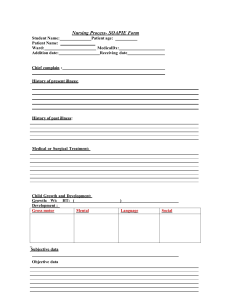
Chapter 4 The Complete Health HistorNURS220 Chapter 4 The Complete Health History The Health History Sequence The purpose to obtain of health history is together subjective data and objective data. Subjective date also include: The Health History Sequence Biographical data Source of history Reason for seeking care Present health or history of present illness Past health Family history Review of systems Functional assessment including activities of daily living (ADLs) Biographical Data Biographical date include: Name Address and phone number Age and birth date Birthplace Sex Marital status Race Ethnic origin Occupation: usual and present Source of History Source of History: Patient, relative, friend Record who furnishes information Reliability of the informant Note whether the person appears well or ill Reason for Seeking Care Reason for Seeking Care: Brief spontaneous statement in person’s own words describing reason for visit Symptom: subjective sensation person feels from disorder What person says is reason for seeking care is recorded and enclosed in quotation marks to indicate person’s exact words Sign: objective abnormality that can be detected on physical examination or in laboratory reports Avoid translating into a medical diagnosis. Present Health or History of Present Illness (HPI) Present Health or History of Present Illness(HPI): Location Character or quality Quantity or severity Timing Setting Aggravating or relieving factors Associated factors Patient’s perception Present Health or History of Present Illness “Tell me about your abdominal pain?” Character/Quality describe symptoms, feeling, appearance, burning, Onset (Timing): when. When did the pain start , when did u feel the problem? Location: where, does it radiate? Duration (Timing): how long. Severity: how bad, pain scale Pattern (Aggravating or relieving factors): what improves it? Worsens it? what make the pain worse or better Associated factors: any other symptoms associated with primary SX(symptoms) such as fever, chill, urine fr. Affects client (Patient’s perception). Potential anxiety Setting – where was the person or what ws the person doing when symptoms started? PQRSTU PQRSTU May find it helpful to organize data/ different pneumonic P: provocative or palliative: what brings it on? What makes it better? Worse? Q: quality or Quantity: how does it look, feel, sound? Intense? Severe? R: region or Radiation – Where is it? Radiating? S: severity scale: Scale 0-10- Better? Worse? T: timing: Onset- when does it occur? How long does it last? How often? U: understand patient’s Perception of the problem. What does it mean? Past Health Past Health: Childhood illnesses; MMRV strep throat, v. cough, chicken pork Accidents or injuries ; head injury, wound, burn, fracture, Serious or chronic illnesses; HIV infection, cancer, Hepatitis, DM, HTN, depression, heart disease, Hospitalizations ; cause of the hospitalization, how long there, name of the doctor, name of the hospital, how recover Surgeries; type of surgery, date, name of hosp/doctor, how the person recover Obstetric history; # of pregnancy, # of miscarry, # of children living, the sex, Immunizations; Last examination date: hearing, EKG, pap smear, mammo Allergies; foods, know the reaction such as rash, running eye, sob Current medications; know the name/brand, does, ask how pt take each day, what it is for, sig affect of it Family History Family History: May use genogram- See page 49 of example of genogram (family tree: 3 generation such as parent, grandpa, sibling Culture and genetics: biographic data, spiritual resources /religion, past health, Health perception Cross-Culture Care Implications Cross-Culture Care Implications: Additional questions for new immigrants Biographical data Spiritual resource and religion: assess if certain procedures cannot be done Past health: what immunizations, if any Health perception How does person describe health and illness How does person see problems he or she is now experiencing Nutrition: taboo foods or food combinations Review of Systems Review of System Purposes: 1- Assess past and present health for each body system 2- check for omitted data 3- Evaluate health promotion practices The order of the examination is generally a head to toe examination. Document as present or absent, or denies headache, cough etc. Avoid terms such as negative or positive. Review of Systems: General overall health state Skin Hair Head Eyes Ears Nose and sinuses Mouth and throat Neck Breast Axilla Respiratory system Cardiovascular Peripheral vascular Gastrointestinal Urinary system Male genital system Female genital system Sexual health Musculoskeletal system Neurologic system Hematologic system Endocrine system Collecting Objective Data: Physical setting; by providing comfort area for pt, gown, pen light Preparing oneself: introduce yourself, explain the procedure, wash hand before or after the procedure Approaching the patient: leave room when pt changing clothes, be organize or limit unnecessary position change Positions for Physical Assessment Positions for Physical Assessment: include Supine Dorsal recumbent Sims position Prone Knee chest Lithotomy Validating Data Validating Data: Validating: purpose is to confirm or verify that subjective and objective data are reliable and accurate. Look for inconsistent findings. Methods of Validation Clarify data Verify data with another health care professional Compare objective findings with subjective findings. Assessment (ADL) Functional Assessment (ADL):Fumeanctional It uses to measure a person selfcare Self-esteem, self-concept Activity and exercise Sleep and rest Nutrition and elimination Interpersonal relationships and resources Spiritual resources Coping and stress management Personal habits Illicit or street drugs Environment and work hazards Intimate partner violence Occupational health Psychosocial Interview - Adolescent Psychosocial Interview-Adolescent: Method of interviewing focuses on assessment of: Home environment, Education and employment, Eating, peer-related Activities, Drugs, Sexuality, Suicide and depression, and Safety from injury and violence