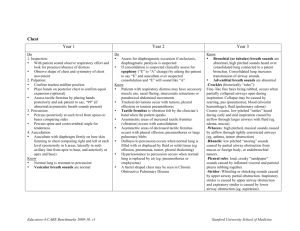
EXAM 3_316 Ch. 19 & 20 Base- top Apex- bottom, apical pulse- 5th intercostal midclavicular There are four valves in the heart. The two atrioventricular (AV) valves separate the atria and the ventricles. The right AV valve is the tricuspid, and the left AV valve is the bicuspid or mitral valve. The valves’ thin leaflets are anchored by collagenous fibers (chordae tendineae) to papillary muscles embedded in the ventricle floor. The AV valves open during the heart's filling phase, or diastole, to allow the ventricles to fill with blood. During the pumping phase, or systole, the AV valves close to prevent regurgitation of blood back up into the atria. The papillary muscles contract at this time so the valve leaflets meet and unite to form a perfect seal without turning themselves inside out. The semilunar (SL) valves are set between the ventricles and the arteries. Each valve has three cusps that look like half moons. The SL valves are the pulmonic valve in the right side of the heart and the aortic valve in the left side of the heart. They open during pumping, or systole, to allow blood to be ejected from the heart. It has two phases, diastole and systole. In diastole the ventricles relax and fill with blood. This takes up two thirds of the cardiac cycle. Heart contraction is systole. During systole blood is pumped from the ventricles and fills the pulmonary and systemic arteries. This is one third of the cardiac cycle. The closure of the AV valves contributes to the first heart sound (S1) and signals the beginning of systole. Matches up with carotid pulse. BEST HEARD: APEX This closure of the semilunar valves causes the second heart sound (S2) and signals the end of systole. BEST HEARD: BASE Third Heart Sound (S3). Normally diastole is a silent event. However, in some conditions ventricular filling creates vibrations that can be heard over the chest. These vibrations are S3. S3 occurs when the ventricles are resistant to filling during the early rapid filling phase (protodiastole). This occurs immediately after S2, when the AV valves open and atrial blood first pours into the ventricles. Abnormal in adults may indicate HF (Right HF- peripheral edema, Left HF- lung sounds (bubbling, crackles)) Abnormal in persons over age 35. Fourth Heart Sound (S4). S4 occurs at the end of diastole, at presystole, when the ventricle is resistant to filling. The atria contract and push blood into a noncompliant ventricle. This creates vibrations that are heard as S4. S4 occurs just before S1. Murmurs: A murmur is a gentle, blowing, swooshing sound that can be heard on chest wall Blood circulating through normal cardiac chambers and valves usually makes no noise. However, some conditions create turbulent blood flow and collision currents. These result in a murmur, much like a pile of stones or a sharp turn in a stream creates a noisy water flow. A murmur is a gentle, blowing, swooshing sound that can be heard on the chest wall. Conditions resulting in a murmur are as follows: 1. Velocity of blood increases (flow murmur) (e.g., in exercise, thyrotoxicosis) 2. Viscosity of blood decreases (e.g., in anemia) 3. Structural defects in the valves (a stenotic or narrowed valve, an incompetent or regurgitant valve) or unusual openings occur in the chambers (dilated chamber, septal defect). A murmur sounds much the same but is caused by a cardiac disorder. Some aortic valve murmurs (aortic stenosis) radiate to the neck and must be distinguished from a local bruit. The murmur of mitral stenosis is low-pitched and rumbling, whereas that of aortic stenosis is harsh. Sounds: Frequency or pitch: high or low pitched. Intensity/loudness: loud or soft. Duration: very short for heart sounds; silent periods are longer. Timing: systole or diastole EXAM 3_316 Aging- increase systolic BP (thickening and stiffening of arteries; arteriosclerosis), left ventricular wall thickens, diastolic BP may decrease later, Electrocardiograph: changes in the ECG occur as a result of histologic changes in the conduction system. These changes include: • Prolonged P-R interval (first-degree AV block) and prolonged Q-T interval, but the QRS interval is unchanged. • Left axis deviation from age-related mild LV hypertrophy and fibrosis in left bundle branch. • Increased incidence of bundle branch block. Hypertension is 2 to 3 times more common among women taking oral contraceptives The prevalence of hypertension is 41.4% for African Americans, 25.8% for American Indians or Alaska natives, 28.1% for Whites, 22.2% for Hispanics, and 18.7% for Asians.1 Compared with Whites, African Americans develop high BP earlier in life, and their average BPs are much higher. This results in African Americans having a greater rate of stroke, death from heart disease, and end-stage kidney disease. Cholesterol- 39.9% of Mexican-American men and 30.4% of Mexican-American women; 30.1% of White men and 29.3% of White women; and 33.1% of African-American men and 31.2% of African-American women. DM- Approximately 12.6% of African Americans 20 years of age and older, 11.8% of Hispanics, 8.4% of Asians, and 7.1% of Whites have DM 1. Describe techniques used to assess the cardiovascular and peripheral vascular systems. Subjective Data: 1. Chest pain 2. Dyspnea (paroxysmal. constant or intermittent. recumbent) 3. Orthopnea (how many pillows) 4. Cough (sputum production, mucoid or purulent. hemoptysis is often a pulmonary disorder but also occurs with mitral stenosis) 5. Fatigue 6. Cyanosis or pallor 7. Edema (common w/heart failure) 8. Nocturia (Recumbency at night promotes fluid resorption and excretion; this occurs with heart failure in the person who is ambulatory during the day) 9. Past cardiac history 10. Family cardiac history 11. Patient-centered care (cardiac risk factors: Collect data regarding elevated cholesterol, elevated BP, blood sugar levels above 100 mg/dL or known DM, obesity, cigarette smoking, low activity level, and length of any hormone replacement therapy for postmenopausal women). 1. Leg pain or cramps (Apply PQRSTU, associated w/anything?) 2. Skin changes on arms or legs (temp- PAD, Critical link-why ask about skin changes related to circulation?) 3. Swelling in arms/legs (edema is bilateral when the cause is generalized (heart failure) or unilateral when it is the result of a local obstruction or inflammation) 4. Lymph node enlargement (occur with infection, malignancies, and immunologic diseases) 5. Meds. 6. Smoking history (constricts arteries, increases coagulability, injures endothelium, and promotes inflammation. strongest risk factor for PAD; starting smoking at ≤16 years more than doubles future pad risk) o Aging: 1. Do you have any known heart or lung disease: hypertension, CAD, chronic emphysema, or bronchitis? 2. Do you take any medications for your illness such as digitalis? Aware of side effects? Have you recently stopped taking your medication? Why? 3. Environment: Does your home have any stairs? How often do you need to climb them? Does this have any effect on ADLs? Assess carotid arteries, the person can be sitting up. To assess jugular veins and the precordium, the person should be supine with the head and chest elevated between 30 and 45 degrees. Stand on the person's right side. The room must be warm—cold makes the person uncomfortable, and shivering interferes with heart sounds. Take scrupulous care to ensure quiet; heart sounds are very soft, and any ambient room noise masks them. EXAM 3_316 Neck vessels o Palpate carotid, auscultate carotid. Note characteristics of its waveform: smooth rapid upstroke. summit rounded and smooth. downstroke more gradual and has a dicrotic notch caused by closure of aortic valve o Carotid sinus hypersensitivity is the condition in which pressure over the carotid sinus leads to a decreased heart rate, decreased BP, and cerebral ischemia with syncope. This may occur in older adults with hypertension or occlusion of the carotid artery. o Auscultate for a bruit. Ask person to take a breath, exhale, and hold it briefly while you listen so that tracheal breath sounds do not mask or mimic a carotid artery bruit. A bruit indicates turbulence from a local vascular cause and is a marker for atherosclerotic disease. This increases the risk of transient ischemic attack (TIA) and ischemic stroke. However, a bruit also occurs in 5% of those age 45 to 80 years who have no significant carotid disease. A carotid bruit is audible when the lumen is occluded by ½ to ⅔. Bruit loudness increases as the atherosclerosis worsens until the lumen is occluded by ⅔. After that, bruit loudness decreases. When the lumen is completely occluded, the bruit disappears. Thus absence of a bruit does not ensure absence of a carotid lesion. A murmur sounds much the same but is caused by a cardiac disorder. Some aortic valve murmurs (aortic stenosis) radiate to the neck and must be distinguished from a local bruit. o Inspect jugular venous pulse. Look for pulsations of internal jugular veins in area of suprasternal notch or around origin of sternomastoid muscle around clavicle. distinguish internal jugular vein pulsation versus carotid artery pulse. It is easy to confuse them because they lie close together Anterior chest o Before you begin, alert person that you always listen to heart in a number of places on chest, and just because you are listening a long time does not necessarily mean that something is wrong o Begin with diaphragm endpiece and use following routine 1. Note rate and rhythm (regular or steady, irregular is abnormal) 2. Identify S1 and S2 3. Assess S1 and S2 separately 4. Listen for extra heart sounds 5. Listen for murmurs o Apical pulse- heave or lift is a sustained forceful thrusting of the ventricle during systole. It occurs with ventricular hypertrophy as a result of increased workload. A right ventricular heave is seen at the sternal border; a left ventricular heave is seen at the apex • Location—The apical impulse should occupy only one interspace, the 4th or 5th, and be at or medial to the midclavicular line • Size—Normally 1 × 2 cm • Amplitude—Normally a short, gentle tap • Duration—Short; normally occupies only first half of systole o Heart auscultation Second right interspace—Aortic valve area Second left interspace—Pulmonic valve area EXAM 3_316 Left lower sternal border—Tricuspid valve area Fifth interspace at around left midclavicular line—Mitral valve area Begin with the diaphragm end piece and use the following routine: (1) note the rate and rhythm, (2) identify S1 and S2, (3) assess S1 and S2 separately, (4) listen for extra heart sounds, and (5) listen for murmurs. The soft diastolic murmur of aortic regurgitation may be heard only when the person is leaning forward in the sitting position. Splitting of S2. A split S2 is a normal phenomenon that occurs toward the end of inspiration in some people. Recall that closure of the aortic and pulmonic valves is nearly synchronous. Because of the effects of respiration on the heart described earlier, inspiration separates the timing of the two valves' closure, and the aortic valve closes 0.06 second before the pulmonic valve. Instead of one DUP, you hear a split sound—T-DUP (Fig. 19-26). During expiration, synchrony returns, and the aortic and pulmonic components fuse together. A split S2 is heard only in the pvalve area (2nd interspace) A fixed split is unaffected by respiration; the split is always there. A paradoxical split is the opposite of what you would expect; the sounds fuse on inspiration and split on expiration Palpation- A thrill is a palpable vibration. It feels like the throat of a purring cat. The thrill signifies turbulent blood flow and directs you to locate the origin of loud murmurs. However, absence of a thrill does not rule out the presence of a murmur. Accentuated first and second heart sounds and extra heart sounds also may cause abnormal pulsations o o Neck 1. Carotid pulse—Observe and palpate 2. Observe jugular venous pulse 3. Estimate jugular venous pressure Precordium Inspection and palpation o 1. Describe location of apical impulse. o 2. Note any heave (lift) or thrill. Auscultation o 1. Identify anatomic areas where you listen. o 2. Note rate and rhythm of heartbeat. o 3. Identify S1 and S2 and note any variation. o 4. Listen in systole and diastole for any extra heart sounds. o 5. Listen in systole and diastole for any murmurs. o 6. Repeat sequence with bell. o 7. Listen at the apex with person in left lateral position o 8. Listen at the base with person in sitting position. o o o EXAM 3_316 Arms o o o o o o flattening of angle and clubbing (diffuse enlargement of terminal phalanges, Normal nail bed angle is 160 degrees) occur with congenital cyanotic heart disease and cor pulmonale. Refill lasting more than 1 or 2 seconds signifies vasoconstriction or decreased cardiac output (hypovolemia, heart failure, shock). The hands are cold, clammy, and pale. Edema of upper extremities occurs when lymphatic drainage is obstructed after breast surgery or radiation. Edema of UE Lymphatic blockage, DVT, infection Radial & ulnar pulse- 3+ Increased/full/bounding; 2+ Normal; 1+ Weak; 0 Absent Full, bounding pulse (3+) occurs with hyperkinetic states (exercise, anxiety, fever), anemia, and hyperthyroidism. Weak, “thready” pulse (1+) occurs with shock and PAD Check the epitrochlear lymph nodes in the depression above and behind the medial condyle of the humerus. Do this by “shaking hands” with the person and reaching your other hand under the person's elbow to the groove between the biceps and triceps muscles, above the medial epicondyle (usually non-palpable) Legs o o o o o o o Peripheral arterial disease (PAD) affects noncoronary vessels and refers to arteries affecting the limbs Legs have three types of veins 1. Deep veins run alongside deep arteries and conduct most of venous return from the legs 2. Superficial veins are great and small saphenous vein 3. Perforators are connecting veins that join two sets Pallor with vasoconstriction; erythema with vasodilation; cyanosis. Locate femoral arteries just below inguinal ligament halfway between pubis and anterior superior iliac spines. To help expose femoral area, particularly in obese people, ask person to bend his or her knees to side in a froglike position. Press firmly and then slowly release, noting pulse tap under your fingertips. If this pulse is weak or diminished, auscultate site for a bruit. Posterior tibial pulse curve your fingers around medial malleolus. Feel the tapping right behind it in groove between malleolus and Achilles tendon. Dorsalis pedis pulse requires a very light touch. Normally it is just lateral to and parallel with extensor tendon of big toe. Do not mistake pulse in your own fingertips for person’s. In adults over 45 years, occasionally either dorsalis pedis or posterior tibial pulse may be hard to find, but not both on the same foot Ask the person to stand so that you can assess venous system: Note any visible, dilated, and tortuous veins. If present, varicose veins cause pain, swelling, fatigue, and cramping. Malnutrition: thin, shiny, atrophic skin; thick-ridged nails; loss of hair; ulcers; gangrene. Malnutrition, pallor, and coolness occur with arterial insufficiency. Diffuse bilateral edema occurs with systemic illnesses. Acute, unilateral, painful swelling and asymmetry of calves of 1 cm or more is abnormal; refer the person to determine whether DVT is present. EXAM 3_316 o o o o o o o o o o o o Skin- Brown discoloration occurs with chronic venous stasis caused by hemosiderin deposits from red blood cell degradation. Venous ulcers occur usually at medial malleolus because of bacterial invasion of poorly drained tissues. With arterial deficit, ulcers occur A unilateral cool foot or leg or a sudden temperature drop as you move down the leg occurs with arterial deficit. Inguinal lymph nodes- abnormal: Nodes that are enlarged, tender, or fixed in area. The popliteal pulse is a more diffuse pulse and can be difficult to localize. With the leg extended but relaxed, anchor your thumbs on the knee and curl your fingers around into the popliteal fossa (Fig. 20-16). Press your fingers forward hard to compress the artery against the bone (the lower edge of the femur or the upper edge of the tibia). Often it is just lateral to the medial tendon. The dorsalis pedis pulse requires a very light touch. Normally it is just lateral to and parallel with the extensor tendon of the big toe. Do not mistake the pulse in your own fingertips for that of the person. Edema- If pitting edema is present, grade it on the following scale: 1+, Mild pitting, slight indentation, no perceptible swelling of the leg 2+, Moderate pitting, indentation subsides rapidly 3+, Deep pitting, indentation remains for a short time, leg looks swollen 4+, Very deep pitting, indentation lasts a long time, leg is grossly swollen and distorted. Bilateral pitting edema calls for an examination of the neck veins. If the neck veins are abnormally distended, the peripheral edema may be related to heart disease or pulmonary hypertension).11 If neck veins are normal, something else may cause the edema Color changes- If you suspect an arterial deficit, raise the legs about 12 inches off the table and ask the person to wag the feet for about 30 seconds to drain off venous blood. The skin color now reflects only the contribution of arterial blood. A light-skinned person's feet normally look a little pale but still should be pink. A dark-skinned person's feet are more difficult to evaluate, but the soles should reveal extreme color change. Dependent rubor (deep blue-red color) occurs with severe arterial insufficiency. Chronic hypoxia produces loss of vasomotor tone and pooling of blood in the veins. Delayed venous filling occurs with arterial insufficiency. *Doppler- used when can’t find pulse, hear a whooshing sound; measures low blood pressure or blood pressure in lower extremity Skin discoloration, skin ulcers, or gangrene, note size and exact location Chronic venous stasis causes brown discoloration and ulceration/infection Chronic arterial deficit causes ulcers on toes If lower legs look asymmetric: measure leg at widest point, taking care to measure other leg in exactly same place, same number of centimeters down from patella or other landmark Palpate for temperature along legs down to feet, comparing symmetric spots Or you may sharply dorsiflex foot toward tibia Pulsus Bigeminus- ectopy, irregular conduction (from somewhere else other than the SA node) Pulsus Paradoxus- changes with respiration cycle EXAM 3_316 2. Identify appropriate cardiovascular and peripheral vascular assessment techniques for clients based on age, development, and other psychosocial or environmental variables. A gradual rise in SBP is common with aging; the DBP stays fairly constant with a resulting widening of pulse pressure. Some older adults experience orthostatic hypotension, a sudden drop in BP when rising to sit or stand. Left ventricular wall becomes thicker but the overall size of the heart does not change Pulse pressure increases No change in resting heart rate or cardiac output at rest Ability of heart to augment Dysrhythmias EKG changes Use caution in palpating and auscultating the carotid artery. Avoid pressure in the carotid sinus area, which could cause a reflex slowing of the heart rate. Pressure on the carotid artery could compromise circulation if already narrowed by atherosclerosis. The chest often increases in anteroposterior diameter with aging. This makes it more difficult to palpate the apical impulse and hear the splitting of S2. The S4 often occurs in older people with no known cardiac disease. Systolic murmurs are common, occurring in over 50% of aging people. The S3 is associated with heart failure and is always abnormal over age 35 years. Occasional premature ectopic beats are common and do not necessarily indicate underlying heart disease. When in doubt, obtain an ECG. However, consider that the ECG records for only one isolated minute in time and may need to be supplemented by a test of 24-hour ambulatory heart monitoring. Peripheral blood vessels grow more rigid with age- arteriosclerosis= rise in systolic blood pressure. Do not confuse this process with atherosclerosis, or the deposition of fatty plaques on the intima of the arteries. Both processes are present with PAD in aging adults. PAD is underdiagnosed and undertreated, yet it is a large cause of morbidity and mortality in the United States. It increases dramatically with age and more men have PAD than women. Aging produces a progressive enlargement of the intramuscular calf veinsprolonged bed rest, prolonged immobilization, and heart failure increase the risk for deep vein thrombosis (DVT) and subsequent pulmonary embolism. Low-dose anticoagulant medication reduces the risk for venous thromboembolism. Loss of lymphatic tissue leads to fewer numbers of lymph nodes in older people and to a decrease in the size of remaining nodes. 3. Differentiate between normal and abnormal cardiovascular and peripheral vascular assessment findings that require further evaluation. Variation in pulses o Weak, thread-1+ o Full bounding-3+ o Pulsus Bigeminus-ectopy, irregular conduction o Pulsus Paradoxus-changes with respiration cycle Ateriosclerosis Atherosclerosis-PVD, CAD, MI Claudication distance Unilateral Edema of LE DVT? Inspect arms for color, size, or any lesions EXAM 3_316 Palpate pulses UE: radial and brachial Inspect legs for color, size, any lesions, or trophic skin changes Palpate temperature of feet and legs Palpate inguinal nodes Palpate pulses LE: femoral, popliteal, posterior tibial, and dorsalis pedis 4. Document health history and results of cardiovascular and peripheral vascular assessments in the client record utilizing documentation best practices. Sample Charting Subjective No chest pain, dyspnea, orthopnea, cough, fatigue, or edema. No history of hypertension, abnormal blood tests, heart murmur, or rheumatic fever in self. Last ECG 2 yrs. PTA, result normal. No stress ECG or other heart tests. o Family history: Father with obesity, smoking, and hypertension, treated diuretic medication. No other family history significant for CV disease. o Personal habits: Diet balanced in 4 food groups, 2 to 3 c. regular coffee/day; no smoking; alcohol, 1 to 2 beers occasionally on weekend; exercise, runs 2 miles, 3 to 4 ×/week; no prescription or OTC medications or street drugs. Objective Neck: Carotids' upstrokes are brisk and = bilaterally. No bruit. Internal jugular vein pulsations present when supine and disappear when elevated to a 45-degree position. Precordium: Inspection. No visible pulsations; no heave or lift. Palpation: Apical impulse in 5th ICS at left midclavicular line; no thrill. Auscultation: Rate 68 bpm, rhythm regular, S1-S2 are crisp, not diminished or accentuated, no S3, no S4 or other extra sounds, no murmurs. Assessment Neck vessels healthy by inspection and auscultation Heart sounds normal, no murmurs Sample Charting Subjective No leg pain, no skin changes, no swelling or lymph node enlargement. No history of heart or vascular problems, diabetes, or obesity. Does not smoke. On no medications. Objective Inspection: Extremities have pink-tan color without redness, cyanosis, or any skin lesions. Extremity size is symmetric without swelling or atrophy. Palpation: Temperature is warm and = bilaterally. All pulses present, 2+ and = bilaterally. No lymphadenopathy. Assessment Healthy tissue integrity Effective tissue perfusion EXAM 3_316 Reference lines pinpoint/map findings vertically on chest o Anterior chest: midsternal line and midclavicular line bisects center of each clavicle at a point halfway between palpated sternoclavicular and acromioclavicular joints. o Posterior chest wall: vertebral (or midspinal) line and scapular line, extends through inferior angle of scapula when arms are at sides of body. o Lateral chest by divided by three lines when arms at 90 degrees: Anterior axillary line: anterior axillary fold where pectoralis major muscle inserts. Posterior axillary line: posterior axillary fold where latissimus dorsi muscle inserts. Midaxillary line: apex of axilla and lies between and parallel to other two In inspiration increasing the size of the thoracic container creates a slightly negative pressure in relation to the atmosphere; therefore air rushes in to fill the partial vacuum. The major muscle responsible for this increase is the diaphragm. During inspiration contraction of the bell-shaped diaphragm causes it to descend and flatten. This lengthens the vertical diameter. Intercostal muscles lift the sternum and elevate the ribs, making them more horizontal. This increases the AP diameter. Expiration is primarily passive. As the diaphragm relaxes, elastic forces within the lung, chest cage, and abdomen cause it to dome up. All this squeezing creates a relatively positive pressure within the alveoli, and the air flows out. Four major functions of respiratory system o Supplying oxygen to the body for energy production o Removing carbon dioxide as a waste product of energy reactions o Maintaining homeostasis (acid-base balance/pH) of arterial blood o Maintaining heat exchange (less important in humans) Negative pressure for inspiration/positive pressure for expiration . Incidence of tuberculosis (TB) has declined in the U.S. o however, persons who are foreign-born and of racial or ethnic minorities have a disproportionately large incidence of TB disease o In 2012 the TB rates were: EXAM 3_316 11.5 times higher in foreign-born than in U.S.-born 8.7 million new cases of TB worldwide o Incidence of multi-resistant TB is increasing Prevalence rate of asthma in the U.S. in 2011 was 8.4%. o Most common chronic disease in childhood with a prevalence rate of 9.5% in children ages 0 to 17 years. o African Americans, Hispanics, and Native Americans experience more asthma-related problems and medical care than do Caucasians or Asians. Ch. 18 1. Describe techniques used to assess the respiratory system. Subjective Data: 1. Cough (sputum? Blood (hemoptosis)? Acute? Chronic?) 2. Shortness of breath (dyspnea? related to food, pollen, position, dust, animals, season, or emotion? paroxysmal nocturnal dyspnea is awakening from sleep with SOB and needing to be upright to achieve comfort, effect on ADLs) 3. Chest pain with breathing (point to it) 4. History of respiratory infections 5. Smoking history 6. Environmental exposure (work) 7. Patient-centered care (vaccines, self-care) Thoracic cage o Note shape and configuration of chest wall. o Spinous processes should appear in a straight line; thorax is symmetric, in an elliptical shape, with downward sloping ribs, about 45 degrees relative to spine; scapulae are placed symmetrically in each hemithorax. Skeletal deformities may limit thoracic cage excursion: scoliosis, kyphosis o Anteroposterior diameter should be less than transverse diameter. o The neck muscles and trapezius muscles should be developed normally for age and occupation. Neck muscles are hypertrophied in COPD from aiding in forced respirations across the obstructed airways. o Position- People with COPD often sit in a tripod position, leaning forward with arms braced against their knees, chair, or bed. This gives them leverage so the abdominal, intercostal, and neck muscles all can aid in expiration o Skin color- cyanosis with tissue hypoxia Posterior chest o Confirm symmetric chest expansion by placing your warmed hands sideways on the posterolateral chest wall with thumbs pointing together at the level of T9/10. Slide your hands medially to pinch up a small fold of skin between your thumbs. o Assess tactile (or vocal) fremitus- Fremitus is a palpable vibration. Sounds generated from the larynx are transmitted through patent bronchi and the lung parenchyma to the chest wall, where you feel them as vibrations. “99” Use palmar base (ball) of fingers or ulnar edge of one hand. Decreased fremitus occurs with obstructed bronchus, pleural effusion or thickening, pneumothorax, or emphysema. Any barrier that comes between the sound and your palpating hand decreases fremitus. Increased fremitus occurs with compression or consolidation of lung tissue (e.g., lobar pneumonia). This is present only when the bronchus is patent and the consolidation extends to the lung surface. Note that only gross changes increase fremitus. Small areas of early pneumonia do not significantly EXAM 3_316 affect it. Rhonchal fremitus is palpable with thick bronchial secretions. Pleural friction fremitus is palpable with inflammation of the pleura o Palpate- Crepitus is a coarse, crackling sensation palpable over the skin surface. It occurs in subcutaneous emphysema when air escapes from the lung and enters the subcutaneous tissue, as after open thoracic injury or surgery. Note any tenderness, skin temperature and moisture, detecting any superficial lumps or masses, and exploring any skin lesions noted on inspection. Lung fields o Resonance is the low-pitched, clear, hollow sound that predominates in healthy lung tissue in the adult. Hyperresonance is a lower-pitched, booming sound found when too much air is present such as in emphysema or pneumothorax. A dull note (soft, muffled thud) signals abnormal density in the lungs, as with pneumonia, pleural effusion, atelectasis, or tumor. Determine diaphragmatic excursion. Percuss to map out the lower lung border in both expiration and inspiration. o Auscultate- Evaluate the presence and quality of normal breath sounds. The person is sitting, leaning forward slightly, with arms resting comfortably across the lap. Instruct the person to breathe through the mouth, a little bit deeper than usual, but to stop if he or she begins to feel dizzy. Side-to-side comparison is most important. Crackles are abnormal. (minimize this by pressing harder or by wetting the hair with damp cloth). You should expect to hear three types of normal breath sounds in adult and older child. Three breath sounds: PITCH AMPLITUDE DURATIO N QUALITY NORMAL LOCATION BRONCHIAL (TRACHEAL) High Loud Inspiration < expiratio n Harsh, hollow tubular Trachea and larynx BRONCHOVESICULAR Moderat e Moderate Inspiration = expiratio n Mixed Over major bronchi where fewer alveoli are located: posterior, between scapulae especially on right; anterior, around upper sternum in 1st and 2nd intercostal spaces VESICULAR Low Soft Inspiration > expiratio n Rustling, like the sound of the wind in the trees Over peripheral lung 4elds where air 5ows through smaller bronchioles and alveoli EXAM 3_316 PITCH o o o o AMPLITUDE DURATIO N QUALITY NORMAL LOCATION Decreased or absent breath sounds occur: 1. When the bronchial tree is obstructed at some point by secretions, mucus plug, or a foreign body 2. In emphysema as a result of loss of elasticity in the lung fibers and decreased force of inspired air; the lungs also are already hyperinflated, so the inhaled air does not make as much noise 3. When anything obstructs transmission of sound between the lung and your stethoscope such as pleurisy or pleural thickening or air (pneumothorax) or fluid (pleural effusion) in the pleural space Increased breath sounds mean that sounds are louder than they should be. They have a high-pitched, tubular quality, with a prolonged expiratory phase and a distinct pause between inspiration and expiration. They sound very close to your stethoscope, as if they were right in the tubing close to your ear. They occur when consolidation (e.g., pneumonia) or compression (e.g., fluid in the intrapleural space) yields a dense lung area that enhances the transmission of sound from the bronchi. When the inspired air reaches the alveoli, it hits solid lung tissue that conducts sound more efficiently to the surface. Note the presence of any adventitious sounds (sounds that are abnormal) in the lungs. If present, they are heard as being superimposed on the breath sounds. They are caused by moving air colliding with secretions in the tracheobronchial passageways or by the popping open of previously deflated airways. Sources differ as to the classification and nomenclature of these sounds, but crackles (or rales) and wheeze (or rhonchi) are terms commonly used by most examiners. If you hear adventitious sounds, describe them as inspiratory versus expiratory, loudness, pitch, and location on the chest wall. Crackles are discontinuous popping sounds heard over inspiration; wheezes are continuous musical sounds heard mainly over expiration. One type of adventitious sound, atelectatic crackles, is not pathologic. They are short, popping, crackling sounds that last only a few breaths. When sections of alveoli are not fully aerated (as in sleepers or in older adults), they deflate slightly and accumulate secretions. Crackles are heard when these sections are expanded by a few deep breaths. Atelectatic crackles are heard only in the periphery, usually in dependent portions of the lungs, and disappear after the first few breaths or after a cough. Voice: The spoken voice can be auscultated over the chest wall just as it can be felt in tactile fremitus described earlier. Normal voice transmission is soft, muffled, and indistinct; you can hear sound through the stethoscope but cannot distinguish exactly what is being said. Pathology that increases lung density enhances transmission of voice sounds. testing for the possible presence of bronchophony, egophony, and whispered pectoriloquy. Eliciting voice sounds EXAM 3_316 usually not done in routine examination. these are supplemental maneuvers that are performed if you suspect lung pathology on basis of earlier data. Anterior chest o Ribs are sloping downward with symmetric interspaces. o Costal angle is within 90 degrees; development of abdominal muscles as expected for person’s age, weight, and athletic condition. Barrel chest has horizontal ribs and costal angle >90 degrees. Hypertrophy of abdominal muscles occurs in chronic emphysema. o Note person’s facial expression; facial expression should be relaxed, indicating unconscious effort of breathing. Tense, strained, tired facies and purse-lipped breathing (the lips in a whistling position) accompany COPD. By exhaling slowly and against a narrow opening, the pressure in the bronchial tree remains positive, and fewer airways collapse. o Assess the level of consciousness; level of consciousness should be alert and cooperative. Cerebral hypoxia may be reflected by excessive drowsiness or anxiety, restlessness, and irritability. o Note skin color and condition; lips and nail beds are free of cyanosis; nails are of normal configuration. Clubbing of distal phalanx occurs with COPD because of growth of vascular connective tissue. Cutaneous angiomas (spider nevi) associated with liver disease or portal hypertension may be evident on the chest. o Respirations- Noisy breathing occurs with severe asthma or chronic bronchitis. Unequal chest expansion occurs when part of the lung is obstructed (pneumonia) or collapsed or when guarding to avoid postoperative or pleurisy pain. Retraction suggests obstruction of respiratory tract or that increased inspiratory effort is needed, as with atelectasis. Bulging indicates trapped air as in the forced expiration associated with emphysema or asthma. Accessory muscles are used in acute airway obstruction and massive atelectasis. Rectus abdominis and internal intercostal muscles are used to force expiration in COPD. Tachypnea and hyperventilation, bradypnea and hypoventilation, periodic breathing o Symmetrical chest expansion. Abnormally wide costal angle with little inspiratory variation occurs with emphysema. Assess tactile fremitus. Palpate chest wall. Percuss- Lungs are hyperinflated with chronic emphysema, which results in hyperresonance where you would expect cardiac dullness. Dullness behind the right breast occurs with right middle lobe pneumonia. Pulmonary function o The forced expiratory time is the number of seconds it takes for the person to exhale from total lung capacity to residual volume. It is a screening measure of airflow obstruction. A forced expiration of 6 seconds or more occurs with obstructive lung disease. Refer this person for more precise pulmonary function studies. Spirometer & pulse oximeter & 6-min walk test (is a safer, simple, inexpensive, clinical measure of functional status in aging adults) 2. Identify appropriate respiratory assessment techniques for clients based on age, development, and other psychosocial or environmental variables. The Aging Adult: The costal cartilages become calcified; thus the thorax is less mobile. Respiratory muscle strength declines after age 50 years and continues to decrease into the 70s. A more significant change is the decrease in elastic properties within the lungs, EXAM 3_316 making them less distensible and lessening their tendency to collapse and recoil. In all, the aging lung is a more rigid structure that is harder to inflate. These changes result in an increase in small airway closure, which yields a decreased vital capacity (the maximum amount of air that a person can expel from the lungs after first filling the lungs to maximum) and an increased residual volume (the amount of air remaining in the lungs even after the most forceful expiration). With aging, histologic changes (i.e., a gradual loss of intra-alveolar septa and a decreased number of alveoli) also occur; therefore less surface area is available for gas exchange. In addition, the lung bases become less ventilated as a result of closing off of a number of airways. This increases the older person's risk for dyspnea with exertion beyond his or her usual workload. The histologic changes also increase the older person's risk for postoperative pulmonary complications. He or she has a greater risk for postoperative atelectasis and infection from a decreased ability to cough, a loss of protective airway reflexes, and increased secretions. The chest cage commonly shows an increased AP diameter, giving a round barrel shape and kyphosis or an outward curvature of the thoracic spine. The person compensates by holding the head extended and tilted back. You may palpate marked bony prominences because of decreased subcutaneous fat. Chest expansion may be somewhat decreased with the older person, although it still should be symmetric. The costal cartilages become calcified with aging, resulting in a less mobile thorax. The older person may tire easily, especially during auscultation when deep mouth breathing is required. Take care that this person does not hyperventilate and become dizzy. Allow brief rest periods or quiet breathing. If the person does feel faint, holding the breath for a few seconds restores equilibrium. Ill patient: Use of a second examiner to assist the patient in terms of positional changes. If no one is available, examiner may roll patient from side to side to facilitate change of position. If rolling technique is used, this may interfere with bilateral assessments of inspection and percussion. 3. Differentiate between normal and abnormal respiratory assessment findings that require further evaluation. Thorax abnormals o Barrel chest- Note equal AP-to-transverse diameter and that ribs are horizontal instead of the normal downward slope. This is associated with normal aging and also with chronic emphysema and asthma as a result of hyperinflation of lungs. o Pectus excavatum- caved in chest o Pectus carinatum- sternum goes out o Scoliosis- A lateral S-shaped curvature of the thoracic and lumbar spine, usually with involved vertebrae rotation. Note unequal shoulder and scapular height and unequal hip levels, rib interspaces flared on convex side o Kyphosis- An exaggerated posterior curvature of the thoracic spine (humpback) that causes significant back pain and limited mobility. Severe deformities impair cardiopulmonary function Respiratory patterns o Sigh- Occasional sighs punctuate the normal breathing pattern and are purposeful to expand alveoli. Frequent sighs may indicate emotional dysfunction and also may lead to hyperventilation and dizziness. EXAM 3_316 Tachypnea- Rapid, shallow breathing. Increased rate, >24 per minute. This is a normal response to fever, fear, or exercise. Rate also increases with respiratory insufficiency, pneumonia, alkalosis, pleurisy, and lesions in the pons. o Bradypnea- Slow breathing. A decreased but regular rate (<10 per minute), as in drug-induced depression of the respiratory center in the medulla, increased intracranial pressure, and diabetic coma. o Hyperventilation- Increase in both rate and depth. Normally occurs with extreme exertion, fear, or anxiety. Hyperventilation blows off CO2, causing a decreased level in the blood (alkalosis). o Hypoventilation- An irregular shallow pattern caused by an overdose of narcotics or anesthetics. May also occur with prolonged bed rest or conscious splinting of the chest to avoid respiratory pain. o Cheyne-Stokes respiration- tachypnea and then long periods of rest (that get longer), happens at the end of life usually; A cycle in which respirations gradually wax and wane in a regular pattern, increasing in rate and depth and then decreasing. The breathing periods last 30 to 45 seconds, with periods of apnea (20 seconds) alternating the cycle. The most common cause is severe heart failure; other causes are renal failure, meningitis, drug overdose, and increased intracranial pressure. Occurs normally in infants and aging persons during sleep. o Biot’s respiration- groups; Similar to Cheyne-Stokes respiration, except that the pattern is irregular. A series of normal respirations (three to four) is followed by a period of apnea. The cycle length is variable, lasting anywhere from 10 seconds to 1 minute. Seen with head trauma, brain abscess, heat stroke, spinal meningitis, and encephalitis. o Chronic obstructive breathing- taught pursed lip breathing, CO2 retention usually; Normal inspiration and prolonged expiration to overcome increased airway resistance. In a person with chronic obstructive lung disease, any situation calling for increased heart rate (exercise) may lead to dyspneic episode (air trapping) because the person does not have enough time for full expiration. 4. Document health history and key components of a respiratory assessment in the client record. o Sample Charting Subjective o Objective o o o o No cough, shortness of breath, or chest pain with breathing. No history of respiratory diseases. Has “one or no” colds per year. Has never smoked. Works in well-ventilated o;ce on a smoke-free campus. Last TB skin test 4 years PTA, negative. Never had chest x-ray. Inspection: AP < transverse diameter. Resp 16/min, relaxed and even. Palpation: Chest expansion symmetric. Tactile fremitus equal bilaterally. No tenderness to palpation. No lumps or lesions. Percussion: Resonant to percussion over lung fields. Diaphragmatic excursion 5 cm and = bilaterally. Auscultation: Vesicular breath sounds clear over lung fields and = bilaterally. No adventitious sounds. Assessment o o Intact thoracic structures Lung sounds clear and equal EXAM 3_316 Discontinuous sounds: Continuous sounds: Crackles—fine Wheeze—sibilant: high pitched Crackles—course Wheeze—sonorous rhonchi: lower pitched Atelectatic crackles- clear after cough Stridor- upper airway obstruction Pleural friction rub