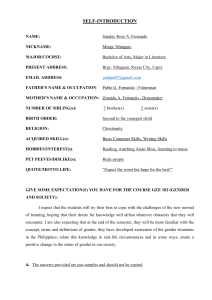
MSK Maneuvers / Diagnostics Is the joint pain: 1. Articular or extraarticular? 2. Acute (<6 wks) or Chronic (>12 wks)? 3. Inflammatory or non-inflammatory? 4. Localized or diffuse? -Inspect and palpate joints immediately above and below the painful areas -If no Sx, Active ROM testing can be done bilaterally at the same time -Examine unaffected side first to develop sense of what is normal for pt. Fernando Vélez Taneil Gibson Treatment Shoulder pain -Determine if pain is from shoulder or distant site ● Shoulder mvmt → pain +/- stiffness and Limited ROM = shoulder ● disorder Normal shoulder exam = referred pain -Is pain Periarticular or Intraarticular? Check Passive and Active ROM ● Active ROM painful but no passive ROM pain = Periarticular issue ○ tendonitis, bursitis ● Active and Passive ROM painful = Intra-articular issue ○ arthritis of glenohumeral joint ○ *Exception ~ impingement syndromes. *Spurling maneuvers: - Extends patient’s neck. - Rotate head towards affected shoulder - Place axial load on the cervical spine - Test is positive if limb pain or paresthesias are produced and the test should be then stopped. - Production of neck pain alone in response to the Spurling maneuver is nonspecific and constitutes a negative test. - The Spurling test has high specificity for the presence of cervical radiculopathy (nerve root compression), but has a low to moderate sensitivity. -Referred pain from Cervical Spine: - neck pain and stiffness - decreased neck ROM (x6) -Up, Down, Left, Right, Ear-toshoulder (left & right) - pain → extending below the elbow - **Conduct Spurling’s Test Rotator Cuff Disorders ● ● ● ● Fernando Vélez Taneil Gibson Rotator Cuff tendonitis Rotator Cuff tear Subacromial bursitis Impingement syndromes ○ From RC or subacromial bursitis. Special test to assess rotator cuff (Impingement) - - Painful arc test - Active ROM triggers pain between 60-120 degrees on abduction. Hawking’s test - Pain when examiner internally rotate the shoulder and elbow Conservative treatment - Ice - Avoid repetitive overhead activities. - Lifting heavy objects - NSAIDS & Acetaminophen. Shoulder Steroid injection - Single glucocorticoid injection to those who fail a - flexed at 90 degrees. - **most sensitive Neer test - Pain with a passive flexion of the shoulder with fixed/stabled scapula (arm pronated). - 90 deg = mild - 60-70 deg = moderate - <45 deg = severe Maneuvers for rotator cuff (Tear) ~ (Passive Strength tests) - Drop arm test - Supraspinatus tear External rotation lag - Weak → Unable to maintain position Supra/infraspinatus and teres minor tear Internal rotation lag - Weak → Unable to maintain - - - position Subscapularis tear Maneuvers for rotator cuff (Composite: Tear & Tendonitis) (Active against resistance) - Empty can / Jobe’s test - Supraspinatus - Pain → Tendonopathy - - Weakness +/- pain → Tear External rotation - Infraspinatus, Teres minor - Pain → Tendonopathy - Fernando Vélez Taneil Gibson Weakness +/- pain → Tear 4-6 weeks of conservative measures or initially to those whose pain is severe. For Full Thickness tear - Orthopedic referral and immediate surgery for healthy individuals. - Conservatively in elderly patients or with major comorbidities. - Partial tear that do not respond to conservative treatment therapy may need surgery. - Internal rotation - Subscapularis - Pain → Tendonopathy - Weakness +/- pain → Tear Imaging Tendinopathies - MSK Ultrasound (Gold standard) - MRI (If Dx: is uncleared) Imaging RC Tears - Pain radiograph - Can show migration relative to position. - MSK Ultrasound - Highly sensitive - MRI - Accurate for full thickness and partial tears is less sensitive. Bicep Pain Hx: Bicep Tendon Palpation ● ● ● Pain on anterior shoulder with radiation distally over the bicep muscle. Pain aggravated by lifting, pulling or repetitive overhead activities. May coexist with rotator cuff issues. Yergason’s Test (Bicipital tendonitis) - Pt’s elbow flexed to 90 deg. Thumb up and elbow on the pr’s side. - Examiner: place one hand on bicipital groove, the other hand on patients wrist. - Examiner attempts to resist active supination and elbow flexion by the patient. Speed’s test - Pt’s forward flexes shoulder with elbow in slight flexion and full supination. - Examiners feels biceps long head. - Pt’s actively flexes arm against examiners downward resistance. Fernando Vélez Taneil Gibson Initially - NSAIDS x7d - Physical therapy - Activity modification Subsequent (If no improvement) - Conservative treatment for 6 weeks. - Consider Ultrasound guided glucocorticoid steroid injection onto the sheath of the long head of the biceps tendon. Patient education after glucocorticoid injection. - Must rest 72 hrs due to rupture risk. Elbow pain **Epicondylitis and Olecranon bursitis = rarely affect elbow ROM! Hx **Normal ROM testing of elbow RULES OUT involvement of elbow joint itself Medial Epicondylitis -Pain localized to the lateral epicondylar process -Aggravated by repetitive contraction of the wrist extensors -Pain localized to medial epicondyle -Aggravated by actions that contract wrist flexors - Golf - Repetitive shaking hands and use of forearm/wrist - Carpenters, Politicians, Gardeners, Tennis players PE DDx Fernando Vélez Taneil Gibson Lateral Epicondylitis -Normal elbow ROM -Pain at lateral epicondyle -Pain with resisted wrist extension, or wrist pronation/ supination with elbow in full extension -Pain with gripping -Decreased grip strength -Normal elbow ROM -Pain at medial epicondyle -Pain with resisted wrist flexion, supination/ pronation with elbow in full extension -Pain with gripping -Decreased grip strength 1. Cervical Radiculopathy a. Referred pain from the neck b. No pain with elbow mvmt but pain moving shoulder or neck 2. Elbow arthritis a. Elbow joint pain b. May see joint effusion c. ROM limited at elbow 3. Fracture 1. Ulnar neuritis a. Ulnar nerve pain b. Radiation into the ulnar side of the hand with sensory and motor Sx in 4th and 5th fingers 2. Cervical Radiculopathy a. Referred pain from the neck b. No pain with elbow mvmt but pain moving shoulder or neck 3. Elbow arthritis a. Elbow joint pain Olecranon bursitis -Elbow swelling with warmth and redness. Causes: -Trauma -Sepsis -RA -Gout -Can fully extend the elbow since elbow joint not involved b. Joint effusion may be seen c. ROM limited in elbow 4. Fracture Dx and Tx Dx: Dx: ● ● Hx and PE X ray only needed if fracture suspected ● ● ● ● Activity modification Counter force bracing Physical therapy Topical and/or oral NSAIDS Tx: Wrist and Hand pain Hx: ● Fernando Vélez Taneil Gibson Hx and PE X ray only needed if fracture suspected ● ● ● ● Activity modification Counter force bracing Physical therapy Topical and/or oral NSAIDS Tx: Carpal Tunnel Syndrome - Median nerve compression within the carpal tunnel - Bilateral symptoms >50% - Diseases/Risk factors: - Obesity - Female gender - Pregnancy - Hypothyroidism - DM - Connective tissue disease ● ● ● Pain worse at night and with repetitive actions Pain and paresthesias limited to the median-innervated fingers ○ Some pain/tingling in hand, wrist ○ Some radiation to arm and all 5 fingers P.E: ● ● ● Tx: Hyperalgesia of median nerve distribution and weakness of thumb abduction and opposition Thenar muscle atrophy- severe disease Phalen and Tinel’s test positive ● ● ● ● PROTECT the joint Aspirate fluid NSAIDS Tx underlying condition - Avoid repetitive hand and wrist movements - Neutral position wrist splinting- used full time - Local steroid injection (10 wks) = short term relief - Oral steroids for 2 wks= relief for 1 mo - NSAIDS - Surgery if: - Nerve testing → - Severe disease Muscle wasting Failure to respond to conservative tx - Knee pain Hx: Location of pain Mechanism of Injury (MOI) Duration of pain Other sx: ● ● ● ● ● ● Stiff joint Swelling Locking Instability Constitutional Sx (fever, weight, fatigue) Joint redness P.E. - - ● Inspect Palpate Active ROM and Passive ROM (if indicated) Maneuvers for knee ligaments and menisci: - Anterior drawer/ Lachman - Posterior drawer - Valgus/ Varus stress - Thessaly/Apley Grind/ McMurray/ Bounce/ SquatDuck walk Effusions: - Bulge - Ballotment - Balloon Diagnostics: - Arthrocentesis - Septic knee - NOT if ligament or meniscus tear - X-Ray - Suspected trauma fracture - OA signs - Looking for foreign body - MRI - if considering surgery or persistent Sx Fernando Vélez Taneil Gibson ● ● ● ● Intolerable pain Due to another disease; treat the disease Restrict weight-bearing activities, use crutches Knee brace Ice, NSAIDS +/- Tylenol Rehab- once pt has painless, full ROM Orthopedic referralarthroscopy - ACL tear MOI -Rapid deceleration + pivot -Knee hyperextension -Popping sound, knee instability, pain= complete tear Meniscal tear*** Plain Radiograph - Acute injury - Meniscal tear PCL tear -Posteriorly directed force on the knee MCL -Direct valgus (medial) force to an extended knee (e.g. motor accident when knee is flexed and strikes dashboard) LCL -Direct varus (lateral) force to a extended leg *less frequent than MCL Meniscus Acute tear: Twisting knee when foot is planted and knee is flexed Can continue to participate in activity Degenerative tear: Can develop with minimal/ no trauma Hx -Joint instability -Medial knee pain -Swelling -Lateral knee pain and swelling -May lock, catch or giveout - Small tear → insidious onset of pain/swelling (stiffness) over 24 hrs - Severe tear → significant pain, ↓ ROM, tearing and pop at time of injury Fernando Vélez Taneil Gibson - Weeks later→ popping, locking, catching and giving out P.E -Large effusion -Lachman and Anterior drawer= ↑ laxity -Posterior drawer test=↑ laxity - POSITIVE Sag/ Godfrey sign -Medial joint line tenderness -Valgus stress= ↑ -Lateral joint line tenderness -Varus stress= ↑ laxity laxity - Plain Radiograph followed by Ottawa Knee Rule. - MRI for patient with persistent Sx despite the initial treatment. ( Dx: Low Back pain Acute < 4 wks Subacute 4-12 wks Chronic >12 wks -Spondylosis ● Degenerative arthritis of spine -Spondylolisthesis ● Anterior displacement of a vertebral body relative to the one below -Spondylolysis ● Fracture of the pars inter-articularis -Spinal stenosis ● Local, segmental or generalized narrowing of vertebral canal by bone or soft tissue. -Radiculopathy ● Impaired nerve root → radiating pain, numbness, tingling or muscle weakness -Sciatica Fernando Vélez Taneil Gibson -Joint line tenderness and effusion -Gait observation to assess impact -Loss of smooth passive/ active motion -Inability to squat or kneel -Palpable pain with McMurray maneuver -Pain elicited by Thessaly, Bounce and Apley grind tests History -Location -Neurologic deficits? -Acute vs Chronic Sx -Character of pain -Worse with or without activity? -Psychosocial risk factors? **Always ask Bowel or bladder issue when there is back pain! Imaging: - Cancer or Vertebral infection- Plain film, MRI, ESR - Cauda equina syndrome or Severe Progressive neurologic deficits Acute Lower Back Pain: - NO prolonged bed rest - Heat - Tylenol, NSAIDS, Muscle relaxants, Benzos, Tramadol, opioids (sparingly!) - Spinal manipulation (*NOT physical therapy) - Follow up in 2-4 wks Subacute/Chronic Back pain: - Remain active - Tylenol, NSAIDS, TCA’s, Benzos, Tramadol, Opioids (Sparingly!) ● Pain, numbness, tingling in the distribution of the sciatic nerve, radiating down the posterior or lateral aspect of the leg. -Cauda equina syndrome ● Loss of bowel and bladder control ● Numbness in groin and saddle area of perineum ● Associate with weakness of the lower ext - MRI or EMG Vertebral Fx - Plain film Ankylosing Spondylitis - Plain film and ESR; Seronegative **Cervical spine nerve roots- exit ABOVE the vertebrae Thoracic and Lumbar nerve roots exit BELOW the like-named vertebrae - Nerve exiting at level L4-L5 is L4 PE: nerve but a disc protrusion→ L5 nerve root impingement syndromes. Categories: 2. 3. 4. Fernando Vélez Taneil Gibson Non specific pain (85%) a. Lumbar strain Pain with Radiculopathy or Spinal Stenosis a. Herniated disc b. Nerve root impingement Pain assc. With another specific spine disorder a. Cancer b. Compression fx (fracture) c. Infection d. Ankylosing spondylitis Pain referred from outside of the back a. Pancreatitis b. Nephrolithiasis c. AAA d. Pyelonephritis - spondyloarthropathy that initially targets sacroiliac joints in young males (15 - 35 yrs). ● ● Skin inspection Inspection- symmetry, bulk, posture ● ● ● Palpation/ ROM Percussion Lumbar disc herniation/ nerve root impingement Straight leg raise (SLR) ● ○ ○ 1. - - Rules out disc radiculopathy and indicates herniated disc ● Crossed straight leg raise ● Rectal exam- evaluates Cauda equina syndrome ○ - *hold pt at the hip when asking them to rotate to prevent them from using the knee/ankles to rotate. Surgery candidates: - Disk herniation causing persistent radiculopathy = Discectomy - Painful spinal stenosis= decompressive laminectomy - Cauda equina syndrome= decompression Specific for radiculopathy *If both SLR and C-SLR are positive it is indicative of Disk Herniation *0-5 for muscle grading (e.g. ⅗) * 0-4 for reflex grading (2+ is normal) Spinal manipulation, massage, Physical therapy, yoga, acupuncture, cognitive behavioral therapy Systemic glucocorticoids for SHORT TERM pain relief, not treatment Trigger point injections of local anesthetic Epidural injections of steroid- Chronic LBP + Sciatica or Radiculopathy **MUST KNOW: Red Flags for serious conditions: ● ● ● ● Hx or new diagnosis of cancer (breast, lung, MM, prostate, renal cell) Unexplained weight loss Failure to improve after 1 mo. No relief with bed rest; pain worse at night or when lying down Suggests→ Metastatic disease to the spine Fernando Vélez Taneil Gibson ● ● Fever Pain worse at night or when lying down ● Hx of IVDA ● Hx of UTI ● Hx of skin infection Suggests → infection (osteomyelitis, epidural abscess) ● ● ● ● ● Morning stiffness Pain not relieved when supine Pain persistent for >3mo Gradual onset Involvement of other joints Suggests → Inflammatory/ Rheumatologic condition (Ankylosing spondylitis, RA etc) ● Hx of Trauma ● Hx of Glucocorticoid use ● Hx of Osteoporosis Suggests → Compression fracture ● Severe leg pain, often bilateral ● Pain improved when seated ● Pseudoclaudication (worsened pain walking, relief with sitting) Suggests→ Spinal Stenosis Fernando Vélez Taneil Gibson ● ● Sciatica Increased pain with cough, sneeze or Valsalva Suggests→ nerve root irritation (radiculopathy) from herniated disc ● ● ● Bowel or bladder dysfunction Sexual dysfunction Saddle anesthesia sensory loss (S3-5) ● Bilateral absence of ankle reflex ● Rapidly progressive neurologic deficits Suggests → Cauda equina syndrome (aka massive midline disc herniation) Rheumatology History **GENERAL CONCEPTS P.E. Terminology Arthralgiasgeneralized joint aches and pains without evidence of arthritis Tenosynovitisinflammation of a tendon or tendon sheaths Myositisinflammation of the muscles Arthritis - joint pain, stiffness, swelling, dec. ROM, deformity, warmth/erythema Enthesitisinflammation at the site of insertion of tendons, ligaments and synovium into bone Serositisinflammation of the serous tissues of the body Synovitisinflammation of the synovium Myalgia- generalized muscle aches and pains Gel phenomenonbrief periods of daytime stiffness/ gelling following inactivity; lasts 3060 mins (seen in OA) Stiffness- ≠ Pain !! ● ● ● Fernando Vélez Taneil Gibson Diagnosis/Labs Joint patterna. Symmetric? i. Gout- asym ii. RA- sym b. Inflammatory? Joints involveda. Number i. Mono- Gout ii. Oligo (2-4)- Reactive arthritis iii. Poly (5+)- SLE, RA, Psoriatic symmetric polyarthritis b. Size i. Small- Rheumatoid arthritis (not DIP) ii. Large- Reactive arthritis iii. Spine- ankylosing spondylitis Extra-articular manifestations? ● Arthrocentesis results a. Color b. Transparency c. Viscosity d. Cell count i. ii. iii. ● Non-inflamm= OA Inflamm- RA, Gout Septic- Bacterial infxn e. Crystals f. Gram stain and culture g. PCR- Lyme disease Lab results a. Inflammation- ESR, CRP, Complement b. AutoAb’s i. ii. iii. iv. ● RF- RA and others ANA- Lupus and others Anti-CCP- RA Anti-ds DNA- SLE Imaging a. Plain Xray- RA, OA b. CT- Bony abnormalities c. MRI- soft tissue abnormalities, inflammation, fluid collection d. US- soft tissue abnormalities (bursitis, synovitis, tendonitis, joint fluid) Treatment -Anti-inflammatory - NSAIDS - Glucocorticoids - Colchicine -Analgesics - Acetaminophen - Opiates - Gabapentin, TCA, SNRI - Topicals→ Capsaicin, Lidocaine -DMARDS (disease modifying anti-rheumatic drugs) - Nonbiologic: -Methotrexate -Hydroxychlororquine -Sulfasalazine -Leflunomide -Azathioprine -Cyclophosphamide -Mycophenolate Mofetil -Cyclosporine -Apremilast - Biologic: -TNFa inhibitors -Non TNF- Rituximab, Anakinra a. Constitutional Sx i. RA= low grade fever b. Dermatologic i. Lupus= malar rash c. Inflamm eye Dx i. Spondyloarthropathies = Uveitis d. Internal Organs i. Lupus= carditis, nephritis Rheumatoid arthritis Presents as bilateral, symmetric, inflammatory polyarthritis Tenderness and swelling of joints - ● -Extra-articular manifestations: soft tissues, skin, vessels, heart, lung, ● muscles Symmetric joint involvement - Anti-Cyclic citrullinated peptide Ab’s (Anti CCP Ab)- 95% specific Active signs of inflammation for 6wks - ↑ ESR and CRP -Produces non-suppurative synovitis ● Mild fusiform soft-tissue PIP swelling= early RA - CBC -30-60 y/o; Female: Male=3:1 ● ● Pain, swelling, warmth in 3+ small ● ● joints of hands/ feet ● ● ● Fernando Vélez Taneil Gibson Skin: ○ ○ → progress to larger joints ○ Swan necking, ulnar deviations, MCP synovitis ● DIP rarely involved Morning stiffness ● >1 hr Insidious onset Fever, malaise, depression, myalgia Eyes: ○ Rheumatoid Factor- 70% - - Pulmonary: ○ Pleuritis ○ Exudative pleural effusion ○ DPLD Normochromic, normocytic anemia Thrombocytosis - - DMARDS ○ Imaging: - Plain films Pyoderma gangrenosum Rheumatoid nodules Keratoconjunctivi tis sicca ● sensitive US - Bony erosions Periarticular osteopenia Subluxations Soft tissue swelling Joint space narrowing MCP and PIP involvement on hand radiograph Synovitis Erosions Non-BiologicMethotrexate ■ ○ Pregnancy test first Biologic-only if inadequate nonbiologic response ● Glucocorticoids - as adjunctive tx ● NSAIDS- adjunctive tx ● Surgery ● Infectious arthritis Arises from hematogenous spread, direct inoculation or contiguous spread from neighboring osteomyelitis, cellulitis or septic bursitis Cardiac: ○ Risk CAD and HF ○ Pericarditis ● ● Fever, chills, rigor Warmth, erythema, pain and swelling of joint Causes: -Staph aureus- MC -Disseminated Gonococcal infection: 1. Vesiculopustular or hemorrhagic macular skin lesions, fever, chills, polyarthralgia 2. Purulent arthritis -Lyme Arthritis - Arthrocentesis CBC Blood cultures ESR, CRP GU, rectal, pharyngeal cxs - If suspect disseminated GC Lyme blood test (ELISA/ Western blot) - If suspect Lyme Imaging - Non specific - May reveal local swelling or joint destruction -Bacterial septic joint= - MRSA: -Vancomycin/ Linezolid -Clindamycin/ Daptomycin - MSSA: - Nafcillin - Cefazolin -Disseminated Gonococcal- IV ceftriaxone (714 d) - Fluoroquinolones - Azithro or Doxy (treats for Chlamydia coinfection) -Lyme arthritis= - Oral doxycycline or Amoxicillin (28 d) -IV Ceftriaxone (28d) if concurrent neuro findings Spondyloarthropathies Fernando Vélez Taneil Gibson A group of 4 disorders: 1. Ankylosing spondylitis 2. Psoriatic arthritis 3. IBD assoc. Arthritis 4. Reactive arthritis ( Reiter’s Syndrome) ...that share the following: Psoriatic arthritis PE: -Inflammatory articular dx + 3 or more of: - Psoriasis - Psoriatic nail dystrophy - Dactylitis/ swelling of entire digit - Negative RF *No specific serologic tests ● ● ● ● RF, Anti-CCP, ANA= negative ↑ ESR and CRP HLA-B27 - can’t confirm or exclude any specific dx Check for chlamydia- some may have asymptomatic - Exercise Steroid injections NSAIDs → then non biologic and - biologic DMARD’s Surgery (if severe, end stage joint/ soft tissue damage) ● ● ● ● Systemic Sclerosis Inflammation of axial skeleton, tendons and entheses Tendone and enthesis calcification HLA-B27 assoc Mucocutaneous, GI and ocular inflammation General Extracutaneous features: -Raynaud phenomenon -Heart burn, dysphagia, diarrhea -HTN, Kidney disease -Dyspnea on exertion -Pulm.HTN, diffuse parenchymal lung disease -Mucocutaneous telangiectasia - Radiologic evidence of juxtaarticular new bone formation ● ● ● ● ● Reduced facial wrinkles, small mouth opening Telangiectasia Calcinosis cutis Sclerodactyly Digital ulcers and pitting ● - Limited Cutaneous Systemic sclerosis (LcSSC) - Thickened skin over hands, face, neck - Sclerodactyly - CREST syndrome features - - Fernando Vélez Taneil Gibson Calcinosis Raynauds Esophageal dysmotility Sclerodactyly Telangiectasia No visceral organ involvement persistent infxn Imaging: ○ Plain films of spine and SI joints = synovitis, axial erosion, new bone ■ ankylosing ○ X-ray= erosive changes ■ psoriatic ANA Anticentromere - LcSSc - CREST Anti-Scl 70 - DcSSC Anti-RNA polymerase III - DcSSC No biopsy because findings are classic and characteristic Therapy based on Organ system: Skin- Pruritus ● Emollients ● Antihistamines MSK- Inflammatory arthritis and Myositis ● MTX ● Glucocorticoids ● Leflunomide Vascular- Raynaud’s ● Avoid cold ● CCB ● Anti-platelets Diffuse cutaneous systemic sclerosis (DcSSc) - Thick skin over chest, abdomen, forearms, upper arms, shoulders + hands, face, neck - Visceral organ involvement Systemic sclerosis sine scleroderma - Fibrosing organ involvement without skin thickening Systemic Vasculitis Giant cell (Temporal) arteritis History: - Scalp pain, HA or tenderness over temporal artery - Weight loss, malaise, low grade fever - Jaw claudication - Blindness (sudden or preceded by amaurosis fugax) GCA ● ● Temporal artery may be erythematous, swollen, tender Diminished pulses GCA - - ↑↑↑ ESR (>50) - Marker of disease activity Temporal artery biopsy definitive diagnosis - Skip lesions can cause false negative GCA ● ● ● ● Polymyalgia Rheumatica - Low grade fever, Fernando Vélez Taneil Gibson PMR PMR PMR ● Tx should never be deferred pending biopsy Oral Prednisone 60mg or 1mg/kg/day for 1 month or until sx resolve, ○ Taper 10% every few weeks IV steroids if visual loss Duration 6-18 months Low dose - - Sjogren’s Syndrome malaise, fever Symmetric proximal pain and stiffness in shoulder, neck and hip - Stiffness in arm 30-60 min; better with activity - Pain worse with activity 2-3x more common than GCA Immune mediated disease -Infiltrative inflammation damages exocrine glands ● ● ● -↑ risk lymphoma -Primary form= no associations -Secondary form- overlaps with RA and SLE - ↑ ESR/ CRP Normal aldolase and CK (muscle enzymes) Normal muscle biopsy CBC - Normocytic anemia - Thrombocytosis MRI/ US: - Bursitis - Synovitis ● ● ● Prednisone (10-20 mg/d) Dramatic improvement w/n 3 days (if not, consider other dx) Can have partial relapse during taper duration= years or indefinitely *inform pt’s of GC side effects: osteoporosis, weight gain, fluid retention, hyperglycemia, myopathy ● ● Keratoconjunctivitis sicca Xerostomia → corneal damage Females 9:1 , ~50y.o -Skin, joints, lung, heart, Gi, kidney, bladder, gyne, heme, PNS/CNS affected May have decreased active and passive ROM (esp active abduction of arms above 90 degrees ) Strength and muscle tone normal No erythema, warmth or swelling and vision ● ● ● impairment Dental caries Dry mucosal membranes Enlarged parotid and lacrimal gland - RF ANA Anti-Ro/ SSA Anti-La/ SSB Lip biopsy for salivary gland inflammation = GOLD standard for Diagnosis *Management depends on Sx’s: -Occular Sicca= - Artificial tears - Topical cyclosporine -Oral Sicca= - Artificial saliva - Sugar free lozenges - Pilocarpine - Good dental hygiene -Vaginal/Skin Sicca = - Lubrication -Arthralgia or rash= - NSAIDs - Hydroxychloroquine - Glucocorticoids (low dose po or Topical) -Lung, Kidney, Nervous system - Glucocorticoids (High dose) -Mtx Fernando Vélez Taneil Gibson - Azathioprine - Cyclophosphamide Mixed Connective Tissue Disease Overlap syndrome that includes features of: - SLE - Systemic sclerosis - +/- Polymyositis ● Anti-U1-Ribonucleoprotein (RNP) antibodies 9:1 female predominance Hx: - Hand edema and synovitis Myositis ↓ esophageal motility and - Fernando Vélez Taneil Gibson fibrosing alveolitis Pulmonary HTN Starts similar to SLE → MCTD Sicca symptoms Pleuropericarditis Membranous nephropathy Trigeminal neuralgia 0 ● ● ● ● Skin ○ Gottron rash ○ Malar rash ○ Photosensitivity ○ Telangiectasia ○ Calcinosis ○ Scleroderma ○ Sclerodactyly Hand edema Synovitis Myositis Trigeminal neuralgia - Anti- U1- RNP Ab = DIAGNOSTIC *Management depends on Sx’s: - ↑ ESR , Leukopenia, -Arthritis and Myositis= - GC - Azathioprine - Methotrexate THrombocytopenia - ANA (speckled pattern) - No ds DNA or Anti-smith Ab (only in SLE!) - Imaging: - High resolution CT of chest - Echocardiography - PFT’s -Raynaud’s Phenomenon Sx - Ca2+ channel blockers -Esophageal dysmotility= - PPI -DPLD = - Cyclophosphamide -Pulmonary HTN= - PDE inhibitors - Enodthelin Neuro Week Cause Motor Neuron disease Upper motor neuron ● “Pyramidal insufficiency” Occur in: ● Neural pathway above anterior horn ● Motor nuclei of cranial nerves ● Brainstem or spinal cord ○ Due to either Stroke, MS, Cerebral palsy or traumatic brain injury Lower motor neuron Occurs in: ● Nerve fibers from the anterior horn of spinal cord ● Cranial motor nuclei to the relevant muscle Amyotrophic Lateral Sclerosis “Lou Gehrig disease” - Fernando Vélez Taneil Gibson Combined UMN and LMN degeneration Fatal Signs/ Symptoms Lab/Investigations Treatment Upper motor neuron - Weakness Slowness Hyperreflexia Spasticity Lower motor neuron - Weakness Atrophy Amyotrophy Fasciculations LMN sx: Dysarthria, dysphagia, fasciculations, asymmetric limb weakness, atrophy. UMN sx: Spastic gait, clonus *No sensory or bowel/bladder deficits Riluzole Headaches Types: 1. Migraine ○ Recurrent attacks ○ Primary neuronal dysfxn → premonitory sx, aura, headache, postdrome Cortical spreading depression: i. Causes aura ii. Activates CN5 afferents iii. Alters BBB permeability 2. Tension 3. Cluster 4. Chronic daily ○ General Dx. is made by Hx, FHx & PE - Imaging (MRI1 or CT2) if Hx, PE & presentation are inconsistent. - LP required unless a benign etiology can be otherwise established. - Psychological state of the pt should be evaluated (relationship between Depression and Pain) Red Flags for 2ry (non migraine or tension) causes: HEADACHe - Hx of worst headache of my life, Pain on Exertion, Age >50, Despite treatment headache persist, Acute onset, CNS findings, HIV or immunosuppression, Fever. Migraine Dx Criteria: 2 or more of these: ● Unilateral pain, throbbing/pulsatile, aggravated by movement, moderate or severe intensity. Plus at least 1 of the following ● N/V, photophobia, phonophobia ● Avg= 4+ hrs Comorbidities ○ ○ *Cutaneous Allodynia is the perception of pain produced by the innocuous stimulation (Brushing hair, touching scalp, etc.) of normal skin and may result from sensitization of central pain pathways of migraine. Variant: “Familial Hemiplegic Migraine” ● Stroke like symptoms and paralysis on one ½ of body ● Lasts hours *Medication-Overuse Headache Evaluate for TIA Temporal Arteritis (Serum ESR & Biopsy) Meningitis (LP) Hemorrhages (CT) Neoplasms (CT) Overuse of analgesic may aggravate headache frequency, markedly reduce the effect of preventive medicines and induce a state of refractory daily or near-daily headaches. D/Dx: 1. 2. 3. 4. Fernando Vélez Taneil Gibson Trigeminal Autonomic Cephalgia (TAC) Idiopathic Intracerebral HTN a. Papilledema (inc CSF pressure) b. Tx: Spinal Tap Medication Overuse Headache a. Tx: preventative meds Temporal arteritis Insomnia, Depression Anxiety Migraine Disability Assessment Score (MIDAS) https://migraine.com/wpcontent/uploads/2012/04/midas.pdf Prophylaxis: Level A NSAIDS - Ibuprofen 5-HT agonist 1B / 1D Rizatriptan 10mg, Eletriptan 80mg, Almotriptan 12.5mg Add Naproxen in patients with auras since monotherapy with triptans are not effective Add Anti-emetics to control N/V. *Contraindicated in pt with Cardiovascular and cerebrovascular problems. Dopamine Antagonist (when above tx fail) Metoclopramide Patient education: Avoid triggers www.achenet.org Excess Caffeine/Alcohol - Maintain diary - Medication Side Effects Non-Medical Tx: ● Stress management ● Acupuncture, massages ● Aromatherapy, Herbs Tension - Bilateral tight, band-like discomfort. Pain builds slowly Fluctuates in severity Behavioral approach Medications 5. a. Biopsy: Giant cells b. Tx: Prednisone Sinus thrombosis a. Diagnosis: MRV - Cluster PE: - Palpate Temporal arteries Fundoscopy Diagnosis/ Labs: ● LP ● MRI, Angiography ○ Suspect aneurysm ○ Suspect AV malformation ○ Add Gadolinium to MRI- suspect BBB crossing Rare form of headaches (0.1%) Deep retro-orbital pain unilateral. - Core feature: Pain reoccurs at about the same time each day and same duration (short) Excruciating intensity Non-Fluctuating & explosive in quality. *Associated with ipsilateral symptoms of cranial parasympathetic autonomic activation: conjunctival injection or lacrimation, rhinorrhea or nasal congestion, or cranial sympathetic dysfunction such as ptosis. Chronic daily ● ● Fernando Vélez Taneil Gibson Not accompanied by N/V, Photosensitivity or Phonophobia Encompases a number of different headaches syndromes, both primary and secondary. Chronic: 15+ days /month for more than 1 month - Acetaminophen NSAIDS 100% Oxygen Inhalation 10-12L/min for 15-20 min Medication Sumatriptan 6mg nasal spray Neurostimulation therapy DBS of the posterior hypothalamic gray matter Meningitis Other Meningitis: 1. Lyme 2. Cryptococcal meningitis 3. Syphilis (3⁰) 4. TB Meningitis Bacterial Community acquired - Strep. Pneumo - Neisseria meningitidis - Listeria monocytogenes - 50-60 y.o immunocompromised Healthcare associated - Staph and Aerobic G(-) bacilli - Neurosurgery w/o prophylaxis - Internal or external ventricular drains - After trauma Viral (Aseptic) - Fernando Vélez Taneil Gibson MCC = Enterovirus Herpes Encephalitis HIV CMV Infections: Mycobacteria, Fungi, Spirochetes Para meningeal infections Bacterial ● Acute severe headache ● Fever ● Photophobia ● N/V ● Nuchal rigidity ● Altered mental status ● Accentuation of pain with eye movement Physical Examination Signs: Bacterial -CT before LP - Rules out Obstructive hydrocephalus -LP - Cell count- ↑ neutrophils - Protein ↑ Opening pressure (1315 Cm H2O) Xanthochromia (yellowing) Prednisone (IV)- Empiric - Minimizes chances of morbidities - Children and adults Ceftriaxone- Tx Meningitis Algorithm: -Blood cultures Viral (Aseptic) ● Fever (low grade) ● Headache ● Alt. mental status ● Stiff neck ● Photophobia ● Self limiting** Viral (Aseptic) - Meningeal inflammation but NEGATIVE bacterial culture - No CT or LP required Viral (Aseptic): Supportive or symptomatic therapy is usually sufficient, and hospitalization is not required unless elderly patient or immunocompromised. - Fungal - Encephalitis Medications Malignancies HIV disease Cryptococcal Meningitis (Indian ink) Encephalitis 1. Herpes simplex virus (HSV) a. b. HSV1 HSV2 2. Other herpes viruses a. b. EBV Varicella-Zoster 3. Enterovirus a. b. Poliovirus Coxsackievirus 4. Mosquito-borne virus a. b. c. d. West nile La Crosse St. Louis Western/ Eastern equine General SX: - Fever - Altered consciousness - Behavioral changes - Hallucinations; - Seizures - Local neurologic findings such as aphasia, hemiparesis, involuntary movements, and cranial nerve deficits. a. b. c. Seizures/ Epilepsy Epilepsy= 2+ unprovoked seizures; related 1. HSV a. Acyclovir 14-21d 2. EBV and VZV a. Acyclovir 14-21d since no current Tx is approved 3. LaCrosse and WNV a. IV Ribavirin mosquito exposure Tick-borne virus ● Sx ~1 week after bite *No therapy currently available for enteroviral, mumps, or measles encephalitis. Measles (Rubeola) Mumps Rubella Types of Seizure: Focal seizure (Contained within one hemisphere). 1. Retained awareness 2. Impaired awareness 3. **Temporal lobe is MC type Fernando Vélez Taneil Gibson - CSF PCR tests: - HSV - EBV - VZV - CMV - HHV-6 - Enterovirus CSF IgM-Ab - West Nile Virus days → weeks after Powassan virusMidwestern USA 6. Rabies virus 7. Childhood infections - Mosquito-borne virus ● Sx of infection appear 5. Tick-borne virus a. Viral Encephalitis: Acute Symptomatic Seizure - Occur at time of insult Within 24 hrs of Metabolic changes During drug/alcohol withdrawal Within 1 week of stroke, brain injury Epilepsy Diagnosis: ● 2+ unprovoked (reflex) seizures more than 24 hrs apart ● 1 unprovoked (reflex) seizure + probability of General Tonic-Clonic: ● Lorazepam/ Diazepam (IV) ● Phenytoin, Phenobarb (maintenance) Absence: ● Divalproex sodium (IV) disorders characterized by seizure tendency - Generalized seizures (Engage both cerebral hemispheres) 4. Typical Absence seizure (Loss of consciousness but no loss of postural control) a. Age 7 → puberty 5. Atypical Absence seizure Loss of both consciousness and postural control). During active phase of CNS infection (encephalitis) Unprovoked Seizure - Unknown etiology Preexisting brain lesion (“Remote symptomatic seizure”) PNS disorder Higher risk of future epilepsy (vs Acute symptomatic seizure) Fernando Vélez Taneil Gibson ● ● ● Generalized Tonic Clonic 6. Tonic contractions of the muscle followed by clonic phase (superimposed periods of muscle relaxation). Causes of Seizures: ● Hypo/Hyperglycemia ● Hyponatremia ● Hypocalcemia ● Hypomagnesemia ● Disorders of porphyrin metabolism ● Withdrawal states ● Uremia ● Drug intoxication ● Hyperthyroidism more seizures ● - “3 spike and wave” MRI- no contrast EEG ○ Generalized Epilepsy ○ Absence ○ Rolandic/ Localizationrelated Epilepsy Monitoring unit○ 3-7 d sleep study Metabolic work up (if indicated) ● Ethosuximide Myoclonic: ● Divalproex sodium (IV) Partial Seizures: ● Phenytoin (“Dilantin”) ● Carbamazepine (XR) ● Divalproex sodium (IV) Others: ● ● ● ● Clonazepam Gabapentin Lamotrigine Felbatol **Patient Education: Seizure precaution, Driving ADR Divalproex: hepatotoxicity, spina bifida, N/V, weight gain, hair loss, teratogenic Carbamazepine: Diplopia, Hyponatremia, Teratogenic Phenobarb: brain function affected Lamotrigine: Steven Johnson syndrome, rash - MC Due to brain scar tissue “Focal epilepsy” Cerebrovascular disease Ischemia Types: 1. Thrombosis 2. Embolism 3. Systemic hypoperfusion ● ● ● ● CT or MRI of brain Cardiac monitoring ○ After ischemic stroke onset Monitor volume and electrolytes Serum glucose: correct if low (<60 mg/dL) - Stabilize airway, breathing and circulation Prevent aspiration Optimize bed head position (30 degrees): - Acute Stroke Sudden onset of neurologic deficit of cerebrovascular origin in patients with Hx of - HTN - DM - Tobacco use - A-Fib - Atherosclerosis Moyamoya Disease Fernando Vélez Taneil Gibson Acute Stroke - Neurological signs reflects the region of the brain involved - Sensory, motor, speech deficits Moyamoya Disease Acute Stroke - Blood work is required to determine the source of the stroke. (CBC, Serum Glucose, Lipid panel, Blood culture (if endocarditis is suspected)). - CT w/o contrast before aspirin or antithrombotic administration. - CT Angiography Intracerebral hemorrhage ↑ ICP Aspiration Cardiopulmonary decompensation O2 desaturation Acute Stroke ● Antithrombotic: Aspirin or Plavix ○ At First 48hrs ○ At Discharge ● Prophylaxis DVT and PE ● High intensity Statin (lipid lowering) ○ ADR: myalgia ● BP reduction ● Behavioral and lifestyle changes Moyamoya Disease Idiopathic vasculopathy that leads to progressive occlusion of blood vessels and proliferation of capillaries at the base of the brain in response to ischemia. - Blocked arteries at basal ganglia - ICA intima thickens - ACA, MCA, PCA = stenosis or occlusion Intracerebral Hemorrhages 1. Intraparenchymal a. Systemic HTN b. Contusion c. Amyloid angiopathy d. Vasculitis e. Neoplasm 2. Subdural a. Ruptured bridging veins b. Shaken baby 3. Epidural a. Middle Meningeal artery rupture 4. Subarachnoid a. Acceleration/ deceleration injuries b. Circle of Willis Aneurysm rupture c. AV malformation Fernando Vélez Taneil Gibson ● Prone to strokes and brain hemorrhages Moyamoya Disease - Angiography Surgery (↑ blood flow): - EDAS (encephalo-duro- Intracerebral Hemorrhages - Loss of consciousness in 50% of pts. - N/V and headaches - Focal Sx depending on the site of the bleed. Subdural: - Altered mental status, slow thinking - Seizure - Vague personality change - Complication= Secondary hydrocephalus Epidural: - Lucid interval: patient can die suddenly Subarachnoid: - Xanthochromia - “Worst headache of my life” - Complication= Secondary stroke (from bv vasoconstriction) - MCC: Rupture of Berry Intracerebral Hemorrhages CT imaging: - Intraparenchymal - Subdural - Epidural - Subarachnoid arterio- synangiosis) EC-IC (intracranial to extracranial) EMS (Encephalo-myosynangiosis) Intracerebral Hemorrhages - Surgery for decompression to prevent brain herniation. - Conservative Neurologic management Aneurysm Neuromuscular disease Myasthenia Gravis - -Autoimmune disorder: Anti-ACh Receptor Ab in the postsynaptic membrane of NMJ -Monitor pt’s for: - Hx of Myasthenic crisis - MG therapy - Thyroiditis, RA, SLE *Assoc with Thymoma - Bulbar Sx: - Dysphagia - Dysarthria - Nasal speech - Low-intensity speech Ptosis Diplopia Progressive weakness throughout the day Dyspnea SOB *Nerve Conduction Study = diagnosis Edrophonium (Tensilon) test= only if a Peripheral neuron deficit CT neck - look for Thymoma (source of Antibodies) AchE inhibitor (initial therapy)” ● Pyridostigmine ● Neostigmine High-dose Glucocorticoids - If contraindicated or ineffective, use Azathioprine, Mycophenolate mofetil, Cyclosporine Surgical removal of Thymoma, if present Crisis: ● Intubation and Mechanical ventilation ○ If Resp failure ○ Temporarily stop Anti-AchE meds ● Plasma exchange ● IVIG (intravenous immunoglobulin) Peripheral Neuropathies Damage to, or disease affecting small nerves → impaired: - Sensation - Movement - Gland/ organ function Fernando Vélez Taneil Gibson Labs: -Clinical test -Monofilament testing- (Diabetic neuropathy) -Reflexes -EMG/ NCV ● NCV- Measures how fast/ well nerve functions ● EMG- needles placed on muscle to determine it’s behavior with contraction Types: 1. Polyneuropathy a. DM b. Guillain-Barre 2. Peripheral neuropathy a. Radiculopathies 3. Neuropathy a. CNS, PNS 4. Mononeuropathy a. Carpal tunnel Syndrome 5. Mononeruopathy multiplex a. Leprosy b. Diabetes Causes: ● Diabetic ○ ● ● ● ● ● ● ● ● ● ● Inflammatory, metabolic and ischemic events Longstanding HIV Critical illness Amyloidosis Vitamin deficiencies Lyme disease Autoimmune Toxic ○ Alcoholic Hereditary Environmental idiopathic Guillain Barre Syndrome (AIDP) AIDP ● Autoimmune condition assoc. with infections: - Campylobacter jejunum - Zika virus -Schwann cell damage Fernando Vélez Taneil Gibson ● ● ● ● Back and Extremity pain ○ GBS pt ○ Presenting Sx Symmetric Weakness starts in legs and ascends ↓ Reflexes- 90% Dysautonomia - 70% Severe resp muscle Lab DX: - LP: - normal cell count - ↑ Protein Dx: - Electrophysiologic studies may reveal Disease-modifying Tx: ● IV IG ● Plasmapheresis ● Supportive therapy, ICU *Majority recover completely “Acute inflammatory demyelinating polyneuropathy” = AIDP ● ● ● ● ● weakness Facial nerve palsy- 50% Oropharyngeal weakness 50% Oculomotor weakness -15% Paresthesia SIADH ○ GBS complication - -Sensory abnormality = rare Muscular dystrophy Group of diseases that cause progressive weakness and loss of muscle mass Duchenne Muscular dystrophy - < 5 yo boys (X-link rec.) - Frameshift mutation Duchenne Muscular dystrophy - - abnormalities, which do not necessarily parallel the clinical disorder in their temporal course. Pathologic examination reveal demyelination, or less commonly, axonal degeneration. Duchenne Muscular dystrophy Weak pelvic girdle ● ↑ Aldolase muscles → progresses ● ● ↑ CK Genetic testing ● PE: superiorly Pseudohypertrophy of calf muscles Dilated cardiomyopathy - MCC death after weeks→ months ○ ○ Gower’s Sign Waddling gait -Variants: 1. Becker dystrophy 2. Myotonic dystrophy Prednisone (.75mg/kg OP/day) - Improves muscle strength and function. - Monitor ADE. Avoid prolonged bed rest or inactivity Physical therapy. Multiple Sclerosis - Fernando Vélez Taneil Gibson Demyelinating UMN disease ● ● Diplopia Ataxia MRI - GOLD standard Acute Tx: - IV Methylprednisolone - - Environmental factors - EBV Neuromyelitis optica ( Devic’s disease is a disorder related to MS. ● ● ● ● ● ● MC affects Caucasian Women, 20-30 y/o ● Scanning speech Intention tremor INO/ nystagmus Neurogenic bladder Paraparesis Hoffman & Babinski Signs Marcus Gunn Pupil - Periventricular plaques Dawson fingers - (“Solumedrol”) ACTH (if solumedrol fails) Other Tx: ● Alemtuzumab ● Daclizumab ● Dimethyl Fumarate ● Fingolimod ● INF-b Dx. Criteria: Primary progressive disease requires at least 1 year of progressive disease, plus 2 or 3 of the following. - At least 1 typical brain lesion. - At least 2 spinal lesions - IgG Oligoclonal banding in the CSF. PE: - Lhermitte Phenomenon - Uhthoff phenomenon Movement disorders Parkinson's Disease - Decreased Dopamine production in the substantia nigra. Sx: - *Extrapyramidal- so no babinski - Fernando Vélez Taneil Gibson Resting muscle tremors Cogwheel Rigidity Bradykinesia Shuffling gait (Paralysis agitans) Loss of balance Tremor is 3 cycles per second and extinguishes with movement. Dopamine Agonist - Bromocriptine - Cabergoline - Pergolide - Pramipexole - Ropinirole Dopamine precursors - L-Dopa / Carbidopa** - Long acting LD/CD - L-Dopa Deep Brain Stimulationadvanced cases Essential Tremors - Movement disorder usually on one side of the body. Cognitive impairment Sx: Timing tremors - Intentional tremor of the hand. - Hands, head and voice tremors - Tremor is > 4 cycles per second, intentional w/o Cogwheel rigidity. ● ● ● Mysoline (high dose250mg 4/day) Alcohol Propranolol Deep Brain Stimulation Memory Loss Testing MMSE test - Includes simple questionnaire and problems in a number of areas. - Time and Place Language Comprehension Basic motor skills Score > 24 is Nml (out of 30) 19 - 23 Mild 10 - 18 Moderate < 9 Severe *Score < 24= think dementia Frontotemporal Dementia - “Pick’s disease” - Primary progressive aphasia - Semantic dementia - Pick complex - Corticobasal degeneration + Progressive Supranuclear Palsy. Behavioral Variant FTD - Changes in social behavior and conduct. - Loss of social awareness. - Poor impulse control. Semantic Dementia - Loss of semantic understanding - Impaired word comprehension - Speech remains fluent Progressive Non-fluent aphasia Fernando Vélez Taneil Gibson Alzheimer Disease - Irreversible progressive brain disorder - Temporal AND Parietal lobes - Progressive difficulty in speech production - Memory and thinking skill loss. Inability to carry out simple tasks Lost in familiar places Inability to differentiate Right vs. Left Sx: - Spinal Cord Disorders Neurofibrillary tangles Plaques NMDA Antagonist - Memantine Normal pressure hydrocephalus - Enlargement of the ventricular size with normal opening pressure on LP. - TRIAD: 1. Dementia 2. Gait disturbances (Magnetic Gait) 3. Urinary Incontinence CT scan Transverse Myelitis - Segmental Spinal Cord injury caused by acute inflammation. - Most cases are idiopathic. Sx: Transverse!! - Corticospinal - Spinothalamic - Dorsal column LP- ↑ WBC Associated with: - MS & SLE - Mixed connective tissue disease - Sjogrens Synd. - Antiphospholipid Ab Synd - Ankylosing spondylitis - RA Subacute Combined Degeneration - Vit. B-12 deficiency or Chronic NO exposure Fernando Vélez Taneil Gibson Cholinesterase Inhibitors - Donepezil - Rivastigmine - Galantamine Ventriculoperitoneal shunt MRI- shows inflamed spinal cord segment Spinal Cord tracts Sx: - Slowly progressive weakness (Truncal and Labs - Increase homocysteine Supplemental treatment with Vit. B12. - (Interfere with methionine synthetase) Lead to dorsolateral white matter degeneration in the spinal cord. Assoc. With Pernicious Anemia Lyme Myelopathy -rare Fernando Vélez Taneil Gibson - peripheral) Peripheral neuropathy Sensory ataxia (Vibration and proprioception) Paresthesia Spasticity Paraplegia Incontinence Decreased Visual acuity MRI - Increase Methylmalonic acid T2 weighted signal of posterior column. Hematology Anemias Acute -Usually due to blood loss Acute - Chronic Chronic - Fatigue - Exertional dyspnea - Exertional palpitation - Angina or CHF - Pallor - Splenomegaly , jaundice (= hemolysis) Chronic ● Fecal occult blood test Microcytic anemia (MCV <80) Iron deficiency - Restless legs - Hair loss - Pallor, cheilitis, atrophic glossitis - Koilonychia Iron deficiency ● Serum iron ↓ Iron deficiency Causes: - Babies-RBC’s made faster than iron intake - Menstrual blood loss - Chronic GI blood loss - Diet, Malabsorption Lead poisoning Fernando Vélez Taneil Gibson Acute SOB Palpitation Exercise intolerance Faintness Hypotension, tachycardia, pallor ● TIBC ↑ ● ● Serum ferritin ↓ Fecal occult blood test ○ Adult male ○ Postmenopause GI endoscopy ● Lead poisoning - Mental retardation Iron deficiency - Oral ferrous sulfate/ gluconate - IV iron Dextran/ sucrose - Treat underlying cause Lead poisoning - EDTA - Succimer - Colicky abdominal pain Wrist drop Skin lesions Gingival lead line Lead poisoning ● X ray- radiodense tibia ● Histo: nucleated RBC with basophilic stippling ● Ringed sideroblasts - Dimercaprol Thalassemia Thalassemia Thalassemia 𝛼 thalassemias- defect in 𝛼 chain production Beta- spelnomegaly, repeated infection Thalassemia 𝛽 thalassemias- defect in 𝛽 chain production Macrocytic anemia (MCV >100) B12 deficiency - Autoimmune (Antiparietal cell Ab) - Gastrectomy Fernando Vélez Taneil Gibson B12 deficiency - Impaired cognition - Disequilibrium - Impaired position and vibration sense - Gait disturbance 𝛽 Thal minor- Hb electrophoresis 𝛽 Thalassemia trait- target cells *Bone marrow aspiration B12 deficiency Diet (meat, fish, dairy, eggs) - Oral B12- indefinitely - Cobalamin 1000 µcg monthly (parenteral)- B12 deficiency ● Pancytopenia ● Rhomberg ● B12 serum levels ● Anti-parietal cell Ab ○ R/o autoimmune indefinitely - Folate deficiency Oral folic acid ● ● ● Folate deficiency - Poor diet (tea and cookies diet) - Alcoholic - Intestinal malabsorption Myelodysplastic syndrome - Elderly - Impaired rbc maturation Drug- induced - Antifolates - Chemotherapy - Anticonvulsants Normocytic anemia (MCV 80-100 fL) *Blood loss w/o iron deficiency (a) Nonhemolytic (b) Hemolytic (a)Non hemolytic: *(reticulocyte count ≤2%) - Anemia of Chronic Disease -Iron deficiency Fernando Vélez Taneil Gibson pernicious anemia Homocysteine ↑ MMA ↑ Upper endoscopy surveillance (risk stomach AdenoCa.) Folate deficiency ● Pancytopenia ● Folate serum levels ● Anti-parietal cell Ab ○ R/o autoimmune pernicious anemia ● Homocysteine ↑ ● Normal MMA Myelodysplastic syndrome ● Pancytopenia -Creatinine and eGFR -Reticulocyte count -Haptoglobin -Bone marrow aspiration -Aplastic anemia -Chronic Kidney disease (b) Hemolytic anemia *(Reticulocyte count >2%) Hereditary Spherocytosis Gallstones (bilirubin) ● ● ● -Hereditary Spherocytosis -Autoimmune hemolytic anemia -G6PD deficiency -Toxins and drugs -Mechanical RBC damage - Heart valve defect - DIC, HUS, TTP Bleeding Disorders Labs: ● ● CBC PT ● PTT ○ Drug/ toxin Hx Recent viral infxn Autoimmune dx? HIV or HCV? ● Thrombocytopenia -Clopidogrel -SSRI Splenectomy Vaccinate against Strep pneumo, HiB, Neisseria meningitidis Hx: PE: ● Labs: ● ● ● ○ (a) Acute ITP -Post viral infection ; Ab’s cross react with platelets Acute ITP ● Sudden onset purpura and petechiae ● (b) Chronic ITP Fernando Vélez Taneil Gibson ● ● ● ● ● Test if on warfarin or have liver dx If pt on Unfractionated heparin ● Factors 2, 7, 9, 10 ○ Vit K Special Tests: ● Thrombin time ● Factor assay ● Ristocetin cofactor assay ● PFA-100 ● Reticulocyte count LDH Haptoglobin (intravascular hemolysis) Coomb’s test (Ab to RBC) Osmotic fragility ○ Hereditary spherocytosis Ultrasound Lymph, liver spleen, skin WBC, RBC ANA Bone marrow Acute ITP - Normal WBC and RBC (vs Acute leukemia) Acute ITP Chronic ITP Chronic ITP Corticosteroids Self limited DDx= Acute Leukemia Chronic ITP -Complicates Hep C and HIV -Drug induced -SLE or autoimmune association DIC ● ● ● - Low platelet count ● ● ● ● ● ● High PT and PTT Low fibrinogen High D-Dimer and FDP Low platelet Schistocytes Microangiopathic hemolytic anemia Any bleeding or bruising sx Menorrhagia Neonates: - Umbilicus bleed - Postcircumcision bleed Post-Aspirin or NSAID use ● ● ● ● ● ● Platelet count normal BT- prolonged PT - normal PTT- prolonged Ristocetin cofactor assay VWF Ag and Activity Type 1: - Desmopressin Hemorrhage out of proportion to trauma Hemarthrosis of weight-bearing joints ● ● ● ● Hb normal or ↓ PTT prolonged Factor VIII and IX assay VWF Ag and activity Desmopressin + Factor (which is deficient) Triggers: -ObGyn catastrophe -Trauma, burns -Sepsis -Hemolytic transfusion rxn -Acute promyelocytic leukemia -Mucin secreting adenoCa. Von Willebrand Disease - Type 1- 66-75% ● ↓# ● Normal function - Type 2- 20-25% ● Normal # ● ↓ Function Asymptomatic Purpura petechiae - Corticosteroids IVIG Rituximab Splenectomy Type 2 and 3: - Recombinant VWF Type 3● Absent VWF Hemophilia - Hemophilia A- Factor VIII deficiency - Hemophilia B- Factor IX deficiency Fernando Vélez Taneil Gibson X linked Venous Thrombosis Inherited -Congenital deficiency or dysfunction of natural anticoagulant Acquired Myeloproliferative Disorders Chronic Myelogenous Leukemia (CML) Inherited Acquired - Arterial and venous thrombosis - PE - Pregnancy loss - +/- SLE or autoimmune dx - Splenomegaly Wells Criteria Inherited ● Abnormal Factor V leiden ● Protein C or S deficiency ● Prothrombin gene mut. ● Antithrombin III deficiency Acquired ● Lupus anticoagulant (anticardiolipin Ab) ● Antiphospholipid Ab ● t(9;22) Polycythemia Vera -Red cells proliferate autonomously -High RBC, WBC, platelets - Dizzy Headache Angina Claudication Cyanosis Splenomegaly Pruritus Warfarin - lifelong ● ● ● ● CBC ○ - Imatinib (Tyrosine Kinase inhibitor) - Regular phlebotomy Low dose aspirin Hydroxyurea, Busulfan (myelosuppressi ve therapy) Ruxolitinib (JAK2 inhibitor) Anemia ○ Thrombocytopenia ○ leukocytosis EPO low High red cell mass JAK2 gene mutation CBC ○ Leukocytosis ○ thrombocytosis - Essential thrombocythemia Clonal proliferation of megakaryocytes (RBC, WBC, Platelets) Fernando Vélez Taneil Gibson - RBC inc or dec. ⇒ headache, dizzy ● ● ● JAK2 gene mut Megakaryocytes Thrombocytosis Myelofibroblasts w/ Myeloid Metaplasia Clonal proliferation of marrow stem cells -Fibrosis of bone marrow Fernando Vélez Taneil Gibson - Splenomegaly ● ● Fibroblasts Anemia, thrombocytopenia, leukocytosis - Ruxolitinib (JAK inhibitor) Oncology Presentation Cancer Staging Signs “B Symptoms”: -Fever -Night Sweats -Weight loss -Pruritus Evaluation ● T- size of primary Tumor (T1, 2, 3) N- presence (1) or absence (0) of lymph Node involvement M- presence (1) or absence (0) of distant Metastasis ● ● ● ● ● Hodgkin’s Disease (Lymphoma) Painless lymphadenopathy Ages 15-35 and 55+ y/o - B symptoms Atypical chest pain Cough SOB - if mediastinal mass Bone pain, painful nodes (less common) (a) Nodular Sclerosis Age 15-30 y/o - MC type F>M Painless lymphadenopathy Fernando Vélez Taneil Gibson -Palpable LN - Neck>Axilla>Inguinal -Check Epitrochlear nodes -Check tonsils and oropharynx -Hepato / Splenomegaly TNM System: ● ● ● ● Biopsy Radionuclide bone scanning CXR, Chest CT, PET Brain MRI CT -Abdomen or pelvis LN biopsy: ReedSternberg cell CBC, CMP, ESR Staging: CT, MRI, PET Ann Arbor Staging System Treatment Complete excision (+/regional LN excision) Debulking surgery or resection Radiation therapy Cytotoxic chemotherapy Hormonal therapy Growth factor inhibitors, Anticell surface marker Ab’s Palliative Care - Radiation and Combination Chemo - Death usually from secondary malignancy -No physical findings if disease is in a nonpalpable node ● ● ● Prominent fibro-sclerotic bands of tissue Reed Sternberg cells Lacunar Chemotherapy Radiotherapy *GOOD prognosis (b) Mixed Cellularity Age 40-50 y/o - MC Male ● Mixed cellular background w/o bands of sclerosis Reed- sternberg cells Prognosis worse than Nodular sclerosis (c) Lymphocyte Predominant type ● Prognosis good ● Nodal effacement with small lymphocytes Reed Sternberg cells ● ● Retroperitoneal LN Reed Sternberg cells Poor prognosis ● ● Lymph node biopsy Immunophenotyping by flow cytometry Staging (Ann Arbor) with CT, MRI, PET Bone Marrow biopsy CBC, CMP, HIV Combination chemotherapy +/- radiation ● Uncommon Male> Female Age ~35 y/o x (d) Lymphocyte depletion Uncommon Most aggressive type Mid→ Older age group Non-Hodgkin Lymphoma Any age, avg 50 y/o Involves LN, spleen and marrow HIV is a risk factor - Fernando Vélez Taneil Gibson Palpable node or B -Abdominal or Testicular mass -Gastric lymphoma -Pallor, Bruising, Petechiae If thrombocytopenia -Palpable LN - Neck>Axilla>Inguinal -Check Epitrochlear nodes ● ● ● -Regimen based on type of lymphoma, prognosis etc -Rituximab - symptoms Mass in GIT or testicle Bone marrow involved: weak, bruising Recurrent infections Acute Leukemias -Check tonsils and oropharynx -Hepato / Splenomegaly -No physical findings if disease is in a nonpalpable node -Bone marrow failure: - Bruising, pallor, bleed, fever, sepsis, lethargy ● ● ● Acute Lymphoblastic Leukemia ALL -MC Children and curable -Lethal in adults ALL Acute Myelogenous Leukemia AML -Any age -(~) curable in children -Highly lethal in adults AML Chronic Lymphocytic Leukemia -Clonal proliferation of mature-appearing but functionally impaired B cells -Anemia -Thrombocytopenia -Neutropenia -Infections (from Ig deficiency) -Mid→ Elderly - Fernando Vélez Taneil Gibson Asymptomatic Blood count= mature CBC ○ Anemia, thrombocytopenia ○ Leukocytosis with blasts Bone marrow aspiration ○ Stain, surface markers, cytogenetics Flow cytometry ALL - - Frequent CNS involvement IV-IG = prophylaxis ● ● ● NO Auer rods Myeloperoxidase stain (-) TdT (+) AML ● ● ● Some Auer rods Myeloperoxidase stain (+) TdT (-) ALL -2-3 yrs chemotherapy: - Induction - Consolidation - CNS-directed - Maintenance -High cure rate if pt lacks high-risk markers AML -2-3 years chemotherapy: - Induction - Consolidation - Maintenance - Most require no Tx - 10-20 year survival - Oral alkylating agents-if dx is progressive Plasma Cell MGUS Multiple Myeloma lymphocytes LN and Spleen involved MGUS -Elderly -Asymptomatic -Minority progress to myeloma Multiple Myeloma ->10% plasma cells in marrow - Invasive Breast Cancer Risk factors: -Age 50-70 y/o -Delayed childbearing, early menarche, late menopause -Exogenous estrogen -Obesity -Radiation to chest (mammography) -Family Hx Multiple Myeloma -Anemia -Thrombocytopenia -Leukopenia -Infections -Bone invasion= - Pain - Pathologic fracture - Hypercalcemia - Mental status - Nausea - Dehydration - polyuria -Renal failure - Asymptomatic on mammography Lump in breast Skin retraction, dimpling, “peau d’orange” Axillary adenopathy Nipple discharge Possible Mets → bone, - Rituximab↑response and survival - Surgery Tamoxifen, Anastrozole = if Multiple Myeloma ● ● ● ● Serum/ urine protein Electrophoresis○ M spike ○ IgG or IgA CBC BMP- hyperCa, renal fxn Bone marrow aspiration and biopsy ↷ ● ● ● ● Diagnostic mammography Biopsy CXR, US, MRI Staging ● ● CXR Chest CT estrogen or progesteroneR’s seen on biopsy - Trastuzumab= if HER2-R seen on biopsy Screening: ● Mammography 40-49 y/o ● Mamm /2years= 50-74 y/o ● liver, lung, pleura, brain Lung Cancer Fernando Vélez Taneil Gibson Risk factors: ● Smoking Symptoms ←regional spread NSCLC: ● ● ● ● Occupational exposure Environmental carcinogens Radiation HIV Paraneoplastic Syndrome in NSCLC: - Hypercalcemia -from PTH-like substance in SCC pt. - → polyuria and obtundation, nausea, confusion, dehydration -Motor and Sensory neuropathy -from SCC and AdenoCa. Paraneoplastic Syndromes in SCLC: - SIADH - Ectopic ACTH secretion - Eaton Lambert Syndrome - Acute sensory neuropathy - Cerebellar degeneration Prostate Cancer Fernando Vélez Taneil Gibson -Predilection for bone metastasis ->50 y/o male -African American or distant metastasis -Paraneoplastic syndrome -Supraclavicular or cervical lymphadenopathy -Dull percussion, ↓ breath sounds= pleural effusion Primary tumor: - Cough, hemoptysis, SOB - (recurring) Pneumonia - Atelectasis ● ● ● ● ● ● Sputum cytology ○ If (+), no invasive biopsy required Bronchoscopy and biopsy ○ Central lesion CT transthoracic biopsy ○ Peripheral lesion Pleural fluid cytology ○ Metastatic lesion Mediastinoscopy and biopsy ○ Used to stage Thoracotomy Regional spread: - Chest wall pain - Arm pain or Horner’s Syndrome - Hoarseness - SVC syndrome - SOB Early= asymptomatic Frequency, urgency, small void, poor stream, dribbling, retention, UTI - Surgery -lobectomy or pneumonectomy Radiotherapy (palliative only) Chemotherapy (extend life by few months) Biologic agents targeting oncogene products SCLC: - Same as NSCLC - Relapses occur Screening: ● Chest CT (non contrast) ○ Annually in eversmoker 50-80 y/o ○ >30 pack year ○ Currently or quit smoking <15 years ago Metastasis: - Bone pain, pathologic fracture - Seizure, impaired cognitive, disequilibrium - Paraplegia, bowel/bladder dysfxn - - ● Prostate exam ○ Nodule or induration ○ Screening starts 50-75 y.o - Watchful waiting Radical prostatectomy Radiation with curative intent *Gleason Grade & Score Grade: 1-5 (3-5= likely mets) Score: 6-10 (higher=worse prognosis) - Metastasis= Anemia or pancytopenia, bone pain ● ● ● ● Colorectal Cancer -Family Hx: - FAP- APC gene - Lynch Syndromemismatch repair gene -Age: 68 y.o, younger ages -Risk Factors: - Red meat - Animal fat intake - Low fiber - IBD Early: ● ● Late: ● ● ● ● ● ● Rectal bleed Pallor - PSA Transrectal Ultrasound Transrectal needle biopsy ○ If Palpable or visible nodule Blind needle biopsies ○ If PSA high but no discrete nodule Colonoscopy Biopsy CT (Staging) CBC, CMP, CEA Weight loss Abdominal mass and tenderness Constipation Cachexia Ascites hepatomegaly 3) Endometrial Cancer Fernando Vélez Taneil Gibson ● ● ● ● Surgery Radiation Adjuvant chemo for stage 3 Biologics Screening: -Screen 50-75 y/o - Choice at 76-85 y/o -Annual FIT -Colonoscopy- most effective -Annual FIT + Sigmoidoscopy -Lesions: 1) 2) If Advanced: - Palliative radiation - bone pain - Surgical castration - “Medical castration” - Flutamide - Leupromide - Cytotoxic chemoDocetaxel Hyperplastic polyp Villous adenoma Sessile polyp -Middle age→ older women -Precursor= Endometrial hyperplasia Risk factors: - Obesity - Unopposed estrogen - Tamoxifen OCP= protective Painless vaginal bleed ● ● ● ● Pelvic exam Biopsy (in office) Cytologic smear of cervix Transvaginal sonography (thickness Hysterectomy Ovarian Cancer - Abdominal discomfort Bowel disturbances Ascites NO PELVIC MASS ● Tumor marker CA-125, CA-19.9 Pelvic ultrasound CT of pelvis and abdomen Cytologic analysis of ascitic fluid Mass biopsy Remission: Surgery, then Chemotherapy ● CT scan, endoscopic Ultrasound, MFRI, ERCP -Pancreaticoduodenectomy (Whipple Procedure) -Chemotherapy -Palliative care ● Ultrasound ○ Cystic vs solid ○ Benign vs malig Fine needle aspiration & cytologic examination *Most curable ● ● ● ● Pancreatic Cancer #4 cause of cancer mortality in USA 75% at head of pancreas *non specific: - Weight loss - Epigastric pain radiates to back - Depression - New onset diabetes - Pruritus - Painless jaundice (if cancer in head of pancreas) Thyroid Cancer Most <55 y/o - Painless lump in thyroid - Cervical lymphadenopathy ● Uroepithelial Cancer (Bladder and Ureter) Renal Cell Cancer Risk factors: - Smoking - Environmental carcinogens - Painless hematuria Irritative void - Painless hematuria Flank pain/ mass - Surgery Radioactive iodine Bladder Cancer: Transurethral removal -Lifelong cystoscopic surveillance CT scan *Poor prognosis Chemotherapy= poor response Growth factor inhibitors= Clear cell type of RCC Fernando Vélez Taneil Gibson