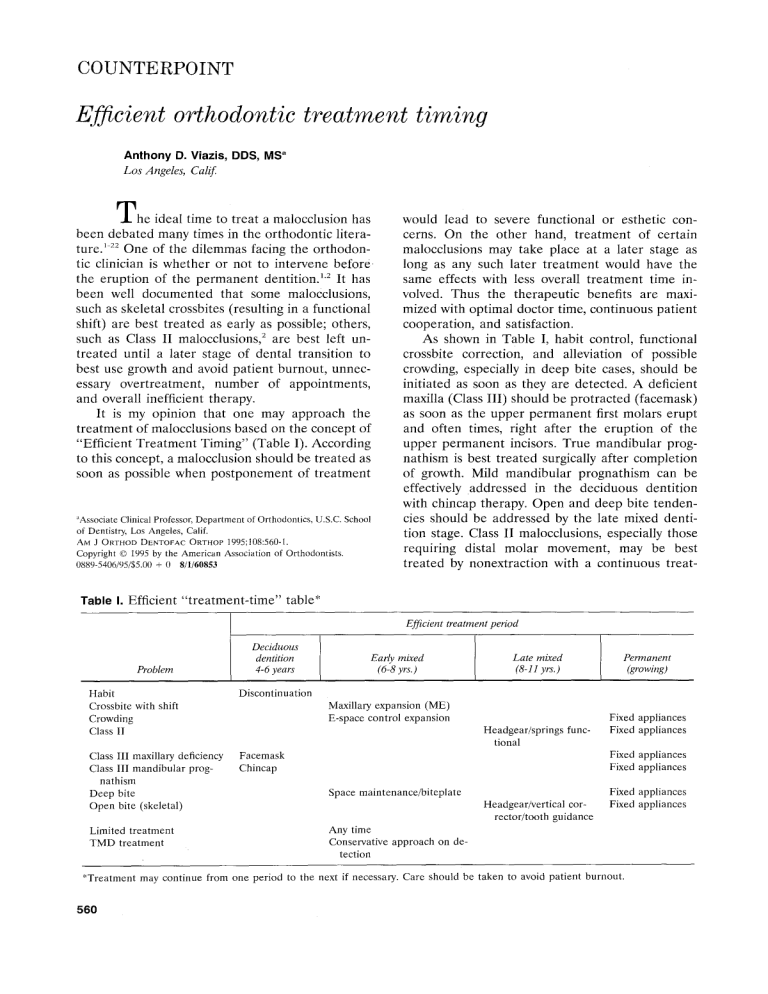
COUNTERPOINT Efficient orthodontic treatment timing Anthony D. Viazis, DDS, MS a Los Angeles; Calif. T h e ideal time to treat a malocclusion has been debated many times in the orthodontic literature. '-22 One of the dilemmas facing the orthodontic clinician is whether or not to intervene b e f o r e the eruption of the permanent dentition. 1"2 It has been well documented that some malocclusions, such as skeletal crossbites (resulting in a functional shift) are best treated as early as possible; others, such as Class I! malocclusions, 2 are best left untreated until a later stage of dental transition to best use growth and avoid patient burnout, unnecessary overtreatment, number of appointments, and overall inefficient therapy. It is my opinion that one may approach the treatment of malocclusions based on the concept of "Efficient Treatment Timing" (Table I). According to this concept, a malocclusion should be treated as soon as possible when postponement of treatment ~Associate Clinical Professor, Department of Orthodontics, U.S.C. School of Dentistry, Los Angeles, Calif. AM J ORTHOD DENTOFAC ORTHOP 1995;108:560-1. Copyright © 1995 by the American Association of Orthodontists. 0889-5406/95/$5.00 + 0 8/1/60853 would lead to severe functional or esthetic concerns. On the other hand, treatment of certain malocclusions may take place at a later stage as long as any such later treatment would have the same effects with less overall treatment time involved. Thus the therapeutic benefits are maximized with optimal doctor time, continuous patient cooperation, and satisfaction. As shown in Table I, habit control, functional crossbite correction, and alleviation of possible crowding, especially in deep bite cases, should be initiated as soon as they are detected. A deficient maxilla (Class Ill) should be protracted (facemask) as soon as the upper permanent first molars erupt and often times, right after the eruption of the upper permanent incisors. True mandibular prognathism is best treated surgically after completion of growth. Mild mandibular prognathism can be effectively addressed in the deciduous dentition with chincap therapy. Open and deep bite tendencies should be addressed by the late mixed dentition stage. Class II malocclusions, especially those requiring distal molar movement, may be best treated by nonextraction with a continuous treat- Table I. Efficient "treatment-time" table* Efficient treatment period Problem Habit Crossbite with shift Crowding Class II Deciduous dentition 4-6 ),ears Late mixed (8-11 yrs.) Permanent (growing) Discontinuation Class III maxillary deficiency Facemask Class III mandibular progChincap nathism Deep bite Open bite (skeletal) Limited treatment TMD treatment Early mixed (6-8 yrs.) Maxillary expansion (ME) E-space control expansion Headgear/springs functional Fixed appliances Fixed appliances Fixed appliances Fixed appliances Space maintenance/biteplate Headgear/vertical corrector/tooth guidance Fixed appliances Fixed appliances Any time Conservative approach on detection *Treatment may continue from one period to the next if necessary. Care should be taken to avoid patient burnout. 560 American Journal of Orthodontics and Dentofacial Orthopedics Volume 108, No. 5 m e n t of 11/2 to 2 y e a r s t h a t starts in t h e l a t e m i x e d dentition, especially on the eruption of the upper first p r e m o l a r s . 2 Finally, any l i m i t e d t r e a t m e n t (single t o o t h crossbite, d i a s t e m a , spacing) c a n be a d d r e s s e d individually p e r p a t i e n t at any age. A n y d y s f u n c t i o n a n d / o r p a i n to t h e t e m p o r o m a n d i b u l a r j o i n t s h o u l d b e a d d r e s s e d as s o o n as it is d e t e c t e d . F i x e d a p p l i a n c e t h e r a p y s h o u l d use t h e n e w technology wires, springs, a n d efficient b r a c k e t designs. I n conclusion, t h e objectives of any t r e a t m e n t b e f o r e e r u p t i o n of all p e r m a n e n t t e e t h a r e to c o r r e c t t h e s k e l e t a l d i s c r e p a n c y b e t w e e n t h e jaws a n d i m p r o v e f u n c t i o n a n d facial esthetics by allowing t h e m to d e v e l o p normally, to c r e a t e an ideal o v e r b i t e a n d overjet r e l a t i o n s h i p , to align t h e a n t e r i o r p e r m a n e n t t e e t h (incisors) a n d r e d u c e t h e c h a n c e of t r a u m a to t h e s e t e e t h , to i m p r o v e t h e w i d t h o f t h e d e n t a l a r c h e s a n d to r e d u c e t h e risk for (1) e x t r a c t i o n o f p e r m a n e n t t e e t h on n o r m a l e r u p t i o n of t h e full p e r m a n e n t d e n t i t i o n a n d (2) for surgery (in severe cases). U n a t t e n d e d o r t h o d o n t i c p r o b l e m s c a n l e a d to i m p a i r m e n t s in s p e e c h , chewing, a n d loss or t r a u m a of t e e t h . O r t h o d o n t i c s can e n h a n c e a p e r s o n ' s s e l f - e s t e e m as t r e a t m e n t b r i n g s t e e t h , jaws, a n d soft tissue into c o r r e c t position. This is a c c o m p l i s h e d with a g o o d level of c o o p e r a tion t h a t a child d e m o n s t r a t e s d u r i n g this p e r i o d . A t r e a t m e n t will b e successful only w h e n t h e p a t i e n t a n d t h e g u a r d i a n a r e satisfied a n d h a p p y a b o u t t h e r e s u l t of t h e r a p y . This is always accomp l i s h e d in an e n v i r o n m e n t of caring t h a t o u r y o u n g patients need. REFERENCES 1. McNamara JA Jr, Brudon WL. Orthodontic and orthopedic treatment in the mixed dentition. Ann Arbor: Needham Press, 1993. 2. Gianelly AA. Paper presented at the combined Orthodontic-Pedodontic conference, Jan. 1993. 3. Gianelly AA, Bednar J, Dietz VS. Japanese NiTi coil used to move molars distally. AM J ORTHOD DENTOFAC ORTHOP 1991;99:564-6. Viazis 561 4. Miura F, Mogi M, Ohura Y, Karibe M. The super-elastic Japanese NiTi alloy wire for use in orthodontics. AM J ORTHOD DENTOFAC ORTHOP 1988;94:89-96. 5. Gianelly A. Class II nonextraction treatment using Sentalloy coils. Summarized by Hawley BP, P C S O Bull 1991:50-1. 6. Bishara SE, Staley RN. Maxillary expansion: clinical implications. AM J ORTHOD DENTOFACORTHOP 1987;91:3-14. 7. Osborn WS, Nanda RS, Currier GF. Mandibular arch perimeter changes with lip bumper treatment. AM J ORTHOD DENTOFAC ORTHOP 1991;99:527-32. 8. Nevant CT, Buschang PH, Alexander RG, Steffen JM. Lip bumper therapy for gaining arch length. AM J ORTHOD DENTOFAC ORTHOP 1991;100:330-6. 9. Cetlin NM, Ten Hoeve A. Nonextraction therapy. J Clin Orthod 1983;17:396-413. 10. Ten Hoeve A. Palatal bar and lip bumpers in nonextraction treatment. J Clin Orthod 1985;19:272-91. 11. Proffit WR. Contemporary orthodontics. St. Louis: CV Mosby, 1986. 12. Woodside DG, Metaxas A, Altuna G. The influence of functional appliance therapy on glenoid fossa remodeling. AM J ORTHOD DENTOFAC ORTHOP 1987;92:181-9. 13. Pancherz H. A cephalometric long-term investigation on the nature of Class II relapse after Herbst appliance treatment. AM J ORTHOD DENTOFACORTHOP 1991;100:220-33. 14. Mitani H. Occlusal and craniofacial growth changes during puberty. AM J ORTEIOD 1977;72:76-84. 15. Sakamoto T. Effective timing for the application of orthopedic force in the skeletal Class Ill malocclusion. AM J ORTHOD 1981;80:411-6. 16. Mitani H. Prepubertal growth of mandibular prognathism. AM J ORTHOD 1981;80:546-53. 17. Graber LW. Chincup therapy for mandibular prognathism. AM J ORTHOD 1977;72:23-41. 18, Graber TM. Thumb and finger sucking. AM J ORTHOD 1959;45:259-64. 19. Viazis AD. The triple-loop corrector. AM J ORTHOD DENTOFAC ORTHOP 1991;100:91-2. 20. Turley PK. Orthopedic correction of Class lII malocclusion with palatal expansion and custom protraction headgear. J Clin Orthod 1988;22:314-25. 21. Lee PK. Behavior of erupting crowded lower incisors. J Clin Orthod 1980;14:24-33. 22. Creekmore TD. Teeth want to be straight. J Clin Orthod 1982;16:745-6. Reprint requests to: Dr. Anthony D. Viazis 1307 8th Ave., Suite 403 Ft. Worth, TX 76104