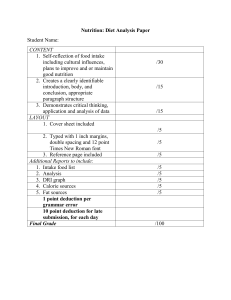
CASE STUDY 18 STROKE Group Members: Lystra Paul, Charis Adams, Asia Edwards OVERVIEW OF CASE STUDY Mrs. Ruth Noland, a 77 year old woman, is transported to the emergency room of University Hospital with the symptoms of slurred speech, numbness on the left side of her face, and weakness of her left arm. UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY 1. Define Stroke. Describe the differences between ischemic and hemorrhagic stroke. A stroke occurs when the blood supply to part of your brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. Due to this brain cells die within minutes. Ischemic Stroke An ischemic stroke is caused by a blood clot that blocks or plugs a blood vessel in the brain. This prevents blood flow to the brain and brain cells begin to die.it can also be caused by stenosis, or narrowing of the artery. This occurs because of atherosclerosis, a disease that causes plaque formation in the arteries. Hemorrhagic Stroke A hemorrhagic stroke is caused by a weakened blood vessel that ruptures and bleeds into the surrounding brain. The blood accumulates and compresses the surrounding brain tissue. There are two types of hemorrhagic strokes are namely intracerebral (within the brain) hemorrhage or subarachnoid hemorrhage. UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY CONT’D 2. What does Mrs. Noland’s score for the NIH Stroke Scale Indicate? Mrs. Noland’s score indicates significant impairment. Her motor skills were severely affected and according to the NIH stroke scale, high scores usually indicate high states of impairment while 0 or lower indicates normal functioning. The NIH stroke scale is an assessment done to determine the effect of acute cerebral infraction. It includes 15 neurological-based questions/tasks scored ranging from 0-3 or 5 with 34 as a possibly. UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY CONT’D 3. What are the factors that place an individual at risk for stroke? Family History/Race: risk increases if a close/immediate family have had a stroke. It is mostly common in African Americans than Caucasians Gender: Mostly common in men than women Age: Chances of a stroke increases above age 55 years Heart Attack: Causes the body to become weaken heightening the tendency of a stroke Cigarette Smoking: The presence of nicotine and carbon monoxide in cigarette smoke UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY CONT’D damages the cardiovascular system increasing the risk of a stroke. Hypertension: Causes the arteries to narrow which makes it easier for cholesterol plaques or blood clots to block blood flow to deep brain tissues. Poor Diet: Diets high in saturated fats, Trans fats and cholesterol can lead to high blood increasing chances of developing medical conditions and a stroke. Drug Abuse: The use of cocaine, amphetamines and heroin can lead to medical complication as well as a stroke. UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY CONT’D 4 What specific signs and symptoms are noted with . Mrs. Noland’s exam and history are consistent with her diagnosis? Sudden Dizziness No Speech or Trouble speaking Paralysis of on the ride side of the body and face UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY CONT’D 5. What is rtPA? Why was it administered? rtPA is short for Recombinant Tissue Plasminogen Activator; commercially known as Alteplase, which is used to alleviate central line blockages caused by clot formation. Administered/ Prescribed at in early stages of ischemic stroke can lead to early detection and alleviation of the blockage, which can cause stroke and partially restore neurologic function. UNDERSTANDING THE DISEASE AND PATHOPHYSIOLOGY 6. Which symptoms that you identified CONT’D in question 4 may place Mrs. Noland at nutritional risk? Explain your rationale. A symptom that can used to identify nutritional risk would be Mrs. Noland’s inability to properly move her face and operate her tongue for speech. This can be considered a nutritional risk because it may pose difficulty for her orally eating and swallowing. UNDERSTANDING NUTRITION THERAPY 7. Define Dysphagia Dysphagia is the medical term for swallowing difficulties. Some people with dysphagia have problems swallowing certain foods or liquids, while others can't swallow at all. Other signs of dysphagia include: coughing or choking when eating or drinking bringing food back up, sometimes through the nose UNDERSTANDING NUTRITION THERAPY a sensation that food is stuck in your throat or chest persistent drooling of saliva being unable to chew food properly a 'gurgly' wet sounding voice when eating or drinking Over time, dysphagia can also cause symptoms such as weight loss and repeated chest infections. UNDERSTANDING NUTRITION THERAPY 8. What is the primary nutrition implication of dysphagia? The primary nutrition implication of dysphagia in the inability to deliver nutrients to the stomach for absorption. This can reduce intake and inability to eat or swallow causing depression. UNDERSTANDING NUTRITION THERAPY 9. Describe the four phases of swallowing: Oral preparation: The chewing of food and mixing it with saliva as the tongue mixes it around, forming bolus. Oral transit: The backward movement of the bolus to the rear of the oral cavity by the tongue squeezing against the hard and soft palates. UNDERSTANDING NUTRITION THERAPY Pharyngeal: The phase begins when the bolus progressed past the facial arches and is quickly followed in succession by the following steps: Elevation of the soft palate, closing off the nasopharynx (prevents oropharyngeal regurgitation). Elevation of the hyoid and larynx with adduction of the vocal cords, protecting the airway. Contraction of the pharynx while the cricopharyngeal sphincter relaxes, allowing food to pass into the esophagus. Breathing resumes. Esophageal: This is the phase which the bolus continues to travel down the esophagus into the stomach. UNDERSTANDING NUTRITION THERAPY UNDERSTANDING NUTRITION THERAPY 10. It is determined that Mrs. Noland dysphagia is centered in the esophageal transit phase, and she has reduced esophageal peristalsis. Which dysphagia diet level is appropriate to try with Mrs. Noland? Peristalsis is slow which causes transit of bolus from the esophagus to stomach to be slow. More time will be needed therefore for her to eat her meals. An appropriate diet level for Mrs. Noland would be level 3-Dysphagia Advanced soft foods that require more chewing ability. UNDERSTANDING NUTRITION THERAPY 11. Describe a bedside swallowing assessment. What are the background and training requirements of a speech-language pathologist? The bedside swallowing assessment is a component of the diagnostic process which comprises of: screening, clinical exam and instrumental assessment. The (SLP) will normally do this assessment. UNDERSTANDING NUTRITION THERAPY It is done to check for signs of dysphagia and aspiration. Firstly the SLP will evaluate: the patient’s medical history; the nature of the patients swallowing problem; the substances that cause these problems; the frequency and severity of the symptoms; they may also ask family members about the patients condition UNDERSTANDING NUTRITION THERAPY Secondly the SLP will observe: The patient’s teeth, lips, jaws, tongue, cheeks, and soft palate. Particular movements like smacking of lips together or sticking out your jaw. Particular sounds, coughs, or clearing of the patients throat. UNDERSTANDING NUTRITION THERAPY Reflexes for gagging and coughing Voice quality after swallowing for “wetness”, which is an indicator of aspiration Bolus control and laryngeal elevation Lastly, the patient will have to swallow multiple substances from water, thicker liquids, pureed foods, soft foods and even regular foods. UNDERSTANDING NUTRITION THERAPY A speech language pathologist works to prevent, assess, diagnose and treat speech, language, social communication, cognitive communication and swallowing disorders in children and adults. They work in different research, education and health care settings. UNDERSTANDING NUTRITION THERAPY Training; Complete an undergraduate program in Communication Sciences and Disorders. Courses done in this degree are: statistics, social/behavioral, physical and biological sciences related to: Normal language development Language Disorders and Phonology Linguistics Anatomy of hearing speech and mechanisms 1. UNDERSTANDING NUTRITION THERAPY 2. Complete CAA-Accredited Graduate Program in Speech- Language Pathology/ Communicative Sciences and Disorders Clinical Practicum Requirement 300-375 hours of supervised practice 3. Complete Post Graduate fellowship 1260 hours UNDERSTANDING NUTRITION THERAPY 4. Take a national exam in Speech Language Pathology (ETS) Educational Testing Services. You can do it while doing the post graduate fellowship or after doing the graduate degree. 5. Apply for the state licensure as a speechlanguage pathologist 6. Consider Professional Certification from (ASHA) UNDERSTANDING NUTRITION THERAPY 12. Describe a modified barium swallow or fiberoptic endoscopic evaluation of swallowing. A modified barium swallow (MBS) is an x-ray procedure done, to examine problems with swallowing. Liquid barium is a white, chalky solution that helps healthcare providers see the pictures more clearly. Barium is mixed with foods and liquids of different consistencies to show how they are swallowed. This helps healthcare providers decide what foods or liquids are good for the patient to consume. AND A fiberoptic evaluation of swallowing (FEES) test is a procedure used to assess how well a patient can swallow. During the procedure, a speech-language pathologist (SLP) passes a thin, flexible instrument called the endoscope through your nose and pharynx. Then it sits in the epiglottis for most of the viewing and then moved down after each swallow so the vocal folds can be seen. The endoscope has a tiny camera and light attached to it. This test also helps to assess if you a patient is having any problems with any part of the swallowing process. UNDERSTANDING NUTRITION THERAPY 13. What is the National Dysphagia Diet? Describe the major difference among the four levels of the diet. The National Dysphagia Diet (NDD), published in 2002 by the American Dietetic Association (now Academy of Nutrition and Dietetics), aims to establish standard terminology and practice applications of dietary texture modification in dysphagia management. The NDD was developed through consensus by a panel of dietitians, SLPs, and a food scientist. UNDERSTANDING NUTRITION THERAPY N.B. This is where the (IDDSI) according to the academy of nutrition and came about. The International Dysphagia Diet Standardization Initiative seeks to create global standardized terminology and definitions for texturemodified foods and thickened liquids to improve the safety and care for individuals with dysphagia. The academy and ASHA together supported May 1, 2019, as the official launch date of the IDDSI implementation in the US. This announcement was made in 2018 at the food and nutrition conference and Expo in Washington D.C. UNDERSTANDING NUTRITION THERAPY NDD Level 1: Dysphagia-Pureed Diet (homogenous, very cohesive, pudding-like, requiring very little chewing ability)- Hot cereals/porridge NDD Level 2: Dysphagia-Mechanical Altered Diet (cohesive, moist, semisolid foods, requiring some chewing). -Bananas NDD Level 3: Dysphagia-Advanced Diet (soft foods that require more chewing ability).-thin-sliced tender chunks or ground meats. Regular (all foods allowed). -Regular foods. Additionally, we have the viscosity levels of thickening liquids which are as follows: Nectar -like level: Fluids run freely off of the spoon, but leaves a mild coating on the spoon. Honey- like level: Fluids slowly drips off of the end of the spoon. Pudding-like level: Fluids remains on the spoon and does not flow off. UNDERSTANDING NUTRITION THERAPY 14. Thickening agents and specialty food products are often used to provide the texture changes needed for the dysphagia diet. Describe one of these products and how they may be incorporated into the diet. There are two types of thickening agents: xanthan gum thickeners and starch based thickeners. One product that can be used is something called the THICKEN UP CLEAR produced by NESTLE. It is a xanthan gum thickener PICTURE UNDERSTANDING NUTRITION THERAPY It’s easy to use, thickens and stabilizes rapidly, won’t continue to thicken overtime, clump free, and remain transparent. It’s clear, odorless, tasteless and low calorie, which are all characteristics of xanthan gum based thickeners. UNDERSTANDING NUTRITION THERAPY Example of how it works; 125 ml to 1 scoop- Gives mildly-thick, nectar-like consistency 125ml to 2 scoops- Gives moderately thick, honey like consistency 125ml to 3-3.5 scoops- Gives extremely thick, pudding/spoon thick consistency It can be used in juices and smoothies. NUTRITION ASSESSMENT 15. Mrs. Noland’s usual body weight is approximately 165 lbs. Calculate and interpret her BMI. UBW= 165lbs (75kg) BMI= kg/m2 (Do working) BMI= 30.5 Obese (Class 1) NUTRITION ASSESSMENT 16. Estimate Mrs. Noland’s energy and protein requirements. Should weight loss or weight gain be included in this estimation? What is your rationale. Nutrient Requirements Mifflin St. Jeor Equation: 10 (wt) + 6.25 (ht) -5(age) -161 (Female) 10 (75) + 6.25(157.5)-5(77)-161 = 1188 multiplied by 1.2 = 1426 For stoke: 1-1.25 g/kg Protein = 1 x 75kg = 75g NUTRITION ASSESSMENT 16. Should weight loss or weight gain be included in this estimation? What is your rationale. Weight loss should be included in estimation or weight maintenance because she is already obese and one of the primary nutrition implications of dysphagia is malnutrition which can lead to weight loss. NUTRITION ASSESSMENT 17. Using Mrs. Noland usual dietary intake, calculate the total number of kilocalories she consumed as well as the energy distribution of kilocalories for protein, carbohydrate, and fat. Mrs. Noland typically consumes 2533 kcal daily Fat: 25% Carbohydrates: 59% Protein: 17% 18. Compare this to the recommended intake for an individual with hyperlipidemia and hypertension. Do these recommendations apply to Mrs. Noland at the present? Mrs. Noland is consuming too much sodium and cholesterol. Her sodium intake is above normal. So I wont say she is following the recommended intake at the time. She should be following the TLC Diet, and DASH diet. NUTRITION ASSESSME NT NUTRITION ASSESSMENT The TLC (Therapeutic Lifestyle Changes) diet is one of several heart-healthy diets that can lower cholesterol and help lower your risk of heart disease or stroke. You get 25% to 35% of your daily calories from fat, mainly from unsaturated fat. You get 50% to 60% of your daily calories from carbohydrates You get less than 7% of your daily calories from saturated fat. You eat no more than 200 milligrams (mg) of cholesterol a day. You avoid trans fat. DASH Diet Diet used to treat hypertension. Standard DASH diet. You can consume up to 2,300 milligrams (mg) of sodium a day. Lower sodium DASH diet. You can consume up to 1,500 mg of sodium a day. And the amount of servings: NUTRITION ASSESSMEN T Grains: 6 to 8 servings a day Vegetables: 4 to 5 servings a day Fruits: 4 to 5 servings a day Dairy: 2 to 3 servings a day Lean meat, poultry and fish: 6 one- ounce servings or fewer a day Nuts, seeds and legumes: 4 to 5 servings a week Fats and oils: 2 to 3 servings a day Sweets: 5 servings or fewer a week NUTRITION ASSESSMENT EAT TRACKER ANALYSIS COMPARED Mrs. Noland had an intake of: 2621.2 mg sodium Saturated fat: 20.2 grams Normal: 99 grams Trans fat: 4.4 grams Cholesterol: 239.6 Normal: Less than 200mg Fruits and Vegetables: 7 servings Grains: 5 servings Milk and alternatives: 2 servings Meat: 2.5 servings 19. Fluid needs: By weight: 30 – 35 ml per weight in kg • = 30ml x 75 kg • = 2,250 ml By age and weight: 1 10 kg of body weight 100ml/kg st • 2nd 10 kg of body weight +50ml/kg • Remaining kg of body weight (age >50) +15ml /kg • 10kg x 100ml = 1000ml • 10kg x 50ml = 500ml • 55kg x 15ml = 825ml • TOTAL = 2325 ml By energy needs: 1ml of fluid per calorie consumed • =1426Kcal x 1ml • = 1426 ml NUTRITION ASSESSMEN T NUTRITION ASSESSMENT 20. Which method of fluid estimation appears most reasonable for Mrs. Noland? Explain We believe that the age and weight fluid calculation is best for Mrs. Noland because it takes into consideration her age which causes major changes in her body and her current weight. This method allows for an adjustment as her weight decreases or increases. NUTRITION ASSESSMENT 21. From the information gathered within the intake domain, list possible nutrition problems using the diagnostic term. Excessive Energy Intake Excessive Oral food and Beverage Intake Inadequate Fluid Intake Chemistry Normal Value Mrs. Noland's Reason for Abnormality Nutritional Implications Transferrin 250 -380 mg/dL 182 mg/dL Poor production in the liver indicating possible liver disease Treatment management should aim to maintain an adequate protein and caloric intake and to correct nutrient deficiencies Alk phosphate 30 -120 U/L 179 U/L Caused by liver disease or bone disorder Increase caloric intake and include nutritional supplements to compensate for deficiencies in fat soluble vitamins. CHOL 120-199 mg/dL 210 mg/dL High levels of LDL Increase in soluble fibre intake. Limit the amount of animal fats and use good fats in moderation Lose extra pounds and maintain a healthy weight HDL-C >55 mg/dL 40 mg/dL High carb diet and excessive weight Increase levels of physical activity, limit intake of saturated and transfat LDL <130 mg/dL 155 mg/dL Low levels of HDL (HDL fights LDL) Increase in soluble fibre intake. Limit the amount of animal fats and use good fats in moderation Lose extra pounds and maintain a healthy weight TG 35-135 mg/dL 198 mg/dL Poor diet Increase in soluble fibre intake. Limit the amount of animal fats and use good fats in moderation Lose extra pounds and maintain a healthy weight NUTRITION ASSESSMENT 23. From the information gathered within the clinical domain, list possible nutrition problems using the diagnostic term. Altered nutrition-related laboratory values Overweight/ Obesity NUTRITION DIAGNOSIS 24. TWO HIGH PRIORITY NUTRTION PROBLEMS AND PES STATEMENT: Excessive sodium intake related to food and nutrition related education deficit as evidenced by estimated sodium intake that is more than recommended. Altered nutrition-related laboratory values related to the liver as evidenced by ALT phosphate levels. NUTRITION DIAGNOSIS 25. For each of the PES statements that you have written, establish an ideal goal (based on signs and symptoms) and an appropriate intervention First PES: Based on the signs and symptoms the goal is to reduce the amount of sodium intake our patient consumes because of her hypertension. She should be enrolled in counselling and put on the DASH Diet where she will have salt restriction. The goal is to reduce her intake of sodium to1500 mg per day for a month to bring her blood pressure down 120/80. NUTRITION DIAGNOSIS Second PES Statement: The goal is to determine why her ALT phosphate levels are high by referring her to a doctor to make a proper medical diagnosis which will then determine if nutrition therapy is mandatory. Dietitians can only make a nutrition diagnosis, but some nutrition counseling can be offered to her introducing her to different liver disease diets. Here are some pointers: What to avoid: Don’t eat foods high in fat, sugar and salt. Stay away from a lot of fried foods including fast food restaurant meals. Talk to your doctor about alcohol and your liver health: Depending on the state of your liver, you should avoid alcohol. Eat a balanced diet: Select foods from all food groups: Grains, fruits, vegetables, meat and beans, milk, and oil. Eat food with fiber: Fiber helps your liver work at an optimal level. Fruits, vegetables, whole grain breads, rice and cereals can take care of your body’s fiber needs. Drink lots of water: It prevents dehydration and it helps your liver to function better. Term Consistency Definition Refers to the way in which a substance holds together Texture Those properties of a food that are sensed by touch in the mouth and in the hands. The state of being thick, sticky, and semi-fluid in consistency. It also refers to the resistance of a fluid to change in shape. Viscosity denotes opposition to flow. Viscosity NUTRITION MONITORING AND EVALUATION Example Pureed vegetables will be smooth and moist. Spoon would not be able to stand in it. Foods can be soft, hard, crunchy, smooth, mushy. Water has low viscosity as it is thin and flows freely, easily taking any shape. 26. To maintain or attain normal nutritional status while reducing danger of aspiration and choking, texture and/or viscosity are personalized for a patient with dysphagia. In the following table, define each term used to describe characteristics of foods and give an example. Orange Juice Raisin bran 2% milk Banana Coffee Sweetener Chicken tortellini soup Saltine crackers Canned pears Iced tea Baked Chicken Baked potato Steamed broccoli Margarine Canned peaches Popcorn Coca-cola Ice cream add a gum thickner can be softened by adding low fat milk substitute with low fat milk should be cut into bite sized pieces should be eliminated as it causes a boost in blood pressure decrease usage graudally ingredients should be cut into bite sized pieces should be avoided use fresh unprocessed pears as a substitute replace with water cut in thin slices/ strip Mash potatoes cut into small chunks use butter as a replacement substitute with fres, unprocessed peaches unsalted plain popcorn, with no butter eliminate use low fat yogurt as a replacement NUTRITION MONITORING AND EVALUATION Using Mrs. Noland’s 24 hour recall, make suggestions for consistency changes or food substitutions to Mrs. Noland and her family 27. NUTRITION MONITORING AND EVALUATION 28. Mrs. Noland would have problems of unilateral paralysis on the right side of her body. Her meals would have to be of the right consistency and texture in order to maintain her nutritional intake and avoid issues connected to dysphagia. Her intake of sodium and fats need to be reduced in order to alleviate her issues of hypertension and hyperlipidemia. This change would mean that Mr. Noland should receive the necessary counselling in this area. Mr. Noland should know that Mrs. Noland’s diet should include more fruits, vegetables, and low-fat dairy foods. He should cut back on foods that are high in saturated fat, cholesterol, and trans fats. Feed her more whole-grain foods, fish, poultry, and nuts and limit sodium, sweets, sugary drinks, and red meats. 29. Yes Mrs. Noland would be an NUTRITION MONITORING AND EVALUATION appropriate candidate for a stroke rehabilitation program because her situation though unfortunate has not left her fully incapacitated. She can benefit from stroke rehabilitation which can help to give her back her independence.