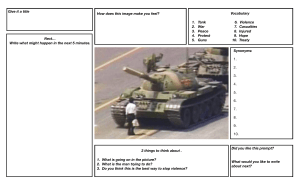
RISK ASSESSMENT AND MANAGEMENT OF AN AGGRESSIVE PATIENT SUMMARY OF CONTENTS OUR MAIN TOPICS TODAY DEFINITION TYPES OF AGGRESSION EPIDEMIOLOGY ETIOLOGY RISK FACTOR IDENTIFICATION TRAINING ISSUES EARLY WARNING SIGNS SPECIAL CONSIDERATION INTERVENTIONS PHARMACOLOGICAL TREATMENT CALIFORNIA STATE HOSPITAL VIOLENCE ASSESSMENT AND TREATMENT (CAL-VAT) GUIDELINES REFERENCES Pixelast | Design and Tech DEFINITION Agitation: a state of heightened arousal that can manifest in a variety of ways, from subtle increases in psychomotor activity to aggressive and/or violent behavior May be caused by a psychiatric disorder, substance use, or occur as a result of a general medical condition, e.g., hypoglycemia or traumatic brain injury There may also be no underlying medical reason and it may simply be a reaction to stressful or extreme circumstances. refers to behavior intended to cause physical injury to others, is descriptive by virtue of its shortterm consequence, harm to others ( Kaplan) The words “aggression” and “violence” are sometimes used synonymously, but in reality, aggression can be physical or non-physical, and directed either against others or oneself. Violence is more of a use of force with an intent to inflict damage. Aggression refers to a heterogeneous construct with substantial semantic overlap with terms for many forms of behaviour with the intent to harm others (Ramirez 2011). Kaplan and Sadock (2007) are of the opinion that many behaviours are aggressive, even though they do not involve direct physical injury. Examples of this behaviour are verbal aggression, coercion, intimidation and social ostracism of others EPIDEMIOLOGY Emergency Care Providers has experienced patient aggression and / or physical assault ETIOLOGY TYPES OF AGGRESSION One study looked at the principle types of aggression and violence that occur in psychiatric patients, and broke it down into three categories: Impulsive violence (the most common category) Predatory violence (purposeful and planned violence) Psychotically-driven violence (least common) IMPULSIVE VIOLENCE Impulsive violence or aggression is actually the most common, and in many ways the most complex, form of violence that occurs in a variety of mental illnesses, including: psychosis mood disorders personality disorders anxiety disorders PTSD Predatory violence is what people typically think of when they think of psychopathy, or someone with antisocial personality disorder. It is violence with a purpose, and that purpose is usually to gain something. They typically show a lack of fear and very little autonomic arousal even when they are being violent. The amygdala and the temporal lobe is underactive and the communication between them has a weak signal. People with predatory violence also have lower affective empathy PSYCHOTIC AGGRESSION Psychotically driven aggression is most often a result of delusional ideation or the belief the person holds that they are in some way being persecuted and being taken advantage of. Psychotic or mentally ill people do have an increased rate of violence compared to the general population. The mentally ill are responsible for around 5% violent crimes, meaning non mentally ill people are responsible for 95%. PSYCHOTIC DELUSIONS LEADING TO VIOLENCE One study looking specifically at the first episodes of psychosis found that in about 458 patients, anger was associated with certain types of delusions that led to the violence (Coid, 2013). The underpinnings of delusion-driven violence usually stems from when people have delusional beliefs that are persecutory in nature. When they believe that someone is out to get them, it removes inhibitions against acting out violently, because that person’s view is they are protecting themselves. Typically, this violence comes from the belief they are being spied on or persecuted. IQ AND AGGRESSION There is also an association between the IQ and aggression (Huesmann, 1987). A recent study in state hospitals looked at what correlated with persisting violence, and across all of the types of violent behavior, cognitive deficits (particularly impairments and executive functioning) were associated with elevated rates of violence. RISK FACTOR IDENTIFICATION There are various approaches to prediction of violence. A clinical prediction is based on an evaluator’s skill, experience, and knowledge Violence risk assessment predictive ability of clinicians and risk identification in pts. Static risk factors are those that either cannot be changed (e.g., age, sex) or are not particularly amenable to change (e.g., psychopathic personality structure.) Dynamic risk factors are those that are amenable to change (e.g., substance abuse, psychotic symptomatology) (Otto, 2000) 4 main domains of risk factors: - dispositional (e.g., demographic, personality, and cognitive variables); -historical (e.g., social history, prior hospitalization and treatment compliance, and history crime and violence); - contextual (e.g., perceived stress, social support and means for violence) -clinical (e.g., diagnosis, symptom patterns, functioning, and substance abuse (Borum, 1996) DISPOSITIONAL RISK FACTORS demographic, personality, racial and other descriptive aspects Gender - males violent more than females, however this is not applicable in mentally ill population. Age- late teens and early twenties are at the highest risks Swanson et al. (1990) found that being male, young and of lower SES increased the risk of violence substantially apart from psychiatric illness Racial boundaries- African- American have high rates of violence compared to Caucasian. According to Swanson et al. (1990), these differential rates disappear when socioeconomic status (SES) is controlled. Determining the role of SES in violent behavior is complicated. Inherent in the determination of SES is confounding factors including; social/neighborhood stress, financial and social resources and other contextual factors (Sampson, Raudenbush, & Earls, 1997) HISTORICAL RISK FACTORS IMPORTANT risk factor in determining risk for future violence The younger an individual is when the first incident of violence and law violation occurs, the higher the risk of violence later in life. It has also been well documented that youth exposed to violence, including those who have been victims of violence, are at an increased risk of becoming aggressive or delinquent (Gorman-Smith & Tolan, 1998). CLINICAL RISK FACTORS Clinical risk factors are diagnostic, symptomatic and functional information about a patient that increases the potential for violent acts in that particular patient. A diagnosis of substance abuse or dependence in mentally ill persons significantly increases the risk for violent behavior directed towards others (Swanson, Holzer, Ganzu et al., 1990) Violence can also occur during the manic phase of bipolar disorder. This can be due to psychosis or gross disorganization of thoughts or behavior (Binder & McNeil, 1988). In assessment of such individuals, consideration of impulsivity, irritability, impaired judgment and impaired decision-making associated with manic episodes and other types of disorders is indicated given the increased prevalence of violence among this group of patients (Otto, 2000) Several of the personality disorder diagnoses have been associated with violence in several contexts. The potential for violence in patients with personality disorders has been related to the degree of psychopathy (Hare, 1998). For example, Tardiff (1998) suggests that though a patient with antisocial personality disorder may appear glib or attractive, the clinician should be prepared for the possibility of violence if the patient’s self-esteem or self-image is threatened. Tardiff goes further to describe violence in persons with borderline personality disorder as a manifestation of affective instability or manipulation and asserts that violence can also occur if such a person feels rejected or abandoned. TRAINING ISSUES First, the clinician must be educated about what information to gather regarding risk. Then, the information must be gathered. This information must be used to estimate risk. And, finally, the clinician must communicate the risk assessment to other members of the team and to those who are responsible for making or implementing the final clinical decision EARLY WARNING SIGNS using acute symptoms as indicators of short-term risk of violence There are many signs that characterize patients that are likely to assault clinicians. Some represent the mental state of the patient, e.g., anger, confusion, hallucinations, excitement, uncooperativeness and impulsivity Chanting, a clenched jaw, flared nostrils, flushed face and clenched or gripping hands are all signs of imminent violence Demanding immediate attention, pacing, restlessness, pushing or slamming things, yelling, profanity, physical aggressiveness and verbal threats can all be early indicators of pending violence Bell (2000) further elaborates warning signs of imminent violence including eye movement and appearance (such as dilation of the pupil or darting eye movements), proximity (such as a patient invading the clinician’s personal space), inability to comply with reasonable limit setting and patient’s perception of fear in the clinician. SPECIAL CONSIDERATION 1. Gender issues 2. Geriatric Patients(older adults) 3. Mental retardation 4. Children and adolescents RISK ASSESSMENT AND MITIGATION Verbal signs Expression of frustration or anger Loud, threatening, or insulting speech Repetitive mumbling Behavioral signs - Suspicious or angry affect -Staring or avoidance of eye contact -Pacing and/or restlessness -Threatening gestures -Signs of anxiety or agitation Other patient factors Evidence of drug or alcohol use Presence of a weapon Rapid risk assessment Call an attending as early as possible and always follow hospital protocol. Approach each patient based on their individual risk assessment. INTERVENTIONS In order for an intervention to be applied appropriately an assessment of the patient’s current risk for violence must be completed. Consideration of dispositional, historical, contextual and clinical risk factors along with gender, age and intellectual capacity will assist in this assessment the presence or absence of the early warning signs discussed previously will assist the clinician in estimating the urgency of the patient’s risk for violence. INTERVENING WITH VIOLENT PATIENTS categorized into potential, imminent and emergent risk potential : large number of risk factors but no acute risk imminent: early warning signs but have not acted out violently yet emergent: pts who are actively engaged in violence against another person EMERGENTLY VIOLENT PATIENTS Insuring the safety of self and others in the vicinity is the most important factor. If the clinician cannot maintain his/her own safety then she can be of no use to anyone else. As such, self-defense measures may also be warranted for the clinician that is isolated or in a situation where help is not readily available When help is present, someone should call for appropriate assistance immediately. If staff trained in restraint are not available then building security or local police can be summoned The clinician should create a safety zone around the patient and clearly identify him/herself as the team leader. No one should be within arm’s length of the patient. Depending on the setting, parenteral medication may also be an option. In situations of emergent violence, physical restraint is often initiated prior to administration of parenteral medication as a highly agitated and emergently violent patient is unlikely to be predictably safe during the administration of the medication. Once safety has been secured the clinician must begin to assess an appropriate disposition for the patient. If psychiatric symptoms are the primary cause of the violence then involuntary psychiatric hospitalization may be required. If there is no acute psychiatric illness mediating the violent behavior police intervention may be warranted. Persons with medical illnesses that have contributed to their violent presentation will likely need referral for appropriate medical care in an environment that can also provide containment while the medical condition is stabilized IMMINENTLY VIOLENT PATIENTS early warning signs two forms of intervention: patient focused and environmental The primary focus of patient focused interventions is de-escalation. Good rapport is an important tool when attempts at verbal de-escalation are made Offering medication empathetically, rather than as a threat, allows the patient to feel a much need sense of control while also having the potential to contribute to deescalating the situation. If these interventions appear to be working, the clinician should continue using a calm, supportive tone of voice. Further reduction of external stimuli can occur. If the attempts at de-escalation are not successful and the patient continues to escalate to emergent violence then the clinician should begin with the interventions for that subset of violent patients as described in the previous slides. POTENTIALLY VIOLENT PATIENT Patients with a potential for violent behavior have been identified as a result of the aforementioned risk assessment. If there is no acute threat the clinician is afforded the opportunity to complete a comprehensive psychiatric evaluation. The underlying psychiatric and non-psychiatric contributors will be identified. The clinician should, with the patient’s consent, treat any underlying psychiatric disorders that are contributing to the patient’s risk of violence. The appropriate treatment setting for potentially violent patients should be carefully assessed. These settings might include outpatient clinic, inpatient hospitalization, day hospital, or referral for specialized treatments such as substance abuse. If non-psychiatric contributors to the potential for violence are identified the clinician should work with the patient on modifying these risk factors. For example, if the current living situation is a stressor and exacerbates the patient’s potential for violence then a referral to social work to explore alternatives may be in order. While these interventions do not provide immediate solution they do address the long term problems and mediate future risks PHARMACOLOGY TREATMENT Drug treatment (kaplans) Anticonvulsants – reduce seizure induced form of aggression Antipsychotics- reduce aggression in both psychotic and nonpsychotic violent patients Lithium – for violent patients Antidepressants- effective in reducing violence in depressed pts B blockers and stimulants – effective in children benzodiazepine Lorazepam commonly used due to its rapidity of action, effectiveness, short half-life, and intramuscular (IM) or intravenous (IV) route of administration . usual dose is 0.5 to 2 mg IV or IM. may cause respiratory depression. Clinicians must be vigilant about monitoring the respiratory function of patients receiving benzodiazepines, either alone or in combination with other drugs. In agitated but cooperative patients, benzodiazepines may be given orally using the same doses first generation antipsychotics a)Haloperidol used effectively for many years to control violent and agitated patients . It can be given IM, or orally It is usually given in doses of 2.5 to 10 mg. All first-generation antipsychotics possess cardiac effects resulting in QT prolongation, with the potential for causing dysrhythmias. b) Chlorpromazine- Treats underlying psychosis therefore longer effect on aggression u Second-generation or atypical antipsychotics ziprasidone 10 to 20 mg IM -used to treat agitated schizophrenic and bipolar patients risperidone -useful in controlling agitation in the elderly olanzapine 10mg----- reduces acute agitation in patient with schizophrenia antidepressants reduce fear, irritability, and anxiety decreases negative mood and aggressive attacks, impulsiveness and irritability in personality disorder patients with posttraumatic agitation Fluoxetine -shown to reduce impulsiveness in patients with borderline personality disorder, but has also been blamed for inducing homicide or suicide. Therefore, it is recommended that this medication be used with caution in aggressive patients. mood stabilizers used to treat aggression, although they are not prototypical for this purpose. Valproate has been used to control aggression in dementia, borderline personality disorder, organic mood syndrome, bipolar disorder, schizophrenia, schizoaffective disorder, and mental retardation. carbamazepine is also used to treat the aggressive symptoms of dementia. lithium carbonate reduces Aggression during manic episodes. Lithium is also used for the aggressive features of mental retardation, and violent behavior of recurrently violent prisoners. REFERENCES Adams, D. & Alien, D. (2001). Assessing the need for reactive behavior management strategies in children with intellectual disability and severe challenging behavior. Journal of Intellectual Disability Research, 45(4), 335--343 Bell, C. C. (2000). Assessment and management of the violent patient. Journal of the National Medical Association, 92(5), 247--253. Bell, C. C., Blount, M. A., & Anderson, T. R. (2002). At work with threats and violence. In P. Backlar, & D. L.Cutler, (Eds.), Ethics in Community Mental Health Care. New York: Kluwer Academic/Plenum Borum, R. (1996). Improving the clinical practice of violence risk assessment. American Psychologist, 51, 945--956. Caracci, G. & Mezzich, J. E. (2001). Culture and urban mental health. Psychiatric Clinics of North America, 24(3), 581--593 Carlsen, D. L., Fleming, K. C., Smith, G. E., et al. (1995). Management of dementia-related behavioral disturbances: A nonpharmacologic approach. Mayo Clinical Proceedings, 70(11), 1108--1115. Chadwick, O., Walker, N., Bernard, S., et al. (2000). Factors affecting the risk of behavior problems in children with severe intellectual disability. Journal of Intellectual Disability Research, 44(2), 108--123 https://www.psychiatrypodcast.com/psychiatrypsychotherapy-podcast/how-to-treat-violent-andaggressive-patient https://www.psychiatrypodcast.com/psychiatrypsychotherapy-podcast/how-to-treat-violent-andaggressivepatients#:~:text=%E2%80%9CCalifornia%20State%20 Hospital%20Violence%20Assessment%20and%20Tre atment%20(Cal-VAT)%20guidelines%E2%80%9D