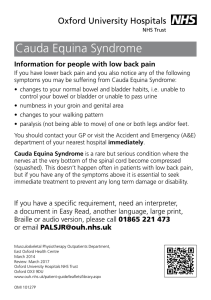
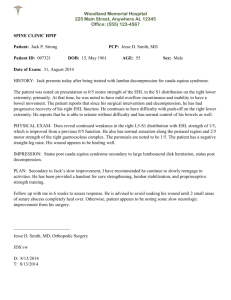
Script Rubric Topic Covered: Cauda Equina Syndrome Karina Monticone ADVANCED CLINICAL TASK QUESTIONS Below are specific task questions pertaining to: ScientificConcepts, History and Physical, Diagnostic Studies, Clinical Intervention, Clinical Therapeutics, and Health Maintenance. Scientific Concepts What are the underlying processes or pathways responsible for the specified topic? o The cauda equina gets its name from Latin for "horse’s tail," because the nerves at the end of the spine visually resemble a horse’s tail as they extend from the spinal cord, through the lumbar spine and over the sacrum, and down the back of each leg (Cauda Equina Syndrome 2021). o The cauda equina consists of about 10 pairs of nerve roots, some of which combine to form larger nerves in the lower body—one example of which is the sciatic nerve (Cauda Equina Syndrome 2021). o The cauda equina is responsible for sensory and motor innervation to the pelvis and lower limbs, as well as bowel and bladder function. If the cauda equina is damaged by inflammation or compression in the low back, symptoms may be severe and may develop quickly. Early medical attention and treatment are crucial for making as full a recovery as possible (Cauda Equina Syndrome 2021). o What are the most likely complications for the specified topic? o Complications: (Gardner et al., 2011) Bladder and bowel dysfunction Sexual dysfunction Sciatic pain Saddle and groin anesthesia Sensory abnormality in the lower body Muscle weakness in the lower body Paralysis Thromboembolic phenomena Neurogenic bladder/bowel Pressure ulcers Heterotopic ossification Osteoporosis Chronic neuropathic pain Spasticity/contractures Recurrent urinary tract infections Urethral stricture Bladder calculi Depression History and Physical Describe key point(s) pertaining to the etiology of disease/disorder assigned o The incidence of Cauda Equina Syndrome is rare (annual incidence between 1.5 to 3.4 cases per million people). There is an estimated prevalence of ~ 1 in 65,000 and about 1000 new cases per year in US. It occurs with 3% of all lumbar disc herniations (Gardner et al., 2011). o It happens to be more common in males. With the 4th decade (30s) of life being the most common age group. It most commonly occurs at the L4-5 level (Gardner et al., 2011). o Cauda equina syndrome (CES) is usually characterized by these so-called 'red flag' symptoms: Severe low back pain (LBP) Sciatica: often bilateral but sometimes absent, especially at L5/S1 with an inferior sequestration Saddle and/or genital sensory disturbance Bladder, bowel and sexual dysfunction List signs and symptoms and unique features of disease/disorder o Urinary retention: the most common symptom. The patient's bladder fills with urine, but the patient does not experience the normal sensation or urge to urinate (Gardner et al., 2011). o Urinary and/or fecal incontinence. The overfull bladder can result in incontinence of urine. Incontinence of stool can occur due to dysfunction of the anal sphincter. o "Saddle anesthesia" sensory disturbance, which can involve the anus, genitals and buttock region (Gardner et al., 2011). o Weakness or paralysis of usually more than one nerve root. The weakness can affect lower extremities (Gardner et al., 2011). o Pain in the back and/or legs (also known as sciatica) (Gardner et al., 2011). o Sexual dysfunction (Gardner et al., 2011). What is the most likely patient stated history finding for the specific topic? o Patients will likely come in (Cauda Equina Syndrome 2021): Spinal lesions and tumors Spinal infections or inflammation Lumbar spinal stenosis Violent injuries to the lower back (gunshots, falls, auto accidents) Birth abnormalities Spinal arteriovenous malformations (AVMs) Spinal hemorrhages (subarachnoid, subdural, epidural) Postoperative lumbar spine surgery complications Spinal anesthesia Diagnostic Studies Describe the diagnosis/lab studies related to the topic with expected findings o Diagnosis (Cauda Equina Syndrome 2021) o AP, lateral Radiographs indications if high suspicion of CES study of choice is MRI can obtain radiographs but initiate process of obtaining MRI immediately findings usually normal with most common cause of lumbar disc herniation may see other cause of spinal canal stenosis o burst fractures o high-grade developmental spondylolisthesis (intact-lamina) o MRI indications study of choice to evaluate neurologic compression o must be performed emergently if cauda equina syndrome is suspected ideally obtained within 1-2 hours of presentation to ER findings often reveals large central disc herniation with complete spinal canal obliteration presence of spinal stenosis epidural hematoma epidural abscess o CT myelography indications study of choice if patient unable to undergo MRI o e.g. pacemaker, MRI-incompatible implants findings sagittal and axial reconstructions can reveal space-occupying lesion partial or complete blockage of contrast o CBC, ESR, CRP concern for infectious etiology (i.e. epidural abscess) o Urodynamic studies preoperative postvoid residual volumes (PVR) recommended to be obtained prior to decompression but not at delay of decompression normal post-void residual volume is less than 50 to 100 mL o PVR values < 200 ml with a 97% negative predictive value for cauda equina syndrome postoperative postvoid residual volume assessment for return of bladder function What is the most appropriate initial diagnostic study for the specific topic? o The initial diagnosis of cauda equina syndrome is made based on findings from the individual's history, symptoms, and physical exam. The physical exam includes testing muscle strength of the lower extremities, evaluating sensation to touch and pain, especially around the groin (perineum), checking the lower extremity reflexes, and evaluating rectal tone, sensation, and reflex (Hsu, 2018). o Imaging studies helpful in the diagnosis include plain x-ray films of the lower back to assess for evidence of trauma or severe arthritis (degenerative changes) (Hsu, 2018). What is the most appropriate definitive diagnostic study for the specific topic? o MRI is the definitive diagnostic test that produces three-dimensional images of body structures using magnetic fields and computer technology (Hsu, 2018). o MRI produces images of the spinal cord, nerve roots and surrounding areas (Hsu, 2018). Clinical Intervention What is the most appropriate initial intervention for the specified topic? o Surgery is truly the initial and definitive intervention (Hsu, 2018). o Cauda equina syndrome is best treated with decompression by a lumbar laminectomy, but a lumbar microdiscectomy may be used given a patient’s unique situation (Hsu, 2018). What are the steps of management for the specified topic? o Once the diagnosis of CES is made and the etiology established, urgent/emergent surgery is usually the treatment of choice. The goal is to free up the compressed nerve roots and give them the best chance of recovery possible. Left untreated, CES can result in permanent paralysis and incontinence (Hsu, 2018). Would there be any appropriate non-pharmacological modalities appropriate for the specified topic (i.e., therapies, counseling, referrals to specialist)? o Prompt surgery is the best treatment for patients with CES (Hsu, 2018). o Treating patients within 48 hours after the onset of the syndrome provides a significant advantage in improving sensory and motor deficits as well as urinary and rectal function (Hsu, 2018). o Any non-pharmacological modalities would not be appropriate. When would a referral be appropriate for the specific topic and to whom would the referral be to? o The only referral would be for a neurosurgeon to perform emergent surgery. Clinical Therapeutics List treatments (gold standards- MOST DEFINITIVE TREATMENT, alternative treatments, etc.) for the disease/disorder: o Emergent surgical decompression (Segun Toyin Dawodu, 2021). microdiscectomy (unilateral laminotomy, medial facetectomy, diskectomy) laminectomy (bilateral laminectomy and medial facetectomy) laminectomy with fusion (rarely indicated) o Corticosteroids modify the body's immune response to diverse stimuli (Segun Toyin Dawodu, 2021). Methylprednisolone (DepoMedrol, Medrol, Medrol Dosepak) This agent decreases inflammation by suppressing migration of polymorphonuclear leukocytes and reversing increased capillary permeability. This prevents further worsening of injury. Treatment must be started within 8 h of injury; treatment apparently has no benefit if started later than 8 h after injury. Late treatment may have detrimental effects (Segun Toyin Dawodu, 2021). o Anti-inflammatory medication may prevent worsening of injury (Segun Toyin Dawodu, 2021). o Anticoagulants provide prophylaxis against thrombotic complications (Segun Toyin Dawodu, 2021). o Use of antispasticity medications to reduce muscle tone is encouraged (Segun Toyin Dawodu, 2021). o Bisphosphonates may be beneficial in patients with bony lesions (Segun Toyin Dawodu, 2021). o Phosphodiesterase type 5 inhibitors treat erectile dysfunction (ED) (Segun Toyin Dawodu, 2021). What is the dosing regimen for the treatment of choice? o While it is not a treatment of choice, it is a drug you can give to help with inflammation. High dose methylprednisolone (kg/30 mg) can be administered by intravenous infusion in the 8th, 16th and 24th hours after injury followed by infusion of the same dosage every 6 hours for 24 hours (Villavicencio, 2019). o Administration of ganglioside GM1 sodium salt beginning within 72 hours of injury may be beneficial; the dose is 100 mg IV qd for 18-32 days (Villavicencio, 2019). What is the treatment of choice if patient is allergic or contraindicated to the most definitive first-line medication? o Surgery is not a contraindication or something that can be allergic to. If one method of surgery doesn’t work out, there are three other types of surgical procedures that can be tried (Villavicencio, 2019). What is the next best treatment if the treatment of choice has not worked or is not an option to choosefrom? o The best outcome for patients with CES involves surgical decompression (e.g., microdiscectomy, wide laminectomy, wide laminectomy with discectomy). Once stabilized, physical therapy may be a part of the patient's recovery program. What are the medication/treatment contraindications for the specified topic? o There are no treatment contraindications. Health Maintenance Are there screening tests recommended for patients with the disease/disorder, if so specify below? o There are no screening tests since epistaxis is an emergent issue. Are there (and if so list below) immunizations that could be used for patients with the disease/disorder? o There are no immunizations. Important information on items of patient counseling, disease prevention, and education that should be discussed with a patient with this disease/disorder: o Recovering from a spinal decompression procedure such as lumbar laminectomy or discectomy can take about four to six weeks. This timeline depends on individual health factors such as age, general health and the cause of the compression. During that time, activities are gradually increased over time while the incision heals and stitches are removed. People who have sedentary jobs that don’t require much lifting or bending can generally get back to work in about four weeks, but people with physically demanding jobs might need to recover for up to four months before returning to work (Villavicencio, 2019). o Healing from the surgery itself is just one part of recovering from cauda equina syndrome, though. The affected nerves must also recover, and that can continue long after incisions are healed (Villavicencio, 2019). o To help with recovery, patients with persistent weakness or instability in the legs, or trouble with bowel and bladder functions, might need physical or occupational therapy, assistive devices like walkers or canes, and bladder retraining during the weeks and months it can take for nerves to recover from damage (Villavicencio, 2019). o Patients with persistent nerve damage causing severe bladder and bowel problems may need to learn strategies such as self-catheterization and techniques for managing bowel problems while nerves heal – a process that can take 18 months to two years, or longer. In some cases, nerve damage can be permanent, and patients need assistance or adaptive devices for daily living (Villavicencio, 2019). o With prompt follow-up and treatment from experienced New Jersey neurosurgeons, most people with cauda equina syndrome are able to recover significant function in the legs and lower body. Your neurosurgeons in the tristate area can work with you and your family to create the cauda equina syndrome recovery treatment plan that’s right for your unique circumstances (Villavicencio, 2019). Visual Image/Chart for the Disease/Disorder Post images/pictures/charts unique to disease/disorder that you find helpful for yourself and for your peers to visually understand the disease/disorder: Citations Cauda Equina Syndrome. Cedars-Sinai. (2021). Retrieved November 25, 2021, from https://www.cedars-sinai.org/health-library/diseases-and-conditions/c/cauda-equinasyndrome.html. Gardner, A., Gardner, E., & Morley, T. (2011, May). Cauda equina syndrome: A review of the current clinical and Medico-legal position. European Spine Journal. Retrieved November 25, 2021, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3082683/. Hsu, P. (2018). Acute lumbosacral radiculopathy. UpToDate. Retrieved November 25, 2021, from https://www.uptodate.com/contents/acute-lumbosacral-radiculopathy-pathophysiologyclinical-features-anddiagnosis?search=cauda+equina+syndrome&source=search_result&selectedTitle=1~99&usa ge_type=default&display_rank=1. Segun Toyin Dawodu, J. D. (2021, October 16). Cauda equina and conus medullaris syndromes. Background, Anatomy, Pathophysiology. Retrieved November 25, 2021, from https://emedicine.medscape.com/article/1148690-overview. Villavicencio, A. (2019). Cauda equina syndrome. Spine. Retrieved November 25, 2021, from https://www.spine-health.com/conditions/lower-back-pain/cauda-equina-syndrome.