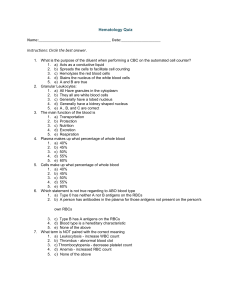
Blood The cardiovascular system consists of three interrelated components: blood, the heart, and blood vessels. Most cells of a multicellular organism cannot move around to obtain oxygen and nutrients and get rid of carbon dioxide and other wastes. Instead, these needs are met by two fluids: blood and interstitial fluid. Blood is a liquid connective tissue that consists of cells surrounded by an extracellular matrix. The extracellular matrix is a liquid portion called plasma and the cellular portion consists of various cells and cell fragments. Interstitial fluid is the watery fluid that bathes body cells and is constantly renewed by the blood. Oxygen brought into the lungs and water and nutrients brought into the gastrointestinal tract are transported by the blood, diffuse from the blood into the interstitial fluid, and then diffuse into body cells. Carbon dioxide and other wastes move in the reverse direction, from the body cells into the interstitial fluid and then into the blood. Blood then transports the wastes to various organs—the lungs, kidneys, skin, and digestive system—for elimination from the body. Blood transports various substances, helps regulate several life processes, and affords protection against disease although, Blood is closely related to other body fluids. In fact, many of the extracellular body fluids (including interstitial fluid, lymph, cerebrospinal fluid, and aqueous humor) arise from the blood during development and are continually replenished by it. The extracellular fluids that nourish, protect, and exchange materials with every cell of the body are derived from the blood, renewed by the blood, and returned to the blood. Based on these relationships, blood has three general functions: 1. Transportation. Blood transports oxygen from the lungs to the cells of the body and carries carbon dioxide from the body cells to the lungs for exhalation. It carries nutrients from the gastrointestinal tract to body cells and hormones from endocrine glands to cells throughout the body. Blood also transports heat and waste products to the lungs, kidneys, and skin for elimination from the body. 2. Regulation. Circulating blood helps maintain homeostasis in all body fluids. Blood plays a role in the regulation of pH through buffers. It also assists in the adjustment of body temperature; the heat-absorbing and coolant properties of the water in blood plasma and its variable rate of flow through the skin allow excess heat to be lost from the blood to the environment. 3. Protection. Blood can clot (become gel-like), which protects against its excessive loss from the cardiovascular system after an injury. In addition, white blood cells protect against disease by carrying on phagocytosis. Several types of blood proteins, including antibodies, interferons, and complement, help protect against disease in a variety of ways PHYSICAL CHARACTERISTICS OF BLOOD Blood is denser and more viscous (thicker) than water, which is part of the reason it flows more slowly than water. The temperature of blood is about 38°C (100.4°F), which is slightly higher than normal body temperature, and it has a slightly alkaline pH ranging from 7.35 to 7.45. The color of blood varies. When saturated with oxygen it is bright red; when unsaturated with oxygen, the blood is dark red to purple. Blood constitutes about 8 percent of the total body weight. The blood volume is 5–6 liters in an average-sized adult male and 4–5 liters in an average-sized adult female. This gender difference in volume is due to the difference in average body size. Blood Group Systems More than 100 types of genetically determined antigens have been detected on the surface of red blood cells. Many of these antigens appear in characteristic patterns, a fact that enables scientists or health-care professionals to identify a person’s blood as belonging to one or more blood groupings; there are at least 14 currently recognized blood group systems. Each system is characterized by the presence or absence of specific antigens on the surface of a red blood cell’s plasma membrane. The two most commonly used categories are the ABO and Rh blood grouping systems. The ABO blood grouping system is based on two antigens, symbolized as A and B. Individuals whose erythrocytes manufacture only antigen A are said to have blood type A. Those who manufacture only antigen B are type B. Individuals who manufacture both A and B are type AB. Those who manufacture neither are type O. Blood plasma usually contains antibodies that react with the A or B antigens if the two are mixed. These are the anti-A antibody, which reacts with antigen A, and the antiB antibody, which reacts with antigen B. You do not have antibodies that react with the antigens of your own RBCs, but you do have antibodies for any antigens that your RBCs lack. For example, if your blood type is B, you have B antigens on your red blood cells, and you have anti-A antibodies in your blood plasma. The Rh blood grouping system is so named because the Rh antigen, called Rh factor, was first found in the blood of the Rhesus monkey. Individuals whose erythrocytes have the Rh antigens (D antigens) are designated Rh+. Those who lack Rh antigens are designated Rh -. As just noted, the presence or absence of certain antigens on red blood cells is the basis for classifying blood into several different groups. Such information is very important when a transfusion is given. A transfusion is the transfer of whole blood or blood components (red blood cells or blood plasma, for example) into the bloodstream. A transfusion may be given to treat low blood volume, anemia, or a low platelet count. However, in an incompatible blood transfusion, antibodies in the recipient’s plasma bind to the antigens on the donated RBCs, which causes agglutination of the RBCs. Agglutination is an antigen–antibody response in which RBCs become cross-linked to one another. When these antigen–antibody complexes form, they activate complement proteins (globulins), which make the plasma membrane of the donated RBCs leaky, causing hemolysis (rupture) of the RBCs and the release of hemoglobin into the blood plasma. The liberated hemoglobin may cause kidney damage. Although quite rare, it is possible for the viruses that cause AIDS and hepatitis B and C to be transmitted through transfusion of contaminated blood products.