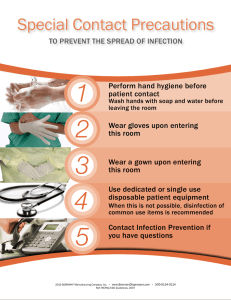
INFECTION & INFLAMMATION NUR134 Clean hands video https://www.youtube.com/watch?v=SMjNCiYvDZQ&feature=related Objectives-found in Leaning Packet 1. Explain the key terms in the textbook reading assignment. 2. Examine the infection cycle and evaluate methods to break the chain of infection. 3. Differentiate the stages and characteristics of infection. 4. Discuss nosocomial infections (Health Care Acquired Infections) and the sites they usually occur. 5. Identify factors that reduce the incidence of Health Care Acquired Infections. 6. Integrate standard precautions during patient care. 7. Differentiate the classifications of pathogens. 8. Explain the body’s normal defense against infection and identify patients at risk for developing infections. 9. Explain the inflammatory response, including signs and symptoms. 10. Utilize the nursing process to assist in the development of a plan of care/concept map for the care of patients with infection and inflammation problems. 11. Apply transmission based precautions. 12. Utilize criteria to evaluate patients’ response to nursing interventions. 13. Evaluate the phases of wound healing and the types of repair. 14. Differentiate the roles of the RN and the LPN in the care of patients with infection and inflammation problems. 15. Review Evidence Based Information in text. Pre lecture Quiz-True or False 1. The portal of exit is the point in the chain of infection in which the organism enters a new host. 2. Bacteria are the smallest of all microorganisms. 3. A person is most infectious during the prodromal stage of illness. 4. Surgical asepsis, or clean technique, involves procedures and practices that reduce the number and transfer of pathogens. 5. Hand hygiene is the most effective way to prevent the spread of organisms. Pre Lecture Quiz-Fill in the Blank 1. The __________________ of a microorganism is the natural habitat of the organism where growth and multiplication occur. 2. ___________________, such as mosquitoes, ticks, and lice, are carriers that transmit organisms from one host to another. 3. The _____________________ response helps the body to neutralize, control, or eliminate an offending agent and to prepare the site for repair 4. ______________________-based precautions are used for patients in hospitals with suspected infection with pathogens that can be transmitted by airborne, droplet, or contact routes. 5. The infection control process of _______________________destroys all pathogenic organisms, including spores. Unfolding Case Study Clark Austin is a 75 year retired person who lives with his wife, Ann. He is admitted to the hospital with acute cholecysitis. He has undergone a choylstectomy and has been transferred to your floor 2 days post op. He has a nasogastric tube to low intermittent suction, one peripheral line, 20g in Right arm, a large abdominal dressing and a history of emphysema. In addition he is on O2 2L/min per NC, and receives a continuous pulse oximetry monitoring. Infection á Definition - Disease state resulting from the presence of pathogens in or on the body Chain of infection Infectious agent Reservoir Portal of exit Mode of transmission Portal of entry Susceptible host http://www.youtube.co m/watch?v=NHHrCZkcF Xk https://www.youtube.com/watch?v=NHHrCZkcFXk Infectious Agent Virulence Invasiveness Number present Ability to live at body temperature & cause illness Examples of agents http://time.com/79 209/solving-themystery-flu-thatkilled-50-millionpeople/ http://time.com/79209/solving-the-mystery-flu-that-killed50-million-people/ Prevalent Resistant Organisms Methicillin –resistant staphylococcus aureus (MRSA) Vancomycin-resistant enterococcus (VRE) Aminoglycoside-resistant pseudomonas (gentamicin, tobramycin, amikacin) CDC | 12 Steps to Prevent Antimicrobial Resistance Among Long-term Care Residents https://www.cdc.gov/antibiotic-use/healthcare/index.html Reservoir Inanimate – soil, water, other environmental sources, medical equipment Animate – people, animals, insects The Inanimate Environment Can Facilitate Transmission X represents VRE culture positive sites ~ Contaminated surfaces increase cross-transmission ~ Abstract: The Risk of Hand and Glove Contamination after Contact with a VRE (+) Patient Environment. Hayden M, ICAAC, 2001, Chicago, IL. Portal of exit Method for the pathogens to leave the source –Respiratory tract –Gastrointestinal tract –Genitourinary tract –Breaks in Skin, mucous membranes –Bloodstream Laboratory Data Indicating Infection Elevated white blood cell count—normal is 5,000 to 10,000/mm3 Increase in specific types of white blood cells Elevated erythrocyte sedimentation rate Presence of pathogen in urine, blood, sputum, or draining cultures Means of transmission 3 Primary Routes Contact -2 modes Direct Indirect Droplet Airbourne 2 Lesser Routes Vehicles Vector Isolation guidelines A group of actions that include hand hygiene and the use of barrier precautions, which intend to reduce the transmission of infectious organisms Precautions apply to all clients, regardless of diagnosis, and implementation of them must occur whenever there’s anticipation of coming into contact with a potentially infectious material. Change personal protective equipment after contact with each client and between procedures with the same client I in contact with large amounts of blood and body fluids Clients in isolation are at higher risk for depression and loneliness. Assist the client and their family to understand the reason and provide sensory stimulation Infection control Standard precautions (tier one) Hand hygiene Appropriate gloving and glove changing Masks, eye protection, face shields if splashing of body fluids Properly clean equipment Proper disposal of trash/laundry Sharps precautions Transmission precautions (tier two) Airborne precautions Droplet precautions Contact precautions Aseptic Technique Includes all activities to prevent or break the chain of infection Two categories Medical asepsis—clean technique Handwashing/clean gloving – best defense against infection Surgical asepsis—sterile technique % Recovery of gram negative bacteria 40 Evidence based Practice Can a Fashion Statement Harm the Patient? 35 Natural (n=31) Artificial (n=27) Polished (n=31) 30 ARTIFICIAL 20 10 10 0 5 POLISHED NATURAL p<0.05 Avoid wearing artificial nails, keep natural nails <1/4 inch if caring for high risk patients (ICU, OR) Edel et. al, Nursing Research 1998: 47;54-59 Portal of entry Respiratory tract URI Gastrointestinal tract Genitourinary tract Breaks in Skin, mucous membranes Bloodstream Susceptible host Factors affecting susceptibility Intact skin and mucous membranes Normal pH levels Body’s white blood cells Age, sex, race, hereditary factors Immunization, natural or acquired Fatigue, climate, nutritional and general health status Stress Use of invasive or indwelling medical devises Unfolding Case Study What are some characteristics of Mr. Austin that put him at risk for infection? Nosocomial infections (Health Care-Associated Infections) Risk Factors Skin integrity Multiple illnesses Invasive procedures/indwelling medical devices Broad spectrum antibiotics Poor aseptic technique Multiple health care personnel Extended length of hospitalization Causes & sites Urinary Tract Surgical/traumatic wounds Respiratory Tract (URI, pneumonia) Blood stream Question Which of the following is the most significant and commonly found infection-causing agent in healthcare institutions? A. Bacteria B. Fungi C. Viruses D. Mold Measures to Reduce Incidence of Nosocomial Infections Constant surveillance by infectioncontrol committees and nurse epidemiologists Written infection-prevention practices for all agency personnel Hand hygiene recommendations Infection control precaution techniques Keeping patient in best possible physical condition Multidrug resistant organisms Prevent infections, thereby preventing the spread of resistance Tracking Improve antibiotic prescribing/stewardship Develop new drugs and diagnostic tests Clostridium difficile (C diff) Seen largely in older adults Symptomatic and asymptomatic reservoirs Prolonged antibiotics kill ‘helpful’ bacteria in intestines then C diff grows! Watery diarrhea, fever, abnormal cramps Prevention of C diff Avoid use of hard to clean equipment (electronic thermometer) Disinfect care items between patients (stethoscope) PPE Meticulous hand hygiene (SOAP AND WATER; C diff not killed by alcohol based hand rubs) Keep environment clean Educate health care providers Definitions Sterilization Disinfectant Antiseptic Factors Determining Use of Sterilization and Disinfection Methods Nature of organisms present Number of organisms present Type of equipment Intended use of equipment Available means for sterilization and disinfection Time Unfolding Case Study This morning you enter Mr. Austin’s room, and he appears anxious, coughs a lot. He is complaining of SOB, and pain in his chest, and his incision site. He states I feel hot, and an extremely tired. You recall yesterday that Mr. Austin rang his call light multiple times with vague complaints, his VS were WNL Course of infection 1. 2. 3. 4. Incubation period—organisms growing and multiplying Prodromal stage—person is most infectious, vague and nonspecific signs of disease Full stage of illness—presence of specific signs and symptoms of disease Convalescent period—recovery from the infection Question In which of the following stages of infection is the patient most contagious? A. Incubation period B. Prodromal stage C. Full stage of illness D. Convalescent period The Iceberg Effect Infected Colonized Infection Clinical manifestations Localized Systemic (generalized) Acute wound Chronic wound Cardinal Signs of Infection Redness Heat Edema Pain Loss of function Unfolding Case Study What would you note in Mr. Austin’s wound if you were suspicious of a wound infection; what other signs and symptoms might he have What nursing interventions would you do first? Infection Sign & Symptoms Depends on agent responsible for infection and the site of the infection. Unfolding Case Study What type of signs and symptoms would Clark Austin have with pnemonia? Systemic or local What type of signs and symptoms would Clark Austin have with a wound infection Systemic or local Infection Diagnostic Tests Vital signs CBC, with differential Cultures Scans Communicable Disease Infectious disease that is highly transmissible to other people. Organizations WHO CDC State Epidemiologist Local public health department Inflammation Localized response to injury or infection. Promotes wound healing Protective function Inflammatory Response 1. Vascular Vasoconstriction Confine the area of injury, limit tissue damage Vasodilatation Flood area with promote healing 2. Results in hyperemia & heat Cellular Increased cellular permeability WBCs move into area-Clean wound-consume debris Results in pain, edema, loss of function Exudate - Accumulation of fluid, dead tissue cells, WBC’s Types of exudate Serous Sanguineous Serosanguineous Purulent Suffix “itis” Indicates inflammation appendicitis sinusitis gastritis bronchitis Immune Response Antigen -part of attacking organism that is responsible for stimulation of Antibodies The Antigen, foreign material, induces a specific immune response The Antibody is an immunoglobin produced by the body in response to a specific antigen Concept in Action-Immune Response Antigen antibody reaction Humoral immunity Humoral response- Production of antibodies to a specific antigen by the B- cell lymphocytes. Antibodies are released into the blood stream. Antibodies bind to the specific antigen causing their destruction. Cellular Mediated Defense Cellular Immune Response T - lymphocytes = T Cells Attack foreign invaders directly Initiated by the binding of an antigen with an antigen receptor located on the surface of the T cell. Results in total destruction of the invading microbes or neutralization of the toxins. Types of Immunity Passive Natural - From the mother Artificial - Injection of serum from immune person Active Natural - Have the disease Artificial - Immunization with antigen CDC guidelines to prevent infection Standard Precautions (Tier One)– Acknowledge that all blood, body fluids excretions or secretions, mucous membranes, tissues, contaminated items, & non intact skin are potentially infectious –ALL Patient contact Transmission Based Precautions(Tier Two) used in addition to standard precautions for patients with suspected infection Airborne Precautions – Used for patients known or suspected to have infections transmitted by airborne transmission (organisms that can be suspended in air for prolonged periods) Droplet Precautions – Used for patients known or suspected to have infections transmitted by the droplet transmission route (organisms may travel 3 feet but are not suspended for long time periods) Contact Precautions – Used for patients known or suspected to have infections transmitted by direct contact or contact with items in the patient’s environment. Unfolding Case Study If Isolation precautions were needed after C & S of sputum comes back what type of precaution might be indicated? What type of PPE? If the wound was draining purulent matter what type of precaution might be indicated? What type of PPE? Personal Protective Equipment and Supplies Gloves Gowns Masks Protective eye gear Room assignments and Isolation-PPE and respiratory protection Airborne Precautions-infection spreads via air (TB, rubeola, varicella) Private room Monitored negative air pressure 6-12 air changes per hour Monitored filtration if air recirculated Door closed; patient stays in room If patient comes out of room (medically necessary) must have on surgical mask Room assignments and Isolation-PPE Droplet Precautions-infection spread in large droplets Private room (if available), door may be open If Patient must come out of room (medically necessary) must wear surgical mask PPE and keep visitors 3 feet from infected person Room assignments and Isolation-PPE Contact Precautions-infection spread by direct or indirect contact with patient or patient’s environment Used with multi drug resistant organisms Limit movement out of room Avoid sharing patient care equipment Latex allergy-risk factors Health care workers People with allergic tendencies People with food allergies (banana, papaya, avocado, potatoes, kiwi, chestnuts, pineapple Latex industry workers People with spina bifida, asthma, or a history of multiple surgical exposures to latex Health care products with latex-common Gloves BP cuff Electrode pads Stethoscopes IV tubing Urinary cath Tourniquets Syringes Surgical masks Baby bottle nipples Plus more Latex allergy-planning care Prevent exposure to latex Treat reaction Question Tell whether the following statement is true or false. Standard precautions should be used when caring for a noninfectious, postoperative patient who is vomiting blood. A. True B. False Wounds Intentional or unintentional Open or closed Acute or chronic http://www.impactlab.net/2009/06/22/ pet-owners-at-increased-risk-ofacquiring-fatal-mrsa-infection/ Unfolding Case Study Use criteria of wound description to describe the type of wound Mr. Austin has How could you help Mr. Austin avoid wound complication of dehiscence or evisceration in a cholecystectomy RUQ surgical wound? Phases of the Wound Healing 1.hemostasis, 2.inflammatory phase, 3.proliferation, 4.maturation Concept in Action-Acute Inflammation 1. Hemostasis 1. Vasoconstriction Platelets accumulate along blood vessels Blood clot seals wound 1. Hemostasis 2. Vasodilation Release of intracellular chemicals Active hyperemia • • • Causes redness and heat Increased vascular permeability • • Causes swelling and pain 1. Hemostasis 3. Increased Vascular Permeability • • • Begins immediately , most active during the first 24 hrs. Fluid, protein, leukocytes move from the capillaries into the tissue spaces. Causes edema & pain 1. Hemostasis Exudate - Accumulation of fluid, dead tissue cells, WBC’s Types of exudate Serous Sanguineous Serosanguineous Purulent 1. Hemostasis As fibrinogen leaves the blood, it is activated to fibrin. Fibrin strengthens blood clot formed by platelets. Clot functions to trap bacteria, preventing their spread, serves as a framework for healing. 2. Inflammatory Phase Follows hemostasis, lasts 4-6 days WBC’s pass through the blood vessels into the wound Acute inflammation-pain, redness, heat, swelling Patient may have a general body response Macrophages enter wound, ingest debris, secrete growth factor Fibroblasts fill the wound 3. Proliferative Phase (Granulation or Reconstruction) - New tissue is generated & the continuity of injured tissues is restored. For healing to progress foreign bodies are removedinterferes with wound healing. Undamaged epithelial cells move from the wound edges under the base of the clot. Cells bridge the gap within 48 hrs. re-establishing the skin’s permeability barrier. Epithelial tissues serve as a barrier between the body & the environment. (new tissue is Granulation tissue) Halts invasion of bacteria, toxic material Blocks fluid & electrolyte loss Fibroblasts (connective tissue) migrate & deposit fibrin Fibrin secretes collagen produces tensile strength Capillaries adjacent to the wound develop buds Buds stretch across the fibrin Capillaries meet and re-establish the blood supply Provides nutrients & blood supply Granulation tissue New reddish color, highly vascular tissue that bleeds easily 4. Remodeling or Maturation Tissues undergo slow progressive change in size & shape for months. Heal by replacement (remodeled) or regeneration Healing by Regeneration Replacement of destroyed tissue cells by cells that are identical or similar in structure and function. Labile Cells Stable Cells Permanent Cells Healing by replacement Collagen continues to be deposited. Shrinkage and contraction Contains fewer pigmented cells & has a lighter color than normal skin. Unfolding Case Study What type of wound Clark Austin have with the cholecystectomy and what type of tissue repair will it heal by? If Mr. Austin develops a sacral pressure ulcer, stage 3; what type of tissue repair will it heal by? If Mr. Austin was admitted with ruptured appendicitis and abdominal abcess; what type of tissue repair will it heal by? Tissue Repair Primary intention- clean, surgical incision Secondary intention- edges do not close, heals from the inside out Tertiary intention- delay in surgical suturing, but is eventually sutured http://what-when-how.com/nursing/special-skin-and-woundcare-client-care-nursing-part-3/ Clean Hand Jive https://www.youtube.com/watch?v=sS-KyhAzeUY&feature=related