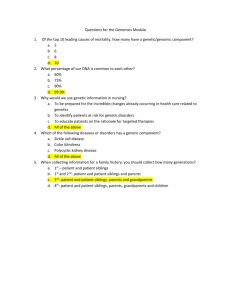
SAVIOR SIBLINGS INTRODUCTION Sickle cell disease(SCD) is a group of inherited red blood cell diseases. Sickle cell disease was first described in 1910 in a dental student with pulmonary symptoms. Herrick coined the term "sickle" to describe the unusual appearance of his patient's red blood cells(Figure 1.0). Healthy red blood cells are round and move through small blood vessels to carry oxygen to all parts of the body. However, the patient who with SCD, red blood cells will become hard and sticky. The sickle cell dies prematurely, leading to a persistent shortage of red blood cells. This will lead to pain and other serious problems. For example, acute chest syndrome and stroke. The advanced and appropriate stem cell therapy provide for the patient to cure the SCD is called “savior siblings’. It refers to the child provide an organ or cell transplant for his or her sibling patient who has the disease difficult to cure, cancer or anemia, stem cell transplantation can best be treated. Figure 1.0 EPIDEMIOLOGY Sickle cell disease affects millions of people worldwide. It’s particularly common among those the ancestors from sub-Saharan Africa; Spanish-speaking areas of the Western Hemisphere (South America, the Caribbean, and Central America); Saudi Arabia; India; Turkey, Greece, Italy and other Mediterranean countries. It is estimated that: SCD affects about 100,000 Americans. SCD occurs in about 1 in every 365 black or African-American babies. SCD occurs in about 1 in every 16,300 Hispanic births. Figure 1.1 About 1 in 13 black or African American babies is born with sickle cell trait . BIOLOGICAL MECHANISM Patients with sickle cell disease are at increased risk of clinically obvious depressive symptoms due to chronic stress caused by multiple disease factors. SCD complications may increase this risk by interacting with the biological processes behind stress and depression. It is now understood that the potential emergence of psychopathology depends on the unique interaction between the pressure in the environment and a person's vulnerability to mental illness.Depressive mood disorders often co-occur with SCD. The prevalence of clinical depression in children with 8 -14 SCD varied from 25% to 56% from one study to another. Among adults, rates of depression were similar to those of other chronic diseases, but ranged from 18 percent to 44 percent, far higher than the 6.8 percent to 7.5 percent reported by African Americans in the general population. Complications of the disease (including fatigue, neurological problems, growth retardation and recurrent pain), combined with multiple stress or such as high frequency of hospitalization and low socioeconomic status, have been associated with depression in depressed patients. SCD. However, the main causal direction of these effects is uncertain, as depression can be predicted, occur with or contribute to these complications. Characteristics Female, n (%) Age, y, mean (SD) SCD with depression* (n = 50) SCD without depression† (n = 92) P 36 (72.0) 45 (48.9) <.01 35.4 (11.8) 33.7 (13.4) .44 Age group, y, n (%) .98 18-34 28 (56.0) 51 (55.4) — 35-49 15 (30.0) 29 (31.5) — ≥50 7 (14.0) 12 (13.0) — 42.4 (72.7) 31.9 (40.0) .27 BMI, kg/m2, mean (SD) SCD diagnosis, n (%) .18 SS 28 (56.0) 63 (68.5) — 1 (2.0) 5 (5.4) — SC 15 (30.0) 20 (21.7) — Sβ+ thalassemia 5 (10.0) 4 (4.4) — SOArab 1 (2.0) 0 (0.0) — Sβ0 thalassemia Severity score, n (%) .93 0 11 (22) 23 (25) — 1 18 (36) 36 (39) — 2 11 (22) 20 (22) — 3 7 (14) 9 (10) — 4 3 (6) 4 (4) — Insurance, n (%) .75 Medicaid 19 (44.2) 41 (52.6) — Medicare 10 (23.3) 14 (18.0) — Private 7 (16.3) 13 (16.7) — No insurance/self-pay 2 (4.7) 5 (6.4) — Other 5 (11.6) 5 (6.4) — SOLUTION Table 1.2 The savior siblings can be used for any disease that is treated with solution through hematopoietic stem cell transplantation. It is targeted at genetic testing (mainly effective single gene) for diseases such as fanconi anemia, congenital pure anemia and thalassemia, in which the fattening brother can be selected as the savior of the brother who did not inherit the disease. The procedure can also be used for children with leukaemia, in which HLA matching is the only requirement and does not rule out any other obvious genetic disease.Multiple embryos are created and preimplantation genetic diagnosis is used to detect and select those embryos that are free of genetic diseases and hLA-matched to existing siblings requiring transplantation. At birth, cord blood is used for hematopoietic stem cell transplantation. Figure1.3 By the way,Messianic siblings will feel that the only reason they were brought into this world is to serve as spare bodies for their siblings, not because their parents wanted another child. This sense of being used will mock them for life, because they were born "on purpose" in this they get older they may feel unloved or unwanted, especially if their siblings die, as they will be useless. If they can no longer achieve their goals, then what's the point of living? Throughout their lives, they had been donating to their siblings and doing what they were supposed to do, and when that was no longer possible, their lives seemed hopeless. ETHICS&ONE WORLD PROBLEM Is it ethical for parents to create messianic siblings? Some argue that parental intent plays a role in considering whether it is ethical to create a messianic sibling. If parents do not intend to have any more children and they only have messianic siblings for the sake of older children, then there is a fear of using messianic siblings as a means to an end. If the parents plan to have more children, then some claim that the messianic sibling was created for her/his own sake and not just for one purpose. The factors from environmental also cause this problem. We often use people as a means to an end, but we don't use them entirely as ends, and that's a significant difference. People often have a second child for the benefit of the first child: they think it's important for the first child to have a sibling as a playmate, to bring the family closer together and so on. Even if the messianic sibling is well loved, there is concern that the child may always feel like a means, at least to some extent. Some believe that the savior's siblings will feel special or even heroic for the role they play in the family, while others worry that they will be psychologically hurt because they always feel like a second fiddle or succedaneum. Possible exploitation of children, such as the potential adverse psychological effects on children born not for themselves but to save others, and the possible emotional reaction of savior siblings upon discovering they were born alone to save the recipient's life, rather than being "wanted" for reasons other than transplantation. From the world's point of view, obviously, it’s not ethical to create the savior siblings. Their existence based on the purpose and utilitarianism. They are meaningless after they provide the organs to their siblings. This is antithetical to philosophy. We could resist more and more savior siblings become the tool or the “medium” to save others. Reference List: Haywood C., Jr (2013). Disrespectful care in the treatment of sickle cell disease requires more than ethics consultation. The American journal of bioethics : AJOB, 13(4), 12–14. https://doi.org/10.1080/15265161.2013.768857 Adam, S. S., Flahiff, C. M., Kamble, S., Telen, M. J., Reed, S. D., & De Castro, L. M. (2017). Depression, quality of life, and medical resource utilization in sickle cell disease. Blood advances, 1(23), 1983–1992. https://doi.org/10.1182/bloodadvances.2017006940 Frenette, P. S., & Atweh, G. F. (2007). Sickle cell disease: old discoveries, new concepts, and future promise. The Journal of clinical investigation, 117(4), 850–858. https://doi.org/10.1172/JCI30920 Strong, K., Kerridge, I., & Little, M. (2014). Savior siblings, parenting and the moral valorization of children. Bioethics, 28(4), 187-193. Trujillo, J. P., & Surralles, J. (2015). Savior siblings and Fanconi anemia: analysis of success rates from the family’s perspective. Genetics in Medicine, 17(11), 935-938. Ohene-Frempong, K., Weiner, S. J., Sleeper, L. A., Miller, S. T., Embury, S., Moohr, J. W., ... & Sickle Cell Disease, T. C. S. O. (1998). Cerebrovascular accidents in sickle cell disease: rates and risk factors. Blood, The Journal of the American Society of Hematology, 91(1), 288-294. Bunn, H. F. (1997). Pathogenesis and treatment of sickle cell disease. New England Journal of Medicine, 337(11), 762-769. Steinberg, M. H. (1999). Management of sickle cell disease. New England Journal of Medicine, 340(13), 1021-1030.