling, foul odor breath 1. imbalanced nutrition; less than body requirements related to oral pain, difficulty chewing and swallowing, surgical resection, and radiation treatment. 2. chronic pain related to the tumor, surgery, or radiation 3. Anxiety related to diagnosis of cancer, uncertain future, potential for disfiguring surgery, and prognosis. 10. What will the physical assessment entail? 11. What are the nursing diagnoses associated with oral cancer? 12. What is the nutritional therapy? many can be malnourished and will require a percutaneous endoscopic gastrostomy (PEG tube) and enteral nutrition before radiation treatment or surgery; parental fluids are given for the first 24 to 48 hours; after that time, enteral nutrition is given by NG or PEG tubing. give small amounts of water when the patient can swallow; observe for signs of choking. 13. What are the overall goals? the goals for the patient are 1) have a patent airway 2) be able to communicate 3) have adequate nutritional intake to promote wound healing 4) have relief of pain and discomfort 14. What is the interprofessional management of a patient with oral cancer usually consists of surgery, care? radiation, chemotherapy, or a combination; the curative treatment is usually surgery and radiation; surgery remains the most effective. 15. What are the nonsurgical radiation therapy can be used only to treat small cancers or when lesions treatment options? cannot be removed; chemotherapy can shrink lesions before surgery, decrease metastasis, sensitize cancer cells to radiation, treat distant metastases; a commonly used drug therapy combination is cisplatin and 5FU; frequent suctioning of the oral cavity is necessary 16. What are the nursing early detection of oral cancer is important; the nurse should teach the implementations for oral cancer? patient to report unexplained pain or soreness in the mouth, unusual bleeding, dysphagia, sore throat, voice changes, swelling/lump in the neck; refer any person with an ulcerative lesion that does not heal within 2 to 3 weeks to the primary care doctor. 17. What is the health impact of good 1. improves quality of life oral hygiene? 2. lowers risk of teeth loss 3. reduces pain and disability 4. assists in early detection of oral and craniofacial cancers 5. decreases risk of developing periodontal disease, gingivitis, dental caries Gastrointestinal Reflux Disease (GERD) [pg. 900-904] 1. What is GERD? it is a chronic symptom of mucosal damage caused by reflux of stomach acid into the lower esophagus; it occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach; this backwash or “acid reflux” can irritate the lining of your stomach. it is the most common upper GI problem. it is a syndrome because it can cause different problems if left untreated. 2. What is the cause of GERD? there is not one single cause of GERD; it is a resultant of the acidic gastric contents into the esophagus overwhelms the esophageal defenses; the HCL combined with pepsin secretions in the reflux mixture cause esophageal irritation and inflammation which is referred to as “esophagitis”; the degree of inflammation depends on the amount and composition of the gastric reflux and on the esophageal mucosal defense mechanisms; chocolate and fatty foods relax the LES; citrus foods, spicy foods, caffeine, alcohol can increase the production of HCL. this muscle keeps the food and secretions from going down the wrong “windpipe”; is a bundle of muscles at the lower end of the esophagus where it meets the stomach; when closed it prevents any acid from backing up; under normal circumstances the LES acts as an anti-reflux barrier; an incompetent LES lets gastric contents move from the stomach to the esophagus when the patient is supine or has an increase in intraabdominal pressure. these will vary by person; persistence of mild symptoms for more than twice a week or moderate to severe symptoms once a week, it is considered GERD; heartburn (pyrosis) is one of the most common symptoms; it is classified as a burning, tight sensation beneath the lower sternum that spreads upwards to the throat or jaw; dyspepsia (indigestion) is pain or discomfort that is felt in the center of the upper abdomen (mainly around the midline); regurgitation is often described as hot, bitter, or sour liquid coming into the throat or the mouth; chest pain 3. What is the lower esophageal sphincter? 4. What are the clinical manifestations? can mimic “angina” but it is described as burning or squeezing or radiating to the back, neck, jaw, or arms; otolaryngologic symptoms includes hoarseness, sore throat, globulus sensation (sense of a lump in the throat). hypersalivation; noncardiac chest pain [MUST BE RULED OUT FROM CARDIAC CHEST PAIN] 5. What are the factors that affect increase pressure lower esophageal sphincter pressure? 1. Urecholine 2. Reglan decrease pressure (contributes to reflux) 1. alcohol 2. chocolate 3. fatty foods 4. nicotine 5. peppermint, spearmint 6. tea, coffee (caffeine) 7. drugs (calcium channel blockers, morphine, diazepam) 6. What are the complications of these are a direct relation to local effects of gastric acid on the esophageal having GERD? mucosa 1. esophagitis: which is inflammation of the lining of the esophagus; if it is not treated it can cause scar tissue formation. scar tissue will decrease the movement and narrow the esophagus tube; sit upright with HOB elevated; add a thickening agent to liquids; observe for coughing. 2. Barret’s esophagitis: also known as “esophageal metaplasia”; it is when normal esophageal cells are replaced with abnormal cells; the flat squamous epithelial cells in the distal esophagus change into columnar epithelial cells; it is a precancerous lesion that increase the patient’s risk for esophageal adenocarcinoma (cancer of the tube that runs from the throat to the stomach). it is reversible if treated early; 1 to 3 years monitoring by endoscopy. 3. respiratory complications: which includes cough, bronchospasm (sudden constriction of the muscles in the walls of the bronchioles) laryngospasm (sudden spasm of the vocal chords), cricopharyngeal spasm (muscles spasm that occurs in the throat). which are due to gastric secretions irritation the upper airway; chronic bronchitis, asthma, and pneumonia may develop from aspiration into the respiratory tract. 4. dental erosion: due to acid reflux into the mouth which affects the posterior teeth. 7. What are the diagnostic tests used? it is based on history and physical examination; barium swallow is mixed **always check the gag reflex after into a solution and is ingested, x-rays are taken to reveal if there is a procedures where the patient is protrusion of the gastric fundus; diagnostic tests are usually based on under sedation** symptoms and the patient’s responses to treatments; upper GI endoscopy is useful in assessing the lower esophageal sphincter competence and the degree of inflammation, scarring, and stricture (abnormal narrowing of a body passage);manometric studies measure pressure in the esophagus and LES and esophageal motility (movement) function; radionuclide tests can detect reflux of gastric contents and the 8. What is the nutritional therapy associated with GERD? 9. What is the drug therapy used for treatment? 10. What are the surgical options? 11. What is the interprofessional care for GERD? rate of esophageal clearance. pH monitoring: 7 pH for the esophagus; if it is 4 pH it means the gastric juices are coming up. diet does not cause GERD; however specific foods can cause irritation or aggravate symptoms; certain foods such as tomato-based products, orange juice, cola, red wine may cause irritation; avoiding late evening meals, nocturnal snacking, and milk especially at night time; also, small frequent meals between meals can help to prevent overdistention of the stomach. drug therapy focuses on decreasing the volume and acidity of reflux, improving LES function, increasing esophageal clearance, and protecting the esophageal mucosa. 1. proton pump inhibitors: are most effective in treating esophagitis; decrease HCL secretion by inhibiting the proton pump/parietal cells responsible for the secretion; decrease irritation of the esophageal and gastric mucosa; can cause headache**, abdominal pain, nausea, diarrhea, vomiting, osteoporosis (older adults); GI Prophylaxis is Protonix 2. H2 receptor blockers: reduce symptoms block the action of histamine on the H2 receptors to decrease HCL production; decrease irritation of the esophageal and gastric mucosa; can cause headache, abdominal pain, constipation, diarrhea 3. Cholinergic: increase LES pressure, improve esophageal emptying in the supine position, and increase gastric emptying; these may cause an increase in HCL acid secretion; can cause lightheadedness, syncope, flushing, diarrhea, stomach cramps, dizziness. 4. Antacids: these produce quick but short-lived relief of heartburn; neutralize HCL acid; should be taken 1-3 hours after meals and at bedtime. do not give antacid with H2 receptor blockers 5. Cytoprotective properties: Carafate; masks symptoms by coating the stomach 6. Prokinetic: these are used to produce gastric emptying and reduce gastric acid reflux. used in situations where patients are on NG tube or PEG tube and there is increased gastric residual volume > 250mL Step 1 “step up” approach: Antacid, H2 Receptor, then PPI Step 2 “step down” approach: PPI, H2 Receptor, antacids the goal of surgical therapy is to reduce reflux by enhancing the integrity of the LES; most surgical procedures are done laparoscopically; Nissen Fundoplication the fundus of the stomach is wrapped around the lower portion of the esophagus to reinforce and repair the defective barrier. the LINX Reflux Management System is an option for patients who have symptoms despite the highest medical treatment; the magnetic beads inside a titanium wire help to strengthen a weakened LES. adverse events could be difficulty swallowing, vomiting, nausea, chest pain, and pain when swallowing food. REMIND PATIENTS WHO HAVE A LINX SYSTEM TO NOT HAVE AN MRI. 1. the head of bed elevated to 30 degrees 2. should not be supine 2 to 3 hours after a meal 3. teach the patient to avoid food and activities that cause reflux such as late night eating (spicy/citrus foods, chocolate, caffeine) 4. void milk products at night because it can stimulate acid production 5. water in between meals instead of with meals because it makes you feel full faster 6. avoid fatty foods because they sit in the stomach longer 7. the patient that is taking proton pump inhibitor medications that they have to take the meds before the first meal of the day 8. the patient on H2 receptor agents that the medications must be taken as prescribed and not to be stopped without checking. 9. postoperative care focuses on preventing respiratory complications, maintaining fluid and electrolyte balance, and preventing infection. 10. measure intake and output 11. when peristalsis returns, only give fluids initially; slowly introduce solids with the goal of resuming a normal diet 12. avoid foods that are gas forming and chew food thoroughly. Notes: thoracic pressure is negative which helps to breath in and out; abdominal pressure is high pressure; the LES has to sit in the high pressure area to have the valve work efficiently; certain conditions where the stomach and esophagus can go into the chest cavity (hiatal hernia); the lining of the stomach is different from the esophagus; when the acid goes to the esophagus it creates an issue; the stomach must stay in the abdominal cavity; the esophagus must stay in the thoracic area; LES control is lost when the hiatus muscle has a “kink”; acid will come back up to cause irritation as well as decreased esophageal clearance and decreased gastric emptying. ASSESSMENT: happen before or after eating; dietary habits; when and where is the pain [radiating?]; do you take any milk or OTC medications; if the patient is relieved by milk or alkaline substances such as antacids then it is presented as GERD. Hiatal Hernia [pg. 904] 1. What is a hiatal hernia? this is a herniation of a portion of the stomach into the esophagus through an opening or hiatus in the diaphragm; in other words, when the upper part of your stomach bulges through the large muscle separating your abdomen and chest; your diaphragm has a small opening (hiatus) through which your food tube (esophagus) passes before connecting to your stomach. the most common abnormality found on x-ray examination of the upper GI tract; most common in older adults (muscle gets weak) and women (pregnancy, C-section) 2. What are the type types of hernias? 1. sliding hernia “reduction”: the junction of the esophagus and stomach “gastro-esophageal” junction and part of the stomach protrude into the chest; this occurs when the patient is supine; the most common type of hernia; the hernia will go back into the abdomen when the patient is standing. 2. paraoesophageal or rolling hernia: the fundus and greater curvature of the stomach roll up through the diaphragm, forming a “pocket” alongside the esophagus; acute herniation is a medical emergency 3. What causes the hiatal hernias? structural changes such as weakening of the muscles in the diaphragm around the esophagogastric opening which occur with aging; increase in intraabdominal pressures such as with obesity, pregnancy, ascites, tumors, intense physical exertion, heavy lifting continuously. 4. What are the clinical manifestations? the manifestations of hiatal hernias are similar to those of patient’s with GERD; dysphagia, heart burn, belching, heartburn, hiccups, nausea, regurgitation, or vomiting 5. What are some of the 1. GERD complications of these hernias? 2. Esophagitis [inflammation of the lining of the esophagus] –if untreated can eat away at the mucosal layer, muscle, and sometimes arteries/veins (arteries are “gushing” and veins are passive/slower bleed) 3. hemorrhage from erosion 4. stenosis [narrowing of the esophagus] - due to scar tissue formation 5. ulcerations of the herniated portion of the stomach 6. strangulation of the hernia – twisting around which causes circulation cut-off which will cause death to the tissue of the esophagus; 7. regurgitation with tracheal aspiration 8. leakage of contents into the abdominal cavity which can cause peritonitis and infection – patient will present with sepsis and high-fever, elevated WBC 6. What are the diagnostic studies esophagram is an x-ray test that takes pictures of the esophagus; with diagnosing hiatal hernias? which is a barium swallow exam; it can show the protrusion of gastric mucosa through the esophageal hiatus endoscopic visualization can be used to examine the lower esophagus for degree of mucosal inflammation or other abnormalities; shows the stage of healing or the phase of the hernia 7. What is the interprofessional 1. teach the patient to reduce intraabdominal pressure by eliminating management for hiatal hernias? constricting garments and avoiding lifts and straining 2. surgical approaches such as herniotomy (excision of the hernia sac), herniorrhaphy (closure of hiatal defect) gastropexy attachment of the stomach sub-diaphragmatically to prevent reherniation) hernioplasty (reconstruction of the hernia) uses a “mesh” like synthetic material to fix are often done laparoscopically. 3. stop smoking 4. elevate HOB 8. What are the goals for treatment? 1) reduce the hernia 2) provide an acceptable LES pressure 3) prevent the movement of the gastroesophageal junction. Notes: it is important that after procedures involving laparoscopic techniques the patient is walking around and passing flatulence; this is because during the procedure the surgeon is placing air into the abdomen; the nurse should make sure the patient can ambulate; this will indicate that the peristalsis is happening; then the patient can advance to ice chips, clear liquid diet, full liquid diet, and then add solid foods. Esophageal Cancer [pg. 905-907] 1. What is esophageal cancer by definition? 2. What causes esophageal cancers? 3. What are the clinical manifestations of this cancer? 4. What are the diagnostic studies of esophageal cancer? 5. What is the nutritional therapy? 6. What does the nursing assessment entail? 6. What are the nursing diagnosis associated with esophageal cancer? also referred to as “esophageal carcinoma” is not a common cancer; this is cancer that runs from the throat to the stomach; most esophageal cancers are adenocarcinomas which begins in the mucus-secreting glands in the esophagus which occurs most often in the lower portion of the esophagus; resemble cancers of the stomach and small intestine; incidence increases with age; primarily between 70 and 84 years; it affects primarily men than women. it is not exactly clear what causes esophageal cancers; there are several important risk factors that can produce this type of cancer; these include Barret’s esophagus, smoking, excessive alcohol intake, obesity, and GERD. achalasia (condition marked by delayed emptying of the lower esophagus. the majority of patients have advanced disease at the time of diagnosis; the cancer spreads via the lymph system with the liver and lung being common sites of metastasis. progressive dysphagia is the most common symptom which means feeling that food is not passing; initially the dysphagia occurs only with meat, then with soft foods, and eventually with liquids; pain will develop later; mostly in the back areas and increases with swallowing; it can radiate to the neck, jaw, ears, and shoulder; also, weight loss without trying, chest pain (pressure or burning), worsening indigestion, coughing or hoarseness; endoscopic biopsy use of a special scope that is passed down the throat into the esophagus to collect a sample of suspicious tissue; the sample is sent to the laboratory to look for cancer cells; used to make a definitive diagnosis endoscopic ultrasonography use of high-frequency waves to produce detailed images of organs; it is an important tool used to stage the esophageal cancer; esophagram (barium swallow) used to show narrowing of the esophagus at the tumor site if a patient undergoes a esophageal surgery, parental nutrition is given; a swallowing study is often done before allowing the patient to have oral fluids; this entails giving the patient 30-60 mL of water hourly and gradually progress to giving small, frequent bland meals; the patient should be in an upright position to avoid aspiration/regurgitation. if the patient is on tube feeding be sure to be aware of signs such as pain, increased temperature, and dyspnea. assess the patient for progressive dysphagia and pain with swallowing; ask the patient about the type of substances such as meats, soft foods, or liquids that cause dysphagia; assess the patient for pain such as substernal, epigastric, or back area for choking, hoarseness, cough, anorexia, weight loss, and regurgitation. 1. chronic pain related to the compression of tumor on surrounding tissues, esophageal stenosis 2. Imbalanced nutrition; less than body requirements related to dysphagia, 7. What are the overall goals for this type of patient? 8. What are the surgical therapy options? 9. What is the treatment option of photodynamic therapy? 10. What is the treatment option of Endoscopic Mucosal Resection and Radiofrequency ablation? 11. What is the treatment option of dilation and stent placement? 12. What is the nursing interprofessional care? odynophagia (painful swallowing), weakness, chemotherapy, and radiation therapy. 3. Risk for aspiration related to difficulty swallowing, choking, and regurgitation. 4. Anxiety and grieving related to diagnosis of cancer, uncertain future, and prognosis. the overall goals are 1) have relief of symptoms, including pain and dysphagia 2) achieve optimal nutritional intake 3) experience a quality of life appropriate to stage of disease and prognosis 1. esophagectomy which is the main surgical treatment for esophageal cancer; the surgeon will remove all or part of the esophagus through an incision in the chest or abdomen or both; use of a Dacron graft (man-made polyester material) to replace the resected part. 2. esophagogastrostomy resection of a portion of the esophagus and anastomosis (a surgical connection between two structures such as blood vessels or loops of he intestine) of the remaining portion of the stomach; artificial communication between esophagus and stomach. 3. esophagoenterostomy resection of a portion of the esophagus and anastomosis of a segment of colon to the remaining portion; surgical formation of direct communication between the esophagus and intestine it is a treatment that uses a drug called Photofrin which is a photosynthesizer or photosynthesizing agent with which cancer cells absorb greatest; when direct light is towards the cancerous area using a fiber passed through an endoscope, the light reacts with the agent and destroys the cancer cells; patients should avoid direct sunlight for up to 4 weeks after the procedure endoscopic mucosal resection (EMR) is an option for small and early stages; procedure to remove early stage cancer and precancerous growths from the lining of the digestive tract; radiofrequency ablation is a procedure used to reduce pain and used to kill cancer cells using electric current. dilation, stent placement, or both can relieve obstruction; dilation increases the lumen of the esophagus; which often relieves dysphagia and allows for improved nutrition; stents or expandable stents may help when dilation is no longer effective; stents allow food and liquid to pass through the stenotic area of the esophagus; may be placed before surgery to improve a patient’s nutritional status. the treatment will be dependent on the location of the tumor or whether invasion or metastasis has occurred; it typically has a poor prognosis because diagnosis is often too late; typical treatment includes surgery, endoscopic ablation, chemotherapy, and radiation therapy; palliative therapy consists of restoring swallowing function and maintaining nutrition and hydration. Gastritis [pg. 909-910] 1. What is gastritis? 2. What is the cause of gastritis? 3. What are the risk factors associated with gastritis? it is inflammation of the gastric mucosa without causes ulceration; irritation or erosion of the lining of the stomach; it can occur suddenly with erosion (acute) or gradually with nonerosion (chronic); it is a common gastrointestinal problem; it is especially common n people older than 60 years old. it is caused by the result of a breakdown in the normal gastric mucosal barrier which normally protects the stomach tissue from the corrosive action of HCL acid and pepsin; once this barrier is broken, the HCL acid and pepsin can diffuse back into the mucosa; the backup can cause tissue edema, disruption of capillary walls with loss of plasma into the gastric lumen as well as possible hemorrhage. drugs aspirin; bisphosphonates (used to treat osteoporosis); corticosteroids (reduce the immune system); iron supplements, and NSAIDs. diet alcohol; large quantities of spicy, irritating foods. microorganisms Helicobacter pylori; (this bacteria decreases the stomach’s ability to produce mucus, making the stomach prone to acid damage) Mycobacterium species (cause of tuberculosis); salmonella organisms (caused by contaminated food and water); staphylococcus organisms (cause of skin infections); cytomegalovirus (common herpesvirus); syphilis (sexual contact bacterial infection). intense emotional responses and CNS lesions (create hypersecretion of HCL) environmental factors radiation and smoking disease/disorders burns (extensive burns can change the immune response, the gastric response is compromised, increased HCL); large hiatal hernia; physiologic stress; Crohn’s disease (chronic inflammatory condition of the GI system); renal failure (causes overproduction of HCL); sepsis (changes the total body system); shock surgeries endoscopic procedures; NG tube never connect to a high volume suction because it will destroy the mucosal barrier 1. drug-related gastritis: NSAIDs including aspirin and corticosteroids inhibit the synthesis of prostaglandins that are protective to the gastric mucosa; makes the mucosa more susceptible to injury; associated with Feldene, Naprosyn, Voltaren, and Ibuprofen. most commonly affect females, being over age of 60, having a history of ulcer disease, taking anticoagulants (it can cause bleeding; ask the patient if they are taking Coumadin, Aspirin, Heparin, Lovenox), other NSAIDs. 2. diet: alcohol use can irritate and erode your stomach lining which makes your stomach more vulnerable to digestive juices; acute damage can range from localized injury to the superficial epithelial cells to destruction of the mucosa. as well as spicy, irritating foods. 3. other factors: gastritis can occur from reflux of bile salts from the duodenum into the stomach because of anatomic changes following surgical procedures; prolonged vomiting; stress; and older age. 4. What is autoimmune gastritis? 5. What are the clinical manifestations of gastritis? 6. What are the diagnostic studies? 7. What are the nursing diagnosis and related goals? this type of gastritis is a chronic inflammatory disease in which the immune system mistakenly destroys a special type of cell called “parietal” cells in the stomach; these cells are designed to secrete HCL and intrinsic factor (which is responsible for vitamin B12 absorption); the progressive loss of parietal cells can lead to iron deficiency along with vitamin B12; the cause of this is unknown but affected people most likely have another autoimmune disorder. acute gastritis symptoms include anorexia, nausea, and vomiting, epigastric tenderness, and a feeling of fullness; hemorrhage is common with alcohol abuse; it is self-limiting, lasting from a few hours to a few days; complete healing of the mucosa is expected; black, tarry stools (melena) is common; chronic gastritis develops slow overtime and if it is not treated may last for years; many people are asymptomatic but can complain of dull pain and loss of appetite after a few bites of food; a client with chronic gastritis may not be able to absorb vitamin B12 due to diminished production of intrinsic factors by the parietal cells of the stomach which can lead to pernicious anemia. many GI symptoms are vague making the diagnosis of GI problems difficult; with acute gastritis diagnosis is based upon the patient’s symptoms and a history of drug or alcohol abuse; a complete patient history and an adequate physical assessment such as dietary habits, bowel habits, and GI complaints; gastric analysis is done to examine the gastric contents and gastric juices which provides information about the presence, amount, or absence of HCL acid, presence of cancer cells, and the types and amounts of enzymes present in the stomach. stool samples can be examined for the presence of occult blood and H. pylori antigen. endoscopy direct visual examination of the gastric lining complete blood count detect anemia from blood loss from chronic gastric bleeding also tests for H. pylori. breath (ammonia chloride), urine (urea), serum (antibodies), stool, gastric tissue biopsy helps to determine H. pylori infection 1. pain related to irritation of gastric mucosa; relief of discomfort by removing irritating factor or agent; focus on teaching client about the causes of gastritis and foods that may aggravate it. 2. nutrition; less than body requirements related to decreased appetite, nausea, vomiting, and pain; improve nutrition by eating balanced diet; NPO if nausea and vomiting is severe and give IV fluid until the symptoms subside; help the patient identify triggers 3. risk for fluid volume and electrolyte imbalance; less than body requirements related to inadequate intake, vomiting; prevent dehydration and maintain moist mucous membranes, good skin turgor, electrolytes returned to normal; capillary filling, vital signs stable; measure intake and output , encourage client to drink 1500 to 2000 mL if able to tolerate; observe skin and mucous membranes 8. What is the nursing interventions acute gastritis: for gastritis 1. bowel rest 2. NPO status until symptoms subside 3. antiemetics are given 4. monitor for dehydration – administer IV fluids 5. NG tube may be used to monitor for bleeding, wash out the precipitating agent from the stomach and keep the stomach empty and free of noxious stimuli (severe cases) 6. clear fluids are resumed, and solids are gradually introduced; if the doctor orders for the NG tube to be taken out; CLAMP the tube, give liquids, wait 30 minutes, and see how the patient is doing. 7. if there is a risk of hemorrhage, vital signs and blood in vomit should be checked frequently. initially postsurgical patients will have bleeding the first 24 hours; profuse bleeding is never a normal sign 8. drug therapy focuses on reducing irritation of the gastric mucosa and providing symptomatic relief (H2 receptor blockers and PPI’s) chronic gastritis: 1. focuses on evaluating and eliminating the specific cause (cessation of alcohol intake, abstinence from drugs, H. pylori) 2. non-irritating diet of 6 small meals per day 3. antacids of small meals 10. What is the nutritional therapy? studies have shown that high-fiber diets such as soluble fiber intake of oats, legumes, barley, and certain fruits); intake of high vitamin A and avoiding alcohol and coffee. Notes: before a patient is discharged from the hospital following gastritis or any type of procedure; there must be return of bowel sounds and bowel movements; look, listen, and feel Constipation [pg. 935-938] 1. What is constipation defined? it is a syndrome; defined by the difficulty or infrequent stools; stools are hard and dry which make them difficult to pass; it can create a feeling of incomplete evacuation; it is generally described as having less than 3 bowel movements a week 2. What causes constipation? 1. taking in insufficient amounts of fiber or fluids 2. decreased physical activity 3. ignoring the urge to defecate (can cause the muscles and mucosa of the rectum to become insensitive to the presence of feces) 4. drugs especially opioids 5. diseases that slow down the GI tract such as diabetes mellitus, Parkinson’s disease, and multiple sclerosis 6. bowel obstruction; narrowing of the colon (bowel stricture) 7. emotions such as anxiety, depression, and stress 8. people that believe constipation is a result of not having a daily bowel movement which results in chronic laxative behavior. it is the anatomic and physiologic change in the colon that occurs with chronic use of stimulant laxatives; more than 3 times per week for at least a year; it is a condition in which the colon becomes dilated and atonic, or “lacking muscle tone”) the symptoms vary by person and can range from mild discomfort to a more severe mimicking an acute abdomen; stools are hard, dry, and difficult to pass; the person may have abdominal distention, bloating, increased flatulence, and increased rectal pressure. hemorrhoids most common complication; it is a result of venous engorgement caused by repeated Valsalva maneuvers or “straining” from hard, impacted stools; straining happens when the patient inspires deeply and holds their breath while contracting the abdominal muscles with bearing down; this will increase the intraabdominal as well as the intrathoracic pressures which can reduce the venous return to the heart (transient drop in arterial pressure) as the patient relaxes the pressure drops and an immediate rise in arterial pressure; these pressure changes may be fatal for the patient who cannot compensate for the sudden increased blood flow returning to the heart. obstipation this is a severe form of constipation or “complete constipation” where the person cannot pass a stool or gas. 3. What is cathartic colon syndrome? 4. What are the clinical manifestations? 5. What are the complications associated with constipation? 6. What are the diagnostic studies related to constipation? 7. What does the nursing assessment entail? 8. What is the nutrition therapy? fecal impaction hardened stool that is stuck in the rectum or lower colon due to chronic constipation; occurs with people who are constipated for a long period of time colonic perforation life threatening which occurs when a hole is formed all the way through the stomach, large bowel, or small intestine; it causes abdominal pain, nausea, vomiting, fever, and an elevated WBC. diverticulitis is a potential complication of chronic constipation; it is a condition where there are small, bulging pouches that can form in the lining of your digestive system; found in the lower portion. it is always important to take a thorough history and physical examination to identify the underlying cause of constipation; the diagnostic tests include abdominal x-ray, barium enema, anorectal manometry, defecography with barium (uses an x-ray to look at the shape and position of the rectum as it empties), fluoroscopy (uses x-ray to obtain real-time moving images), and colonic transit tests (it is a diagnostic procedure that offers information as to how long it takes for food to travel through the digestive system). subjective data: 1. past medical history: bowel obstruction, irritable bowel syndrome, colorectal disease. 2. medication history: aluminum and calcium antacids, anticholinergics, antidepressants, opioids, diuretics, iron, laxatives, enemas *ask the patient about usual defecation patterns, diet, exercise, laxative use, and past history such as obstetric injuries that could contribute functional health patterns: 1. chronic laxative or enema abuse; 2. changes in diet or mealtime, inadequate fiber and fluid intake; 3. change in usual elimination patterns; hard, difficult to pass stool; decrease in frequency and amount of stools; flatus; abdominal distention 4. change in daily activities, sedentary lifestyle 5. abdominal pain on defecation 6. acute or chronic stress objective data: 1. general: lethargy 2. integumentary: anorectal fissures, hemorrhoids, abscesses 3. gastrointestinal: abdominal distention, hypoactive or absent bowel sounds; palpable abdominal mass, fecal impaction, small hard dry stool, stool with blood diet is an important factor! improved symptoms when increase of dietary fiber intake; dietary fiber is found in fruits, vegetables, and grains; wheat bran and prunes are especially effective for preventing and treating constipation; the purpose of dietary fiber is to add bulk to the stool directing by attracting water; the adequate fluid intake is 2L per day unless contraindicated; tell the patient that increasing fiber intake may initially increase gas production 9. What is the drug therapy used for constipation? 10. What are the nursing implementations and health promotions? because of fermentation in the colon which will decrease over several days. bulk forming use: absorbs water, increases bulk, thereby stimulating peristalsis and works usually within 24 hours; comments: contraindicated in patients with abdominal pain, nausea, and vomiting as well as patients suspected of having appendicitis, biliary tract obstruction; must be taken with fluids (>8OZ) best choice for initial treatment; examples: Cirucel, Metamucil, Hydrocil, Fiberall, Konsyl stool softeners and lubricants uses: lubricate intestinal tract and soften feces making hard stools easier to pass; does not affect peristalsis and usually softens in 72 hours and lubricates in 8 hours; comments: can block absorption of fat-soluble vitamins such as vitamin K which can increase risk of bleeding in patients on anticoagulants. examples: Colace, Surfak, Fleet’s Oil Retention Enema saline and osmotic solutions uses: cause retention of fluid in intestinal lumen caused by osmotic effect and typically works in 15 minutes to 3 hours; comments: magnesium-containing products may cause hypermagnesemia in patients with renal insufficiency. examples: magnesium salts, magnesium citrate, milk of magnesia, sodium phosphates, MiraLAX. stimulants uses: increase peristalsis by irritating colon wall and stimulating enteric nerves and usually works within 12 hours; comments: cause melanosis coli (brown or black pigmentation of colon; most widely abused laxatives; should not be used in patients with impaction or constipation. examples: Ex-Lax, Dulcolax, Correctol, Doxidan, Senokot. Selective Chloride Channel Activator uses: increases intestinal fluid secretion and motility and usually works within 24 hours. comments: used in the treatment of idiopathic constipation and irritable bowel syndrome with constipation (women only); contraindicated in patients with history of mechanical GI obstruction. examples: Amitiza intestinal secretagogue uses: increases fluid secretion and accelerates intestinal transit and usually works within 24 hours. comments: used in treatment of idiopathic constipation and irritable bowel syndrome. examples: Linzess 1. eat dietary fiber: 20 to 30g of fiber per day; gradually increase the amount of fiber eaten over 1 to 2 weeks (softens hard stool and adds bulk to stool; foods high in fiber such as vegetables and fruits, beans, and breakfast cereals; fiber supplements: Metamucil, Citrucel, FiberCon; eat prunes or drink prune juice daily; prunes stimulate defecation. 2. drink fluids: drink 2L per day; avoid caffeinated coffee, tea, and cola; caffeine stimulates fluid loss through urine 3. exercise regularly: three times per week; exercise stimulates bowel motility and moves stool through the colon 4. establish a regular time to defecate: first thing in the morning or after the first meal of the day; this is because people often have the urge to defecate at these times 5. do not delay defecation: respond to the urge to have a bowel movement as soon as possible; delaying will result in hard stools and a decrease “urge” to defecate; water is absorbed from stool by the intestine over time; the colon will become less sensitive in the presence of stool. 6. record your bowel elimination pattern: develop a habit of recording when you have a bowel movement to help in early detection 7. avoid laxatives and enemas: people who overuse them are unable to have a bowel movement without them. 8. defecation position: sitting on a commode with the knees higher than the hips; allows for gravity to aid in defecation; flexing of the hips straightens the angle between the anal canal and rectum so that stool flows out; place a foot stool in front of the toilet to promote flexion of the thighs. if the patient is in bed, elevate the head of the bed as high as they can tolerate and provide as much privacy as possible. Diarrhea [pg. 929-933] 1. What is diarrhea defined? it is the passage of at least 3 loose or liquid stools per day; it can also be defined as acute, lasting for 14 days or less, persistent lasting greater than 14 days, and chronic diarrhea lasting 30 days or longer. 2. What is the cause of diarrhea? the primary cause of diarrhea is when a person ingests infectious organisms; however, viruses cause most cases of infectious diarrhea; most are mild and last less than 24 hours; a person’s age, gastric acidity, intestinal microflora, and immune status influence susceptibility to pathogenic organisms; older adults are more likely to suffer life-threatening diarrhea. Escherichia coli is a type of enterohemorrhagic E. coli that is the most common cause of bloody diarrhea; it is transmitted by undercooked beef or chicken contaminated with the bacteria or in fruits and vegetables exposed to contaminated manure; it is manifested by low grade fever, severe abdominal cramping, bloody diarrhea, and vomiting; it can lasts 5 to 7 days; Giardia lamblia is the most common intestinal parasite that causes diarrhea; it is highly contagious; it is transmitted via fecal-oral route and is found in fresh lakes and rivers as well as swimming pools, water parks, and hot tubs; it is manifested by abdominal cramps, nausea, diarrhea, and may interfere with nutrient absorption. 1. alter secretion and absorption of the enterocytes (intestinal absorption cells) of the small intestine without causing inflammation 2. impair absorption by destroying cells, cause inflammation in the colon and produce toxins that cause damage 3. secretory diarrhea result of bacterial or vial infections; the ingested pathogens survive in the GI tract long enough to absorb into the enterocytes which changes the permeability and results in the over secretion of water, sodium, and chloride ions into the bowel 4. the organisms can enter the body by contaminated food or contaminated drinking water 5. Traveler’s diarrhea, when a person travels to a country with poor sanitation habits 6. antibiotics kill off the normal flora, making the person more susceptible to pathogenic organisms 7. immunocompromised patients receiving jejunal enteral nutrition are specifically prone to foodborne infections; this is because they bypass the stomach’s acid environment and do not contain the poorly digestible fiber that is necessary for normal flora 8. taking medications designed to decrease stomach acid such as proton pump inhibitors and histamine H2 receptor blockers increase the likelihood that the pathogens will survive. 3. What are the two most common organisms that infect a person with diarrhea? 4. What are the different ways in which infectious organisms can attack the intestines? 5. What are the clinical manifestations? 6. What are the diagnostic studies used? 7. What does the nursing assessment entail? 8. What are the nursing diagnosis associated with diarrhea? 9. What are the goals of treatment? 10. What is the drug therapy? infections usually produce large-volumes of water stools, cramping, and periumbilical pain; a person could have low-grade fever or no fever at all; often experience nausea and vomiting before the diarrhea begins; infections of the colon and distal small bowel produce fever and frequent bloody diarrhea with a small volume; severe diarrhea produces life threatening dehydration, electrolyte imbalances, and acid-base imbalances. stool cultures are done only in patients who are very ill, have a high fever, or have had diarrhea longer than 3 days; the stools are examined for blood, mucus, WBCs, and parasites. cultures reliably identify the organism ova and parasite testing is for people who have had diarrhea more than 2 weeks measuring stool electrolytes, pH, and osmolality is used for patients with chronic diarrhea to determine whether the diarrhea is from decreased fluid absorption or increased fluid secretion. increased hematocrit, blood urea nitrogen (BUN), creatinine levels are signs of a fluid deficit a thorough history and physical examination is necessary; ask the patient to describe his or her stool patterns with associated symptoms; focus on the duration, frequency, character, and consistency of the stool; ask about medications they are taking such as antibiotics and laxatives that are known to cause diarrhea; determine whether the patient has traveled to a foreign country, been at a day care facility recently, food intolerances, and food preparation practices. objective data: 1. general survey: lethargy, sunken eyeballs, fever, malnutrition 2. integumentary: pallor, dry mucous membranes, poor skin turgor, perianal irritation 3. gastrointestinal: frequent soft to liquid stools that may alternate with constipation; abdominal distention; hyperactive bowel sounds; pus, blood, mucus or fat in stools. 4. urinary: decreased output; concentrated urine 1. diarrhea related to acute infectious process 2. deficient fluid volume related to excessive fluid loss and decreased fluid intake the overall goals are 1) no transmission of the microorganism causing the infectious diarrhea 2) cessation of diarrhea and resumption of normal bowel patterns 3) normal fluid, electrolyte, and acid-base balances 4) normal nutritional status 5) no perianal/perineal skin breakdown Pepto-Bismol decreases secretions and used to prevent Traveler’s diarrhea Mitrolan bulk-forming agent that absorbs excessive fluid from diarrhea to form a gel; it is used when intestinal mucosa cannot absorb fluids Imodium, Pepto Diarrheal Control inhibits peristalsis, delays transit, increases absorption of fluid from stools 10. What is the complication of C. difficile? 11. How is C. difficile prevented? 12. How is C. difficile treated? 13. What are the nursing implementations? Lomotil opioid and anticholinergic; it decreases peristalsis and intestinal motility. this disease is highest in patients receiving antimicrobial, chemotherapy, or immunosuppressive agents; also, ICU stays, prolonged hospital stays, having surgery, receiving drugs that suppress gastric acid; C. difficile spores can survive for up to 70 days on objects including commodes, telephones, thermometers, bedside tables, and floors. it can prevented by meticulous hand washing with soap and water; frequently changing gloves. it is treated with Flagyl which is the first line of treatment of mild to moderate cases; or vancomycin which is used for severe cases and in patients who do not respond to Flagyl therapy within 5 to 7 days (it is given orally or by enema) Fecal microbiota transplantation (FMT) is becoming one of the most effective treatments for C. difficile; it reestablishes healthy intestinal flora by infusing fecal bacteria obtained from healthy donor stools into the patient’s colon; the feces is obtained from the donor and consists of pureed, liquid, slurry consistency using saline, water, or pasteurized cow’s milk; it is placed in the GI tract via an enema, nasoenteral tube, or during endoscopy. 1. strict infection control precautions are necessary; consider all cases of acute diarrhea infectious until the cause is known; 2. wash your hands before and after contact with each patient when handling bodily fluids of any kind 3. teach the patient and caregiver to wash contaminated clothing with soap and water 4. immediately put patients with C. difficile in isolation and ensure that the visitors wear proper PPEs; 5. infected patients should have their own stethoscopes and thermometers 6. ensure that surfaces and equipment are disinfected with a 10% bleach solution or a disinfectant that is labeled C. difficile sporicidal. Peptic Ulcer Disease [pg. 910-919] 1. What is peptic ulcer disease by definition? characterized by erosion of the GI mucosa from the digestive action of HCL and pepsin; any portion of the GI tract that is in contact with these enzymes are at risk for ulcer development; lower esophagus, stomach, duodenum 2. What are the two types of peptic ulcers? acute ulcers is associated with superficial erosion with minimal inflammation; it is often short in duration and resolves quickly if it is identified. chronic ulcers has a long duration, erodes through the muscular walls with the formation of fibrous tissue or scar tissue formation; it can be present continuously for months or intermittently throughout life. 3. What is the cause of peptic ulcer disease? it develops only in an acidic environment; pepsinogen, changes to pepsin in the presence of HCL and a pH of 2 to 3; surface mucosa of stomach is renewed about every 3 days; the mucosa can continually repair itself except in extreme instances helicobacter pylori has A and B antigens; O+; it is transmitted through fecal-oral route or oral-oral route; bacteria in the stomach can survive a long time by colonizing the gastric epithelial cells within the mucosal layer; bacteria produces Urea which metabolizes urea-producing ammonium chloride; this activates the immune response and the release of inflammatory cytokines which leads to increased gastric secretion and tissue damage; aspirin and NSAIDs because they inhibit synthesis of prostaglandins which is a protective barrier of the mucosal layer. 4. What are the destroyers of the mucosal barrier? . What are the duodenal ulcers? 6. What are the gastric ulcers? 7. What are the three major complications of PUD? 8. What are the diagnostic studies? corticosteroids decreases the rate of mucosal cell renewal which decreases the protective effects; patients with COPD, asthma which reduce the immune response. lifestyle alcohol, smoking, coffee, and stress pain is located in the mid-epigastric region, it can also be located in the back; pain is relieved with antacids and food; it occurs 2-5 hours after meals; it can cause “burning” or “cramp-like” feelings; H. pylori infection is 90% the pain is high in the epigastrium; pain is aggravated with food; most commonly found in the antrum; more prevalent in women and those that are over the age of 50; more likely to result in obstruction; cause “burning” and “epigastric pressure”; pain happens 1-2 hours after meals; H. pylori infection is 80% 1. hemorrhage: most common; ulcer through a major blood vessel; develops from erosion; changes in vital signs and an increase in the amount and redness of aspirate often is a signal; patient’s pain will decrease because the blood helps to neutralize the acidic contents; check vital signs (blood pressure, pulse, respirations) and abdominal distention (pain with palpation) LOC, administer fluids; must preserve the brain 2. perforation: most lethal complication; often located on lesser curvature of the stomach; the ulcer penetrates through the serosal surface with spillage of gastric or duodenal contents into the peritoneal cavity; large perforations require immediate surgery; small perorations can seal themselves but can cause fibrinous fusion which creates strictures that can obstruct the flow of intestinal contents; immediate focus is to stop the spillage of gastric or duodenal contents into the peritoneal cavity and restore blood volume; the NG tube can provide continuous aspiration and gastric decompression to stop spillage; circulating volume is replaced with lactated Ringer’s and albumin solutions (substitute for the fluids lost from the vascular and interstitial space. 3. gastric outlet obstruction: obstructions are due to edema, inflammation, edema, pylorospasm and fibrous scar tissue formation; ulcers are located in the antrum (lower most portion of the stomach) and duodenum; patients will have projective vomiting because the pyloric sphincter develops scar tissue and contents are not moving out of the stomach; the pressure increases forcing the food back up; aim of therapy is to decompress the stomach, correct any existing fluid imbalances, and improve the patient’s general state; continuous decompression; IV fluids and electrolytes are replaced according to the degree of dehydration, vomiting, and electrolytes. endoscopy most accurate diagnostic procedure; allows for direct view of the duodenal and gastric ulcers biopsy of the antral mucosa gold standard for diagnosing H. pylori urea breath test identify active infection; urea is the by-product of the metabolism of H. pylori bacteria 9. What is the medical regimen? 10. What is the drug therapy? 11. What is the nutritional therapy? barium contrast studies used for patients who can not do an endoscopy; the barium swallow does not go past the pyloric sphincter. laboratory analysis CBC to check for anemia secondary to ulcer bleeding; urinalysis; serum amylase determination (pancreatic function), liver enzymes stool examination presence of blood 1. adequate rest 2. dietary modification 3. drug therapy 4. elimination of smoking and alcohol 5. stress management patient can be discharged if pain disappears within 3 to 6 days. 1. Proton Pump Inhibitors: these are more effective than H2 receptor blockers; are used in combination with antibiotics to treat ulcers caused by H. pylori. 2. Histamine H2 Receptor Blockers: promotes ulcer healing; the onset of action is 1 hour and therapeutic effects last up to 12 hours; Famotidine, ranitidine, cimetidine can be given orally or IV; Nizatidine is only given orally. 3. Antacids: increase gastric pH by neutralizing the HCL acid which reduces the acid content of the chyme; the neutralizing effects taken on an empty stomach last only 20 to 30 minutes; if they are taken after meals can last up 3 to 4 hours; with the NG tube in place the stomach contents should be aspirated and tested for the pH level; they can also enhance the absorption of drugs such as dicoumarol (anticoagulant) and amphetamines; antacids high in sodium such as sodium citrate should be used cautiously in older adults and patients with hypertension and renal failure; renal failure patients should not take magnesium preparations because of the risk of magnesium toxicity; 4. Cytoprotective Drug Therapy: provides cytoprotection (chemical compounds provide protection to cells against harmful agents) for the esophagus, stomach, and duodenum; does not have any acid-neutralizing capabilities; it is most effective at a low pH and is given 60 minutes before or after an antacid; Sucralfate 5. Anticholinergics: are occasionally used for pelvic ulcer disease; result in reduced acid secretion; however, they are associated with a number of side effects such as dry mouth, warm skin, flushing, thirst, tachycardia, dilated pupils, blurred vision, and urinary retention. nutrition helps to minimize the occurrence of expected complications; because of gastric resection decreases the stomach’s size, patients must reduce their meal size accordingly and limit drinking fluids with meals. 1. divide meals into 6 small frequent meals to avoid overloading the stomach 2. do not take fluids with meals but at least 30-45 mins before or after; this helps prevent distention or a “feeling of fullness” 3. avoid concentrated sweets; the immediate ingestion of sugared fluids or 12. What is the surgical therapy? 13. What is the nursing management for preoperative and postoperative care? 14. What are the postoperative complications of surgery? candy relieves hypoglycemic symptoms. 4. increase protein and fats to promote rebuilding of body tissues and to meet energy needs such as meat, cheese, and eggs 5. dry foods with a low carbohydrate content Billroth I: Gastroduodenostomy partial gastrectomy with removal of the distal 2/3 of the stomach and cross-connection of the gastric stump of the duodenum Billroth II: Gastrojejunostomy same as above but the gastric stump has a cross connection to the jejunum Vagotomy (decreases gastric acid secretion) surgical operation where one or more of the branches of the vagus nerve are severed. Pyloroplasty surgical enlargement of the pyloric sphincter to allow for easy passage of contents from the stomach. reducing the amount of time that the food will stay in the stomach; preoperative care 1. teach the patient what to expect after surgery including comfort measures, pain relief, coughing and breathing exercises, use of an NG tube, and IV fluid replacement postoperative care 1. NG tube is used to decompress the remaining portion of the stomach; observe the gastric aspirate for color, amount, and odor (aspirate is usually bright red at first with a gradual darkening within the first 24 hours after; color will then change to a yellow-green within 36 to 48 hours; 2. the NG should remain patent so that gastric secretions do not accumulate this can result in 1) rupture of sutures 2) leakage of gastric contents into the peritoneal cavity 3) hemorrhage 4) possible abscess formation 3. observe the patient for signs of decreased peristalsis, abdominal distention, and lower abdominal discomfort which can indicate intestinal obstruction; 4. monitor and record intake and output every 4 hours 5. splinting the area with a pillow while encouraging the patient to deep breath helps prevent respiratory complications; 6. encourage early ambulation before the NG tube is removed, the patient begins clear liquids to determine the tolerance level; the stomach may be aspirated within 1 to 2 hours to assess amount remaining; if fluids are well tolerated then the NG tube is removed; fluids are increased in frequency, slow progression to regular foods then to 6 small meals a day. Dumping Syndrome – happens within 15 to 30 minutes; it occurs because of the surgical removal of a large portion of the stomach and pyloric sphincter; the stomach no longer has control over the gastric chyme entering the small intestine; a large bolus of hypertonic fluid will enter the intestine which causes fluid to go into the bowel; this creases a decrease in plasma volume; the patient describes feelings of weakness, sweating, palpitations, and dizziness due to the sudden 15. What does the nursing assessment consist of? 16. What are the nursing diagnosis associated with PUD? 17. What are the goals of PUD? 18. What are the nursing implementations? 19. What should the nurse teach the patient and caregiver? decrease in plasma volume usually last 1 hour after eating; borborygmic (audible abdominal sounds produced by hyperactive intestinal peristalsis) Postprandial hypoglycemia – uncontrolled gastric emptying of a bolus of fluid that is high in carbohydrate; this bolus results in hyperglycemia because it is not sitting in the stomach to be digested, it is getting rid of quickly which is why it causes reflex hypoglycemia; symptoms are similar to hypoglycemia; sweating, weakness, mental confusion, palpitations, tachycardia, anxiety; usually 2 hours after eating Bile Reflux gastritis – because of the construction or removal of the pylorus it can result in reflux of bile into the stomach; this prolonged contact will cause the bile to damage the gastric mucosa; the main symptom is continuous epigastric stress which increases after meals; vomiting relieves the distress but not for too long; Cholestyramine (Questran) is given before or with meals; it binds with the bile salts that are the source of irritation. subjective data 1. medication history of aspirin, corticosteroids, NSAIDs functional health patterns 1. health management: chronic alcohol abuse, smoking, caffeine use; family history of peptic ulcer disease 2. nutrition: hematemesis, dyspepsia, heartburn, belching, weight loss 3. elimination: black, tarry stools 4. coping: acute or chronic stress objective data 1. general: anxiety, irritability 2. gastrointestinal: epigastric tenderness 1. acute pain related to increased gastric secretions 2. ineffective health management related to lack of knowledge of longterm management 3. nausea related to acute exacerbation of disease process the overall goals are 1) adhere to the prescribed therapeutic regimen 2) experience a reduction in or absence of discomfort 3) exhibit no signs of GI complications 4) have complete healing of the peptic ulcer 5) make appropriate lifestyle changes early detection and effective treatment of ulcers is important with reducing mobility risks associated acute phase the patient can be NPO for a few days; an NG tube is inserted and connected to intermittent suction; IV fluid replacement; regular mouth care alleviates the dry mouth; cleaning and lubricating the nares facilitate breathing and decrease soreness; laboratory test results such as hematocrit, hemoglobin, and electrolytes determine the type and amount of fluids given; take vital signs initially and then at least hourly to detect and treat shock; record intake and output; physical and emotional rest is helpful (quiet and restful) 1. follow dietary modifications including avoiding foods that may cause epigastric stress 2. avoid cigarettes 3. reduce or eliminate alcohol intake 4. avoid OTC drugs unless approved; many preparations contain ingredients such as aspirin 5. do not interchange brands of antacids, H2 receptor blockers, and PPI 6. take all medications as prescribed 7. report any of the following: increased nausea and vomiting, increased epigastric pain, bloody emesis or tarry stools Notes: D (sandostatin inhibits the production of HCL); G (gastric cells); protective function is the G cells and the nonprotective agents are the D cells and enterochomal cells; Muscine; epithelial layer, the tight junctions between the stomach cells, restoration and regeneration, and prostaglandins are protective naturally to the digestive organs. under normal conditions, a physiologic balance exists between gastric acid secretion and gastroduodenal mucosal defenses; mucosal injury occur when the balance between the aggressive factors and the defense mechanisms is disrupted. Stomach Cancer [pg. 919-921] 1. What is stomach cancer defined? which is also called “gastric cancer’; it is defined as an adenocarcinoma of the stomach; it begins when cancer cells form in the inner lining of the stomach which grow into a tumor; higher in men than women by a 2:1 ratio; mostly affects older people with the average age of people being diagnosed at 69. 2. What is the cause and pathophysiology? there are many factors related but no single causative agent; it most likely begins with a nonspecific reason such as an H. pylori infection, autoimmune-related inflammation, or repeated exposure to irritants such as bile, antinflammatory agents, and tobacco usage. it spreads by direct extension and typically infiltrates rapidly to the surrounding tissues (liver); it has been associated with diets containing smoked foods, salted fish/meats, and pickled vegetables; smoking and obesity both increase these risks. often spread to adjacent organs before any symptoms may occur; the person will appear as pale and weak with complaints of fatigue, weakness, dizziness, and shortness of breath (extreme cases); the patient will experience unexplained weight loss, indigestion, abdominal discomfort with pain; anemia is common (caused by chronic blood loss as the lesion erodes through the mucosa or loss of intrinsic factor; supraclavicular lymph nodes that are hard and enlarged can be evidence of metastasis via the thoracic duct. upper GI endoscopy is the best diagnostic tool; uses a fluoroscopic x-ray using a contrast medium to show structural abnormalities; the patient should be NPA for at least 8 hours and to avoid smoking. tissue biopsy and subsequent histologic exam important in diagnosing cancer endoscopic ultrasound (CT, PET) used to stage the disease laparoscopy done to determine peritoneal spread blood study detect anemia and determines the severity elevations in liver enzymes/amylase indicate liver and pancreatic involvement stool examination provides evidence of occult or gross bleeding the location and extent of the lesion, the patient’s physical condition, and surgeon’s preference determine surgery the surgical goal is to remove as much as the stomach as necessary to remove the tumor; lesions that are located in the antrum or pyloric region 3. What are the clinical manifestations? 4. What are the diagnostic studies for stomach cancer? 5. What is the surgical therapy? are treated by Billroth I or II; lesion is located in the fundus then a total gastrectomy is performed (most cases). 6. What does the nursing assessment entail? 7. What are the nursing diagnosis associated? 8. What are the overall goals for this type of diagnosis? 9. What is the preoperative care for this patient? 10. What is the postoperative care for this patient? 11. What is the health promotion role of stomach cancer? it is important to obtain a nutritional assessment; especially about appetite and changes in eating patterns over the last 6 months; determine the patient’s normal weight with any recent changes; unexplained weight loss is common; cachexia (weakness and wasting away) due to decreased oral intake. 1. imbalanced nutrition, less than body requirements related to inability to ingest, digest, or absorb nutrients 2. acute pain related to underlying disease process and side effects of surgery, chemotherapy, or radiation therapy the overall goals are 1) experience minimal discomfort 2) achieve optimal nutrition 3) maintain a degree of spiritual and psychological wellbeing preoperative care when the diagnostic tests confirm cancer it is important to provide the family with emotional and physical support for this difficult time; the patient must have a positive nutritional state to help with wound healing in order to be admitted for surgery; diet may be challenging but it will consist mainly of commercial liquid supplements and vitamins; packed RBCs and fluid volume restoration may be given prior; monitor hemoglobin and hematocrit postoperative care typically with the total gastrectomy is an NG tube insertion (large amounts of drainage will not come out because of the removal of the stomach); the tube is removed when intestinal peristalsis has begun; small amounts of clear liquid, once the liquids are tolerated without concern then fluid intake is increased until solid food is added (closely observe for signs of fluid leakage such as increased temperature and dyspnea) IV or oral replacement of Vitamin C, D, D, K, and B complexes as well as cobalamin is necessary because these are normally absorbed in the duodenum; skin care, oral care, fluid therapy, and nutrition are very essential 1. identifying the patient at risk because of specific disorders such as H. pylori infection, anemia, and achlorhydria (absence of hydrochloric acid in the gastric secretions). 2. possibility of stomach cancer in a patient who is treated for peptic ulcer disease and fails to have relief with prescribed therapy. Upper Gastrointestinal Bleeding [pg. 921-925] 1. What is upper gastrointestinal bleeding defined? 2. What is the cause of upper GI bleeds? it is a symptom of a disorder in your digestive tract; commonly referred to as bleeding in your upper gastrointestinal tract; it can be a signal of a serious disease; approximately 300,000 hospital admissions occur each year for upper GI bleeding it can occur in the upper or lower portion of the GI tract; the most serious loss of blood from the upper GI tract, however, is characterized by sudden onset, insidious occult bleeding that can become a significant problem; the severity depends on venous, capillary, or arterial; arterial bleeds are profuse with the blood being red, meaning that it has not come into contact with the HCL in the stomach; venous bleeds are characterized by oozing or running of dark colored blood which is low pressurized; capillary bleeds is characterized by trickling of blood; the longer the passage of blood through the intestines, the darker the stool color because of the breakdown of hemoglobin and release of iron 3. What are the different types of 1. hematemesis: “bloody” vomitus which appears as fresh, bright red Upper GI bleeding? blood; or “coffee-ground” appearance which is dark, grainy digested blood 2. melena: black, “tarry” stools which often have a noxious smell are caused by the digestion of blood in the GI tract; the “black” appearance is from the presence of iron 3. occult bleeding: small amounts of blood in gastric secretions, vomitus, or stools; detectable only by a guaiac test. 4. What is the major cause of upper GI one of the major causes of bleeding are drugs such as aspirin, NSAIDs, bleeding? and corticosteroids which account for 40% of the cases of bleeding; many OTC preparations contain aspirin; it is important to take a careful history of all commonly used drugs when this is suspected. 5. What are the diagnostic studies? endoscopy is the primary tool for diagnosing the source of upper GI bleeding. angiography is an examination by x-ray of blood and lymph vessels, carried out after radiopaque dye is introduced; it is used when endoscopic procedures cannot be done or when bleeding is persistent laboratory studies CBC (hematocrit and hemoglobin values provide a baseline for guiding further treatment) BUN (with significant hemorrhage – GI tract bacteria break down proteins which elevates these levels), electrolytes, prothrombin time, partial 6. What does the nursing assessment entail? 7. What is the assessment for emergency situations? 8. What is the initial treatment for acute gastrointestinal bleeding? thromboplastin time, liver enzymes, ABGs, and a crossmatch for possible blood transfusions. subjective data 1. past medical history: precipitating events before bleeding episode, previous bleeding episode and treatments, peptic ulcer disease 2. medications: aspirin, NSAIDs, corticosteroids, anticoagulants functional health patterns 1. health management: family history of bleeding, history of smoking or alcohol abuse 2. nutrition: weight loss 3. elimination: diarrhea, black/tarry stools, decreased urine output, sweating 4. activity: dizziness, weakness, fainting 5. perceptual: epigastric pain, abdominal cramping objective data 1. general: fever 2. integumentary: clammy, cool, pale skin; pale mucous membranes, nail beds and conjunctivae, spider angiomas, peripheral edema 3. respiratory: rapid, shallow respirations 4. cardiovascular: tachycardia, weak pulse, orthostatic hypotension, slow capillary refill 5. gastrointestinal: red or “coffee-ground” vomitus; tense/rigid abdomen, ascites, black tarry stools 6. urinary: decreased urine output; concentrated urine 7. neurologic: agitation, restlessness, decreasing level of consciousness a complete history of events leading to the bleeding episode is deferred until emergency care has been initiated focus assessment 1. signs and symptoms of shock such as tachycardia, weak pulse, hypotension, cool extremities, prolonged capillary refill, and apprehension 2. level of consciousness, vital signs (every 15 to 30 minutes), and skin color 2. urine output is one of the best measures of organ perfusion; 3. hemodynamic monitoring provides an accurate and quick assessment of blood flow 4. check the abdomen for distention, guarding, and peristalsis immediate intervention has started; ask the following questions; 1. is there a history of previous bleeding episodes? 2. has the patient received blood transfusions in the past? 3. Were there any transfusion reaction? 4. Are there any other illnesses (liver, cirrhosis) 5. Does the patient have a religious preference that prohibits the use of blood or blood products? 1. if unresponsive, assess CAB 2. if responsive, monitor ABCs 3. establish an IV access with large bore catheter and start IV fluids 9. What are the nursing diagnosis involved with upper GI bleeds? 10. What are the overall goals for this patient? 11. What is the endoscopic therapy? 12. When is surgical intervention indicated? 13. What is the drug therapy? 14. What does the health promotion entail? isotonic crystalloid solutions such as Lactated Ringer’s solution is started 4. give O2 via nasal cannula or a non-breather mask to increase saturation 5. initiate ECG monitoring 6. obtain blood for CBC, clotting studies, and type of transfusion 7. insertion of an NG tube (as needed) observe aspirate for blood 8. insert indwelling catheter for hourly assessment 9. give an IV proton pump inhibitor (PPI) to decrease acid secretions 10. auscultate lung sounds and closely observe respiratory effort 11. keep the head of the bed elevated 1. deficient fluid volume related to acute loss of blood and gastric secretions 2. ineffective peripheral tissue perfusion related to loss of circulating volume the overall goals for this patient are 1) to have no further GI bleeding 2) have the cause of the bleeding identified and treated 3) experience a return to a normal hemodynamic state 4) experience minimal or no symptoms of pain or anxiety this is the first line of management for upper GI bleeds; it is performed within the first 24 hours of bleeding to help diagnosis and determine the need for surgical intervention; the two most common procedures are multipolar electrocoagulation and the thermal probe which coagulates tissue by directly applying a heating element to the bleeding sites. it is indicated when bleeding continues regardless of the therapy that is provided and when the site of bleeding has been identified; it is necessary when the patient continuously bleeds after an infusion of 2000 mL of whole blood; also, if the patient remains in shock for more than 24 hours. drugs are used to decrease the bleeding, decrease HCL acid secretion, and neutralize the HCL acid that is present; PPIs are used in high doses (because the acidic environment can alter platelet function and interfere with clot stabilization); injection therapy with epinephrine (produces tissue edema which puts pressure on the source of bleeding; Sandosatin or vasopression is given when upper GI bleeding is from esophageal or gastric. 1. teach the at-risk patient to avoid known gastric irritants such as alcohol and smoking and to take only prescribed medications 2. avoid severe coughing or sneezing because it can increase pressure on the already fragile varices and can result in massive hemorrhage 3. patients who require regular doses of aspirin, corticosteroids, or NSAIDs should take them with a snack to help lessen the irritation 4. teach the patient about the disease process, drugs, and increased risks for GI bleeding. Polyps of the Large Intestine [pg. 953] 1. How are colorectal polyps defined? these are growths that appear on the surface of the colon; they are small clumps of cells that form on the lining of the colon or rectum; they arise from the mucosal surface of the colon and project into the lumen. 2. What are the two sizes? sessile: flat, broad-based and are attached directly to the intestinal wall; are a greater cancer risk because they’re tricky to find and may be overlooked for years; their flat appearance hides them in the thick mucus membranes that line the colon and stomach; pedunculated: attached to the intestinal wall by a thin, narrow, elongated stalk; polyps tend to be sessile when small and become pedunculated as they enlarge; can be found anywhere in the large intestine (proximal colon) the most common signs and symptoms are rectal bleeding and occult blood in the stool; however most patients tend to be asymptomatic. 1. hyperplastic polyps which are non-neoplastic growths; rarely grow large (>5 mm) which are generally benign growths on the lining of the large intestine; a growth in which extra cells project out from tissues inside the body that have repaired damaged tissue, especially along the digestive tract. 2. adenomatous polyps: which are neoplastic and closely linked to colorectal adenocarcinoma; benign but can be a precursor lesions to colorectal cancer; there are three types; tubular (because of the rounded nature of the neoplastic glands that form it), tubulovillous (grows in the colon and may become malignant), villous (occur more frequently in the rectum and rectosigmoid). colonoscopy is preferred; it allows evaluation of the total colon; all polyps are considered abnormal and should be removed; it is an inherited disorder characterized by hundreds and thousands of polyps in the colon that become cancerous, typically around the age of 40; it is an autosomal dominant trait meaning that 50% of the offspring of the patient with FAP carry the FAP gene; these patients are at risk for cancers of the thyroid, small intestine, liver, and brain; lifetime surveillance is essential; a family history should be undergone during childhood. 3. What are the most common signs and symptoms? 4. What are the two types of polyps of the intestine? 5. How are polyps of the large intestine diagnosed? 6. What is familial adenomatous polyposis (FAP)? Colorectal Cancer [pg. 954-958] 1. How is colorectal cancer defined? 2. What is the cause of this type of cancer? 3. What are the risk factors associated with colorectal cancer? 4. What are the clinical manifestations? 5. What is the difference between the right-sided tumor and the left-sided tumor growth? 6. What are the diagnostic tools used to diagnose colorectal cancer? it is cancer of the large intestine which is the final part of your digestive tract; it is the second leading cause of cancer-related deaths and is the third most common cancer in men and women; it is more common in men than in women; mortality rates are highest among African Americans; mostly detected in people older than 50. there is no single risk factor that accounts for this type of cancer; the highest risk is those with first-degree relatives and people with irritable bowel syndrome; adenocarcinoma is the most common type which accounts for 85%; when the tumor grows inside the body; it invades and penetrates the muscle; since venous blood leaving the colon and rectum flows through the portal vein and the inferior rectal vein, the liver is a common site of metastasis; also in the lungs, bones, and brain. 1. family history of colorectal cancer (first-degree) 2. personal history of inflammatory bowel disease 3. personal history of colorectal cancer 4. family or personal history of familial adenomatous polyposis (FAP) 5. obesity with a body mass index > 30 kg/m2 6. red meat consumption for more than 7 servings per week 7. cigarette smoking 8. alcohol consumption of more than 4 drinks per week 9. personal history of diabetes mellitus this type of cancer has an insidious onset with the symptoms not appearing until the disease has advanced; typical manifestations are iron deficiency anemia, rectal bleeding, abdominal pain, change in bowel habits, intestinal obstruction, perforation; 1. early disease: nonspecific findings such as weight loss and fatigue 2. more advanced disease: abdominal tenderness, palpable abdominal mass, hepatomegaly, ascites. right sided lesions are most likely to cause diarrhea and are the more common; it causes anemia in most cases; left sided lesions are not as common as the right side and are detected later; hematochezia (fresh blood in the stool). a thorough history with close attention to family history colonoscopy this is the gold standard for screening because the entire colon can be observed; during this procedure, biopsies can be obtained, immediately removed, and sent to the lab; FOBT (fecal occult blood test) and FIT (fecal immunochemical test) look for blood in the stool; stool tests must be done frequently since tumor bleeds occur at intervals and are easily missed if only a single test is done. once tissue biopsies have confirmed the diagnosis then additional laboratory studies are done such as CBC (anemia) and liver function tests; CT scan and MRIs are used to check the depth of penetration of tumor into the bowel wall. 8. What is the testing schedule? 9. What does the nursing assessment entail? 10. What are the nursing diagnosis associated with colorectal cancer? 11. What are the overall goals for the patient diagnosed? 12. What is the surgical therapy? 13. What are the various kinds of procedures used? 1. flexible sigmoidoscopy – every 5 years 2. colonoscopy – every 10 years unless there is a first-degree relative that developed colorectal cancer before age 60 or two first-degree relatives with the cancer then they should be done every 5 years. 3. double-contrast barium enema – every 5 years 4. CT colonography (virtual colonoscopy) – every 5 years 5. FOBT – every year 6. FIT – every year subjective data 1. paste health history: villous adenoma, adenomatous polyps, inflammatory bowel disease 2. medication history: use of any medications affecting bowel function functional health problems 1. health management: family history of colorectal cancer, breast cancer, ovarian cancer, weakness, fatigue 2. nutrition: high-calorie, high-fat, low-fiber diet, weight loss 3. elimination: change in bowel habits, alternating diarrhea and constipation, defecation urgency, rectal bleeding, black and tarry stools, increased flatus, feelings of incomplete evacuation. perceptual: abdominal and low back pain; tenesmus (continual or recurrent inclination to evacuate bowels) objective data 1. general: pallor, cachexia, lymphadenopathy (disease of the lymph node) 2. gastrointestinal: palpable abdominal mass, distention, ascites, and hepatomegaly (liver metastasis) 1. diarrhea or constipation related to altered bowel elimination patterns 2. ineffective coping related to diagnosis of cancer and side effects of treatment. the overall goals are 1) normal bowel elimination patterns 2) quality of life appropriate to the disease process 3) relief of pain 4) feelings of comfort and well-being the decision for surgical therapy depends on the location, ability to restore normal bowel function, and continence; stage I: removal of the tumor and at least 5 cm of intestine on either side of the tumor as well as nearby lymph nodes; the remaining cancer-free ends are sewn back together via anastomosis. stage II: treated with wide resection and re-anastomosis; chemotherapy is used along with surgery if the stage II tumor is high-risk. stage III: treated with surgery and chemotherapy; radiation and chemotherapy are done before surgery to reduce the size of the tumor stage IV: once the cancer has spread to distant sites (metastasis) any surgery is palliative; along with radiation and chemotherapy used to control the spread and to provide pain relief. abdominal-perineal resection (APR) the tumor is in the distal rectum; about 1-2 cm from the anorectal junction and the sphincters cannot be preserved; involves removing the entire rectum with the tumor; the patient will have a permanent colostomy. 14. What are the goals of surgical therapy? 15. What is the TMM classification of colorectal cancer? 16. What is the lymph node involvement classification? lower anterior resection (LAR) tumor is in the mid or proximal rectum; it may be possible to preserve the sphincters; involves removing the rectum and anastomosing the colon to the anal canal; a temporary ileostomy or colostomy may be done to divert stool and allow time for the anastomosis to heal (8-12 weeks) colonic J-pouch created by folding the distal colon back on itself and suturing it to form a “pouch” which replaces the rectum as a reservoir for stool; the patient will have a temporary ostomy to allow the J-pouch sutures to heal before stool can enter it; coloplasty made by slitting the side of a section of colon a short distance proximal to the anus; which stretches out the colon making it wider. the overall goals of surgery are 1) complete resection of the tumor 2) a thorough exploration of the abdomen to determine if the cancer has spread 3) removing all lymph nodes that drain the area where the cancer is located 4) restoring bowel continuity for normal bowel function to return 5) preventing surgical complication Tx – primary tumor cannot be assessed because of incomplete information Tis – carcinoma; cancer is in earliest stage and has not grown beyond mucosa layer T1 – tumor has grown beyond mucosa into the submucosa T2 – tumor has grown through submucosa into muscle (muscular propria) T3 – tumor has grown through the muscle into the subserosa but not to neighboring organs or tissues T4 – tumor has spread completely through the colon or rectal wall and into nearby tissues or organs Nx – lymph nodes cannot be assessed N0 – no regional lymph node involvement is found N1 – cancer is found in 1-3 nearby lymph nodes N2 – cancer is found in 4+ nearby lymph nodes 17. What is the metastasis classification Mx – presence of distant metastasis cannot be assessed system? M0 – no distant metastasis is seen M1 – distant metastasis is present 17. How is colon cancer staged based stage 0: Tis + N0 + M0 off of the above classifications? stage 1: T1 or T2 + N0 + M0 18. What is the nursing implementation for this cancer? 19. What is the health promotion? stage 2: T3 + N0 + M0 stage 3: any T + N1 + M0 stage 4: any T, any M, M1 1. if healthy bowel is restored, normal bowel function is to be maintained and routine postoperative care is appropriate 2. if there is an open wound with drains (Jackson-Pratt or Hemovac) and an ostomy then sterile dressing changes, care of drains, and patient/caregiver teaching about the ostomy. 3. carefully assess all drainage for amount, color, and consistency; drainage is usually serosanguineous 4. examine the wound regularly and record bleeding, excessive drainage, and unusual odors 5. patients may experience phantom rectal pain (which is a sensation when the body feels as if it needs to evacuate but the rectum is no longer present ; this is normal and will subside over time 6. if the wound is closed, assess the incision for suture integrity, signs and symptoms of wound inflammation as well as infection 7. observe the skin around the drain; and keep the area clean and dry 1. encourage all person’s over the age of 50 to have regular screening to help identify those at high risks 2. provide teaching about bowel cleansing for outpatient diagnostic procedures; patient should follow a low-residue or full liquid diet the day before the procedure; 2L of polyethylene glycol lavage is done the night before and the other 2L is done 4-6 hours before procedure