Pediatric Nursing Exam 3 Study Guide
advertisement
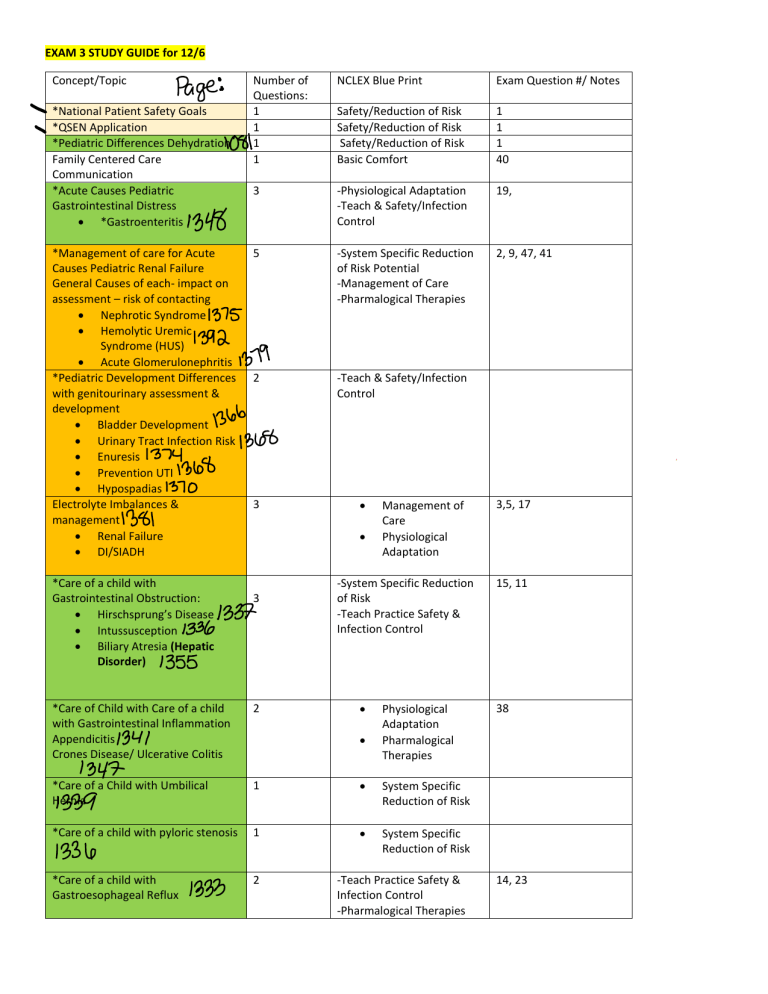
EXAM 3 STUDY GUIDE for 12/6 Concept/Topic *National Patient Safety Goals *QSEN Application *Pediatric Differences Dehydration Family Centered Care Communication *Acute Causes Pediatric Gastrointestinal Distress *Gastroenteritis *Management of care for Acute Causes Pediatric Renal Failure General Causes of each- impact on assessment – risk of contacting Nephrotic Syndrome Hemolytic Uremic Syndrome (HUS) Acute Glomerulonephritis *Pediatric Development Differences with genitourinary assessment & development Bladder Development Urinary Tract Infection Risk Enuresis Prevention UTI Hypospadias Electrolyte Imbalances & management Renal Failure DI/SIADH *Care of a child with Gastrointestinal Obstruction: Hirschsprung’s Disease Intussusception Biliary Atresia (Hepatic Disorder) Number of Questions: 1 1 1 1 NCLEX Blue Print Exam Question #/ Notes Safety/Reduction of Risk Safety/Reduction of Risk Safety/Reduction of Risk Basic Comfort 1 1 1 40 3 -Physiological Adaptation -Teach & Safety/Infection Control 19, 5 -System Specific Reduction of Risk Potential -Management of Care -Pharmalogical Therapies 2, 9, 47, 41 2 -Teach & Safety/Infection Control 3 3 Management of Care Physiological Adaptation -System Specific Reduction of Risk -Teach Practice Safety & Infection Control *Care of Child with Care of a child with Gastrointestinal Inflammation Appendicitis Crones Disease/ Ulcerative Colitis 2 *Care of a Child with Umbilical Hernia 1 System Specific Reduction of Risk *Care of a child with pyloric stenosis 1 System Specific Reduction of Risk *Care of a child with Gastroesophageal Reflux 2 Physiological Adaptation Pharmalogical Therapies -Teach Practice Safety & Infection Control -Pharmalogical Therapies 3,5, 17 15, 11 38 14, 23 *Liver failure, Blood products when to administer them, interpret labs, parent teaching, splenectomy 5 Bleeding Disorder Hemophilia Disseminated intravascular coagulation (DIC) Anemia Thalassemia Management of Care Physiological Adaptation Teach Practice Safety & Infection Control System Specific and Reduction of Risk 4,7,25, 29 , 32,44, 43 *Risk for Neurological Injury Differences Pediatric & Adult patients *Neurological Assessment Pediatric Patient Pupils Central Nervous System Checks Glasgow Coma Scale Posturing *Increased Cranial Pressure Pediatric Differences Signs/symptoms Management 1 -Teaching & Safety 37 3 -Physiological Adaptation 13, 30 3 -Safety/Reduction of Risk -Evaluate Pharmalogical Therapies 6, 16,36 *Management of Child with Meningitis *Management of Pediatric Patient with Renal Failure 1 -System Specific Reduction of Risk -Management of Care -Basic Comfort Care -Health Promotion -Evaluate Pharmalogical Therapies 42 *Care of Child with Cleft Lip Repair 2 35, 28 *Care of Child with Trans Esophageal Atresia 1 -Physiological Adaptation -Teach & Practice Safety Physiological Adaptation *Care of a Pediatric Client in Sickle Cell Crisis 2 -Management of Care -Pharmalogical Therapies 33, 18 *Care of Pediatric Patient with Seizures 3 2 Physiological Adaptation Pharmalogical Therapies Teach & Practice Safety *Care of a Child with Cerebral Palsy 1 Pharmalogical Therapies *Care of child neural tube defect 1 -System Specific Reduction of Risk 20, 49 8, 27, 31 2 Bladder Development Differences with genitourinary assessment GU Assessment: Urinary Tract Infection Risk vary by age (Pyelonephritis is upper UTI) & (Cystitis=Lower UTI) A. Urinary stasis enhances risk of UTI. Stasis may be caused by neurogenic bladder or abnormal function. UTI treatment: Need to know what organism to prescribe the right antibiotics. Do sterile procedure such as clean catch. Give antibiotics after culture received. Prevention of UTI to Teach: Female to wipe front to back, teach sexual activity void afterwards, don’t hold urine, hydration, avoid bubble baths/hottub, potty breaks, don’t wear tight underwear. ALL antibiotic must be finished. Antibiotics for UTI: <2 years of age prescribed Bactrim, Trimethoprim. This med prevents reoccurring UTI. Cephalosporins: Ceftriaxone, cephalexin, cefepime. LAB: Urinalysis, urine culture, VCUG Manifestations of UTI: Infants: Fever, irritability, poor appetite, low weight, smelly urine Preschooler: Fever, enuresis, regression of toileting, urgency, dysuria (pain when peeing). School age: hold bladder because it hurts, Fever, they can verbalize pain. Nursing Management for Hypospadias recommend 6-12m: B. Males Structural Defects Like: Assessment: Assess urethra & Pull foreskin back. Also look for inguinal hernias and cryptorchidism→ one or no testes descending) Postop: protect surgical site → penis wrapped in simple dressing & urethral stent or catheter for drainage. Urine will have blood tingle for several days. -Don’t bathe with stent -Encourage intake and Strict I & O -Double diaper to protect operative site -Apply KY jelly to prevent skin from sticking on diaper -Restrict infant from applying pressure to site -Call doctor if urine leaks any other area than penis OR one void returning from surgery. Meds: oxybutynin to manage bladder spasms but treat its constipation Enuresis: Bedwetting, loss of bladder control. By 5yrs of age it should be controlled. Enuresis relating to UTI→ Primary enu: child never had a dry night because of maturational delay. Secondary enu: Child is dry for 6months then begins to bed wet due to stress, infections, disorders. Assessment: Assess abdomen for distension. Family history intake, Any potential causes such as DM, DI, UTI, Constipation. Management of care for Acute Causes Pediatric Renal Failure General Causes of each- impact on assessment – risk of contacting System Specific Reduction of Risk Potential- Management of Care -Pharmalogical Therapies Acute Glomerulonephritis: Body’s Immune response to bacteria creates antigen-antibody which causes inflammation of the glomerulus within the nephron in kidneys: leaks RBC & mild protein. Symptoms are: ↓ GFR of toxins out of blood, ↓regulation of fluid and electrolytes, and poor regulation of acid-base balance. Causes: Streptococcal infection of skin or pharynx. affects boys 2-6yrs. Impetigo (skin infection) patients are at risk. Treatment: Antibiotics, check trough levels. Assessment finding: Fever Cloudy urine (pyuria), Anorexia, N/V, Malaise, HTN due to water retention Hematuria - RBC in urine, ↓urine(watch K) , mild Proteinuria. ↑ BUN & Cr. Swollen face during morning. Tea-colored urine. ATTENSION REQUIRED sign of encephalopathy: headache & photophobia Nursing interventions: Vital signs (close assessment BP risk for HTN) treat with ACE inhibitors I/O closely , daily weights Assess for dehydration if restricting fluid Diet- low NA & low protein Assess UA for any infection Modify activity to allow for rest Electrolytes monitor: ↑K, ↓ca, ↓ Na NephrOtic Syndrome Changes to the glomeruli. No blood in urine, but Kidney can’t hold albumin/prOtein so, massive loss of it leaks into urine and liver makes more lipids. ↓ oncotic pressure within blood vessel causing fluid shifts like peripheral edema. Clinical manifestations: Proteinuria, Ascites, edema, wt gain, HTN, urine contains foamy/frothy, Hypoalbuminemia. Bad cold. Interventions: Prevent infection. I/O. Assess urine for protein. Abd girth & weights. Prevent infection. Diet, low NA. Support -Assess for blot clots. Turn q 2hrs. Medications: Corticosteroids: (To ↓ excretion of albumin/ protein & inflammation) -prednisone →IV is Methprednisolone. Side effects are HTN, cushion disease, ↑appetite, wt. gain, immunosuppressant, steroids need to be weaned and not abrupted, avoid immunizations. -1. Albumin: helps return the fluid to the bloodstream from the subcutaneous tissue. H20+Albunin will ↓edema -2. Diuretics: Lasix to get rid of fluid. This will also improve sodium levels. (↓ fluid retention) Hemolytic Uremic Syndrome (HUS) An acute renal failure. Caused by E. Coli, this produces a toxin that attaches to glomeruli and cause arterioles to swell and become occluded with Fibrin and platelet causing clots. RBC’s become damaged while traveling through narrow vessel. This results in Anemia. Spleen removes these and liver can enlarge over time. S/S: V/D. Hematuria. LABS: Mild proteinuria, ↑BUN&CR. ↑Reticulocyte ct. Assessment: hematuria Fluid overload, Anemia , Thrombocytopenia, Arrhythmias Pale, easy bruising, Nursing interventions: o o o o o Dialysis Assess electrolytes give replacement Assess Respiratory-s/s: fluid overload Assess neuro affects CNS, have hypoxic events AVOID antibiotics because they increase risk of HUS. Management of Pediatric Patient with Renal Failure Acute Kidney Failure: Days→ weeks→ Reversible Sudden loss of kidney function. Unable to regulate volume and composition of urine (fluid balances & electrolytes) ↓renal blood flow leading ↑BUN Hypovolemia common cause of ARF from dehydration: treat with fluids. Chronic Kidney failure: Month→ Years→ Permanent damage Permanent damage to kidneys characterized by Significant ↓ GFR <60ml/min resulting in accumulation of metabolic waste product in blood. Interventions: Trend Labs: CA, K, P, Na Monitor EKG→ Hyperkalemia causes peak T waves Fluid Status Diuretics for HTN or antihypertensive Diet Education LABS: Creatinine level(↑), creatinine clearance, GFR(↓), BUN(↑) Creatinine level is 0.5-1.20mg/dl Interventions: Monitor I &O & Daily Weight Vital signs→ hypertension Assess fluid overload→ listen to lungs Trend labs→ Na, K, Ca Administer HTN medications and diuretics as needed Assess for infection i. Avoid aminoglycosides like gentamycin, vancomycin Assess neurological changes→ electro abnormalities CRRT/Dialysis support as needed Low protein preserves renal function ↓BUN Food Low, NA, K Growth Failure risk, hormones will be ordered Assess neurological status because of Na Assess for s/s anemia→ Child doesn’t produce epoetin Assess for infections careful administration of antibiotics. Gentamycin, vanco. Continuation of Chronic Kidney failure(End stage renal disease) Dialysis→ Ped difference→ are sensitive to fluid shifts -They Don’t tolerate volume &Electrolyte disturbances (RISK) Transplant: Rejection and Infection Risk Balance managing immunosuppression ↑ if sign of rejection but now ↑ for infection S/S of rejection to teach parents? Rejection, fever, malaise, decreased urine output, tachycardia, tachypnea, weight gain, poor appetite REJECTION most common cause transplant failure. Questions: What are their v/s? Wt before & after? What is the goal fluid removed? Dry wt?→ Body wt at the end of dialysis at which the patient can remain normotensive until the next dialysis. PREVENT→ A central line-associated bloodstream infection (CLABSI) by: 15sec scrub, sterile drape, mask both, sterile technique. Peritoneal Dialysis (removes at a slower rate) Hemodialysis CRRT Similar to hemodialysis EXCEPT it is done continuously in ICU for pt who don’t tolerate large volumes of Child comes to hospital 3x/wk 4-6hrs fluid removal. Achieves rapid correction of F& E Important to know how much fluid goes in/out abnormalities but Can be done at home requires close Elevate HOB to ↓ pressure from Dialysate on the monitor. diaphragm Disequilibrium Provide small meals & administer through TF. syndrome can occur ↑glucose concentration dialysate if edema & Complication: Hypotension, hypertensive present infection, shock Complications: -Peritonitis→ tenderness, cloudy dialysate, fever→ Place antibiotic in dialysis fluid. Side note: Diabetes Insipidus: Dry, Low specific gravity, urinate a lot, treat with vasopressin. SIADH: A lot of fluid, gain wt because they have too much anti diuretic hormone. Fluid overload→ Fluid restrictions. Wilms tumor AKA nephroblastoma→ Malignant tumor usually presented as a solid mass in the abd. S/s? Firm mass on 1 side of abd→ STOP PALPATING CALL HCP. Pallor, Wt loss. Fever. N/V. Hematuria. BP change. Nursing care? How is treated? Surgical removal & Chemo. Pain Management→ Morphine, Hydrocodone Fluid balance-strict I/O, daily weight Frequent Vital signs Trending Labs→ Hematocrit, WBC, electrolytes Infection Control Zofran/ Benadryl, ONDANSTETRON to manage N/V Doxorubicin-results heart complication. Need echo or EKG before starting. Watch for cardiac output. Vincristine-results tumor lysis syndrome. Watch for peripheral neuropathy Cyclophosphamide-Watch for hemorrhagic cystitis. (Bleeding of bladder ) Pediatric Differences in GI Infants do not have voluntary control over swallowing until about 6 weeks of age and this puts them at risk for aspiration. Newborn stomach holds 90ml’s. That’s why we feed small amounts. About 1yr of age capacity is 360ml. 3yr old has 5fl.oz That’s why we teach parents about feeding. insufficient enzymes such as lipase, amylase which leads to gas so bring knees to chest. Simethicone. Glucogenesis is immature –risk hypoglycemia low sugar By 18 months, child has control over excretory functions (pooping) GI nursing assessment Family history: How is the child’s intake? What is their output like? How many wet diapers/urine output? What are stools like? Frequency, consistency, color? Any hx of disease? Any Nausea? Vomiting-color & consistency, bile? Spitting up, reflux, burning in throat? Chest pain? Remember that GI dysfunction leads to electrolyte imbalances and impact nutrition because of malabsorption. GI dysfunction: Constipation: decreased in passing stool. #1 cause of abdominal pain in children. Educate on high fiber rich foods. Minimize dairy products. Cause: diet, activity, poor fluid intake, disease, psychologic. GI Dysfunction: Gastroenteritis(acute diarrhea) inflammation of the stomach/ intestines that is accompanied by V/D. Affects any part in GI tract. Common cause is Rotavirus (cause loose watery stools) C.Diff, E.coli. Child can become quickly dehydrated and at risk of hypovolemic shock if fluid not replaced. Encourage parent to get rotavirus vaccine. Symptoms: Abdominal distention. Pain. Cramping. N/V Anorexia. Watery stools Dehydration fever Nursing interventions: Fluid/electrolytes→ Get specific gravity to look at dehydration, BUN, Cr. Infection Control→ Handwashing, contact isolation, monitor stools, collect stool sample. Fluid volume deficit→ Body weight in baby’s is high percent of water. Monitor for dehydration. I &O, assess skin turgor, provide fluids. Weight the child for accurate fluid balance. Also, postop tonsillectomy clients are at risk for dehydration because of not being able to swallow. Dehydration Not enough fluid in the extracellular compartment (vascular + interstitial). Cause: fever, ↓fluid intake, burns, diabetes, V/D. Late signs: Hypotension, tachycardia, tachypnea, cyanosis Teach/Interventions: Keep track of wet diapers any loose stool and vomiting. Replace loss fluids w/ 60-120ml if <10kg.>10kg replace w/ 120140ml. 3-5ml q 5min Avoid high sugars like juice because it ↑ gas & diarrhea Bone fractures makes child not drink fluids. Oral fluid replacement for mild to moderate Electrolyte drink (Pedialyte, Gatorade) Obtain urine for specific gravity testing Ex; A child is being treated for dehydration with intravenous fluids. The child currently weighs 13 kg and is estimated to have lost 7% of his normal body weight. The nurse is double checking the IV rate the healthcare provider prescribed. The formula the healthcare provider used was for maintenance fluids: 1000 mL for 10 kg of body weight plus 50 mL for every kilogram over 10 for 24 hours. Replacement fluid is the percentage of lost body weight × 10 per kg of body weight. According to the calculation for maintenance plus replacement fluid, which hourly IV rate will the nurse implement for 24 hours? 86 mL/hr Care of a child with Gastrointestinal Obstruction: Hirschsprung’s Disease congenital absence of ganglion cells in the walls of the large intestine and anus. This leads to decrease motility of peristalsis and leads to obstruction of bowel. What does that look like? N/V. At risk to decrease perfusion to that organ. ↓ blood supply. Tissue necrosis. Lactic acid turning patient to acidotic state. Infection occurring into septic shock. Major complication is: Perforation. →s/s: ↑temp, pain, hypovolemia, Clinical manifestations: Enterocolitis (Inflammation of intestine) , constipation, bloody diarrhea, abd pain, fever. n/v. -In newborns s/s→ After birth, No meconium 24-48hrs. Abd distension. -Older child s/s→ History of chronic constipation. FTT No wt gain, malnutrition, pencil thin stool. TX: Surgical removal aganglionic bowel section. Ask how much of the bowel they removed? Less surface area in the bowel the more likely for malnutrition because nutrients aren’t being absorbed= loose watery stools. A colostomy is created afterwards, then they come back later date to do a pull through and reconnect to anus. Pre op: For an 8yr old, let child see pics, hold a ostomy bag put on skin/bear.Educate fam on stoma. Output of ostomy. Trends. Use skin prep and use a template to cut out in ostomies. DO NOT USE ADHESIVE ENHANCER ON NEONATE. Skin is FRAGILE. Contains latex. Post op: Encourage deep breathing, perfusion, BP, I&O, Electrolyte imbalances, monitor for infection. Daily wt. Watch for bowel function. Intussusception AKA telescoping When one portion of the intestine prolapses into another intestine. MEDICAL EMERGENCY!→obstructed blood flow, necrosis, hemorrhage. LIFE THREATING, lactic acid buildup, sepsis. S/S: Sharp pain, Currant-jelly bloody stools. Vomiting. TX: Barium enema or air to unfold back out of intestine. Nursing care: Assess s/s perforation, NG decompression, hydration, vitals, pain, progression to regular diet, stool assessment Biliary Atresia-closure or absence of bile duct. Cholestasis→ disruption of bile flow to duodenum. Dx: liver bx, labs, H&P TX: Kasai procedure (palliative) & Liver transplant Necrotizing enterocolitis (NEC) serious illness in newborns. It happens when tissue in the large (colon) gets inflamed. This inflammation/infection damages and kills some tissue in your baby’s colon. Side note: When every there’s a bowel section removed, they will be in PN. Nsg: Support: Show them supplies, BP checks on doll Nutrition: Maximize nutrition→ Oral during day and at night TPN. Meds: Actigall→ promotes bile flow. A, D, K vitamins help w/ absorption. -surgery teaching and d/c teaching Liver failure: r/t Tylenol ingestion. Another cause of liver failure is Hepatitis. S/S: Bruising r/t ↓ platelet productions, ascites r/t to albumin not being synthesized. Jaundice r/t liver not removing bilirubin. #1 Encephalopathy r/t ammonia levels not being excreted→ alters LOC & alters Blood brain barrier→ CueC: ICP→ Give mannitol. Lactulose is given to ↓ ammonia levels. #2 CueC: Hemorrhage. So liver synthesizes clotting factors, Vit K, platelets. If liver don’t synthesize expect LABS: ↑PTT/INR. To replace clotting factors Give fresh frozen plasma! Process of administration Blood product: 1.) Crossmatching, double check, patient identity at bed side. You have 4hrs once you spike. Any allergies, 2-person check. Check bag: lot, discoloration, expiration date& time, appropriate volume and rate. Compatible only with NS. Observation’s 1st half hr. Monitor for any reaction→ stop blood flush line. Allergic reaction→ Benadryl. If Anaphylactic reaction→ IM EPI. Care of a child with Gastroesophageal Reflux aka Acid reflex the return of gastric contents back up through the esophageal sphincter. Peds have short narrow esophagus small stomach that increases the risk of aspiration. Clinical manifestation: Spitting up, vomiting, arching while feeding, poor growth, fussy baby. Sinus infections. Desaturation when feeding. Older children: chest pain, abd pain, burn in the throat. DX: History, esophageal ph probe, Allergy testing due to formula they might be taking, moms diet cut on LACTOSE. Endoscopy. TX: depends on severity. Also, feeding modification. MILD Wedge(Places child in high position) , 30 minutes positioned upright afterwards avoid carseats , thickened feeds, small/freq feeds, meds (h2 and PPIs SEE BELOW, some reglan to ↑ GI motility), frequent burbing. SEVERE -Surgery (fundoplication) to prevent formula from going up -Tube feeds for FTT (NG vs NJ tube?) Care of Child with Care of a child with Gastrointestinal Inflammation Appendicitis AKA McBurney’s point Inflammation of the vermiform appendix, near the end of the cecum RLQ. If inflamed become painful, burst and causes sepsis/ peritonitis. Average age 10-19yrs. Clinical manifestations: N/V (bile), Pain, Fever, Child not willing to play, not willing to jump, Diaphoretic, ill appearing. Dehydrated. Diagnosis: Take history and vital signs ↑HR, ↑RR. Abd pain. Physical assessment. Labs: CBC, CMP, CRP→ looks for inflammation, urinalysis Treatment: NPO, Pre-op: expect IVF, Pain medications, freq assessment and vitals. Perforated→ laparoscopy vs open appendectomy→ Not perforated Post op: Respiratory→ Hypoxemia, GI function to return, infection give antibiotics. Watch for inadequate nutrition. Use a splint pillow and place on the abdomen when coughing to decrease discomfort. Ulcerative Colitis (inflammation & sores) Inflammation of mucosa only( large intestine) & rectal S/S: 1# Diarrhea, abdominal pain, cramping LQ, bloody stools While resting the bowel, give IVMF. ↑WBC count due to inflammation Crohn’s Disease (inflammation) Chronic, inflammatory process involving mucosa and submucosa. Occurs randomly in GI tract Fistulas and ulcers common S/S: Anal lesions, anorexia, growth grid, pain, wt loss. While resting the bowel, give parental nutrition→ risk for hyperglycemia. Apply central line. Also decompress stomach to low intermit. Small frequent meals, decrease fiber intake, High calorie supplements Dx: labs Hematocrit & hemoglobin because of bleeding, Electrolyte imbalances, Endoscopy, colonoscopy Tx: bowel rest, medication to ↓ inflammatory, maximize nutrition, surgery correction. Nsg care: support, nutrition, rest, comfort/pain. Cluster care. Small frequent meals. Make a dairy to keep track. MEDS: Control inflammation. Example: Corticosteroids such as prednisone help suppress inflammatory response. Long term effects? Immunosuppressants. Need to be tapered steroids can’t be stop abrupted.. First line of treatment. Decrease inflammation of intestine Example: Aminosalicylates→ decrease inflammation of intestine Help decrease T cells that contribute to inflammatory response. Example: Immunosuppression such as methotrexate, cyclosporine, mycophenolate. Risk?→ Immunosuppressants, sepsis. Wash hands. Vaccines up to date. Decreases active inflammation: Biological Therapies -Tumor Necrosis factor medications such as Remicade. Side effects? ↓immune system increase infection. Supplements: Vitamins, Zinc, Folic Acid Meckel Diverticulum Small pouch on the intestine wall located on the intestine. Pouch can rupture and causing irritation & ulceration. Assess: ↓BP, fever, hypoactive BT. Labs: H&H, CBC, CRP. Postop: clear diet, resp function, GI function return. Assess BT. Care of Child with Cleft Lip Repair Cleft palate small or large fissure in facial process from lip up to nasal septum. Failure of the maxillary process to fuse. 6-18months repaired. Occurs during 1st trimester. Factors caused: Genetic, smoking, glucocorticoid use(prednisone), Folate Pre op: Complications: -Aspiration: Use a nipple elongated hole, OT therapy to access swallow, hold baby up not in car seat positioned. Ris for hearing/ speech. -Parental support: Encourage family to breast feed, hold and interact w/ infant. Have normal milestones. Post op: Do respiratory assessment, can they handle secretions? , Ped assessment→ guard the suture line. (any inflammation), Pain management. Need to be placed in an immobilizer and turned q 2hrs. Nutrition: maintain IV fluids until NPO is done Use syringe or doppler for oral intake. No prone positioning only supine. NO rough foods. No straws. NO PACIFER or sucking. No suction. Care of Child with Trans Esophageal Atresia Physiological Adaptation Tracheoesophageal Fistula Failure for the esophagus to do a continuous passage and rather connects to trachea. Increasing risk for aspiration, pneumonia, nutrition. S/S: Choking, cyanosis, coughing. Excessive saliva. DX: Ultrasound, X-ray Surgical Repair: - Ligation of fistula ( goal is to reconnect structures) - Gastrostomy (feeding tube until reconnection is done) Preop- continual suction of esophagus, NPO, IVF, I&O, ↑HOB 30 degrees Post-op: GTube edu, IVF/PN until gastrostomy or oral tolerated, antibiotics, care site. Can use a pacifier during feedings it is important to use oral stimulation even if food is through GTube. Lipids. Care of a child with pyloric stenosis Hypertrophic Pyloric Stenosis S/S: Projectile vomiting occurs 30mins after a feed. Wt loss. DX: Olive size mass in epigastrium. TX: pyloromyotomy. Pre op: Gastric decompression if feeding not tolerated. Post op: Feed very slow progression. Same stuff for GI surgery. Care of a Child with Umbilical Hernia Umbilical Hernia Intestines protrude through the umbilical area causing reduction in blood flow to area. Low birth weight. Notice at 6 months of age. Resolves on its own. However, the piece of bowel twisting and doesn’t go back in then we worry about necrosis & perforation. S/S: Abd distension, vomiting. DX: X-ray, CT, Ultrasound TX: Bulge may be decreased with manual pressure watch until 1yr of age. (this changes abd pressure.) Another hernia is Omphalocele Intra-abdominal contents herniate through umbilical cord has peritoneal layer (intestines, liver) Place in radiant warmer Anemia disorders Sickle Cell Disease autosomal recessive disorder(both parents) hereditary form of anemia. Abnormal hemoglobin “S” on RBC. It’s very sensitive to low O2. (Hypoxia). Spleen 1st organ affected Normal→ Hemoglobin “A”. Sickle cell crisis occurs when sickle-shaped red blood cells clump together and block small blood vessels that carry blood to certain organs. So, anything that requires more o2 like #1 hypoxia, altitude, infections, #2dehydration, infection, #3hypothermia will cause these RBC “S” to become elongated crescent sickle shaped, stiff and sticky causing obstruction capillary blood flow. Nursing Interventions/Meds: 1. Prevent sickling→ hydration, Avoid activities, (high altitude), Maintain oxygenation, Consider Hydroxyurea decreases sickling by increasing fetal hemoglobin 2. Prevent Infection→ Freq neuro assessment, Assess s/s infection, Immunizations (flu shot), Oral prophylaxis by 2 months of age, any fever, CBC, cultures, avoid sick people 3. Manage pain→ Bedrest to decrease body’s demands, apply heat to promote vasodilation, PCA –Morphine/ hydromorphone (Dilaudid), Scheduled NSAIDS –ketorolac (Toradol) IV or Ibuprofen (PO) for fever, Fluids, Methylprednisolone to ↓inflammation ↑Possible Splenectomy?? Assess for infection. Breathe deep frequently to avoid atelectasis. _______________________________________________________________________________ Aplastic Anemia: is caused the bone marrow producing inadequate cells.” S/S: Fatigue and fever. Beta Thalassemia: blood disorder that reduces production of hemoglobin and lack of oxygen in the body. Three types: -Thalassemia minor/ Thalassemia trait—mild anemia, may not be present. -Thalassemia intermediate—moderate to severe anemia plus splenomegaly -Thalassemia major— “Cooley’s anemia”—severe anemia requiring transfusions to survive S/S: by 6M severe anemia, Pallor, tachycardia, hypoxemia, FTT, jaundice(later) r/t liver Dx: Hgb electrophoresis→ reveals ↓production of 1 globin chain Nursing Care: 1.) Hgb levels sufficiency to promote G&D & minimize bone marrow production because it leads to deformity’s 2.) prevent complications of frequent blood transfusions because they have a lot of iron in them. Excessive iron can lead to enlarged liver & HF. Thing to eliminate excess iron is Chelation therapy. → Deferoxamine (Desferal)(IV)to prevent iron overload or Deferasiorax (Exjade)(PO) help more compliance therapy 3.) blood transfusion Common Type of reaction and S/S of blood transfusion Bleeding Disorder Hemophilia: A group of hereditary bleeding disorders caused by a lack of specific clotting factors in the blood. X linked recessive trait. S/S: Mobility(cuts, falls, head trauma), Limited ROM, Pain ,swelling , Internal (blood in urine). Easy bruising, pallor. Advise to wear protective gear for sports. Labs: low levels of factor VIII or IX, prolonged PTT, Normal platelet count, PT, and fibrinogen Nursing interventions: 1. Assess for bleeding & apply pressure to area. 2. Replace missing clotting factors→ fresh frozen plasma or DDAVP or desmopressin via IV, Causes 2 to 4 times’ increase in factor VIII activity 3. [Transfusions as needed (pack RBC’S)→cross match with 2nd RN. watch 1st 20ml, give slow, at risk for circulatory overload, s/s of any reaction. Can use NS. ] Shave only w/ electric razor, ROM after bleeding stops to prevent contractures. Avoid injections. Common DX: Risk for Impaired Physical Mobility related to joint stiffness and contractures Disseminated intravascular coagulation (DIC) Life threating in which the clotting cascade (thrombin+fibrin) is abnormally activated resulting in widespread clot formation in small vessels throughout the body. Common cause: Sepsis, Hypoxia, shock. Emboli, toxins. Risk for bleeding& hemorrhage if left untreated. →Replace w/ RBC’s. Heparin provides immediate anticoagulation when thrombosis occurs. S/S: oozing from IV sites, tachycardia, hypotension (late), prolonged bleeding times, blood in urine/BM Labs: PT →Prolonged→ tx: Fresh frozen plasma. PTT →Prolonged→ tx: Fresh frozen plasma. Fibrinogen→ Low→ tx: Fibrinogen Platelets→ Low→ tx: Platelets D Dimer: ↑ measures? Looks at remains of a clot. DIC status Nursing interventions: / Blood product 1. Treat the underlining problem causing inflammatory process 2. Replace clotting factors→ fresh frozen plasma has clotting factors. Replace platelets as well→ Blood platelet. Fibrinogen→ Fibrinogen blood. If you need blood product that will impact H&H give→ red blood cells. 3. multisystem disorder so maximizes tissue perfusion→ give O2 and monitor V/S 4. Treat the underlying cause first. 5. Avoid injections, assess for bleeding & shock. Infectious Diseases Like Meningitis: inflammation of the meninges in the brain can be caused by either bacterial or vial agents. Bacterial Meningitis Viral (Aseptic) Meningitis Acute inflammation of the meninges Inflammatory of the meninges caused by surrounding CNS (brain/spinal cord). enteroviruses. ↑Protein levels. ↓Glucose levels. Impaired No isolation required gas exchange. S/S: headache, fever, malaise, maculopapular Hib vaccine given at 2M. rash. LP reveals ↑WBC, ↑protein, normal glucose Nursing interventions: Caused by Strep (pneumococcal), E. cluster care, dark room, ↓inflammation, (meds), coli, TB, Neisseria meningitides fluids, PN, alert for nuero changes & ICP (Meningococcal) present with a purpuric petechial rash that progress into septic shock! Assessment S/S: Neck stiff, Purpuric & Petechial rash→ Risk hypovolemic shock, Headache, Light sensitive, Risk for SIADH (Too much ADA so not voiding enough = decrease UOutP)causing hyponatremia, Kerning (flex knee and extend if pain or resistance then +), +Brudzinski (head and knees flexed), Seizures→ maintain airway -Basilar skull fracture (raccoon eyes) Nursing interventions: Neuro assessment Comfort for pain HA, N/V, fever Vaccines→ HIB, Pneum.., Mening… Antibiotics for infection-isolation for 24h/ Observe client for shiver Droplet Isolation Care of child neural tube defect: (Spina Bifida) Neural tissue containing brain & spinal that protrudes along the lumbar or sacral on the spine. Myelomeningocele is a neural tube defect in which the meninges and spinal cord are exposed. folic acid is important during pregnancy to prevent neural tube defects Chorionic villus sampling(CVS) is used 1st trimester to diagnosis genetic studies. It cannot detect neural tube defect. Nursing interventions: Prevent infection→ aseptic care Cover lesion with moist sterile dressing Position on abdomen or semi-prone because of bulging sack Calorie restriction to prevent obesity Monitor for ICP: Bulging fontanels, cries, irritability & spreading suture lines. Late sign→ Sundown eyes. Care of a child on Cerebral Palsy movement and posture development disorder resulting in activity limitations. Spasticity interferes with muscle & bone growth. Cause: Unknown S/S: Muscle instability, hypotonia, seizures. Clinched fists. Promote safety with proper mobility devices including safety belts & helmets. High calorie diet and increase fiber Follow up with care teams: PT, OT Baclofen is administered (O) or Pump to ↓ spasticity/spasms. Side effect: Hypotonia. Ranitidine effective in ↓ GI side effects of CP Botulinum toxin injections help temporarily control of spasticity. Risk for Neurological Injury Differences Ped & Adult -Top heavy large head -Neck muscles weak→ Contrecoup brain injury→ Concussion Priority: Hemorrhage, ICP, LOC. Family Edu: Come back to ER if unable to arose. Vomiting. headaches. Change in gait. Eye disturbance. No contact sports for 6 months. -Skull expands until 2yr→ICP that can split open sutures -Prone to brain injury when falling Neurological Assessment Pediatric Patient Assessment: irritable, not want to eat, high-pitched cry, split sutures for ICP, full/bulging, LOC Fontanel… Toddlers→ owwie, confused •Pupils (PERRLA), Fixed, uneven pupils→ herniation medical emergency •Central Nervous System Checks) Neuro (1) MSK: face symmetry, tone are they strong (2) Motor: No response to painful stimuli (3) Sensation: younger kids they would move from sensation. (a) Unconscious →corneal reflex (cotton on eye and see if blink) (b) Gag reflex (abnormal function of cranial nerves) (c) Dolls → (neg response) turns head and eyes are midline (cranial nerve damage) •Glasgow Coma Scale <8 intubate. Late sign (1) Fixed, uneven pupils→ herniation medical emergency (2) Cushing’s triad →increase BP (trying to perfuse brain), ↓ HR, irregular respirations, wide BP pressure readings= ICP. •Posturing→ Decorticate (Love), Decerebrate (wrist out)→stiff, abducted, hype pronated, plantar feet. Increased Cranial Pressure→ Normal ICP is <15. Tx required >20mmHg. Priorities 1. Airway, Aspiration 2. Cerebral blood flow – elevated HOB Semi-fowlers, midline, decrease stimulation, higher Na+ & serum osmolarity for HYPER state so fluid goes out of brain and into vessel. a. Meds→ mannitol (osmotic diuretic) ↓ blood viscosity, pulls fluid from brain = ↑ U.output b. Hypertonic Saline 2-3% to drive Na+ up needs Central line w/ 3% (pulls fluid from brain). 3. CT, MRI, nuclear brain scan, EEG, X-Ray →once stable •Signs/symptoms Early Dizziness/Vertigo Diplopia/Visual Changes Changes in LOC Restless/Irritable (control this short goal) Pupils not as reactive Bulging Fontanel/ Widened Sutures High Pitch Cry Late Significant decrease in LOC Cushing Triad Fixed Dilated Pupils Papilledema on eye exam •Management HOB 30 degree, midline. NO ROM exercises Turning side to side by Log roll. Avoid activities that may ↑ ICP. (cluster care, dark environment) Sedation given for things patient cant tolerate like: Suctioning. Close neuro assessment (Cushing’s, LOC, N/V, headaches) ICP monitor? EVD Medications to decrease Mannitol, 3 % NS given central line CO2 causes→ vasodilation, ↑ cerebral blood flow, ↑ ICP. Co2 should be 35-38mmHg. Give O2. Intraventricular monitor placed for Cerebral edema=fluid restriction Care of Pediatric Patient with Seizures Abnormal electrical discharge from the brain to body. They can be focal or generalized. Epilepsy= repeated seizures. Hyponatremia=Seizures Q: What was child doing? What movements were seen? How long episodes last? Tonic-Clonic Absence Infantile Spasms Tonic (arms up, body stiff), Absent (A lot more of) (3-12Y) – Infantile spasm (form of Clonic (rhythmic jerking last 5-10 secs rarely exceed epilepsy, hard to treat)– 4-18M motion) 1-2 mins and followed 30sec. Monitor for brief 50-100x a day by post seizure phase lasting interruptions. (May stop talking) a. Jerking mins – hrs a. Triggered by flashing lights, b. Stare, eye blinking A.) Drooling/secretion not hyperventilation c. Tonic-Clonic swallowed b. 15sec Stare off then blink d. Lip smacking B.) Eyes rolling, dilated. c. Eye fluttering e. regression developmental Never use oral thermometer d. Lip smacking milestones/delays Febrile Seizures→ occurs high temp. Prophylaxis rarely done. Diazepam rectal. tepid bath will bring down the temperature; patting, instead of rubbing, will help keep the child’s temperature down and ↑ oral fluids. Nursing care/Meds Home management i. Airway→ suction, O2 i. Triggers ii. Assess neuro 5-10min→v/s, circulation ii. CPR training iii. Med Benzodiazepines (Lorazepam, diazepam) SE: Hypotension, resp depression, tachycardia Phenobarbital for long-term→ give Vit D and folic acid for nutrition cause sedation SE: Nystagmus.→ collect blood specimen. Phenytoin(Dilantin) →frequent dental care, change in urine color (pink-brown shades) Carbamazepine (Tegretol) →photosensitivity Valproic acid (Depakote) given w/ foods to ↓ gastrointestinal irritation. iii. Rectal diazepam iv. Activity restrictions v. Safety devices → no swimming alone iv. IV access (patent) v. Protect from injury vi. Thermoregulation→ Fever r/t febrile seizure Status Epilepticus Last more than 20 minutes or 2 or more seizures without return to baseline in between. Series of seizures where child does not regain baseline LOC Medical ER that can lead to brain damage, respiratory failure, & arrest. Treatment : Maintain AIRWAY, IV→ Versed or Ativan, Phenobarb, Diastat per rectum if no IV.